Associated Medial Meniscal Injury with ACL Reconstruction Results in Poorer Strength and Jump Tests Outcomes: A 6-Month Analysis of 504 Patients from the MERIScience Cohort
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
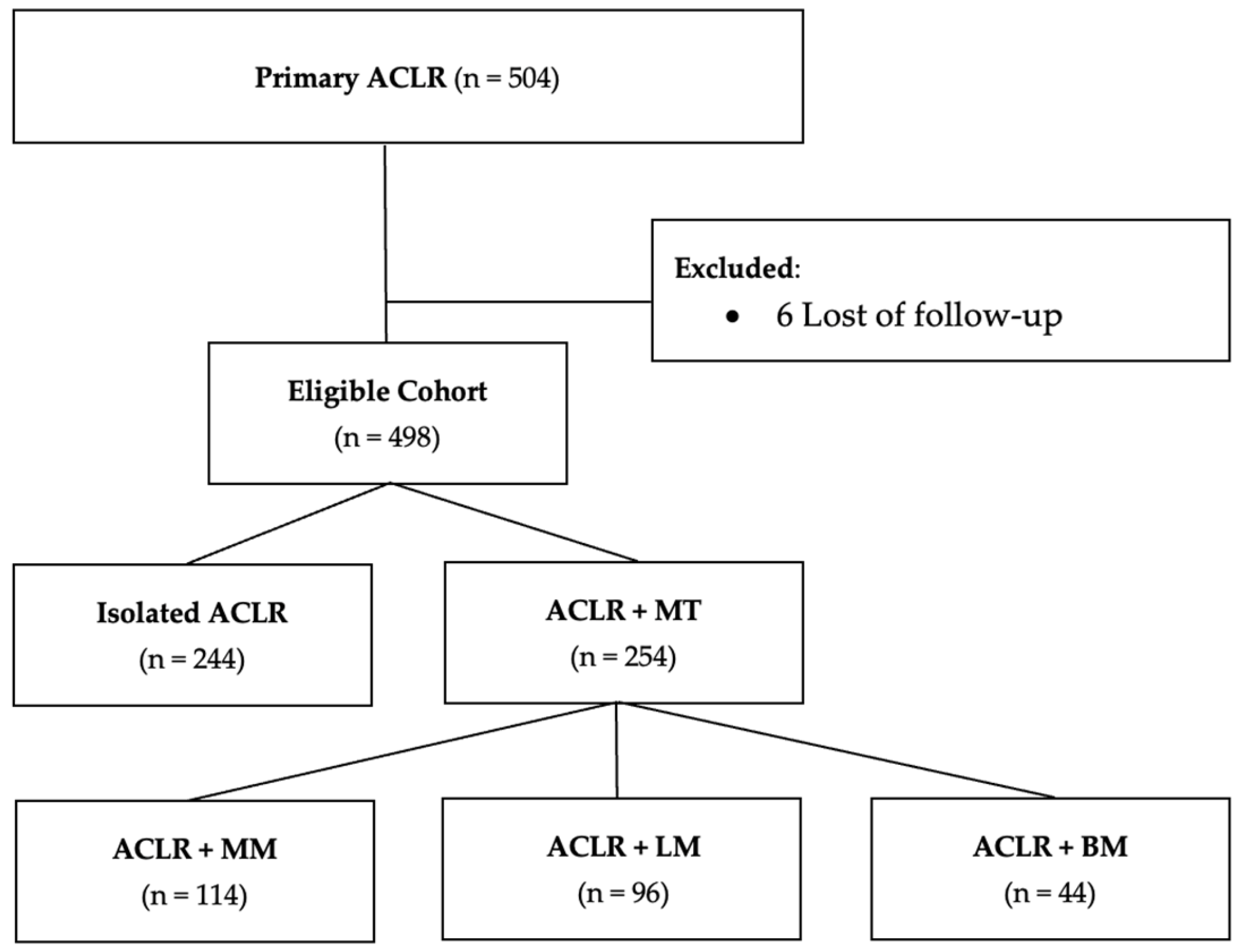
2.2. Study Population
2.3. Surgical Technique
2.4. Outcome Assessment
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Effects of Meniscal Injuries on Isokinetic Tests (Table 2)
- -
- A significant quadricipital deficit at a velocity of 240°/s (14% ± 14% vs. 18% ± 18%, p = 0.02),
- -
- A hamstring (H) deficit at a velocity of 30°/s (18% ± 18% vs. 14% ± 18%, p = 0.02),
- -
- And an imbalance in the hamstring/quadricipital (H/Q) ratio (68% ± 27% vs. 80% ± 67% p = 0.02).
