Psychiatric Disorders in Patients with Chronic Obstructive Pulmonary Disease: Clinical Significance and Treatment Strategies
Abstract
1. Introduction
2. Overview of Common Psychiatric Disorders in COPD
Risk Factors for Psychiatric Disease in COPD
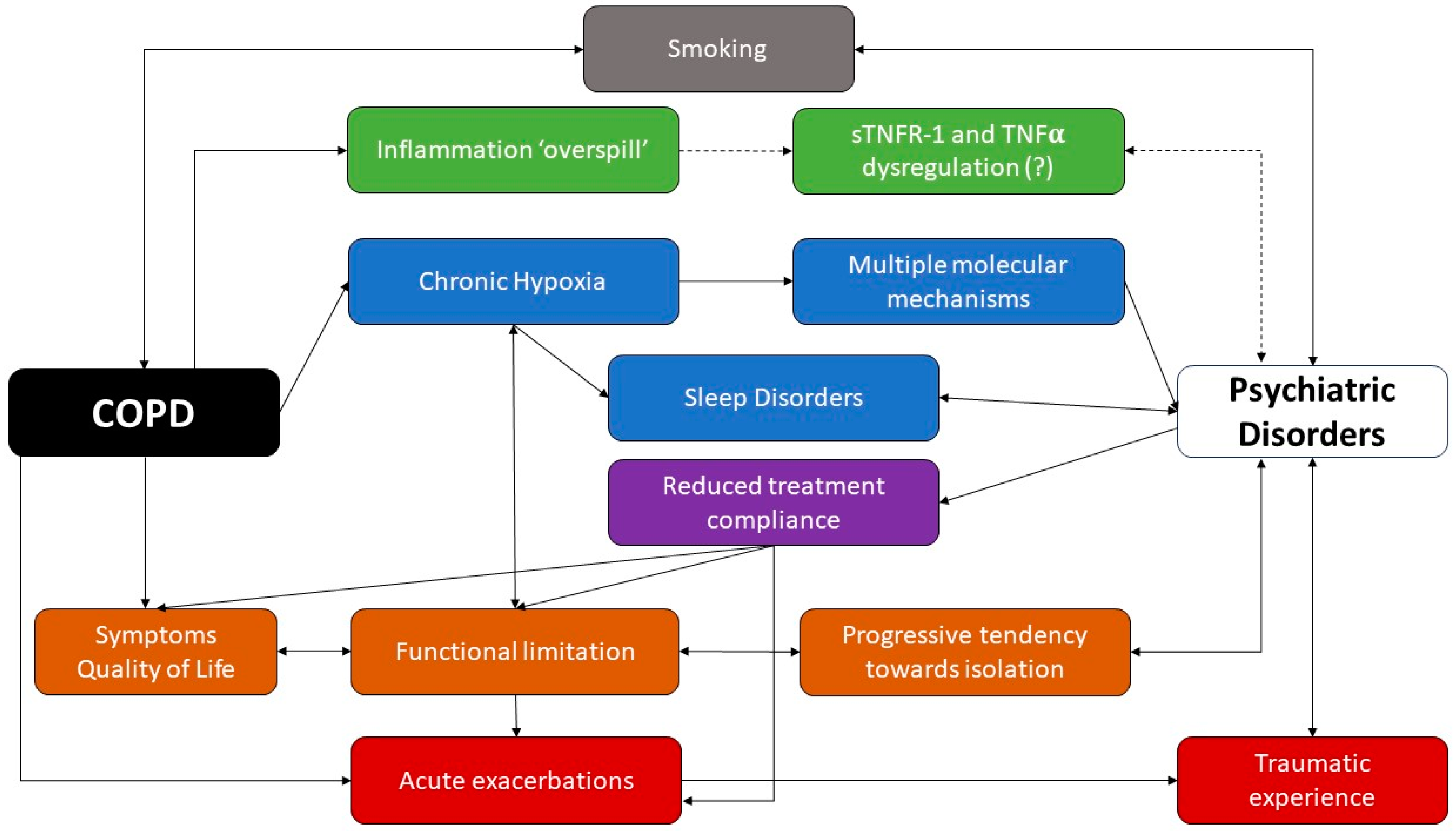
3. Bidirectional Relationship Between COPD and Psychiatric Disorders
3.1. Etiology and Pathophysiological Mechanisms Linking COPD and Psychiatric Disorders
3.2. Impact of Psychiatric Disorders on COPD Outcomes
4. Assessment and Diagnosis of Main Psychiatric Disorders in COPD
Multidisciplinary Teams: Role of Primary Care, Pulmonologists and Psychologists
5. Treatment Strategies for Psychiatric Disorders in COPD
6. Future Directions in Research and Clinical Practice
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Celli, B.; Fabbri, L.; Criner, G.; Martinez, F.J.; Mannino, D.; Vogelmeier, C.; Montes de Oca, M.; Papi, A.; Sin, D.D.; Han, M.K.; et al. Definition and Nomenclature of Chronic Obstructive Pulmonary Disease: Time for Its Revision. Am. J. Respir. Crit. Care Med. 2022, 206, 1317–1325. [Google Scholar] [CrossRef] [PubMed]
- Adeloye, D.; Chua, S.; Lee, C.; Basquill, C.; Papana, A.; Theodoratou, E.; Nair, H.; Gasevic, D.; Sridhar, D.; Campbell, H.; et al. Global and Regional Estimates of COPD Prevalence: Systematic Review and Meta–Analysis. J. Glob. Health 2015, 5, 020415. [Google Scholar] [CrossRef] [PubMed]
- López-Campos, J.L.; Tan, W.; Soriano, J.B. Global Burden of COPD. Respirology 2016, 21, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Iheanacho, I.; Zhang, S.; King, D.; Rizzo, M.; Ismaila, A.S. Economic Burden of Chronic Obstructive Pulmonary Disease (COPD): A Systematic Literature Review. Int. J. Chronic Obstr. Pulm. Dis. 2020, 15, 439–460. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The 10 Leading Causes of Death in the World, 2000 and 2012. 2015. Available online: http://www.who.int/mediacentre/factsheets/fs310/en/ (accessed on 26 August 2024).
