How a Gauze Sponge Roll Enhances Surgical Exposure in Thumb Carpometacarpal Arthroplasty: A Technical Note
Abstract
1. Introduction
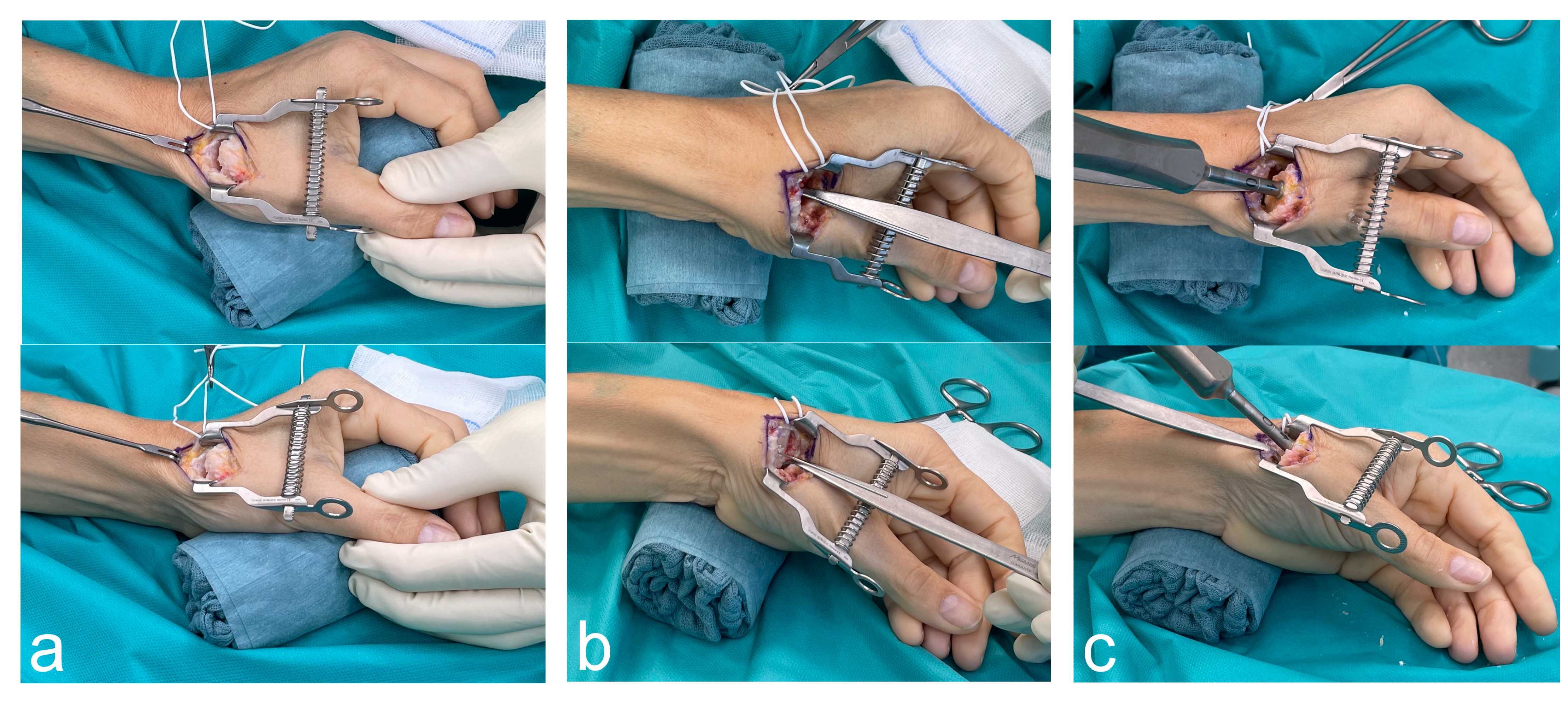
2. Surgical Technique
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- de la Caffinière, J.Y. Prothèse totale trapézo-métacarpienne. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1974, 60, 299–308. [Google Scholar]
- Holme, T.J.; Karbowiak, M.; Clements, J.; Sharma, R.; Craik, J.; Ellahee, N. Thumb CMCJ prosthetic total joint replacement: A systematic review. EFORT Open Rev. 2021, 6, 316–330. [Google Scholar] [CrossRef]
- Bæk Hansen, T. Joint replacement for trapeziometacarpal osteoarthritis: Implants and outcomes. J. Hand Surg. Eur. Vol. 2021, 46, 115–119. [Google Scholar] [CrossRef]
- Froschauer, S.M.; Holzbauer, M.; Hager, D.; Schnelzer, R.; Kwasny, O.; Duscher, D. Elektra prosthesis versus resection-suspension arthroplasty for thumb carpometacarpal osteoarthritis: A long-term cohort study. J. Hand Surg. Eur. Vol. 2019, 45, 452–457. [Google Scholar] [CrossRef]
- Kollig, E.; Weber, W.; Bieler, D.; Franke, A. Failure of an uncemented thumb carpometacarpal joint ceramic prosthesis. J. Hand Surg. Eur. Vol. 2017, 42, 599–604. [Google Scholar] [CrossRef]
- Herren, D.B.; Beaulieu, J.-Y.; Calcagni, M.; Erling, C.; Jung, M.; Kaulich, A.; Mühldorfer-Fodor, M.; Papaloïzos, M.; Rosenkranz, A.; Vögelin, E.; et al. Aktuelle Trends bei der Implantation der Touch-Prothese am Daumensattelgelenk: Ergebnisse des 1. deutschsprachigen Anwendertreffens. Handchir. Mikrochir. Plast. Chir. 2024, 56, 201–211. [Google Scholar] [CrossRef]
- Maes-Clavier, C.; David, E.; Biau, D.; Hustin, C.; Rotari, V. Évaluation de la courbe d’apprentissage des prothèses trapézométacarpiennes Maia par le LC-CUSUM Test. Chir. Main. 2015, 34, 383. [Google Scholar] [CrossRef]
- Dumartinet-Gibaud, R.; Bigorre, N.; Raimbeau, G.; Jeudy, J.; Saint Cast, Y. Arpe total joint arthroplasty for trapeziometacarpal osteoarthritis: 80 thumbs in 63 patients with a minimum of 10 years follow-up. J. Hand Surg. Eur. Vol. 2020, 45, 465–469. [Google Scholar] [CrossRef]
