Radical Cystectomy with Ileal Orthotopic Neobladder after 70 Years Leads to Worse Health-Related Quality of Life
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Selection Criteria
2.2. Data Collection and Follow-Up
2.3. Primary Outcome and Statistical Analysis
3. Results
3.1. Baseline Characteristics
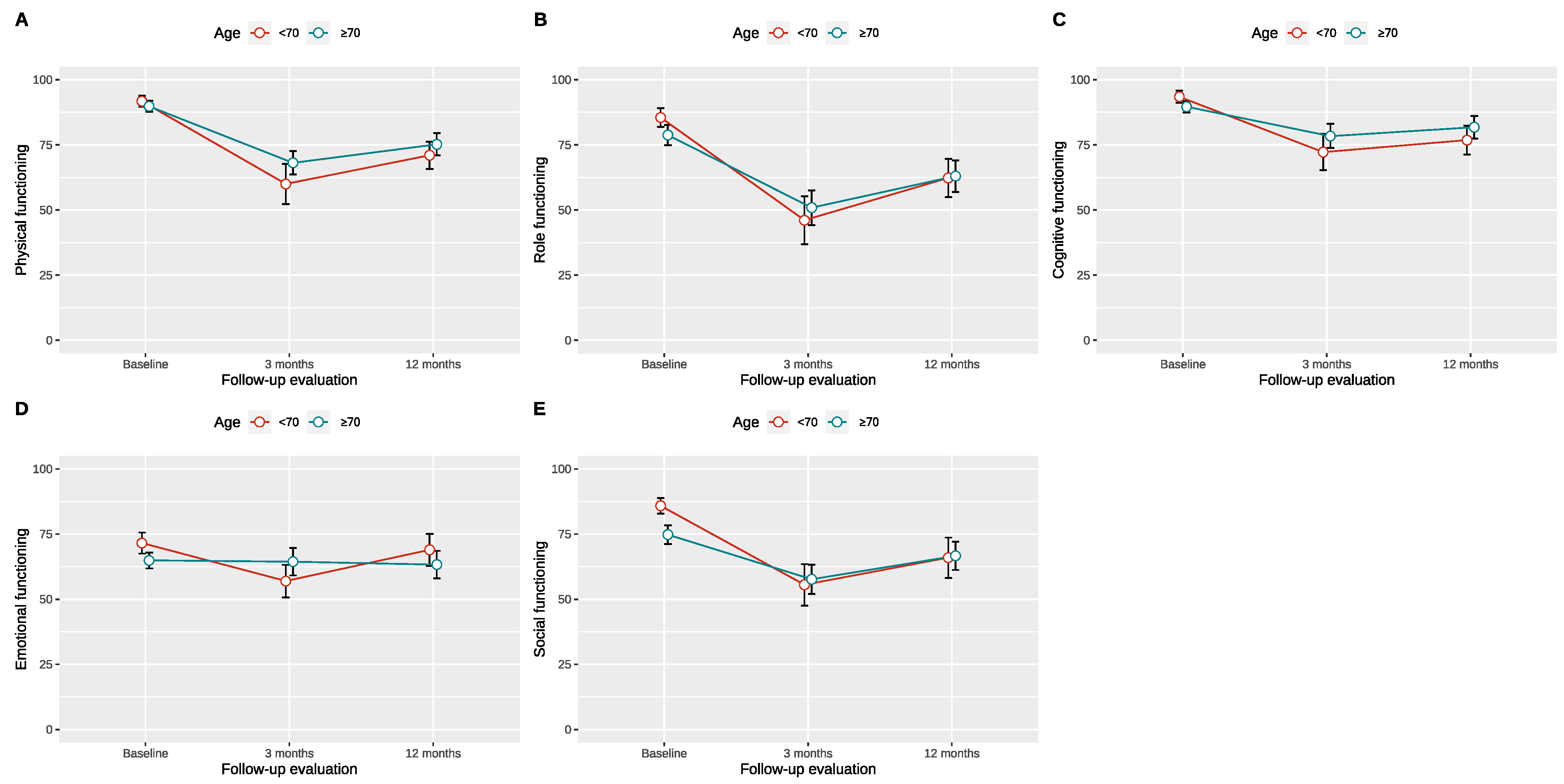
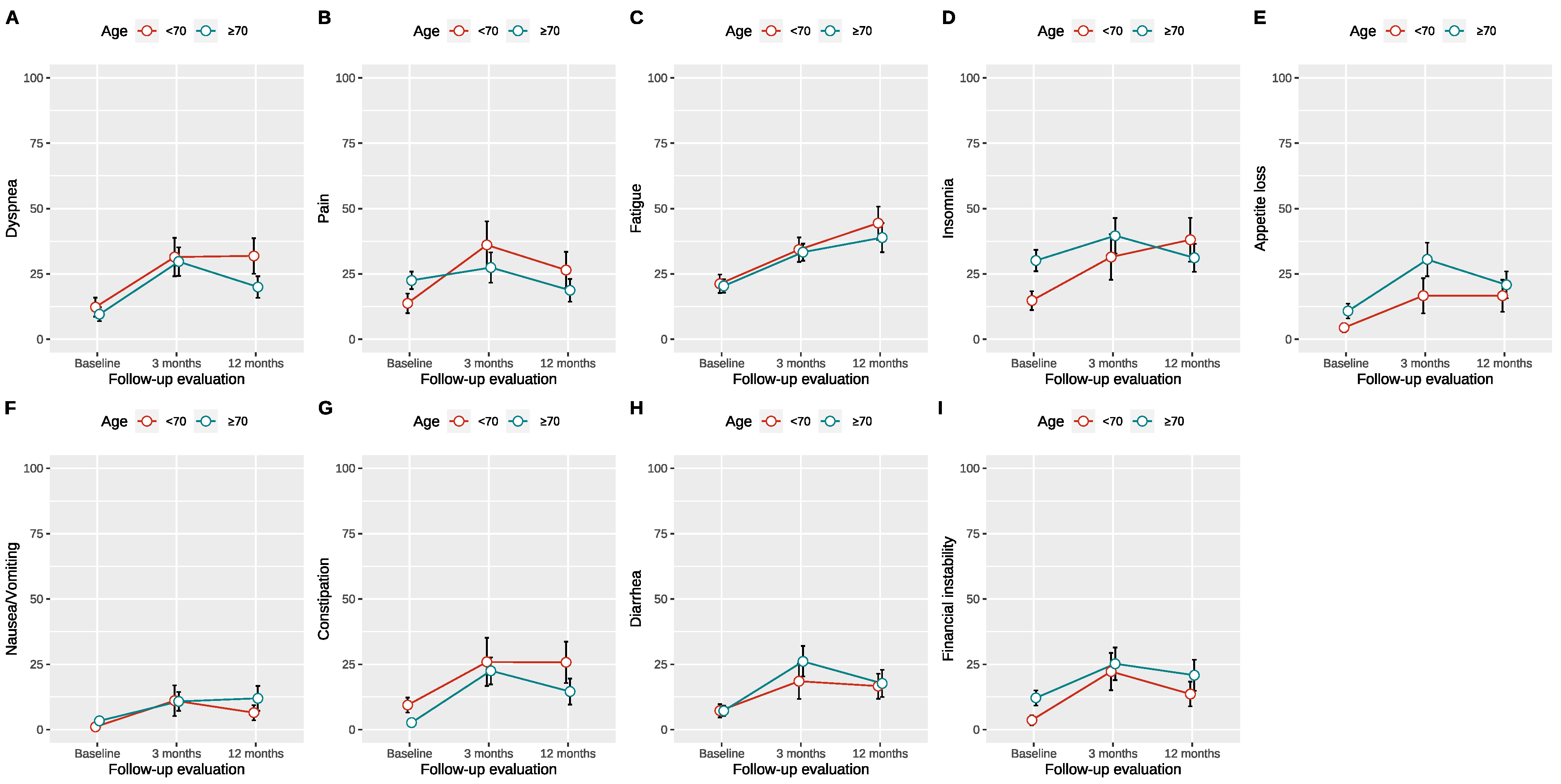
3.2. Health-Related Quality of Life over Time
3.3. Threshold of Age at the Time of Surgery for a Reduced HRQOL
3.4. Health-Related Quality of Life Outcomes Based on the Age Threshold
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Richters, A.; Aben, K.K.H.; Kiemeney, L.A.L.M. The global burden of urinary bladder cancer: An update. World J. Urol. 2020, 38, 1895–1904. [Google Scholar] [CrossRef] [PubMed]
- Pyrgidis, N.; Volz, Y.; Ebner, B.; Kazmierczak, P.M.; Enzinger, B.; Hermans, J.; Buchner, A.; Stief, C.; Schulz, G.B. The effect of hospital caseload on perioperative mortality, morbidity and costs in bladder cancer patients undergoing radical cystectomy: Results of the German nationwide inpatient data. World J. Urol. 2024, 42, 19. [Google Scholar] [CrossRef] [PubMed]
- Klemm, J.; Fisch, M.; Laukhtina, E.; Dahlem, R.; Shariat, S.F.; Vetterlein, M.W. Continent diversion is losing its momentum: A nationwide trend analysis from Germany 2005–2021. BJU Int. 2024, 133, 154–157. [Google Scholar] [CrossRef]
- Pyrgidis, N.; Sokolakis, I.; Haltmair, G.; Hatzichristodoulou, G. The Short- and Long-Term Effect of Radical Cystectomy in Frail Patients With Bladder Cancer. Clin. Genitourin. Cancer 2023, 21, e291–e298. [Google Scholar] [CrossRef] [PubMed]