- AL Wachami, N.; Guennouni, M.; Iderdar, Y.; Boumendil, K.; Arraji, M.; Mourajid, Y.; Bouchachi, F.Z.; Barkaoui, M.; Louerdi, M.L.; Hilali, A.; et al. Estimating the Global Prevalence of Chronic Obstructive Pulmonary Disease (COPD): A Systematic Review and Meta-Analysis. BMC Public Health 2024, 24, 297. [Google Scholar] [CrossRef]
- Su, W.-C.; Juan, H.-L.; Lee, J.-I.; Huang, S.-P.; Chen, S.-C.; Geng, J.-H. Secondhand Smoke Increases the Risk of Developing Chronic Obstructive Pulmonary Disease. Sci. Rep. 2024, 14, 7481. [Google Scholar] [CrossRef]
- Venkatesan, P. GOLD COPD Report: 2024 Update. Lancet Respir. Med. 2024, 12, 15–16. [Google Scholar] [CrossRef]
- dos Santos, N.C.; Miravitlles, M.; Camelier, A.A.; de Almeida, V.D.C.; Maciel, R.R.B.T.; Camelier, F.W.R. Prevalence and Impact of Comorbidities in Individuals with Chronic Obstructive Pulmonary Disease: A Systematic Review. Tuberc. Respir. Dis. 2022, 85, 205–220. [Google Scholar] [CrossRef]
- Blakemore, A.; Dickens, C.; Guthrie, E.; Bower, P.; Kontopantelis, E.; Afzal, C.; Coventry, P. Depression and Anxiety Predict Health-Related Quality of Life in Chronic Obstructive Pulmonary Disease: Systematic Review and Meta-Analysis. Int. J. Chronic Obstr. Pulm. Dis. 2014, 9, 501–512. [Google Scholar] [CrossRef]
- Martínez-Gestoso, S.; García-Sanz, M.-T.; Carreira, J.-M.; Salgado, F.-J.; Calvo-Álvarez, U.; Doval-Oubiña, L.; Camba-Matos, S.; Peleteiro-Pedraza, L.; González-Pérez, M.-A.; Penela-Penela, P.; et al. Impact of Anxiety and Depression on the Prognosis of Copd Exacerbations. BMC Pulm. Med. 2022, 22, 169. [Google Scholar] [CrossRef]
- Chaudhary, S.; Nanda, S.; Tripathi, A.; Sawlani, K.; Gupta, K.; Himanshu, D.; Verma, A. Prevalence of Psychiatric Comorbidities in Chronic Obstructive Pulmonary Disease Patients. Lung India 2016, 33, 174. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wu, X.; Lai, W.; Long, E.; Zhang, X.; Li, W.; Zhu, Y.; Chen, C.; Zhong, X.; Liu, Z.; et al. Prevalence of Depression and Depressive Symptoms among Outpatients: A Systematic Review and Meta-Analysis. BMJ Open 2017, 7, e017173. [Google Scholar] [CrossRef] [PubMed]
- Vestbo, J.; Hurd, S.S.; Agustí, A.G.; Jones, P.W.; Vogelmeier, C.; Anzueto, A.; Barnes, P.J.; Fabbri, L.M.; Martinez, F.J.; Nishimura, M.; et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2013, 187, 347–365. [Google Scholar] [CrossRef] [PubMed]
- Laurin, C.; Labrecque, M.; Dupuis, G.; Bacon, S.L.; Cartier, A.; Lavoie, K.L. Chronic Obstructive Pulmonary Disease Patients with Psychiatric Disorders Are at Greater Risk of Exacerbations. Psychosom. Med. 2009, 71, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Atlantis, E.; Fahey, P.; Cochrane, B.; Smith, S. Bidirectional Associations between Clinically Relevant Depression or Anxiety and COPD. Chest 2013, 144, 766–777. [Google Scholar] [CrossRef]
- Yohannes, A.M.; Kaplan, A.; Hanania, N.A. Anxiety and Depression in Chronic Obstructive Pulmonary Disease: Recognition and Management. Cleve Clin. J. Med. 2018, 85, S11–S18. [Google Scholar] [CrossRef]
- Al-Gamal, E. Quality of Life, Anxiety and Depression among Patients with Chronic Obstructive Pulmonary Disease and Their Spouses. Issues Ment. Health Nurs. 2014, 35, 761–767. [Google Scholar] [CrossRef]
- Abrams, T.E.; Vaughan-Sarrazin, M.; Vander Weg, M.W. Acute Exacerbations of Chronic Obstructive Pulmonary Disease and the Effect of Existing Psychiatric Comorbidity on Subsequent Mortality. Psychosomatics 2011, 52, 441–449. [Google Scholar] [CrossRef]
- Su, V.Y.-F.; Hu, L.-Y.; Yeh, C.-M.; Chiang, H.-L.; Shen, C.-C.; Chou, K.-T.; Chen, T.-J.; Lu, T.; Tzeng, C.-H.; Liu, C.-J. Chronic Obstructive Pulmonary Disease Associated with Increased Risk of Bipolar Disorder. Chronic Respir. Dis. 2017, 14, 151–160. [Google Scholar] [CrossRef]
- Tsai, P.-J.; Liao, Y.-T.; Lee, C.T.-C.; Hsu, C.-Y.; Hsieh, M.-H.; Tsai, C.-J.; Hsieh, M.-H.; Chen, V.C.-H. Risk of Bipolar Disorder in Patients with COPD: A Population-Based Cohort Study. Gen. Hosp. Psychiatry 2016, 41, 6–12. [Google Scholar] [CrossRef]
- Santos, G.; Ferreira, A.R.; Gonçalves-Pinho, M.; Freitas, A.; Fernandes, L. The Impact of Comorbid Psychiatric Disorders on Chronic Obstructive Pulmonary Disease (COPD) Hospitalizations: A Nationwide Retrospective Study. Soc. Psychiatry Psychiatr. Epidemiol. 2024. [Google Scholar] [CrossRef] [PubMed]
- Baghai-Ravary, R.; Quint, J.K.; Goldring, J.J.P.; Hurst, J.R.; Donaldson, G.C.; Wedzicha, J.A. Determinants and Impact of Fatigue in Patients with Chronic Obstructive Pulmonary Disease. Respir. Med. 2009, 103, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Yohannes, A.M.; Alexopoulos, G.S. Depression and Anxiety in Patients with COPD. Eur. Respir. Rev. 2014, 23, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Maurer, J.; Rebbapragada, V.; Borson, S.; Goldstein, R.; Kunik, M.E.; Yohannes, A.M.; Hanania, N.A. Anxiety and Depression in COPD. Chest 2008, 134, 43S–56S. [Google Scholar] [CrossRef] [PubMed]
- Matte, D.L.; Pizzichini, M.M.M.; Hoepers, A.T.C.; Diaz, A.P.; Karloh, M.; Dias, M.; Pizzichini, E. Prevalence of Depression in COPD: A Systematic Review and Meta-Analysis of Controlled Studies. Respir. Med. 2016, 117, 154–161. [Google Scholar] [CrossRef]
- Sampaio, M.S.; Vieira, W.D.A.; Bernardino, Í.D.M.; Herval, Á.M.; Flores-Mir, C.; Paranhos, L.R. Chronic Obstructive Pulmonary Disease as a Risk Factor for Suicide: A Systematic Review and Meta-Analysis. Respir. Med. 2019, 151, 11–18. [Google Scholar] [CrossRef]