- Froschauer, S.M.; Holzbauer, M.; Mihalic, J.A.; Kwasny, O. TOUCH® Prosthesis for Thumb Carpometacarpal Joint Osteoarthritis: A Prospective Case Series. J. Clin. Med. 2021, 10, 4090. [Google Scholar] [CrossRef]
- Reischenböck, V.; Marks, M.; Imhof, J.; Schindele, S.; Herren, D.B. Management of the capsule in trapeziometacarpal joint implant arthroplasty: Resection versus repair. J. Hand Surg. Eur. Vol. 2024, 49, 1104–1109. [Google Scholar] [CrossRef]
- Brinkhorst, M.; Streekstra, G.; van Rosmalen, J.; Strackee, S.; Hovius, S. Effects of axial load on in vivo scaphoid and lunate kinematics using four-dimensional computed tomography. J. Hand Surg. Eur. Vol. 2020, 45, 974–980. [Google Scholar] [CrossRef]
- Thillemann, J.K.; Dremstrup, L.; Hansen, T.B.; Stilling, M. The mechanical fixation of a cementless conical cup in cortical versus cancellous trapezial bone: An experimental study. J. Hand Surg. Eur. Vol. 2021, 46, 146–153. [Google Scholar] [CrossRef]
- Duerinckx, J.; Perelli, S.; Caekebeke, P. Short report letter: Cortical contact is unnecessary to prevent stem subsidence in cementless trapeziometacarpal arthroplasty. J. Hand Surg. Eur. Vol. 2018, 43, 98–99. [Google Scholar] [CrossRef]
- Kapandji, A. Cotation clinique de l’opposition et de la contre-opposition du pouce. Ann. Chir. Main. 1986, 5, 67–73. [Google Scholar] [CrossRef]
- Brauns, A.; Caekebeke, P.; Duerinckx, J. The effect of cup orientation on stability of trapeziometacarpal total joint arthroplasty: A biomechanical cadaver study. J. Hand Surg. Eur. Vol. 2019, 44, 708–713. [Google Scholar] [CrossRef]
- Bricout, M.; Rezzouk, J. Complications and failures of the trapeziometacarpal Maia® prosthesis: A series of 156 cases. Hand Surg. Rehabil. 2016, 35, 190–198. [Google Scholar] [CrossRef]
- Decot, B.; Manon, J.; Lambeaux, G.; Mathieu, D.; Barbier, O.; Libouton, X. Trapeziometacarpal total joint replacement as an alternative to trapeziectomy depends on trapezium height: Retrospective study of 67 patients. Hand Surg. Rehabil. 2020, 39, 113–119. [Google Scholar] [CrossRef]
