Implications of Preoperative C-Reactive Protein Levels in Heart Transplant Patients—A Single-Center Retrospective Study
Abstract
1. Introduction
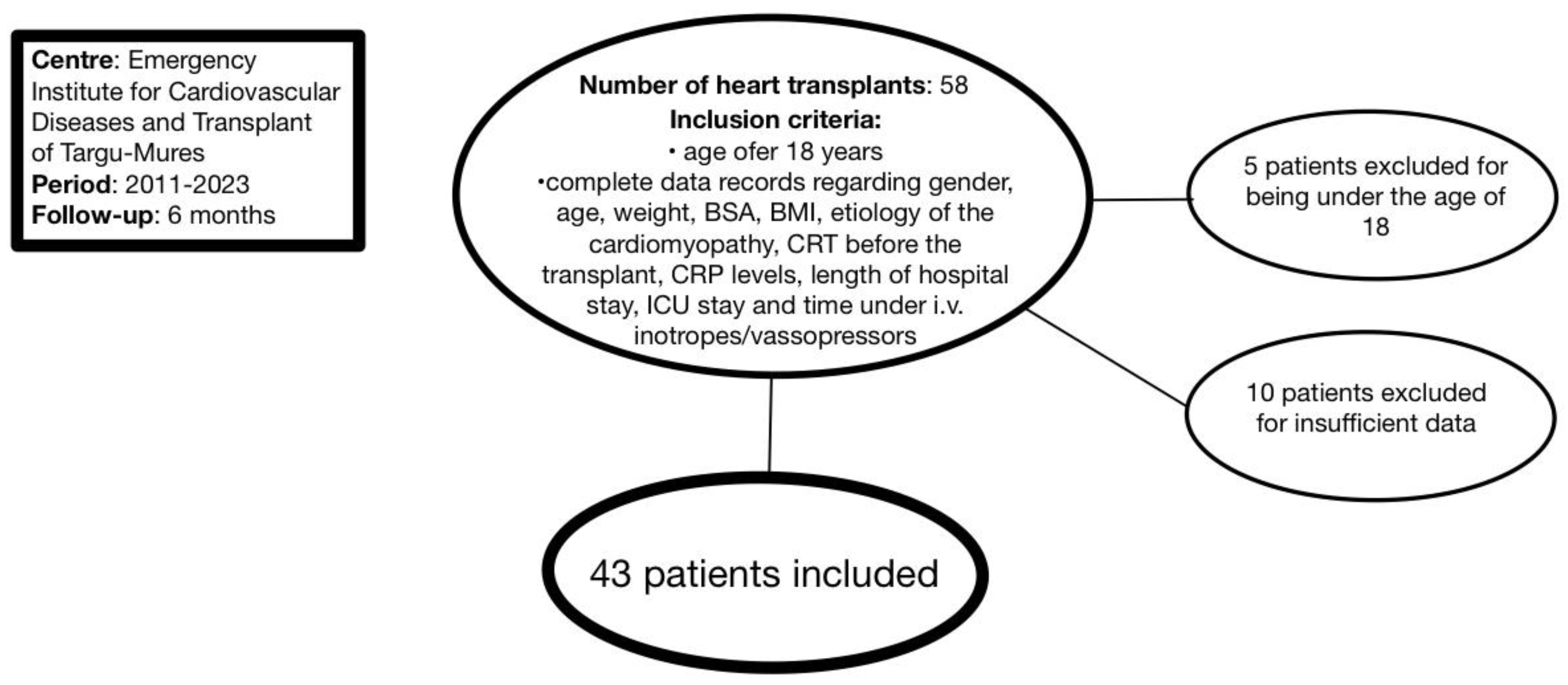
2. Materials and Methods
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ammar, K.A.; Jacobsen, S.J.; Mahoney, D.W.; Kors, J.A.; Redfield, M.M.; Burnett, J.C., Jr.; Rodeheffer, R.J. Prevalence and Prognostic Significance of Heart Failure Stages: Application of the American College of Cardiology/American Heart Association Heart Failure Staging Criteria in the Community. Circulation 2007, 115, 1563–1570. [Google Scholar] [CrossRef] [PubMed]
- Mohebi, R.; Wang, D.; Lau, E.S.; Parekh, J.K.; Allen, N.; Psaty, B.M.; Benjamin, E.J.; Levy, D.; Wang, T.J.; Shah, S.J.; et al. Effect of 2022 ACC/AHA/HFSA Criteria on Stages of Heart Failure in a Pooled Community Cohort. J. Am. Coll. Cardiol. 2023, 81, 2231–2242, Erratum in J. Am. Coll. Cardiol. 2023, 82, 1051. [Google Scholar] [CrossRef] [PubMed]
- Bozkurt, B.; Ahmad, T.; Alexander, K.M.; Baker, W.L.; Bosak, K.; Breathett, K.; Fonarow, G.C.; Heidenreich, P.; Ho, J.E.; Hsich, E.; et al. Heart Failure Epidemiology and Outcomes Statistics: A Report of the Heart Failure Society of America. J. Card. Fail. 2023, 29, 1412–1451. [Google Scholar] [CrossRef] [PubMed]
- Bacușcă, A.E.; Burlacu, A.; Tinică, G.; Enache, M.; Ţărus, A.; Gavriluţă, C.; Brinza, C.; Hanganu, B.; Ioan, B.G. Organ Procurement, Donation, and Transplant Awareness in an Urban Eastern European Region: A General Population Survey. Ann. Transplant. 2022, 27, e938016. [Google Scholar] [CrossRef]
- Wilhelm, M.J. Long-Term Outcome Following Heart Transplantation: Current Perspective. J. Thorac. Dis. 2015, 7, 549. [Google Scholar] [CrossRef] [PubMed]
- Awad, M.A.; Shah, A.; Griffith, B.P. Current Status and Outcomes in Heart Transplantation: A Narrative Review. Rev. Cardiovasc. Med. 2022, 23, 11. [Google Scholar] [CrossRef]
- Alyaydin, E.; Welp, H.; Reinecke, H.; Tuleta, I. Predisposing Factors for Late Mortality in Heart Transplant Patients. Cardiol. J. 2021, 28, 746–757. [Google Scholar] [CrossRef]
- Frye, C.C.; Bery, A.I.; Kreisel, D.; Kulkarni, H.S. Sterile Inflammation in Thoracic Transplantation. Cell Mol. Life Sci. 2021, 78, 581–601. [Google Scholar] [CrossRef]