| Variable | Isolated ACLR (n = 244) | ACLR + MM (n = 114) | p Value | ACLR + LM (n = 96) | p Value | ACLR + BM (n = 44) | p Value |
|---|---|---|---|---|---|---|---|
| Quadriceps | |||||||
| Deficit 60°/s (%) | 21 ± 16 | 22 ± 18 | 0.53 | 21 ± 16 | 0.16 | 20 ± 18 | 0.60 |
| Deficit 240°/s (%) | 14 ± 14 | 18 ± 18 | 0.02 | 14 ± 14 | 0.98 | 18 ± 17 | 0.09 |
| Hamstrings | |||||||
| Deficit 30°/s (%) | 14 ± 18 | 18 ± 18 | 0.02 | 14 ± 17 | 0.54 | 15 ± 17 | 0.40 |
| Deficit 60°/s (%) | 12 ± 14 | 14 ± 15 | 0.13 | 13 ± 16 | 0.39 | 11 ± 17 | 0.90 |
| Deficit 240°/s (%) | 08 ± 17 | 10 ± 17 | 0.15 | 16 ± 16 | 0.16 | 11 ± 17 | 0.02 |
| Non-injured H/Q 60°/s ratio (%) | 58 ± 42 | 57 ± 12 | 0.63 | 67 ± 97 | 0.26 | 59 ± 11 | 0.95 |
| Operated H/Q 60°/s ratio (%) | 64 ± 17 | 68 ± 29 | 0.20 | 63 ± 21 | 0.52 | 68 ± 20 | 0.20 |
| Non-injured H/Q 240°/s ratio (%) | 64 ± 21 | 67 ± 24 | 0.11 | 63 ± 23 | 0.83 | 71 ± 24 | 0.04 |
| Operated H/Q 240°/s Ratio (%) | 68 ± 27 | 80 ± 67 | 0.02 | 65 ± 27 | 0.37 | 78 ± 32 | 0.03 |
3.3. Effect of Meniscal Injuries on One-Foot Tests (Table 3)
| Variable | Isolated ACLR (n = 244) | ACLR + MM (n = 114) | p Value | ACLR + LM (n = 96) | p Value | ACLR + BM (n = 44) | p Value |
|---|---|---|---|---|---|---|---|
| Single hop for distance (SHD) | |||||||
| Non-injured knee (cm) | 125 ± 53.9 | 117 ± 60 | 0.23 | 123 ± 58 | 0.73 | 92 ± 53.1 | <0.001 |
| Operated knee (cm) | 111 ± 53.5 | 103 ± 57 | 0.22 | 109 ± 55 | 0.80 | 79 ± 49.5 | <0.001 |
| Deficit (%) | 12 ± 14 | 12 ± 15 | 0.75 | 11 ± 55 | 0.57 | 14 ± 15 | 0.30 |
| Triple hop for distance (THD) | |||||||
| Non-injured knee (cm) | 366 ± 160.9 | 339.1 ± 174 | 0.18 | 359 ± 170 | 0.73 | 272 ± 160.1 | <0.001 |
| Operated knee (cm) | 335 ± 160.2 | 305.4 ± 165 | 0.13 | 315 ± 171 | 0.34 | 245 ± 155.4 | <0.001 |
| Deficit (%) | 09 ± 13 | 10 ± 11 | 0.33 | 10 ±14 | 0.29 | 10 ± 14 | 0.3 |
| Side-hop test (Side-HT) | |||||||
| Non-injured knee (n) | 49 ± 14 | 46 ± 14 | 0.14 | 49 ± 13 | 0.74 | 46 ± 15 | 0.30 |
| Operated knee (n) | 42 ± 17 | 38 ± 17 | 0.06 | 43 ± 15 | 0.57 | 39 ± 17 | 0.40 |
| Deficit (%) | 16 ± 20 | 20 ± 23 | 0.15 | 13 ± 19 | 0.29 | 15.5 ± 41 | 0.88 |
| Single-leg landing (SLL) | |||||||
| Non-injured knee (%) | 20 ± 40 | 30 ± 46 | 0.035 | 34 ± 48 | 0.005 | 21 ± 41 | 0.82 |
| Operated knee (%) | 31 ± 46 | 39 ± 49 | 0.11 | 39 ± 49 | 0.36 | 24 ± 43 | 0.38 |
| Single-leg squat (SLS) | |||||||
| Non-injured knee (%) | 27 ± 44 | 37 ± 48 | 0.06 | 45 ± 50 | 0.001 | 19.0 ± 40 | 0.29 |
| Operated knee (%) | 40 ± 49 | 51 ± 50 | 0.05 | 54 ± 50 | 0.02 | 45 ± 50 | 0.49 |
3.4. Effect of Meniscal Injuries on the Non-Injured Limb (Table 2 and Table 3)
3.5. Effects of Meniscal Injuries on ACL-RSI (Table 4 and Table 5)
| Variable | Isolated ACLR (n = 244) | ACLR + MM (n = 114) | p Value | ACLR + LM (n = 96) | p Value | ACLR + BM (n = 44) | p Value |
|---|---|---|---|---|---|---|---|
| 6 months ALC-RSI (%) | 64.5 ± 19.0 | 63.0 ± 20.0 | 0.51 | 66.5 ± 19.7 | 0.75 | 66.7 ± 17.8 | 0.48 |
| MM (n = 114) | LM (n = 96) | |||||
|---|---|---|---|---|---|---|
| Variable | Repair (n = 75) | Meniscectomy (n = 39) | p Value | Repair (n = 62) | Meniscectomy (n = 34) | p Value |
| 6 months ACL-RSI (%) | 64.5 ± 18.8 | 60.2 ± 22.2 | 0.27 | 65.2 ± 19.5 | 69.0 ± 20.0 | 0.37 |