- Hynninen, M.J.; Bjerke, N.; Pallesen, S.; Bakke, P.S.; Nordhus, I.H. A Randomized Controlled Trial of Cognitive Behavioral Therapy for Anxiety and Depression in COPD. Respir. Med. 2010, 104, 986–994. [Google Scholar] [CrossRef]
- Rahi, M.S.; Thilagar, B.; Balaji, S.; Prabhakaran, S.Y.; Mudgal, M.; Rajoo, S.; Yella, P.R.; Satija, P.; Zagorulko, A.; Gunasekaran, K. The Impact of Anxiety and Depression in Chronic Obstructive Pulmonary Disease. Adv. Respir. Med. 2023, 91, 123–134. [Google Scholar] [CrossRef]
- Stoeckel, M.C.; Esser, R.W.; Gamer, M.; Büchel, C.; von Leupoldt, A. Brain Responses during the Anticipation of Dyspnea. Neural Plast. 2016, 2016, 6434987. [Google Scholar] [CrossRef]
- Willgoss, T.G.; Yohannes, A.M. Anxiety Disorders in Patients with COPD: A Systematic Review. Respir. Care 2013, 58, 858–866. [Google Scholar] [CrossRef]
- Larsen, C.H.; Bendstrup, E.; Neergaard, M.A. Screening Tools for Depression and Anxiety in Patients with Chronic Obstructive Pulmonary Disease—A Systematic Review. COPD J. Chronic Obstr. Pulm. Dis. 2021, 18, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Patten, S.B.; Williams, J.V.A. Chronic Obstructive Lung Diseases and Prevalence of Mood, Anxiety, and Substance-Use Disorders in a Large Population Sample. Psychosomatics 2007, 48, 496–501. [Google Scholar] [CrossRef] [PubMed]
- Robinson, J. Role of Self-Medication in the Development of Comorbid Anxiety and Substance Use Disorders. Arch. Gen. Psychiatry 2011, 68, 800. [Google Scholar] [CrossRef] [PubMed]
- Khantzian, E.J. The Self-Medication Hypothesis of Substance Use Disorders: A Reconsideration and Recent Applications. Harv. Rev. Psychiatry 1997, 4, 231–244. [Google Scholar] [CrossRef]
- Zareifopoulos, N.; Bellou, A.; Spiropoulou, A.; Spiropoulos, K. Prevalence of Comorbid Chronic Obstructive Pulmonary Disease in Individuals Suffering from Schizophrenia and Bipolar Disorder: A Systematic Review. COPD J. Chronic Obstr. Pulm. Dis. 2018, 15, 612–620. [Google Scholar] [CrossRef]
- Zareifopoulos, N.; Bellou, A.; Spiropoulou, A.; Spiropoulos, K. Prevalence, Contribution to Disease Burden and Management of Comorbid Depression and Anxiety in Chronic Obstructive Pulmonary Disease: A Narrative Review. COPD J. Chronic Obstr. Pulm. Dis. 2019, 16, 406–417. [Google Scholar] [CrossRef]
- Di Marco, F.; Verga, M.; Reggente, M.; Maria Casanova, F.; Santus, P.; Blasi, F.; Allegra, L.; Centanni, S. Anxiety and Depression in COPD Patients: The Roles of Gender and Disease Severity. Respir. Med. 2006, 100, 1767–1774. [Google Scholar] [CrossRef]
- Cleland, J.A.; Lee, A.J.; Hall, S. Associations of Depression and Anxiety with Gender, Age, Health-Related Quality of Life and Symptoms in Primary Care COPD Patients. Fam. Pract. 2007, 24, 217–223. [Google Scholar] [CrossRef]
- Tang, T.; Li, Z.; Lu, X.; Du, J. Development and Validation of a Risk Prediction Model for Anxiety or Depression among Patients with Chronic Obstructive Pulmonary Disease between 2018 and 2020. Ann. Med. 2022, 54, 2181–2190. [Google Scholar] [CrossRef]
- Figueiredo, D.; Gabriel, R.; Jácome, C.; Cruz, J.; Marques, A. Caring for Relatives with Chronic Obstructive Pulmonary Disease: How Does the Disease Severity Impact on Family Carers? Aging Ment. Health 2014, 18, 385–393. [Google Scholar] [CrossRef]
- Chavannes, N.; Huibers, M.; Schermer, T.; Hendriks, A.; van Weel, C.; Wouters, E.; van Schayck, C. Associations of Depressive Symptoms with Gender, Body Mass Index and Dyspnea in Primary Care COPD Patients. Fam. Pract. 2005, 22, 604–607. [Google Scholar] [CrossRef] [PubMed]
- Hanania, N.A.; Müllerova, H.; Locantore, N.W.; Vestbo, J.; Watkins, M.L.; Wouters, E.F.M.; Rennard, S.I.; Sharafkhaneh, A. Determinants of Depression in the ECLIPSE Chronic Obstructive Pulmonary Disease Cohort. Am. J. Respir. Crit. Care Med. 2011, 183, 604–611. [Google Scholar] [CrossRef] [PubMed]
- Lou, P.; Zhu, Y.; Chen, P.; Zhang, P.; Yu, J.; Zhang, N.; Chen, N.; Zhang, L.; Wu, H.; Zhao, J. Prevalence and Correlations with Depression, Anxiety, and Other Features in Outpatients with Chronic Obstructive Pulmonary Disease in China: A Cross-Sectional Case Control Study. BMC Pulm. Med. 2012, 12, 53. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Batra, S.; Prasad, R.; Verma, A.; Jilani, A.Q.; Kant, S. A Study on the Prevalence of Depression and the Severity of Depression in Patients of Chronic Obstructive Pulmonary Disease in a Semi-Urban Indian Population. Monaldi Arch. Chest Dis. 2018, 88, 902. [Google Scholar] [CrossRef] [PubMed]
- An, L.; Lin, Y.-X.; Yang, T.; Zhang, H.; Jiao, X.; Zhang, S.; Chang, X.-H.; Wang, Z.-M.; Wang, C. Predictive Validity of BODE Index for Anxious and Depressive Symptoms in Patients with Chronic Obstructive Pulmonary Disease. Chin. Med. J. 2010, 123, 1845–1851. [Google Scholar]
- Jordan, A.; Sivapalan, P.; Eklöf, J.; Vestergaard, J.B.; Meteran, H.; Saeed, M.I.; Biering-Sørensen, T.; Løkke, A.; Seersholm, N.; Jensen, J.U.S. The Association between Use of ICS and Psychiatric Symptoms in Patients with COPD—A Nationwide Cohort Study of 49,500 Patients. Biomedicines 2021, 9, 1492. [Google Scholar] [CrossRef]
- Alturaymi, M.A.; Almadhi, O.F.; Alageel, Y.S.; Bin Dayel, M.; Alsubayyil, M.S.; Alkhateeb, B.F. The Association between Prolonged Use of Oral Corticosteroids and Mental Disorders: Do Steroids Have a Role in Developing Mental Disorders? Cureus 2023, 15, e37627. [Google Scholar] [CrossRef]