- Cerruto, M.A.; D’Elia, C.; Siracusano, S.; Gedeshi, X.; Mariotto, A.; Iafrate, M.; Niero, M.; Lonardi, C.; Bassi, P.; Belgrano, E.; et al. Systematic review and meta-analysis of non RCT’s on health related quality of life after radical cystectomy using validated questionnaires: Better results with orthotopic neobladder versus ileal conduit. Eur. J. Surg. Oncol. 2016, 42, 343–360. [Google Scholar] [CrossRef]
- Volz, Y.; Eismann, L.; Pfitzinger, P.; Westhofen, T.; Ebner, B.; Jokisch, J.-F.; Buchner, A.; Schulz, G.; Schlenker, B.; Karl, A.; et al. Long-term Health-related Quality of Life (HRQOL) After Radical Cystectomy and Urinary Diversion—A Propensity Score-matched Analysis. Clin. Genitourin. Cancer 2022, 20, e283–e290. [Google Scholar] [CrossRef]
- Pyrgidis, N.; Sokolakis, I.; Haltmair, G.; Hatzichristodoulou, G. The effect of urinary diversion on renal function after cystectomy for bladder cancer: Comparison between ileal conduit, orthotopic ileal neobladder, and heterotopic ileocecal pouch. World J. Urol. 2022, 40, 3091–3097. [Google Scholar] [CrossRef] [PubMed]
- Berger, I.; Martini, T.; Wehrberger, C.; Comploj, E.; Ponholzer, A.; Wolfgang, M.; Breinl, E.; Dunzinger, M.; Hofbauer, J.; Höltl, W.; et al. Perioperative complications and 90-day mortality of radical cystectomy in the elderly (75+): A retrospective, multicentre study. Urol. Int. 2014, 9, 296–302. [Google Scholar] [CrossRef]