- Gondi, K.T.; Kaul, D.R.; Gregg, K.S.; Golbus, J.R.; Aaronson, K.D.; Murthy, V.L.; Konerman, M.C. Cytomegalovirus Infection Is Associated with Impaired Myocardial Flow Reserve after Heart Transplantation. J. Heart Lung Transplant. 2024, 43, 432–441. [Google Scholar] [CrossRef]
- Schonian, U.; Crombach, M.; Maser, S.; Maisch, B. Cytomegalovirus-Associated Heart Muscle Disease. Eur. Heart J. 1995, 16, 46–49. [Google Scholar] [CrossRef]
- Labarrere, C.A.; Woods, J.R.; Hardin, J.W.; Jaeger, B.R.; Zembala, M.; Deng, M.C.; Kassab, G.S. Early Inflammatory Markers Are Independent Predictors of Cardiac Allograft Vasculopathy in Heart-Transplant Recipients. PLoS ONE 2014, 9, e113260. [Google Scholar] [CrossRef] [PubMed]
- Battes, L.C.; Caliskan, K.; Rizopoulos, D.; Constantinescu, A.A.; Robertus, J.L.; Akkerhuis, M.; Manintveld, O.C.; Boersma, E.; Kardys, I. Repeated Measurements of NT-pro-B-Type Natriuretic Peptide, Troponin T, or C-Reactive Protein Do Not Predict Future Allograft Rejection in Heart Transplant Recipients. Transplantation 2015, 99, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, M.S.; Chen, H.J.; Warshofsky, M.K.; Sciacca, R.R.; Wasserman, H.S.; Schwartz, A.; Rabbani, L.R.E. Elevated Levels of Plasma C-Reactive Protein Are Associated with Decreased Graft Survival in Cardiac Transplant Recipients. Circulation 2000, 102, 2100–2104. [Google Scholar] [CrossRef]
- Toscano, G.; Bottio, T.; Gambino, A.; Bagozzi, L.; Guariento, A.; Bortolussi, G.; Gallo, M.; Tarzia, V.; Gerosa, G. Orthotopic Heart Transplantation: The Bicaval Technique. Multimed. Man. Cardiothorac. Surg. 2015, 2015, mmv035. [Google Scholar] [CrossRef]
- Kittleson, M.M. Changing Role of Heart Transplantation. Heart Fail. Clin. 2016, 12, 411–421. [Google Scholar] [CrossRef]
- Hognestad, A.; Endresen, K.; Wergeland, R.; Stokke, O.; Geiran, O.; Holm, T.; Simonsen, S.; Kjekshus, J.K.; Andreassen, A.K. Plasma C-Reactive Protein as a Marker of Cardiac Allograft Vasculopathy in Heart Transplant Recipients. J. Am. Coll. Cardiol. 2003, 42, 477–482. [Google Scholar] [CrossRef] [PubMed]
- Radley, G.; Pieper, I.L.; Ali, S.; Bhatti, F.; Thornton, C.A. The Inflammatory Response to Ventricular Assist Devices. Front. Immunol. 2018, 9, 2651. [Google Scholar] [CrossRef]