3.6. Effects of Meniscal Treatment (Table 6 and Table 7)
| ACLR + MM (n = 114) | ACLR + LM (n = 96) | |||||
|---|---|---|---|---|---|---|
| Variable | Repair (n = 75) | Meniscectomy (n = 39) | p Value | Repair (n = 62) | Meniscectomy (n = 34) | p Value |
| Quadriceps | ||||||
| Deficit 60°/s (%) | 22 ± 19 | 24 ± 16 | 0.55 | 19 ± 19 | 17 ± 18 | 0.56 |
| Deficit 240°/s (%) | 17 ± 18 | 20 ±18 | 0.44 | 12 ± 15 | 14 ± 13 | 0.44 |
| Hamstrings | ||||||
| Deficit 30°/s (%) | 19 ± 17 | 18 ± 19 | 0.84 | 17 ± 18 | 14 ± 17 | 0.84 |
| Deficit 60°/s (%) | 14 ± 15 | 14 ± 15 | 0.98 | 12 ± 17 | 15 ± 14 | 0.53 |
| Deficit 240°/s (%) | 10 ± 17 | 10 ± 18 | 0.94 | 9 ± 16 | 13 ± 16 | 0.94 |
| Non-injured H/Q 60°/s ratio (%) | 56 ± 12 | 59 ± 10 | 0.17 | 72 ± 22 | 59 ± 11 | 0.17 |
| Operated H/Q 60°/s ratio (%) | 67 ± 32 | 68 ± 20 | 0.88 | 63 ± 22 | 63 ± 18 | 0.88 |
| Non-injured H/Q 240°/s ratio (%) | 65 ± 23 | 70 ± 25 | 0.93 | 62 ± 22 | 65 ± 26 | 0.25 |
| Operated H/Q 240°/s ratio (%) | 80 ± 79 | 79 ± 34 | 0.93 | 63 ± 26 | 69 ± 29 | 0.94 |
| ACLR + MM (n = 114) | ACLR + LM (n = 96) | |||||
|---|---|---|---|---|---|---|
| Variable | Repair (n = 75) | Meniscectomy (n = 39) | p Value | Repair (n = 62) | Meniscectomy (n = 34) | p Value |
| Single Hop for Distance (SHD) | ||||||
| Healthy knee (cm) | 118 ± 53 | 118 ± 64 | 0.79 | 116 ± 57 | 134 ± 58 | 0.79 |
| Operated knee (cm) | 105 ± 57 | 98 ± 59 | 0.54 | 104 ± 58 | 119 ± 50 | 0.54 |
| Deficit (%) | 12 ± 15 | 13 ± 14 | 0.83 | 10 ± 13 | 13 ± 11 | 0.83 |
| Triple Hop for distance (THD) | ||||||
| Healthy knee (cm) | 344 ± 171 | 327 ± 182 | 0.66 | 342 ± 168 | 390 ± 172 | 0.65 |
| Operated knee (cm) | 312 ± 162 | 290 ± 173 | 0.54 | 304 ± 174 | 336 ± 167 | 0.54 |
| Deficit (%) | 10 ± 11 | 10 ± 11 | 0.93 | 11 ± 15 | 10 ± 11 | 0.92 |
| Side-hop test (Side-HT) | ||||||
| Healthy knee (n) | 47.1 ± 13.2 | 44.0 ± 16.0 | 0.33 | 46.9 ± 15.1 | 53.4 ±12 | 0.33 |
| Operated knee (n) | 39.4 ± 17.1 | 34.8 ± 17.9 | 0.24 | 41.3 ± 15.4 | 46.9 ± 15.1 | 0.24 |
| Deficit (%) | 19.4 ± 21.5 | 21.1 ± 25.8 | 0.73 | 13.2 ± 20 | 13.8 ± 17.9 | 0.73 |
| Single-Leg Landing (SLL) | ||||||
| Healthy knee (cm) | 25 ± 43 | 42 ± 50 | 0.07 | 35 ± 48 | 33 ± 48 | 0.07 |
| Operated knee (cm) | 33 ± 47 | 51 ± 50 | 0.06 | 42 ± 50 | 33 ± 48 | 0.06 |
| Deficit (%) | ||||||
| Single-Leg Squat (SLS) | ||||||
| Healthy knee (%) | 33 ± 47 | 43 ± 50 | 0.31 | 45 ± 50 | 44 ± 50 | 0.31 |
| Operated knee (%) | 48 ± 50 | 57 ± 50 | 0.39 | 55 ± 50 | 53 ± 50 | 0.39 |
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hagino, T.; Ochiai, S.; Senga, S.; Yamashita, T.; Wako, M.; Ando, T.; Haro, H. Meniscal Tears Associated with Anterior Cruciate Ligament Injury. Arch. Orthop. Trauma. Surg. 2015, 135, 1701–1706. [Google Scholar] [CrossRef] [PubMed]
- Cinque, M.E.; Chahla, J.; Mitchell, J.J.; Moatshe, G.; Pogorzelski, J.; Murphy, C.P.; Kennedy, N.I.; Godin, J.A.; LaPrade, R.F. Influence of Meniscal and Chondral Lesions on Patient-Reported Outcomes After Primary Anterior Cruciate Ligament Reconstruction at 2-Year Follow-Up. Orthop. J. Sports Med. 2018, 6, 2325967117754189. [Google Scholar] [CrossRef] [PubMed]