- Duerinckx, J.; Caekebeke, P. Trapezium anatomy as a radiographic reference for optimal cup orientation in total trapeziometacarpal joint arthroplasty. J. Hand Surg. Eur. Vol. 2016, 41, 939–943. [Google Scholar] [CrossRef]
- Lussiez, B.; Ledoux, P.; Falaise, C. Prothèse trapèze-métacarpienne à double mobilité: Revue d’une série de 132 cas à plus de 1 an de recul. Rev. Chir. Orthopédique Traumatol. 2017, 103, S61. [Google Scholar] [CrossRef]
- Lussiez, B.; Falaise, C.; Ledoux, P. Dual mobility trapeziometacarpal prosthesis: A prospective study of 107 cases with a follow-up of more than 3 years. J. Hand Surg. Eur. Vol. 2021, 46, 961–967. [Google Scholar] [CrossRef]
- Martin-Ferrero, M. Ten-year long-term results of total joint arthroplasties with ARPE® implant in the treatment of trapeziometacarpal osteoarthritis. J. Hand Surg. Eur. Vol. 2014, 39, 826–832. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holzbauer, M.; Mihalic, J.A.; Gotterbarm, T.; Froschauer, S.M. How a Gauze Sponge Roll Enhances Surgical Exposure in Thumb Carpometacarpal Arthroplasty: A Technical Note. J. Clin. Med. 2024, 13, 6179. https://doi.org/10.3390/jcm13206179
Holzbauer M, Mihalic JA, Gotterbarm T, Froschauer SM. How a Gauze Sponge Roll Enhances Surgical Exposure in Thumb Carpometacarpal Arthroplasty: A Technical Note. Journal of Clinical Medicine. 2024; 13(20):6179. https://doi.org/10.3390/jcm13206179
Chicago/Turabian StyleHolzbauer, Matthias, Julian Alexander Mihalic, Tobias Gotterbarm, and Stefan Mathias Froschauer. 2024. "How a Gauze Sponge Roll Enhances Surgical Exposure in Thumb Carpometacarpal Arthroplasty: A Technical Note" Journal of Clinical Medicine 13, no. 20: 6179. https://doi.org/10.3390/jcm13206179
APA StyleHolzbauer, M., Mihalic, J. A., Gotterbarm, T., & Froschauer, S. M. (2024). How a Gauze Sponge Roll Enhances Surgical Exposure in Thumb Carpometacarpal Arthroplasty: A Technical Note. Journal of Clinical Medicine, 13(20), 6179. https://doi.org/10.3390/jcm13206179