- Donlon, N.E.; Mohan, H.; Free, R.; Elbaghir, B.; Soric, I.; Fleming, C.; Balasubramanian, I.; Ivanovski, I.; Schmidt, K.; Mealy, K. Predictive Value of CRP/Albumin Ratio in Major Abdominal Surgery. Ir. J. Med. Sci. 2020, 189, 1465–1470. [Google Scholar] [CrossRef]
- Zhang, H.; Shi, J.; Xie, H.; Liu, X.; Ruan, G.; Lin, S.; Ge, Y.; Liu, C.; Chen, Y.; Zheng, X.; et al. Superiority of CRP-Albumin-Lymphocyte Index as a Prognostic Biomarker for Patients with Gastric Cancer. Nutrition 2023, 116, 112191. [Google Scholar] [CrossRef]
- Pham Vu, T.; Nguyen Thi Thuy, D.; Truong Quy, K.; Nguyen Thi Thu, H.; Nguyen Van, D.; Diem Thi, V.; Do Manh, H.; Nguyen Trung, K.; Do, Q.; Tran Viet, T.; et al. Serum hs-CRP Measured Prior to Transplantation Predicts New-Onset Diabetes After Transplantation in Renal Transplant Recipients. Transpl. Immunol. 2021, 66, 101392. [Google Scholar] [CrossRef]
- Uzum, Y.; Turkkan, E. Predictivity of CRP, Albumin, and CRP to Albumin Ratio on the Development of Intensive Care Requirement, Mortality, and Disease Severity in COVID-19. Cureus 2023, 15, e33600. [Google Scholar] [CrossRef] [PubMed]
- António, N. Reduction of Systemic Inflammation After Cardiac Resynchronization Therapy: A New Form of Response? Rev. Port. Cardiol. 2018, 37, 115–116. [Google Scholar] [CrossRef] [PubMed]
- Lappegård, K.T.; Bjørnstad, H.; Mollnes, T.E.; Hovland, A. Effect of Cardiac Resynchronization Therapy on Inflammation in Congestive Heart Failure: A Review. Scand. J. Immunol. 2015, 82, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Shinohara, T.; Takahashi, N.; Saito, S.; Okada, N.; Wakisaka, O.; Yufu, K.; Hara, M.; Nakagawa, M.; Saikawa, T.; Yoshimatsu, H. Effect of Cardiac Resynchronization Therapy on Cardiac Sympathetic Nervous Dysfunction and Serum C-Reactive Protein Level. Pacing Clin. Electrophysiol. 2011, 34, 1225–1230. [Google Scholar] [CrossRef]
- Bilchick, K.; Kothari, H.; Narayan, A.; Garmey, J.; Omar, A.; Capaldo, B.; McNamara, C. Cardiac Resynchronization Therapy Reduces Expression of Inflammation-Promoting Genes Related to Interleukin-1β in Heart Failure. Cardiovasc. Res. 2020, 116, 1311–1322. [Google Scholar] [CrossRef]
- Abraham, W.T.; Hayes, D.L. Cardiac Resynchronization Therapy for Heart Failure. Circulation 2003, 108, 2596–2603. [Google Scholar] [CrossRef]
