Psychological Well-Being and Quality of Life in Laryngeal Cancer Patients across Tumor
Abstract
1. Introduction
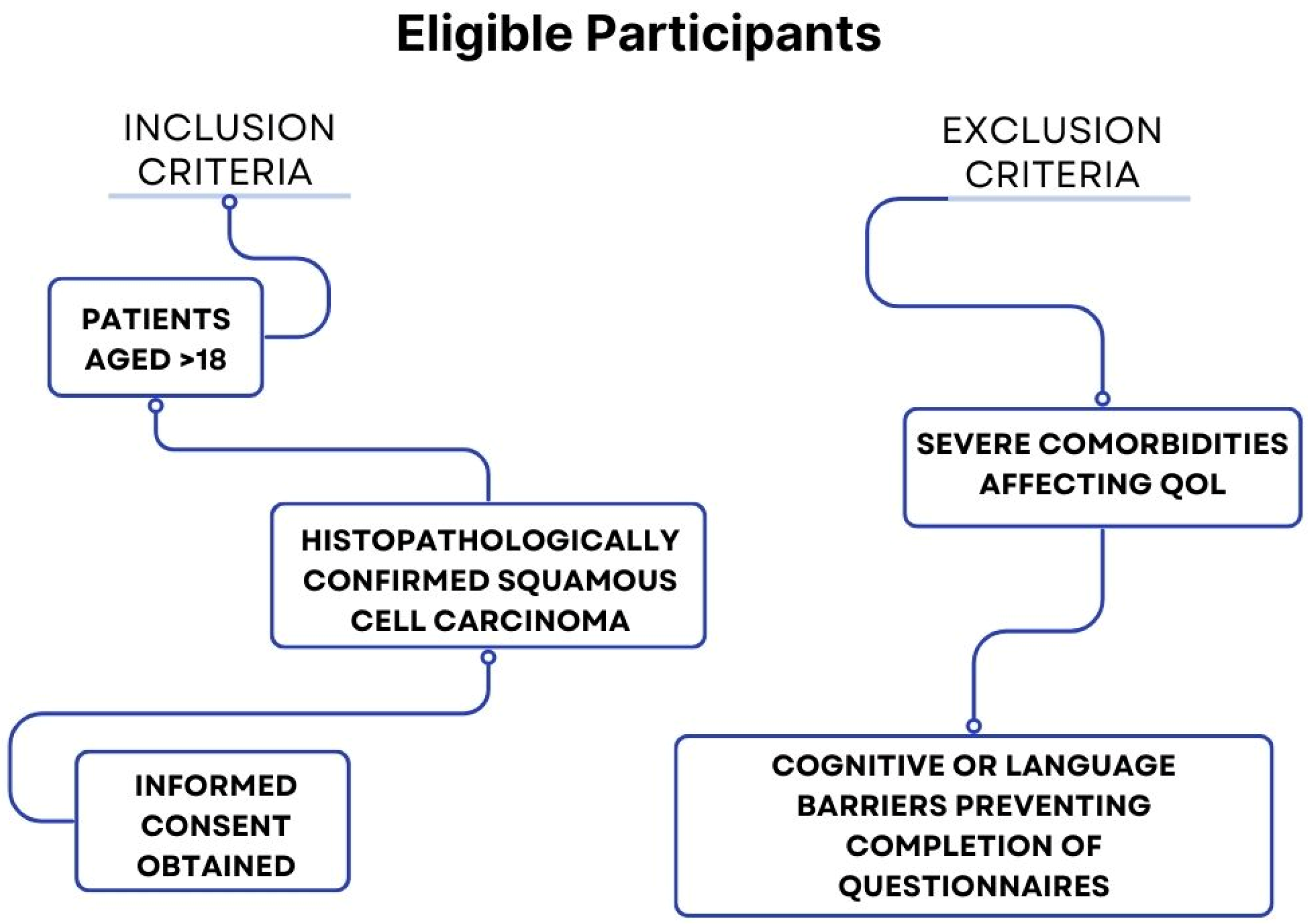
2. Materials and Methods
2.1. Study Design
2.2. Psychological and Quality-of-Life Assessments
- Hospital Anxiety and Depression Scale (HADS): HADS is designed to assess the levels of anxiety and depression in patients. It includes 14 items divided into two subscales: anxiety (HADS-A) and depression (HADS-D). Each item is scored from 0 to 3, resulting in a total score range of 0 to 21 for each subscale. Scores of 0–7 indicate normal levels, no anxiety/depression (A/D), 8–10 suggest mild A/D, 11–14 moderate A/D, and 15–21 represent severe A/D.