- Gornitzky, A.L.; Lott, A.; Yellin, J.L.; Fabricant, P.D.; Lawrence, J.T.; Ganley, T.J. Sport-Specific Yearly Risk and Incidence of Anterior Cruciate Ligament Tears in High School Athletes: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2016, 44, 2716–2723. [Google Scholar] [CrossRef] [PubMed]
- Erivan, R.; Tardieu, A.; Villatte, G.; Ollivier, M.; Jacquet, C.; Descamps, S.; Boisgard, S. Knee Surgery Trends and Projections in France from 2008 to 2070. Orthop. Traumatol. Surg. Res. 2020, 106, 893–902. [Google Scholar] [CrossRef]
- Ardern, C.L.; Taylor, N.F.; Feller, J.A.; Webster, K.E. Fifty-Five per Cent Return to Competitive Sport Following Anterior Cruciate Ligament Reconstruction Surgery: An Updated Systematic Review and Meta-Analysis Including Aspects of Physical Functioning and Contextual Factors. Br. J. Sports Med. 2014, 48, 1543–1552. [Google Scholar] [CrossRef]
- Mohan, R.; Webster, K.E.; Johnson, N.R.; Stuart, M.J.; Hewett, T.E.; Krych, A.J. Clinical Outcomes in Revision Anterior Cruciate Ligament Reconstruction: A Meta-Analysis. Arthroscopy 2018, 34, 289–300. [Google Scholar] [CrossRef]
- Gifstad, T.; Foss, O.A.; Engebretsen, L.; Lind, M.; Forssblad, M.; Albrektsen, G.; Drogset, J.O. Lower Risk of Revision with Patellar Tendon Autografts Compared with Hamstring Autografts: A Registry Study Based on 45,998 Primary ACL Reconstructions in Scandinavia. Am. J. Sports Med. 2014, 42, 2319–2328. [Google Scholar] [CrossRef]
- Barber-Westin, S.D.; Noyes, F.R. Factors Used to Determine Return to Unrestricted Sports Activities after Anterior Cruciate Ligament Reconstruction. Arthroscopy 2011, 27, 1697–1705. [Google Scholar] [CrossRef]
- Al-Gburi, M.; Kristiansen, J.B.; Christensen, K.B.; Krogsgaard, M.R. Functional Performance Tests, Clinical Measurements, and Patient-Reported Outcome Measures Do Not Correlate as Outcomes 1 Year after Anterior Cruciate Ligament Reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5905–5912. [Google Scholar] [CrossRef]
- Meredith, S.J.; Rauer, T.; Chmielewski, T.L.; Fink, C.; Diermeier, T.; Rothrauff, B.B.; Svantesson, E.; Hamrin Senorski, E.; Hewett, T.E.; Sherman, S.L.; et al. Return to Sport after Anterior Cruciate Ligament Injury: Panther Symposium ACL Injury Return to Sport Consensus Group. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 2403–2414. [Google Scholar] [CrossRef]
- Blakeney, W.G.; Ouanezar, H.; Rogowski, I.; Vigne, G.; Guen, M.L.; Fayard, J.-M.; Thaunat, M.; Chambat, P.; Sonnery-Cottet, B. Validation of a Composite Test for Assessment of Readiness for Return to Sports After Anterior Cruciate Ligament Reconstruction: The K-STARTS Test. Sports Health 2018, 10, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Gokeler, A.; Welling, W.; Zaffagnini, S.; Seil, R.; Padua, D. Development of a Test Battery to Enhance Safe Return to Sports after Anterior Cruciate Ligament Reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Grassi, A.; Vascellari, A.; Combi, A.; Tomaello, L.; Canata, G.L.; Zaffagnini, S.; SIGASCOT Sports Committee. Return to Sport after ACL Reconstruction: A Survey between the Italian Society of Knee, Arthroscopy, Sport, Cartilage and Orthopaedic Technologies (SIGASCOT) Members. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Øiestad, B.E.; Engebretsen, L.; Storheim, K.; Risberg, M.A. Knee Osteoarthritis after Anterior Cruciate Ligament Injury: A Systematic Review. Am. J. Sports Med. 2009, 37, 1434–1443. [Google Scholar] [CrossRef]