- Auricchio, A.; Stellbrink, C.; Sack, S.; Block, M.; Vogt, J.; Bakker, P.; Huth, C.; Schöndube, F.; Wolfhard, U.; Böcker, D.; et al. Long-Term Clinical Effect of Hemodynamically Optimized Cardiac Resynchronization Therapy in Patients with Heart Failure and Ventricular Conduction Delay. J. Am. Coll. Cardiol. 2002, 39, 2026–2033. [Google Scholar] [CrossRef]
- Bristow, M.R.; Feldman, A.M.; Saxon, L.A. Heart Failure Management Using Implantable Devices for Ventricular Resynchronization: Comparison of Medical Therapy, Pacing, and Defibrillation in Chronic Heart Failure (COMPANION) Trial. J. Card. Fail. 2000, 6, 276–285. [Google Scholar] [CrossRef]
- Cazeau, S.; Leclercq, C.; Lavergne, T.; Walker, S.; Varma, C.; Linde, C.; Garrigue, S.; Kappenberger, L.; Haywood, G.A.; Santini, M.; et al. Effects of Multisite Biventricular Pacing in Patients with Heart Failure and Intraventricular Conduction Delay. N. Engl. J. Med. 2001, 344, 873–880. [Google Scholar] [CrossRef]
- Hare, J.M. Cardiac-Resynchronization Therapy for Heart Failure. N. Engl. J. Med. 2002, 346, 1902–1905. [Google Scholar] [CrossRef]
- Asher, J.; Houston, M. Statins and C-Reactive Protein Levels. J. Clin. Hypertens. 2007, 9, 622–628. [Google Scholar] [CrossRef] [PubMed]
- Mingo-Santos, S.; Moñivas-Palomero, V.; Garcia-Lunar, I.; Mitroi, C.D.; Goirigolzarri-Artaza, J.; Rivero, B.; Oteo, J.F.; Castedo, E.; González-Mirelis, J.; Cavero, M.A.; et al. Usefulness of Two-Dimensional Strain Parameters to Diagnose Acute Rejection After Heart Transplantation. J. Am. Soc. Echocardiogr. 2015, 28, 1149–1156. [Google Scholar] [CrossRef] [PubMed]
- da Costa, R.C.P.L.; Rodrigues, A.C.T.; Vieira, M.L.C.; Fischer, C.H.; Monaco, C.G.; Filho, E.B.L.; Bacal, F.; Caixeta, A.; Morhy, S.S. Evaluation of the Myocardial Deformation in the Diagnosis of Rejection After Heart Transplantation. Front. Cardiovasc. Med. 2022, 9, 991016. [Google Scholar] [CrossRef] [PubMed]
- Resende, M.V.C.; Vieira, M.L.C.; Bacal, F.; Andrade, J.L.; Stolf, N.A.; Bocchi, E.A. Tissue Doppler Echocardiography in the Diagnosis of Heart Transplantation Rejection. Arq. Bras. Cardiol. 2011, 97, 8–16. [Google Scholar] [CrossRef]
- Miller, C.A.; Naish, J.H.; Shaw, S.M.; Yonan, N.; Williams, S.G.; Clark, D.; Bishop, P.W.; Ainslie, M.P.; Borg, A.; Coutts, G.; et al. Multiparametric Cardiovascular Magnetic Resonance Surveillance of Acute Cardiac Allograft Rejection and Characterisation of Transplantation-Associated Myocardial Injury: A Pilot Study. J. Cardiovasc. Magn. Reson. 2014, 16, 52. [Google Scholar] [CrossRef]