- Warrington, T.P.; Bostwick, J.M. Psychiatric Adverse Effects of Corticosteroids. Mayo Clin. Proc. 2006, 81, 1361–1367. [Google Scholar] [CrossRef]
- Brown, E.S.; Chandler, P.A. Mood and Cognitive Changes During Systemic Corticosteroid Therapy. Prim. Care Companion CNS Disord. 2001, 3, 17. [Google Scholar] [CrossRef]
- Salpeter, S.R.; Ormiston, T.M.; Salpeter, E.E. Cardiovascular Effects of β-Agonists in Patients with Asthma and COPD. Chest 2004, 125, 2309–2321. [Google Scholar] [CrossRef]
- Malaz Boustani, M. The Cognitive Impact of Anticholinergics: A Clinical Review. Clin. Interv. Aging 2009, 4, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Coupland, C.A.C.; Hill, T.; Dening, T.; Morriss, R.; Moore, M.; Hippisley-Cox, J. Anticholinergic Drug Exposure and the Risk of Dementia. JAMA Intern. Med. 2019, 179, 1084. [Google Scholar] [CrossRef] [PubMed]
- Divo, M.; Cote, C.; de Torres, J.P.; Casanova, C.; Marin, J.M.; Pinto-Plata, V.; Zulueta, J.; Cabrera, C.; Zagaceta, J.; Hunninghake, G.; et al. Comorbidities and Risk of Mortality in Patients with Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2012, 186, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Bian, Y.; Zhao, Y.; Jin, Z.; Liu, L.; Li, G. The Impact of Depression and Anxiety on Chronic Obstructive Pulmonary Disease Acute Exacerbations: A Prospective Cohort Study. J. Affect. Disord. 2021, 281, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Yohannes, A.M.; Mülerová, H.; Lavoie, K.; Vestbo, J.; Rennard, S.I.; Wouters, E.; Hanania, N.A. The Association of Depressive Symptoms with Rates of Acute Exacerbations in Patients with COPD: Results from a 3-Year Longitudinal Follow-up of the ECLIPSE Cohort. J. Am. Med. Dir. Assoc. 2017, 18, 955–959.e6. [Google Scholar] [CrossRef]
- Hong, Y.J.; Kim, Y.; Moon, J.-Y.; Park, S.; Lee, J.-K.; Jung, K.-S.; Yoo, K.H.; Kim, Y.-I.; Choi, J.Y. Associations between Depression and Anxiety Index and Frequency of Acute Exacerbation in Chronic Obstructive Pulmonary Disease. Ther. Adv. Respir. Dis. 2023, 17. [Google Scholar] [CrossRef]
- Sethi, J.M.; Rochester, C.L. Smoking and Chronic Obstructive Pulmonary Disease. Clin. Chest Med. 2000, 21, 67–86. [Google Scholar] [CrossRef]
- Fluharty, M.; Taylor, A.E.; Grabski, M.; Munafò, M.R. The Association of Cigarette Smoking with Depression and Anxiety: A Systematic Review. Nicotine Tob. Res. 2017, 19, 3–13. [Google Scholar] [CrossRef]
- Ouellette, D.R.; Lavoie, K. Recognition, Diagnosis, and Treatment of Cognitive and Psychiatric Disorders in Patients with COPD. Int. J. Chronic Obstr. Pulm. Dis. 2017, 12, 639–650. [Google Scholar] [CrossRef]
- American Psychiatric Association, DSM-5 Task Force. Diagnostic and Statistical Manual of Mental Disorders: DSM-5TM, 5th ed.; American Psychiatric Publishing, Inc.: Arlington, VA, USA, 2013; ISBN 979-0-89042-559-6. [Google Scholar]
- Schachter, S.; Singer, J. Cognitive, Social, and Physiological Determinants of Emotional State. Psychol. Rev. 1962, 69, 379–399. [Google Scholar] [CrossRef]
- Assaf, E.A.; Badarneh, A.; Saifan, A.; Al-Yateem, N. Chronic Obstructive Pulmonary Disease Patients’ Quality of Life and Its Related Factors: A Cross-Sectional Study of the Jordanian Population. F1000Res 2022, 11, 581. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Nyunt, M.S.Z.; Gwee, X.; Feng, L.; Feng, L.; Kua, E.H.; Kumar, R.; Ng, T.P. Life Event Stress and Chronic Obstructive Pulmonary Disease (COPD): Associations with Mental Well-Being and Quality of Life in a Population-Based Study. BMJ Open 2012, 2, e001674. [Google Scholar] [CrossRef] [PubMed]
- Miravitlles, M.; Ribera, A. Understanding the Impact of Symptoms on the Burden of COPD. Respir. Res. 2017, 18, 67. [Google Scholar] [CrossRef] [PubMed]
- Pumar, M.I.; Gray, C.R.; Walsh, J.R.; Yang, I.A.; Rolls, T.A.; Ward, D.L. Anxiety and Depression-Important Psychological Comorbidities of COPD. J. Thorac. Dis. 2014, 6, 1615–1631. [Google Scholar] [CrossRef]
- Lange, P.; Marott, J.L.; Vestbo, J.; Ingebrigtsen, T.S.; Nordestgaard, B.G. Socioeconomic Status and Prognosis of COPD in Denmark. COPD J. Chronic Obstr. Pulm. Dis. 2014, 11, 431–437. [Google Scholar] [CrossRef]
- Chetty, U.; McLean, G.; Morrison, D.; Agur, K.; Guthrie, B.; Mercer, S.W. Chronic Obstructive Pulmonary Disease and Comorbidities: A Large Cross-Sectional Study in Primary Care. Br. J. Gen. Pract. 2017, 67, e321–e328. [Google Scholar] [CrossRef]
- Sinden, N.J.; Stockley, R.A. Systemic Inflammation and Comorbidity in COPD: A Result of “overspill” of Inflammatory Mediators from the Lungs? Review of the Evidence. Thorax 2010, 65, 930–936. [Google Scholar] [CrossRef]
- Lu, Y.; Feng, L.; Feng, L.; Nyunt, M.S.; Yap, K.B.; Ng, T.P. Systemic Inflammation, Depression and Obstructive Pulmonary Function: A Population-Based Study. Respir. Res. 2013, 14, 53. [Google Scholar] [CrossRef]
- Liu, T.; Zhong, S.; Liao, X.; Chen, J.; He, T.; Lai, S.; Jia, Y. A Meta-Analysis of Oxidative Stress Markers in Depression. PLoS ONE 2015, 10, e0138904. [Google Scholar] [CrossRef]
- Goldstein, B.I.; Kemp, D.E.; Soczynska, J.K.; McIntyre, R.S. Inflammation and the Phenomenology, Pathophysiology, Comorbidity, and Treatment of Bipolar Disorder. J. Clin. Psychiatry 2009, 70, 1078–1090. [Google Scholar] [CrossRef]