- EORTC QLQ-H&N35 (European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Head and Neck 35): This module is specifically designed for head and neck cancer patients and is used alongside the QLQ-C30. It includes 35 items addressing symptoms such as pain, swallowing difficulties, speech problems, and sensory issues. Similar to the QLQ-C30, scores are standardized on a scale from 0 to 100.
2.3. Data Collection Timeline
- Pre-Treatment (at diagnosis): initial assessments were conducted to establish baseline psychological and quality-of-life measures.
- Post-Treatment: follow-up assessments were conducted at 3 months post-treatment to track long-term outcomes and recovery patterns.
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Igissin, N.; Zatonskikh, V.; Telmanova, Z.; Tulebaev, R.; Moore, M. Laryngeal Cancer: Epidemiology, Etiology, and Prevention: A Narrative Review. Iran. J. Public Health 2023, 52, 2248–2259. [Google Scholar] [CrossRef] [PubMed]
- Global Cancer Observatory (GCO). Available online: https://gco.iarc.who.int/media/globocan/factsheets/cancers/14-larynx-fact-sheet.pdf (accessed on 2 September 2024).
- Liberale, C.; Soloperto, D.; Marchioni, A.; Monzani, D.; Sacchetto, L. Updates on Larynx Cancer: Risk Factors and Oncogenesis. Int. J. Mol. Sci. 2023, 24, 12913. [Google Scholar] [CrossRef]
- Chiesa-Estomba, C.M.; Barillari, M.R.; Mayo-Yáñez, M.; Maniaci, A.; Fakhry, N.; Cammaroto, G.; Ayad, T.; Lechien, J.R. Non-Squamous Cell Carcinoma of the Larynx: A State-of-the-Art Review. J. Pers. Med. 2023, 13, 1084. [Google Scholar] [CrossRef]
- Howren, M.B.; Christensen, A.J.; Karnell, L.H.; Funk, G.F. Psychological factors associated with head and neck cancer treatment and survivorship: Evidence and opportunities for behavioral medicine. J. Consult. Clin. Psychol. 2013, 81, 299–317. [Google Scholar] [CrossRef]
- Leano, A.; Korman, M.B.; Goldberg, L.; Ellis, J. Are we missing PTSD in our patients with cancer? Part I. Can. Oncol. Nurs. J. 2019, 29, 141–146. [Google Scholar] [PubMed]
- Bonafede, M.; d’Errico, A.; Rugarli, S.; Mensi, C.; Miligi, L.; Calisti, R.; Della Gatta, R.; Piro, S.; Melis, P.; Vasselli, D.; et al. The psychological impact of diagnosis of sinonasal, nasopharyngeal, and laryngeal cancers: A systematic review. Front. Psychol. 2024, 15, 1355186. [Google Scholar] [CrossRef] [PubMed]
- van Beek, F.E.; Jansen, F.; Baatenburg de Jong, R.J.; Langendijk, J.A.; Leemans, C.R.; Smit, J.H.; Takes, R.P.; Terhaard, C.H.J.; Custers, J.A.E.; Prins, J.B.; et al. Psychological Problems among Head and Neck Cancer Patients in Relation to Utilization of Healthcare and Informal Care and Costs in the First Two Years after Diagnosis. Curr. Oncol. 2022, 29, 3200–3214. [Google Scholar] [CrossRef] [PubMed]