- Pazdernik, M.; Wichterle, D.; Chet, Z.; Bedanova, H.; Kautzner, J.; Melenovsky, V.; Karmazin, V.; Malek, I.; Stiavnicky, P.; Tomasek, A.; et al. Heart Rate and Early Progression of Cardiac Allograft Vasculopathy: A Prospective Study Using Highly Automated 3-D Optical Coherence Tomography Analysis. Clin. Transplant. 2020, 34, e13773. [Google Scholar] [CrossRef]
- Foroutan, F.; Alba, A.C.; Guyatt, G.; Duero Posada, J.; Ng Fat Hing, N.; Arseneau, E.; Meade, M.; Hanna, S.; Badiwala, M.; Ross, H. Predictors of 1-Year Mortality in Heart Transplant Recipients: A Systematic Review and Meta-Analysis. Heart 2018, 104, 151–160. [Google Scholar] [CrossRef]
- Wever-Pinzon, O.; Edwards, L.B.; Taylor, D.O.; Kfoury, A.G.; Drakos, S.G.; Selzman, C.H.; Fang, J.C.; Lund, L.H.; Stehlik, J. Association of Recipient Age and Causes of Heart Transplant Mortality: Implications for Personalization of Post-Transplant Management—An Analysis of the International Society for Heart and Lung Transplantation Registry. J. Heart Lung Transplant. 2017, 36, 407–417. [Google Scholar] [CrossRef]
- Kavarana, M.N.; Savage, A.; O’Connell, R.; Rubinstein, C.S.; Flynn-Reeves, J.; Joshi, K.; Stroud, M.R.; Ikonomidis, J.S.; Bradley, S.M. Composite Risk Factors Predict Survival After Transplantation for Congenital Heart Disease. J. Thorac. Cardiovasc. Surg. 2013, 146, 888–893. [Google Scholar] [CrossRef]
- Huma, L.; Suciu, H.; Avram, C.; Suteu, R.-A.; Danilesco, A.; Baba, D.-F.; Moldovan, D.-A.; Sin, A.-I. Tricuspid Annular Plane Systolic Excursion-to-Systolic Pulmonary Artery Pressure Ratio as a Prognostic Factor in Heart Transplant Patients. Medicina 2024, 60, 1078. [Google Scholar] [CrossRef]
- Varga, A.; Moldovan, D.A.; Pop, M.; Benedek, I.; Kövecsi, A.; Dumbrava, R.A.; Iancu, D.G.; Cristescu, L.; Huma, L.; Tilea, I. FIP1L1–PDGFRα-Positive Loeffler Endocarditis—A Distinct Cause of Heart Failure in a Young Male: The Role of Multimodal Diagnostic Tools. Diagnostics 2023, 13, 1795. [Google Scholar] [CrossRef] [PubMed]
- Cater, R.; Taylor, J. The Experiences of Heart Transplant Recipients’ Spouses During the Pretransplant Waiting Period: Integrative Review. J. Clin. Nurs. 2017, 26, 2865–2877. [Google Scholar] [CrossRef]