- Kivimäki, M.; Shipley, M.J.; Batty, G.D.; Hamer, M.; Akbaraly, T.N.; Kumari, M.; Jokela, M.; Virtanen, M.; Lowe, G.D.; Ebmeier, K.P.; et al. Long-Term Inflammation Increases Risk of Common Mental Disorder: A Cohort Study. Mol. Psychiatry 2014, 19, 149–150. [Google Scholar] [CrossRef] [PubMed]
- Bratek, A.; Zawada, K.; Beil-Gawełczyk, J.; Beil, S.; Sozańska, E.; Krysta, K.; Barczyk, A.; Krupka-Matuszczyk, I.; Pierzchała, W. Depressiveness, Symptoms of Anxiety and Cognitive Dysfunctions in Patients with Asthma and Chronic Obstructive Pulmonary Disease (COPD): Possible Associations with Inflammation Markers: A Pilot Study. J. Neural Transm. 2015, 122, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Krishnadas, R.; Cavanagh, J. Depression: An Inflammatory Illness?: Figure 1. J. Neurol. Neurosurg. Psychiatry 2012, 83, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Zinellu, E.; Zinellu, A.; Fois, A.G.; Carru, C.; Pirina, P. Circulating Biomarkers of Oxidative Stress in Chronic Obstructive Pulmonary Disease: A Systematic Review. Respir. Res. 2016, 17, 150. [Google Scholar] [CrossRef] [PubMed]
- Juszczyk, G.; Mikulska, J.; Kasperek, K.; Pietrzak, D.; Mrozek, W.; Herbet, M. Chronic Stress and Oxidative Stress as Common Factors of the Pathogenesis of Depression and Alzheimer’s Disease: The Role of Antioxidants in Prevention and Treatment. Antioxidants 2021, 10, 1439. [Google Scholar] [CrossRef]
- Hill, K.; Geist, R.; Goldstein, R.S.; Lacasse, Y. Anxiety and Depression in End-Stage COPD. Eur. Respir. J. 2008, 31, 667–677. [Google Scholar] [CrossRef]
- Feng, J.; Yang, Q.; Wang, Y.; Cao, J.; Chen, B. Intermittent Hypoxia from Obstructive Sleep Apnea May Cause Neuronal Impairment and Dysfunction in Central Nervous System: The Potential Roles Played by Microglia. Neuropsychiatr. Dis. Treat. 2013, 9, 1077–1086. [Google Scholar] [CrossRef]
- Burtscher, J.; Niedermeier, M.; Hüfner, K.; van den Burg, E.; Kopp, M.; Stoop, R.; Burtscher, M.; Gatterer, H.; Millet, G.P. The Interplay of Hypoxic and Mental Stress: Implications for Anxiety and Depressive Disorders. Neurosci. Biobehav. Rev. 2022, 138, 104718. [Google Scholar] [CrossRef]
- Padgett, D.A.; Glaser, R. How Stress Influences the Immune Response. Trends Immunol. 2003, 24, 444–448. [Google Scholar] [CrossRef]
- Woo, S.; Zhou, W.; Larson, J.L. Stigma Experiences in People with Chronic Obstructive Pulmonary Disease: An Integrative Review. Int. J. Chronic Obstr. Pulm. Dis. 2021, 16, 1647–1659. [Google Scholar] [CrossRef]
- Brown, E.S. Effects of Glucocorticoids on Mood, Memory, and the Hippocampus. Ann. N. Y. Acad. Sci. 2009, 1179, 41–55. [Google Scholar] [CrossRef] [PubMed]
- Wium-Andersen, M.K.; Orsted, D.D.; Nordestgaard, B.G. Tobacco Smoking Is Causally Associated with Antipsychotic Medication Use and Schizophrenia, but Not with Antidepressant Medication Use or Depression. Int. J. Epidemiol. 2015, 44, 566–577. [Google Scholar] [CrossRef] [PubMed]
- Montserrat-Capdevila, J.; Godoy, P.; Marsal, J.R.; Barbé, F.; Pifarré, J.; Alsedà, M.; Ortega, M. Overview of the Impact of Depression and Anxiety in Chronic Obstructive Pulmonary Disease. Lung 2017, 195, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Dury, R. COPD and Emotional Distress: Not Always Noticed and Therefore Untreated. Br. J. Community Nurs. 2016, 21, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Windisch, W.; Freidel, K.; Schucher, B.; Baumann, H.; Wiebel, M.; Matthys, H.; Petermann, F. The Severe Respiratory Insufficiency (SRI) Questionnaire A Specific Measure of Health-Related Quality of Life in Patients Receiving Home Mechanical Ventilation. J. Clin. Epidemiol. 2003, 56, 752–759. [Google Scholar] [CrossRef]
- Willgoss, T.G.; Goldbart, J.; Fatoye, F.; Yohannes, A.M. The Development and Validation of the Anxiety Inventory for Respiratory Disease. Chest 2013, 144, 1587–1596. [Google Scholar] [CrossRef]
- Kühl, K.; Kuhn, C.; Kenn, K.; Rief, W. Der COPD-Angst-Fragebogen (CAF): Ein Neues Instrument Zur Erfassung Krankheitsspezifischer Ängste Bei COPD-Patienten. PPmP—Psychother. Psychosom. Med. Psychol. 2011, 61, e1–e9. [Google Scholar] [CrossRef]
- Tamburrino, M.B.; Lynch, D.J.; Nagel, R.W.; Smith, M.K. Primary Care Evaluation of Mental Disorders (PRIME-MD) Screening for Minor Depressive Disorder in Primary Care. Prim. Care Companion J. Clin. Psychiatry 2009, 11, 339–343. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder. Arch. Intern. Med. 2006, 166, 1092. [Google Scholar] [CrossRef]
- Bratås, O.; Grønning, K.; Forbord, T. Psychometric Properties of The Hospital Anxiety and Depression Scale and The General Health Questionnaire-20 in <scp>COPD</Scp> Inpatients. Scand. J. Caring Sci. 2014, 28, 413–420. [Google Scholar] [CrossRef]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An Inventory for Measuring Clinical Anxiety: Psychometric Properties. J. Consult. Clin. Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Kabacoff, R.I.; Segal, D.L.; Hersen, M.; Van Hasselt, V.B. Psychometric Properties and Diagnostic Utility of the Beck Anxiety Inventory and the State-Trait Anxiety Inventory with Older Adult Psychiatric Outpatients. J. Anxiety Disord. 1997, 11, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M. The Assessment of Anxiety States by Rating. Br. J. Med. Psychol. 1959, 32, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Spielberger, C.D. State-Trait Anxiety Inventory: Bibliography, 2nd ed.; Consulting Psychologists Press: Palo Alto, CA, USA, 1989. [Google Scholar]