- Beaufils, P.; Pujol, N. Management of Traumatic Meniscal Tear and Degenerative Meniscal Lesions. Save the Meniscus. Orthop. Traumatol. Surg. Res. 2017, 103, S237–S244. [Google Scholar] [CrossRef]
- Cox, C.L.; Huston, L.J.; Dunn, W.R.; Reinke, E.K.; Nwosu, S.K.; Parker, R.D.; Wright, R.W.; Kaeding, C.C.; Marx, R.G.; Amendola, A.; et al. Are Articular Cartilage Lesions and Meniscus Tears Predictive of IKDC, KOOS, and Marx Activity Level Outcomes after Anterior Cruciate Ligament Reconstruction? A 6-Year Multicenter Cohort Study. Am. J. Sports Med. 2014, 42, 1058–1067. [Google Scholar] [CrossRef]
- Pedersen, M.; Johnson, J.L.; Grindem, H.; Magnusson, K.; Snyder-Mackler, L.; Risberg, M.A. Meniscus or Cartilage Injury at the Time of Anterior Cruciate Ligament Tear Is Associated With Worse Prognosis for Patient-Reported Outcome 2 to 10 Years After Anterior Cruciate Ligament Injury: A Systematic Review. J. Orthop. Sports Phys. Ther. 2020, 50, 490–502. [Google Scholar] [CrossRef]
- Sarraj, M.; Coughlin, R.P.; Solow, M.; Ekhtiari, S.; Simunovic, N.; Krych, A.J.; MacDonald, P.; Ayeni, O.R. Anterior Cruciate Ligament Reconstruction with Concomitant Meniscal Surgery: A Systematic Review and Meta-Analysis of Outcomes. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3441–3452. [Google Scholar] [CrossRef]
- Casp, A.J.; Bodkin, S.G.; Gwathmey, F.W.; Werner, B.C.; Miller, M.D.; Diduch, D.R.; Brockmeier, S.F.; Hart, J.M. Effect of Meniscal Treatment on Functional Outcomes 6 Months After Anterior Cruciate Ligament Reconstruction. Orthop. J. Sports Med. 2021, 9, 23259671211031281. [Google Scholar] [CrossRef]
- Byrne, L.; King, E.; Mc Fadden, C.; Jackson, M.; Moran, R.; Daniels, K. The Effect of Meniscal Pathology and Management with ACL Reconstruction on Patient-Reported Outcomes, Strength, and Jump Performance Ten Months Post-Surgery. Knee 2021, 32, 72–79. [Google Scholar] [CrossRef]
- Redler, L.H.; Sugimoto, D.; Bassett, A.J.; Kocher, M.S.; Micheli, L.J.; Heyworth, B.E. Effect of Concomitant Meniscal Tear on Strength and Functional Performance in Young Athletes 6 Months After Anterior Cruciate Ligament Reconstruction With Hamstring Autograft. Orthop. J. Sports Med. 2021, 9, 23259671211046608. [Google Scholar] [CrossRef] [PubMed]
- Sonnery-Cottet, B.; Daggett, M.; Fayard, J.-M.; Ferretti, A.; Helito, C.P.; Lind, M.; Monaco, E.; de Pádua, V.B.C.; Thaunat, M.; Wilson, A.; et al. Anterolateral Ligament Expert Group Consensus Paper on the Management of Internal Rotation and Instability of the Anterior Cruciate Ligament—Deficient Knee. J. Orthop. Traumatol. 2017, 18, 91–106. [Google Scholar] [CrossRef] [PubMed]
- Wadhwa, V.; Omar, H.; Coyner, K.; Khazzam, M.; Robertson, W.; Chhabra, A. ISAKOS Classification of Meniscal Tears-Illustration on 2D and 3D Isotropic Spin Echo MR Imaging. Eur. J. Radiol. 2016, 85, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Colombet, P.; Graveleau, N. Minimally Invasive Anterior Semitendinosus Harvest: A Technique to Decrease Saphenous Nerve Injury. Arthrosc. Tech. 2016, 5, e139–e142. [Google Scholar] [CrossRef]