- Heyda, A.; Księżniak-Baran, D.; Wygoda, A.; Składowski, K. Low Post-Treatment Quality of Life and the High Incidence of Pain Are Common and Significantly Exacerbated in Depressed Head and Neck Patients Treated with Definitive Accelerated Radiotherapy. Cancers 2024, 16, 79. [Google Scholar] [CrossRef] [PubMed]
- Mansour, M.; Joseph, G.R.; Joy, G.K.; Khanal, S.; Dasireddy, R.R.; Menon, A.; Barrie Mason, I.; Kataria, J.; Patel, T.; Modi, S. Post-traumatic Stress Disorder: A Narrative Review of Pharmacological and Psychotherapeutic Interventions. Cureus 2023, 15, e44905. [Google Scholar] [CrossRef] [PubMed]
- Williamson, J.S.; Ingrams, D.; Jones, H. Quality of life after treatment of laryngeal carcinoma: A single centre cross-sectional study. Ann. R. Coll. Surg. Engl. 2011, 93, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Brook, I. Late side effects of radiation treatment for head and neck cancer. Radiat. Oncol. J. 2020, 38, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Anschuetz, L.; Shelan, M.; Dematté, M.; Schubert, A.D.; Giger, R.; Elicin, O. Long-term functional outcome after laryngeal cancer treatment. Radiat. Oncol. 2019, 14, 101. [Google Scholar] [CrossRef] [PubMed]
- Sharma, Y.; Mishra, G.; Parikh, V. Quality of Life in Head and Neck Cancer Patients. Indian J. Otolaryngol. Head Neck Surg. 2019, 71, 927–932. [Google Scholar] [CrossRef] [PubMed]
- Gunjawate, D.R.; Ravi, R. Psychosocial Adjustments after Advanced Laryngeal Cancer Treatment—A Systematic Review. Indian J. Palliat. Care 2021, 27, 431–438. [Google Scholar] [CrossRef] [PubMed]
- Muzzatti, B.; Bomben, F.; Flaiban, C.; Piccinin, M.; Annunziata, M.A. Quality of life and psychological distress during cancer: A prospective observational study involving young breast cancer female patients. BMC Cancer 2020, 20, 758. [Google Scholar] [CrossRef] [PubMed]
- Kularatna, S.; Whitty, J.A.; Johnson, N.W.; Jayasinghe, R.; Scuffham, P.A. A comparison of health state utility values associated with oral potentially malignant disorders and oral cancer in Sri Lanka assessed using the EQ-5D-3 L and the EORTC-8D. Health Qual. Life Outcomes 2016, 14, 101. [Google Scholar] [CrossRef] [PubMed]
- Mathew, B. Effectiveness of psychological intervention package on anxiety and wellness level among patients with anxiety disorders. J. Fam. Med. Prim. Care 2022, 11, 6704–6713. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Li, J.; Shi, Y.; Wang, T.; Zhang, A.; Shao, N.; Wang, Z. Psychological intervention improves life quality of patients with laryngeal cancer. Patient Prefer. Adherence 2017, 11, 1723–1727. [Google Scholar] [CrossRef] [PubMed]
- Campbell, G.; Glazer, T.A.; Kimple, R.J.; Bruce, J.Y. Advances in Organ Preservation for Laryngeal Cancer. Curr. Treat. Options Oncol. 2022, 23, 594–608. [Google Scholar] [CrossRef] [PubMed]
| Pre-Treatment | Post-Treatment | ||||||
|---|---|---|---|---|---|---|---|