- Arnau, R.C.; Meagher, M.W.; Norris, M.P.; Bramson, R. Psychometric Evaluation of the Beck Depression Inventory-II with Primary Care Medical Patients. Health Psychol. 2001, 20, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Chen, X.; Guo, Y.; Zhang, T.; Lin, J.; Ding, X. Effects of Cognitive Behavioral Therapy in Patients with Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-analysis. Worldviews Evid. Based Nurs. 2024, 21, 288–306. [Google Scholar] [CrossRef]
- Wei, X.; Guo, K.; Shang, X.; Wang, S.; Yang, C.; Li, J.; Li, Y.; Yang, K.; Li, X.; Zhang, X. Effects of Different Interventions on Smoking Cessation in Chronic Obstructive Pulmonary Disease Patients: A Systematic Review and Network Meta-Analysis. Int. J. Nurs. Stud. 2022, 136, 104362. [Google Scholar] [CrossRef]
- Yohannes, A.M.; Alexopoulos, G.S. Pharmacological Treatment of Depression in Older Patients with Chronic Obstructive Pulmonary Disease: Impact on the Course of the Disease and Health Outcomes. Drugs Aging 2014, 31, 483–492. [Google Scholar] [CrossRef]
- Trifirò, G.; Crisafulli, S. Is Antidepressant Use a Concern for Patients with COPD? Thorax 2024, 79, 3–4. [Google Scholar] [CrossRef]
- Vozoris, N.T.; Wang, X.; Austin, P.C.; Stephenson, A.L.; O’Donnell, D.E.; Gershon, A.S.; Gill, S.S.; Rochon, P.A. Serotonergic Antidepressant Use and Morbidity and Mortality among Older Adults with COPD. Eur. Respir. J. 2018, 52, 1800475. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Zheng, Y.; Xu, C.; Yang, H.; Wang, Z.; Zhou, L.; Wan, Y.; Zheng, D.; Zhu, J. Sertraline Hydrochloride Treatment for Patients with Stable Chronic Obstructive Pulmonary Disease Complicated with Depression: A Randomized Controlled Trial. Clin. Respir. J. 2016, 10, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, H.F.; Lederer, D.; Lovasi, G.S.; Hiura, G.; Ventetuolo, C.E.; Barr, R. Selective Serotonin Reuptake Inhibitors and Lung Function in the Multi-Ethnic Study of Atherosclerosis Lung Study. Respir. Med. 2022, 196, 106805. [Google Scholar] [CrossRef] [PubMed]
- Volpato, E.; Toniolo, S.; Pagnini, F.; Banfi, P. The Relationship between Anxiety, Depression and Treatment Adherence in Chronic Obstructive Pulmonary Disease: A Systematic Review. Int. J. Chronic Obstr. Pulm. Dis. 2021, 16, 2001–2021. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Simoni-Wastila, L.; Albrecht, J.S.; Huang, T.; Moyo, P.; Khokhar, B.; Harris, I.; Langenberg, P.; Netzer, G.; Lehmann, S.W. The Association of Antidepressant Treatment with COPD Maintenance Medication Use and Adherence in a Comorbid Medicare Population: A Longitudinal Cohort Study. Int. J. Geriatr. Psychiatry 2018, 33, e212–e220. [Google Scholar] [CrossRef]
- Borson, S.; McDonald, G.J.; Gayle, T.; Deffebach, M.; Lakshminarayan, S.; VanTuinen, C. Improvement in Mood, Physical Symptoms, and Function with Nortriptyline for Depression in Patients with Chronic Obstructive Pulmonary Disease. Psychosomatics 1992, 33, 190–201. [Google Scholar] [CrossRef]
- Yohannes, A.M.; Jin, J.W.; Kunik, M.E. Benefit–Risk Assessment of Psychotropic Drugs in Older Patients with Chronic Obstructive Pulmonary Disease. Drugs Aging 2022, 39, 323–332. [Google Scholar] [CrossRef]
- Pollok, J.; van Agteren, J.E.; Carson-Chahhoud, K.V. Pharmacological Interventions for the Treatment of Depression in Chronic Obstructive Pulmonary Disease. Cochrane Database Syst. Rev. 2018, 2018. [Google Scholar] [CrossRef]
- Vozoris, N.T.; Fischer, H.D.; Wang, X.; Stephenson, A.L.; Gershon, A.S.; Gruneir, A.; Austin, P.C.; Anderson, G.M.; Bell, C.M.; Gill, S.S.; et al. Benzodiazepine Drug Use and Adverse Respiratory Outcomes among Older Adults with COPD. Eur. Respir. J. 2014, 44, 332–340. [Google Scholar] [CrossRef]
- Dahan, A.; van Lemmen, M.; Jansen, S.; Simons, P.; van der Schrier, R. Buprenorphine: A Treatment and Cause of Opioid-Induced Respiratory Depression. Br. J. Anaesth. 2022, 128, 402–404. [Google Scholar] [CrossRef]
- Cohn, M.A.; Morris, D.D.; Juan, D. Effects of Estazolam and Flurazepam on Cardiopulmonary Function in Patients with Chronic Obstructive Pulmonary Disease. Drug Saf. 1992, 7, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Currow, D.C.; Agar, M.R. Benzodiazepine Prescribing in People with Chronic Obstructive Pulmonary Disease: Clinical Considerations. Drugs Aging 2020, 37, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Man, G.C.W.; Hsu, K.; Sproule, B.J. Effect of Alprazolam on Exercise and Dyspnea in Patients with Chronic Obstructive Pulmonary Disease. Chest 1986, 90, 832–836. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.P.; Despars, J.A.; Stansbury, D.W.; Avalos, K.; Light, R.W. Effects of Buspirone on Anxiety Levels and Exercise Tolerance in Patients with Chronic Airflow Obstruction and Mild Anxiety. Chest 1993, 103, 800–804. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.-J.; Yeh, C.-M.; Chao, T.-F.; Liu, C.-J.; Wang, K.-L.; Chen, T.-J.; Chou, P.; Wang, F.-D. The Use of Benzodiazepine Receptor Agonists and Risk of Respiratory Failure in Patients with Chronic Obstructive Pulmonary Disease: A Nationwide Population-Based Case-Control Study. Sleep 2015, 38, 1045–1050. [Google Scholar] [CrossRef]