- Colombet, P.; Saffarini, M.; Bouguennec, N. Clinical and Functional Outcomes of Anterior Cruciate Ligament Reconstruction at a Minimum of 2 Years Using Adjustable Suspensory Fixation in Both the Femur and Tibia: A Prospective Study. Orthop. J. Sports Med. 2018, 6, 2325967118804128. [Google Scholar] [CrossRef]
- Boutsiadis, A.; Brossard, P.; Panisset, J.-C.; Graveleau, N.; Barth, J. Minimally Invasive Combined Anterior and Anterolateral Stabilization of the Knee Using Hamstring Tendons and Adjustable-Loop Suspensory Fixation Device: Surgical Technique. Arthrosc. Tech. 2017, 6, e419–e425. [Google Scholar] [CrossRef]
- Beaufils, P.; Hulet, C.; Dhénain, M.; Nizard, R.; Nourissat, G.; Pujol, N. Clinical Practice Guidelines for the Management of Meniscal Lesions and Isolated Lesions of the Anterior Cruciate Ligament of the Knee in Adults. Orthop. Traumatol. Surg. Res. 2009, 95, 437–442. [Google Scholar] [CrossRef]
- Gerritsen, L.M.; van der Lelij, T.J.N.; van Schie, P.; Fiocco, M.; van Arkel, E.R.A.; Zuurmond, R.G.; Keereweer, S.; van Driel, P.B.a.A. Higher Healing Rate after Meniscal Repair with Concomitant ACL Reconstruction for Tears Located in Vascular Zone 1 Compared to Zone 2: A Systematic Review and Meta-Analysis. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 1976–1989. [Google Scholar] [CrossRef]
- Thaunat, M.; Fayard, J.M.; Guimaraes, T.M.; Jan, N.; Murphy, C.G.; Sonnery-Cottet, B. Classification and Surgical Repair of Ramp Lesions of the Medial Meniscus. Arthrosc. Tech. 2016, 5, e871–e875. [Google Scholar] [CrossRef]
- Sonnery-Cottet, B.; Praz, C.; Rosenstiel, N.; Blakeney, W.G.; Ouanezar, H.; Kandhari, V.; Vieira, T.D.; Saithna, A. Epidemiological Evaluation of Meniscal Ramp Lesions in 3214 Anterior Cruciate Ligament-Injured Knees From the SANTI Study Group Database: A Risk Factor Analysis and Study of Secondary Meniscectomy Rates Following 769 Ramp Repairs. Am. J. Sports Med. 2018, 46, 3189–3197. [Google Scholar] [CrossRef]
- Webster, K.E.; Feller, J.A.; Lambros, C. Development and Preliminary Validation of a Scale to Measure the Psychological Impact of Returning to Sport Following Anterior Cruciate Ligament Reconstruction Surgery. Phys. Ther. Sport 2008, 9, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Drouin, J.M.; Valovich-mcLeod, T.C.; Shultz, S.J.; Gansneder, B.M.; Perrin, D.H. Reliability and Validity of the Biodex System 3 pro Isokinetic Dynamometer Velocity, Torque and Position Measurements. Eur. J. Appl. Physiol. 2004, 91, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Almangoush, A.; Herrington, L.; Jones, R. Physical Therapy and Rehabilitation A Preliminary Reliability Study of a Qualitative Scoring System of Limb Alignment during Single Leg Squat. Phys. Ther. Rehabil. 2014, 1, 2. [Google Scholar] [CrossRef][Green Version]
- Munro, A.; Herrington, L.; Comfort, P. Comparison of Landing Knee Valgus Angle between Female Basketball and Football Athletes: Possible Implications for Anterior Cruciate Ligament and Patellofemoral Joint Injury Rates. Phys. Ther. Sport 2012, 13, 259–264. [Google Scholar] [CrossRef]