| Characteristic | Total (N = 75) (%) | HADS-A | HADS-D | EORTC QLQ-H&N35 | HADS-A | HADS-D | EORTC QLQ-H&N35 |
| (Mean ± SD); p-Value | |||||||
| Age | 12.1 ± 3.2; 0.112 | 13.3 ± 3.5; 0.580 | 56.4 ± 7.1; 0.022 | 9.0 ± 2.7; 0.130 | 10.2 ± 3.0; 0.600 | 48.5 ± 6.3; 0.018 | |
| 44–50 | 12 (16%) | 8.9 ± 1.7 | 9.4 ± 2.0 | 45.6 ± 5.1 | 6.3 ± 1.8 | 7.5 ± 2.1 | 39.8 ± 4.9 |
| 51–60 | 20 (26.7%) | 11.2 ± 2.4 | 12.6 ± 2.9 | 53.7 ± 6.2 | 8.8 ± 2.2 | 10.1 ± 2.6 | 45.5 ± 5.4 |
| 61–70 | 28 (37.3%) | 14.5 ± 2.6 | 15.8 ± 3.2 | 62.8 ± 7.3 | 11.5 ± 2.4 | 13.2 ± 2.9 | 56.7 ± 6.9 |
| 71+ | 15 (20%) | 17.3 ± 3.0 | 18.9 ± 3.8 | 72.1 ± 8.5 | 15.1 ± 3.0 | 16.4 ± 3.7 | 65.3 ± 7.8 |
| Gender | |||||||
| Male | 46 (61.3%) | 12.7 ± 2.3; 0.033 | 14.1 ± 2.8; 0.181 | 58.3 ± 6.5; 1.000 | 9.6 ± 2.1; 0.040 | 10.9 ± 2.6; 0.200 | 50.2 ± 5.8; 0.900 |
| Female | 29 (38.7%) | 10.3 ± 2.1; 0.307 | 11.5 ± 2.5; 0.313 | 51.2 ± 5.7; 1.000 | 7.9 ± 2.0; 0.320 | 9.1 ± 2.3; 0.330 | 44.1 ± 5.1; 0.950 |
| Environment | |||||||
| Urban | 49 (65.3%) | 11.5 ± 2.4; 0.053 | 12.8 ± 2.7; 0.961 | 54.1 ± 6.3; 1.000 | 8.7 ± 2.1; 0.050 | 10.2 ± 2.5; 0.950 | 46.7 ± 5.4; 0.980 |
| Rural | 26 (34.7%) | 13.2 ± 2.5; 0.616 | 14.5 ± 3.0; 0.449 | 59.7 ± 7.0; 1.000 | 10.1 ± 2.2; 0.610 | 11.4 ± 2.8; 0.470 | 51.3 ± 6.2; 0.990 |
| Tumor Stage | |||||||
| Stage I | 13 (17.3%) | 7.5 ± 1.8; 0.003 | 8.2 ± 2.1; 0.004 | 40.5 ± 5.3; 0.005 | 5.2 ± 1.5; 0.010 | 6.4 ± 2.0; 0.015 | 35.2 ± 4.7; 0.008 |
| Stage II | 26 (34.7%) | 10.4 ± 2.3; 0.050 | 11.0 ± 2.9; 0.045 | 50.3 ± 6.7; 0.060 | 8.3 ± 2.1; 0.055 | 9.0 ± 2.5; 0.050 | 42.8 ± 5.4; 0.065 |
| Stage III | 29 (38.7%) | 14.1 ± 2.5; 0.200 | 15.5 ± 3.2; 0.150 | 60.7 ± 7.8; 0.180 | 12.2 ± 2.4; 0.210 | 13.8 ± 2.8; 0.160 | 55.3 ± 7.1; 0.190 |
| Stage IV | 7 (9.3%) | 18.9 ± 3.1; 0.450 | 20.3 ± 4.1; 0.300 | 75.6 ± 9.3; 0.400 | 16.7 ± 3.0; 0.460 | 18.5 ± 3.9; 0.320 | 68.4 ± 8.6; 0.420 |
| Treatment Type | |||||||
| Total Laryngectomy | 20 (26.7%) | 12.4 ± 2.3; 0.050 | 13.7 ± 2.8; 0.180 | 58.2 ± 6.5; 0.020 | 9.1 ± 2.0; 0.045 | 10.5 ± 2.6; 0.190 | 48.7 ± 5.3; 0.018 |
| Partial Laryngectomy | 15 (20.0%) | 10.2 ± 2.1; 0.065 | 11.4 ± 2.5; 0.220 | 50.4 ± 5.8; 0.025 | 7.8 ± 1.9; 0.060 | 8.9 ± 2.3; 0.230 | 42.3 ± 5.0; 0.022 |
| Laser Cordectomy | 10 (13.3%) | 8.7 ± 1.9; 0.080 | 9.6 ± 2.2; 0.240 | 45.3 ± 5.0; 0.030 | 6.5 ± 1.8; 0.075 | 7.5 ± 2.1; 0.250 | 38.9 ± 4.5; 0.028 |
| Radiotherapy | 15 (20.0%) | 11.5 ± 2.4; 0.070 | 12.8 ± 2.7; 0.200 | 55.1 ± 6.3; 0.035 | 8.7 ± 2.1; 0.065 | 10.2 ± 2.5; 0.210 | 47.4 ± 5.7; 0.032 |
| Chemoradiotherapy | 15 (20.0%) | 13.9 ± 2.7; 0.055 | 15.3 ± 3.1; 0.190 | 62.5 ± 7.2; 0.040 | 10.5 ± 2.3; 0.050 | 12.1 ± 2.9; 0.200 | 54.6 ± 6.8; 0.038 |
| Measure | Pre-Treatment (Mean ± SD) | Post-Treatment (Mean ± SD) | p-Value |
|---|---|---|---|
| HADS-A (Anxiety) | 8.426 ± 3.120 | 6.870 ± 3.050 | 0.015 |