- El-Solh, A.A.; Lawson, Y.; Wilding, G.E. Association between Hypnotic Use and All-Cause Mortality in Patients with Chronic Obstructive Pulmonary Disease and Insomnia. Int. J. Chronic Obstr. Pulm. Dis. 2023, 18, 2393–2404. [Google Scholar] [CrossRef]
- Wang, M.-T.; Tsai, C.-L.; Lin, C.W.; Yeh, C.-B.; Wang, Y.-H.; Lin, H.-L. Association between Antipsychotic Agents and Risk of Acute Respiratory Failure in Patients with Chronic Obstructive Pulmonary Disease. JAMA Psychiatry 2017, 74, 252. [Google Scholar] [CrossRef]
- Ferraris, A.; Blasco, B.; Tentoni, N.; Del Olmo, F.; Barrera, T.; Angriman, F.; Szmulewicz, A.G. Antipsychotic Use and Bloodstream Infections Among Adult Patients with Chronic Obstructive Pulmonary Disease. J. Clin. Psychiatry 2021, 82, 32060. [Google Scholar] [CrossRef]
- Mantere, O.; Trontti, K.; García-González, J.; Balcells, I.; Saarnio, S.; Mäntylä, T.; Lindgren, M.; Kieseppä, T.; Raij, T.; Honkanen, J.K.; et al. Immunomodulatory Effects of Antipsychotic Treatment on Gene Expression in First-Episode Psychosis. J. Psychiatr. Res. 2019, 109, 18–26. [Google Scholar] [CrossRef]
- Williams, M.T.; Johnston, K.N.; Paquet, C. Cognitive Behavioral Therapy for People with Chronic Obstructive Pulmonary Disease: Rapid Review. Int. J. Chronic Obstr. Pulm. Dis. 2020, 15, 903–919. [Google Scholar] [CrossRef]
- Godschalx-Dekker, J.A.; Mooren, K.J.M. Treatment of Anxiety in COPD with CBT. Ned. Tijdschr. Voor Geneeskd. 2022, 165, D5995. [Google Scholar]
- Heslop-Marshall, K.; Baker, C.; Carrick-Sen, D.; Newton, J.; Echevarria, C.; Stenton, C.; Jambon, M.; Gray, J.; Pearce, K.; Burns, G.; et al. Randomised Controlled Trial of Cognitive Behavioural Therapy in COPD. ERJ Open Res. 2018, 4, 00094–02018. [Google Scholar] [CrossRef] [PubMed]
- Tian, L.; Zhang, Y.; Li, L.; Wu, Y.; Li, Y. The Efficacy of Mindfulness-Based Interventions for Patients with COPD: A Systematic Review and Meta-Analysis Protocol. BMJ Open 2019, 9, e026061. [Google Scholar] [CrossRef] [PubMed]
- Chan, R.; Giardino, N.; Larson, J. A Pilot Study: Mindfulness Meditation Intervention in COPD. Int. J. Chronic Obstr. Pulm. Dis. 2015, 10, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Malpass, A.; Kessler, D.; Sharp, D.; Shaw, A. MBCT for Patients with Respiratory Conditions Who Experience Anxiety and Depression: A Qualitative Study. Mindfulness 2015, 6, 1181–1191. [Google Scholar] [CrossRef]
- Coventry, P.A.; Bower, P.; Keyworth, C.; Kenning, C.; Knopp, J.; Garrett, C.; Hind, D.; Malpass, A.; Dickens, C. The Effect of Complex Interventions on Depression and Anxiety in Chronic Obstructive Pulmonary Disease: Systematic Review and Meta-Analysis. PLoS ONE 2013, 8, e60532. [Google Scholar] [CrossRef]
- Coventry, P.; Panagioti, M.; Scott, C.; Blakemore, A. Overview of the Prevalence, Impact, and Management of Depression and Anxiety in Chronic Obstructive Pulmonary Disease. Int. J. Chronic Obstr. Pulm. Dis. 2014, 9, 1289–1306. [Google Scholar] [CrossRef]
- Whiting, P.F.; Wolff, R.F.; Deshpande, S.; Di Nisio, M.; Duffy, S.; Hernandez, A.V.; Keurentjes, J.C.; Lang, S.; Misso, K.; Ryder, S.; et al. Cannabinoids for Medical Use. JAMA 2015, 313, 2456. [Google Scholar] [CrossRef]
| Reference | Study Type | Disease | Subjects (n) | Reported Prevalence |
|---|---|---|---|---|
| [12] | Case-control study | Generalized anxiety disorder | COPD = 74 Controls = 74 | 5.41% 1.35% |
| Major depressive episode | COPD = 74 Controls = 74 | 2.70% 0 | ||
| Panic disorder | COPD = 74 Controls = 74 | 4.05% 0 | ||
| Substance dependence | COPD = 74 Controls = 74 | 16.21% 1.35% | ||
| [26] | Metanalysis | Depression | COPD = 5552 Controls = 5211 | 27.1% [25.9–28.3] * 10.0% [9.2–10.8] * |
| [25] | Review | Depression and anxiety | - | Depression: 10–42% Anxiety: 10–19% |
| [33] | Observational study | Depression | Chronic bronchitis = 1440 Emphysema = 518 Controls = 32,509 | 8.7% (6.8–10.7) § 7.5% (4.7–10.2) 3.6% (3.3–3.8) |
| Bipolar disorder | Chronic bronchitis = 1440 Emphysema = 518 Controls = 32,509 | 3.3% (2.1–4.6) - 0.8% (0.7–0.9) | ||
| Panic disorder | Chronic bronchitis = 1440 Emphysema = 518 Controls = 32,509 | 6.5% (4.6–8.3) - 1.8% (1.6–2.0) | ||
| Social phobia | Chronic bronchitis = 1440 Emphysema = 518 Controls = 32,509 | 7.2% (5.3–9.1) 6.5% (3.7–9.2) 2.8% (2.5–3.0) | ||
| Substance dependence | Chronic bronchitis = 1440 Emphysema = 518 Controls = 32,509 | 7.9% (5.0–10.8) - 2.8% (2.6–3.0) | ||
| [31] | Metanalysis | Generalized anxiety disorder | COPD inpatients = 358 COPD outpatients = 333 | 10–55% 13–46% |
| Clinical Scales | Clinical Function and Psychometric Structure | Authors |
|---|---|---|
| Severe Respiratory Insufficiency (SRI) | A specific measure of health-related quality of life in patients receiving home mechanical ventilation. The scale is provided by a five-point Likert scale, a scaling method that measures either positive or negative responses. Scores ranging between 0 and 100. Higher scores are attributed to better health-related quality of life (HRQL). | [87] |
| Anxiety Inventory for Respiratory Disease (AIR) | A scale to screen and measure anxiety in patients with COPD. The score range is from 0 to 30, and the high scores indicate elevated symptoms of anxiety. | [88] |
| COPD Anxiety Questionnaire (CAF) | CAF is a self-report scale developed to measure specifically anxiety in patients with COPD. Each item is rated by the patients themselves using a five-point Likert scale ranging from “never” (scored 0) to “always” (scored 4), with a total score ranging from 0 to 100. Higher scores indicate high levels of anxiety. | [89] |