- Ekegren, C.L.; Miller, W.C.; Celebrini, R.G.; Eng, J.J.; MacIntyre, D.L. Reliability and Validity of Observational Risk Screening in Evaluating Dynamic Knee Valgus. J. Orthop. Sports Phys. Ther. 2009, 39, 665–674. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Chaory, K.; Poiraudeau, S. [Rating scores for ACL ligamentoplasty]. Ann. Readapt. Med. Phys. 2004, 47, 309–316. [Google Scholar] [CrossRef]
- Hughes, J.D.; Lawton, C.D.; Nawabi, D.H.; Pearle, A.D.; Musahl, V. Anterior Cruciate Ligament Repair: The Current Status. J. Bone Joint Surg. Am. 2020, 102, 1900–1915. [Google Scholar] [CrossRef]
- Bohu, Y.; Klouche, S.; Herman, S.; Gerometta, A.; Lefevre, N. Évaluation Des Facteurs Psychologiques Associés Au Retour Au Sport Habituel Après Ligamentoplastie Du LCA: Étude Prospective à 1 an de Recul Selon Le Score ACL-RSI. Rev. Chir. Orthop. Et Traumatol. 2014, 100, e23. [Google Scholar] [CrossRef]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S.; Colosimo, A.J.; McLean, S.G.; van den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical Measures of Neuromuscular Control and Valgus Loading of the Knee Predict Anterior Cruciate Ligament Injury Risk in Female Athletes: A Prospective Study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef]
- Desai, N.; Andernord, D.; Sundemo, D.; Alentorn-Geli, E.; Musahl, V.; Fu, F.; Forssblad, M.; Samuelsson, K. Revision Surgery in Anterior Cruciate Ligament Reconstruction: A Cohort Study of 17,682 Patients from the Swedish National Knee Ligament Register. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1542–1554. [Google Scholar] [CrossRef] [PubMed]
- Edwards, P.K.; Ebert, J.R.; Joss, B.; Ackland, T.; Annear, P.; Buelow, J.-U.; Hewitt, B. Patient Characteristics and Predictors of Return to Sport at 12 Months After Anterior Cruciate Ligament Reconstruction: The Importance of Patient Age and Postoperative Rehabilitation. Orthop. J. Sports Med. 2018, 6, 2325967118797575. [Google Scholar] [CrossRef] [PubMed]
- Nagai, T.; Schilaty, N.D.; Laskowski, E.R.; Hewett, T.E. Hop Tests Can Result in Higher Limb Symmetry Index Values than Isokinetic Strength and Leg Press Tests in Patients Following ACL Reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 816–822. [Google Scholar] [CrossRef] [PubMed]
- Gerfroit, A.; Marty-Diloy, T.; Laboudie, P.; Graveleau, N.; Bouguennec, N. Correlation between Anterior Cruciate Ligament–Return to Sport after Injury Score at 6 Months after Anterior Cruciate Ligament Reconstruction and Mid-Term Functional Test Results: An Observational Study at 5-Year Follow-Up. J. Clin. Med. 2024, 13, 4498. [Google Scholar] [CrossRef]
- Sadeqi, M.; Klouche, S.; Bohu, Y.; Herman, S.; Lefevre, N.; Gerometta, A. Progression of the Psychological ACL-RSI Score and Return to Sport After Anterior Cruciate Ligament Reconstruction: A Prospective 2-Year Follow-up Study From the French Prospective Anterior Cruciate Ligament Reconstruction Cohort Study (FAST). Orthop. J. Sports Med. 2018, 6, 2325967118812819. [Google Scholar] [CrossRef]
- Moretti, L.; Bortone, I.; Delmedico, M.; Cassano, D.G.; Caringella, N.; Bizzoca, D.; Moretti, B. Clinical, Biomechanical, and Self-Reported Health Status After ACL Reconstruction With Meniscal Repair in Soccer Players: Results at Minimum 1-Year Follow-Up. Orthop. J. Sports Med. 2023, 11, 23259671231177309. [Google Scholar] [CrossRef]