| HADS-D (Depression) | 10.960 ± 4.723 | 8.450 ± 4.570 | 0.022 |
| EORTC QLQ-H&N35 | 61.600 ± 25.791 | 55.200 ± 24.503 | 0.030 |
| Stage | Treatment Type | Total n (%) | HADS-A Pre (Mean ± SD) | HADS-D Pre (Mean ± SD) | EORTC QLQ-H&N35 Pre (Mean ± SD) | HADS-A Post (Mean ± SD) | HADS-D Post (Mean ± SD) | EORTC QLQ-H&N35 Post (Mean ± SD) |
|---|---|---|---|---|---|---|---|---|
| Stage I | Radiotherapy | 10 (13.3%) | 8.5 ± 1.7 | 9.2 ± 2.0 | 45.2 ± 5.4 | 6.1 ± 1.6 | 7.1 ± 1.9 | 38.9 ± 4.9 |
| Stage I | Partial Laryngectomy | 5 (6.7%) | 8.1 ± 1.8 | 8.9 ± 1.9 | 44.1 ± 5.2 | 6.5 ± 1.7 | 7.3 ± 2.0 | 39.5 ± 5.0 |
| Stage I | Laser Surgery | 3 (4.0%) | 7.8 ± 1.5 | 8.7 ± 1.8 | 42.9 ± 4.9 | 6.3 ± 1.5 | 7.0 ± 1.8 | 37.8 ± 4.6 |
| Stage II | Radiotherapy | 8 (10.7%) | 10.2 ± 2.0 | 11.1 ± 2.5 | 51.2 ± 5.8 | 8.0 ± 2.1 | 9.1 ± 2.3 | 43.7 ± 5.5 |
| Stage II | Partial Laryngectomy | 7 (9.3%) | 10.0 ± 2.1 | 10.7 ± 2.4 | 50.8 ± 6.0 | 7.8 ± 2.0 | 8.9 ± 2.1 | 42.5 ± 5.2 |
| Stage II | Laser Surgery | 5 (6.7%) | 9.7 ± 2.0 | 10.5 ± 2.3 | 49.5 ± 5.6 | 7.6 ± 1.9 | 8.7 ± 2.0 | 41.9 ± 5.0 |
| Stage III | Total Laryngectomy | 12 (16.0%) | 13.9 ± 2.6 | 14.9 ± 3.1 | 61.4 ± 6.8 | 11.3 ± 2.4 | 12.5 ± 2.9 | 55.0 ± 6.3 |
| Stage III | Chemoradiotherapy | 10 (13.3%) | 14.1 ± 2.7 | 15.1 ± 3.3 | 60.8 ± 6.9 | 11.5 ± 2.5 | 12.7 ± 2.9 | 54.5 ± 6.5 |
| Stage IV | Total Laryngectomy | 10 (13.3%) | 17.2 ± 3.1 | 18.8 ± 3.6 | 71.8 ± 8.0 | 14.5 ± 2.9 | 16.3 ± 3.5 | 66.0 ± 7.5 |
| Stage IV | Chemoradiotherapy | 15 (20.0%) | 17.5 ± 3.0 | 19.0 ± 3.8 | 70.9 ± 7.9 | 14.7 ± 3.0 | 16.5 ± 3.7 | 65.2 ± 7.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murariu, M.O.; Boia, E.R.; Horhat, D.I.; Mot, C.I.; Balica, N.C.; Trebuian, C.I.; Brici, A.C.; Zahoi, D.E. Psychological Well-Being and Quality of Life in Laryngeal Cancer Patients across Tumor. J. Clin. Med. 2024, 13, 6138. https://doi.org/10.3390/jcm13206138
Murariu MO, Boia ER, Horhat DI, Mot CI, Balica NC, Trebuian CI, Brici AC, Zahoi DE. Psychological Well-Being and Quality of Life in Laryngeal Cancer Patients across Tumor. Journal of Clinical Medicine. 2024; 13(20):6138. https://doi.org/10.3390/jcm13206138
Chicago/Turabian StyleMurariu, Maria Octavia, Eugen Radu Boia, Delia Ioana Horhat, Cristian Ion Mot, Nicolae Constantin Balica, Cosmin Iosif Trebuian, Alexandru Cristian Brici, and Delia Elena Zahoi. 2024. "Psychological Well-Being and Quality of Life in Laryngeal Cancer Patients across Tumor" Journal of Clinical Medicine 13, no. 20: 6138. https://doi.org/10.3390/jcm13206138
APA StyleMurariu, M. O., Boia, E. R., Horhat, D. I., Mot, C. I., Balica, N. C., Trebuian, C. I., Brici, A. C., & Zahoi, D. E. (2024). Psychological Well-Being and Quality of Life in Laryngeal Cancer Patients across Tumor. Journal of Clinical Medicine, 13(20), 6138. https://doi.org/10.3390/jcm13206138