| Primary Care Evaluation of Mental Disorders Patient Questionnaire (PRIME-MD PQ) | The PRIME-MD PQ is a self-administered one-page questionnaire consisting of 26 yes/no questions about the presence of symptoms and signs during the past month. | [90] |
| Generalized Anxiety Disorder seven-item scale (GAD-7) | This seven-item scale (GAD-7) is used to screen for anxiety or to measure its severity. Although designed as a screening tool for generalized anxiety, the GAD-7 also performs reasonably well as a screening tool for three other common anxiety disorders—panic disorder, social anxiety disorder, and post-traumatic stress disorder. GAD-7 total score for the seven items ranges from 0 to 21. Scores of 5, 10, and 15 represent cut points for mild, moderate, and severe anxiety, respectively. | [91] |
| General Health Questionnaire-version 20 (GHQ-20) | It is a self-administered screening scale for identifying minor psychiatric disorders. It consists of 20 items asking respondents to compare their current status with their normal situation. Answers are scored on a four-point Likert-type scale ranging from 0 (less than usual) to 3 (much more than usual). Scores can range from 0 to 60, and lower scores means better mental health. | [92] |
| Beck Anxiety Inventory (BAI) | A self-administered scale consisting of a list of 21 items that measures how much the patient has been bothered by that symptom during the past month. Scores ranging from 0 to 63: minimal anxiety levels (0–7), mild anxiety (8–15), moderate anxiety (16–25), and severe anxiety (26–63). | [93,94] |
| Hamilton Anxiety Rating Scale (HARS) | The scale consists of 14 items, each defined by a series of symptoms, and measures both psychic anxiety (mental agitation and psychological distress) and somatic anxiety (physical complaints related to anxiety). A total score ranging from 0–56: scores <17 indicates mild severity; between 18–24 indicates mild to moderate severity; between 25–30 indicates moderate to severe. | [95] |
| State—Trait Anxiety Inventory (STAI) | It is a 40-item self-report measure of anxiety using a four-point Likert-type scale (from 0 to 3 points) for each item. It has two scales: State anxiety, i.e., how one feels at the moment; and Trait anxiety, i.e., how one generally feels. It is composed of 20 items to be rated on a 1–4 scale, with higher scores meaning higher levels of anxiety; the cut-off score for the presence of relevant anxiety symptoms is 40. | [96] |
| Beck Depression Inventory (BDI) | It is a 21-item, multiple-choice inventory. Respondents are asked to rate each item based on four response choices according to the severity of the symptoms, ranging from the absence of a symptom to an intense level, during the past week. Each question is scored on a four-point scale ranging from no impairment (0) to severe impairment (3). The maximum score is 63; a cut-off score indicative of mild depressive symptoms is higher than 10, and for severe depressive symptoms the cut-off score is higher than 30. | [97] |
| Hospital Anxiety and Depression Scale (HADS) | It is a 14-item self-report scale for symptoms of depression and anxiety in a general medical population of patients. Each item is scored on a scale ranging from 0 (no symptom) to 3 (severe symptom). Scores ranging from 8–10 indicate doubtful cases, while scores ≥ 11 indicate clinically relevant cases. A cut-off score ≥ 8 can be considered optimal for both sensitivity and specificity for the diagnosis of clinically relevant anxiety and depression. | [98] |
| Patient Health Questionnaire (PHQ-9) | It is a multipurpose instrument for screening, diagnosing, monitoring, and measuring the severity of depression. Scores range from 0 to 27, where high scores mean greater presence of depressive symptoms. | [99] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moretta, P.; Cavallo, N.D.; Candia, C.; Lanzillo, A.; Marcuccio, G.; Santangelo, G.; Marcuccio, L.; Ambrosino, P.; Maniscalco, M. Psychiatric Disorders in Patients with Chronic Obstructive Pulmonary Disease: Clinical Significance and Treatment Strategies. J. Clin. Med. 2024, 13, 6418. https://doi.org/10.3390/jcm13216418
Moretta P, Cavallo ND, Candia C, Lanzillo A, Marcuccio G, Santangelo G, Marcuccio L, Ambrosino P, Maniscalco M. Psychiatric Disorders in Patients with Chronic Obstructive Pulmonary Disease: Clinical Significance and Treatment Strategies. Journal of Clinical Medicine. 2024; 13(21):6418. https://doi.org/10.3390/jcm13216418
Chicago/Turabian StyleMoretta, Pasquale, Nicola Davide Cavallo, Claudio Candia, Anna Lanzillo, Giuseppina Marcuccio, Gabriella Santangelo, Laura Marcuccio, Pasquale Ambrosino, and Mauro Maniscalco. 2024. "Psychiatric Disorders in Patients with Chronic Obstructive Pulmonary Disease: Clinical Significance and Treatment Strategies" Journal of Clinical Medicine 13, no. 21: 6418. https://doi.org/10.3390/jcm13216418
APA StyleMoretta, P., Cavallo, N. D., Candia, C., Lanzillo, A., Marcuccio, G., Santangelo, G., Marcuccio, L., Ambrosino, P., & Maniscalco, M. (2024). Psychiatric Disorders in Patients with Chronic Obstructive Pulmonary Disease: Clinical Significance and Treatment Strategies. Journal of Clinical Medicine, 13(21), 6418. https://doi.org/10.3390/jcm13216418