- Burker, E.J.; Evon, D.M.; Ascari, J.C.; Loiselle, M.M.; Finkel, J.B.; Mill, M.R. Relationship Between Coping and Depression in Heart Transplant Candidates and Their Spouses. Prog. Transplant. 2006, 16, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Hackshaw, A. Small Studies: Strengths and Limitations. Eur. Respir. J. 2008, 32, 1141–1143. [Google Scholar] [CrossRef] [PubMed]
- Holman, A.; Karner-Huţuleac, A.; Ioan, B. Factors of the Willingness to Consent to the Donation of a Deceased Family Member’s Organs Among the Romanian Urban Population. Transplant. Proc. 2013, 45, 3178–3182. [Google Scholar] [CrossRef]
- Blaum, C.; Brunner, F.J.; Kröger, F.; Braetz, J.; Lorenz, T.; Goßling, A.; Ojeda, F.; Koester, L.; Karakas, M.; Zeller, T.; et al. Modifiable Lifestyle Risk Factors and C-Reactive Protein in Patients with Coronary Artery Disease: Implications for an Anti-Inflammatory Treatment Target Population. Eur. J. Prev. Cardiol. 2021, 28, 152–158. [Google Scholar] [CrossRef]

| Parameter | Result |
|---|---|
| Gender, males (n, %) | 37 (86.04) |
| Age, years (Mean, SD) | 44.46 (10.45) |
| Weight, kg (Mean, SD) | 76.00 (15.79) |
| BSA, sqm (Mean, SD) | 1.91 (0.23) |
| BMI, kg/sqm (Mean, SD) | 24.55 (4.07) |
| Etiology of cardiomyopathy, non-ischemic (n, %) | 32 (74.41) |
| CRT before the transplant, yes (n, %) | 9 (20.93) |
| Total hospital stay, days (Mean, SD) | 59.48 (66.58) |
| ICU stay, days (Mean, SD) | 51.39 (63.07) |
| Time under i.v. inotropes/vasopressors, days (Mean, SD) | 8.74 (13.20) |
| Parameter | r (95% CI) | p Value |
|---|---|---|
| Males | 0.03 (−0.27–0.34) | 0.81 * |
| Age | 0.04 (−0.27–0.34) | 0.78 * |
| Weight | 0.12 (−0.18–0.41) | 0.40 * |
| BSA | 0.16 (−0.15–0.45) | 0.29 * |
| BMI | 0.12 (−0.19–0.41) | 0.41 * |
| Nonischemic cardiomyopathy | −0.01 (−0.32–0.29) | 0.92 * |
| CRT | −0.37 (−0.61–−0.07) | 0.01 * |
| Hospital stay | <0.01 (−0.31–0.30) | 0.99 * |
| ICU stay | 0.09 (−0.22–0.39) | 0.54 * |
| Time under i.v. inotropes or vasopressors | −0.03 (−0.33–0.28) | 0.84 * |
| 6-month mortality | 0.35 (0.05–0.60) | 0.02 * |
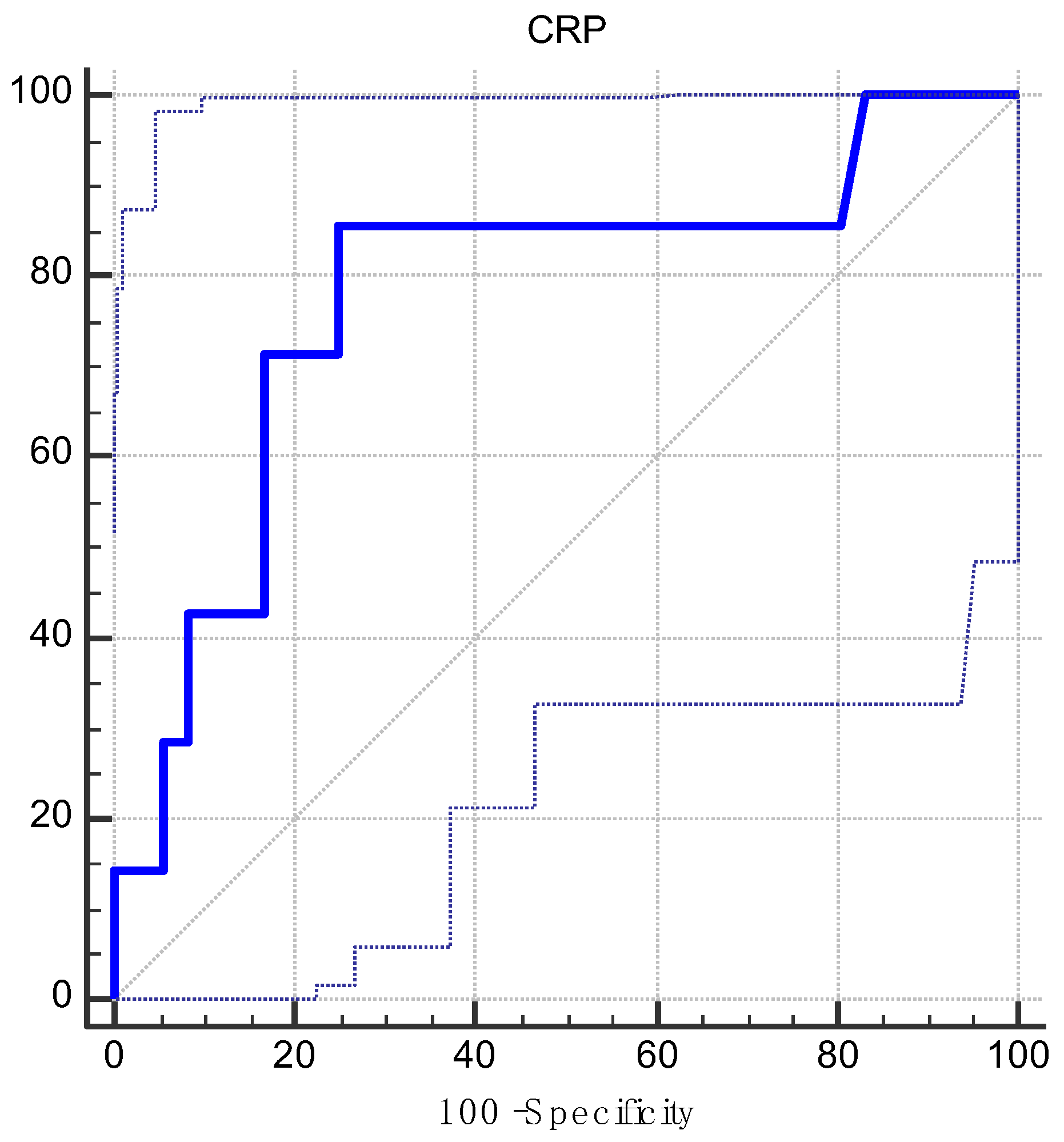
| AUC | 0.78 |
| 95% CI | 0.62–0.89 |
| z statistic | 2.50 |
| p value | 0.01 |
| Youden index | 0.60 |
| Associated criterion | >1.66 |
| Sensitivity | 85.71 |
| Specificity | 75.00 |