- Mesnard, G.; Fournier, G.; Joseph, L.; Shatrov, J.G.; Lustig, S.; Servien, E. Does Meniscal Repair Impact Muscle Strength Following ACL Reconstruction? SICOT J. 2022, 8, 16. [Google Scholar] [CrossRef]
- Wenning, M.; Heitner, A.H.; Mauch, M.; Gehring, D.; Ramsenthaler, C.; Paul, J. The Effect of Meniscal Repair on Strength Deficits 6 Months after ACL Reconstruction. Arch. Orthop. Trauma. Surg. 2020, 140, 751–760. [Google Scholar] [CrossRef]
- Claes, S.; Hermie, L.; Verdonk, R.; Bellemans, J.; Verdonk, P. Is Osteoarthritis an Inevitable Consequence of Anterior Cruciate Ligament Reconstruction? A Meta-Analysis. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1967–1976. [Google Scholar] [CrossRef]
- Franck, F.; Saithna, A.; Vieira, T.D.; Pioger, C.; Vigne, G.; Le Guen, M.; Rogowski, I.; Fayard, J.-M.; Thaunat, M.; Sonnery-Cottet, B. Return to Sport Composite Test After Anterior Cruciate Ligament Reconstruction (K-STARTS): Factors Affecting Return to Sport Test Score in a Retrospective Analysis of 676 Patients. Sports Health 2021, 13, 364–372. [Google Scholar] [CrossRef]
| Variable | Values |
|---|---|
| Age at surgery (years), mean ± SD | 27.6 ± 1.9 (14–58) |
| Sex, n (%) | |
| Male | 316 (63.5) |
| Female | 182 (36.5) |
| Knee right/left, n (%) | 267 (53.6)/231 (46.4) |
| Isolated ACLR, n (%) | 244 (49.0) |
| ACLR associated with MT, n (%) | 254 (51.0) |
| MM injury | 114 (44.9) |
| LM injury | 96 (37.8) |
| BM injury | 44 (17.3) |
| Meniscal treatment, n (%) | |
| MM repair | 75 (65.8) |
| MM meniscectomy | 39 (34.2) |
| LM repair | 62 (64.6) |
| MM meniscectomy | 34 (35.4) |
| Anterolateral Ligament Reconstruction, n (%) | 153 (30.7) |
| Pre-injury Tegner Activity Scale, mean ± SD | 7.1 ± 0.9 (2–9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cazemajou, C.; Marty-Diloy, T.; Graveleau, N.; Laboudie, P.; Bouguennec, N. Associated Medial Meniscal Injury with ACL Reconstruction Results in Poorer Strength and Jump Tests Outcomes: A 6-Month Analysis of 504 Patients from the MERIScience Cohort. J. Clin. Med. 2024, 13, 7251. https://doi.org/10.3390/jcm13237251
Cazemajou C, Marty-Diloy T, Graveleau N, Laboudie P, Bouguennec N. Associated Medial Meniscal Injury with ACL Reconstruction Results in Poorer Strength and Jump Tests Outcomes: A 6-Month Analysis of 504 Patients from the MERIScience Cohort. Journal of Clinical Medicine. 2024; 13(23):7251. https://doi.org/10.3390/jcm13237251
Chicago/Turabian StyleCazemajou, Clément, Thibault Marty-Diloy, Nicolas Graveleau, Pierre Laboudie, and Nicolas Bouguennec. 2024. "Associated Medial Meniscal Injury with ACL Reconstruction Results in Poorer Strength and Jump Tests Outcomes: A 6-Month Analysis of 504 Patients from the MERIScience Cohort" Journal of Clinical Medicine 13, no. 23: 7251. https://doi.org/10.3390/jcm13237251
APA StyleCazemajou, C., Marty-Diloy, T., Graveleau, N., Laboudie, P., & Bouguennec, N. (2024). Associated Medial Meniscal Injury with ACL Reconstruction Results in Poorer Strength and Jump Tests Outcomes: A 6-Month Analysis of 504 Patients from the MERIScience Cohort. Journal of Clinical Medicine, 13(23), 7251. https://doi.org/10.3390/jcm13237251