| Parameter | Group 1 | Group 2 | p Value |
|---|---|---|---|
| 6-month mortality (n, %) | 1 (3.57) | 6 (40.00) | <0.01 Ψ |
| Gender, male (n, %) | 23 (82.14) | 14 (93.33) | 0.40 Ψ |
| Age, years, Mean (SD)/Median | 43.32 (11.08)/43.50 | 46.60 (9.13)/46.00 | 0.33 * |
| Weight, kg, Mean (SD)/Median | 74.64 (17.41)/73.50 | 78.53 (12.36)/78.00 | 0.44 * |
| BSA, sqm, Mean (SD)/Median | 1.89 (0.25)/1.88 | 1.96 (0.17)/1.99 | 0.36 * |
| BMI, kg/sqm, Mean (SD)/Median | 24.26 (4.39)/24.10 | 25.08 (3.47)/24.60 | 0.63 ** |
| Etiology of cardiomyopathy, nonischemic (n, %) | 21 (75.00) | 11 (73.33) | 1.00 Φ |
| CRT before transplantation, yes (n, %) | 9 (32.14) | 0 (0.00) | 0.06 Ψ |
| Hospital stay, days, Mean (SD)/Median | 50.53(30.99)/40.00 | 79.57(107.93)/36.50 | 0.86 ** |
| ICU stay, days, Mean (SD)/Median | 40.75 (23.95)/33.50 | 71.26 (100.88)/34.00 | 0.49 ** |
| Time under i.v. inotropes/vasopressors, days, Mean (SD)/Median | 5.60 (3.97)/4.00 | 14.60 (20.88)/5.00 | 0.89 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huma, L.; Suciu, H.; Avram, C.; Suteu, R.-A.; Danilesco, A.; Baba, D.-F.; Moldovan, D.-A.; Sin, A.-I. Implications of Preoperative C-Reactive Protein Levels in Heart Transplant Patients—A Single-Center Retrospective Study. J. Clin. Med. 2024, 13, 7466. https://doi.org/10.3390/jcm13237466
Huma L, Suciu H, Avram C, Suteu R-A, Danilesco A, Baba D-F, Moldovan D-A, Sin A-I. Implications of Preoperative C-Reactive Protein Levels in Heart Transplant Patients—A Single-Center Retrospective Study. Journal of Clinical Medicine. 2024; 13(23):7466. https://doi.org/10.3390/jcm13237466
Chicago/Turabian StyleHuma, Laurentiu, Horatiu Suciu, Calin Avram, Radu-Adrian Suteu, Alina Danilesco, Dragos-Florin Baba, Diana-Andreea Moldovan, and Anca-Ileana Sin. 2024. "Implications of Preoperative C-Reactive Protein Levels in Heart Transplant Patients—A Single-Center Retrospective Study" Journal of Clinical Medicine 13, no. 23: 7466. https://doi.org/10.3390/jcm13237466
APA StyleHuma, L., Suciu, H., Avram, C., Suteu, R.-A., Danilesco, A., Baba, D.-F., Moldovan, D.-A., & Sin, A.-I. (2024). Implications of Preoperative C-Reactive Protein Levels in Heart Transplant Patients—A Single-Center Retrospective Study. Journal of Clinical Medicine, 13(23), 7466. https://doi.org/10.3390/jcm13237466