- Witjes, J.A.; Bruins, H.M.; Cathomas, R.; Compérat, E.M.; Cowan, N.C.; Gakis, G.; Hernández, V.; Espinós, E.L.; Lorch, A.; Neuzillet, Y.; et al. European Association of Urology Guidelines on Muscle-invasive and Metastatic Bladder Cancer: Summary of the 2020 Guidelines. Eur. Urol. 2021, 79, 82–104. [Google Scholar] [CrossRef]
- Cerruto, M.A.; D’Elia, C.; Siracusano, S.; Saleh, O.; Gacci, M.; Cacciamani, G.; De Marco, V.; Porcaro, A.B.; Balzarro, M.; Niero, M.; et al. Health-Related Quality of Life after Radical Cystectomy for Bladder Cancer in Elderly Patients with Ileal Orthotopic Neobladder or Ileal Conduit: Results from a Multicentre Cross-Sectional Study Using Validated Questionnaires. Urol. Int. 2018, 100, 346–352. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; De Haes, J.C.J.M.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30, a quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Shariat, S.F.; Sfakianos, J.P.; Droller, M.J.; Karakiewicz, P.I.; Meryn, S.; Bochner, B.H. The effect of age and gender on bladder cancer: A critical review of the literature. BJU Int. 2010, 105, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.S.; Bochner, B.H.; Chou, R.; Dreicer, R.; Kamat, A.M.; Lerner, S.P.; Lotan, Y.; Meeks, J.J.; Michalski, J.M.; Morgan, T.M.; et al. Treatment of Non-Metastatic Muscle-Invasive Bladder Cancer: AUA/ASCO/ASTRO/SUO Guideline. J. Urol. 2017, 198, 552–559. [Google Scholar] [CrossRef]
- Imbimbo, C.; Mirone, V.; Siracusano, S.; Niero, M.; Cerruto, M.A.; Lonardi, C.; Artibani, W.; Bassi, P.; Iafrate, M.; Racioppi, M.; et al. Quality of Life Assessment With Orthotopic Ileal Neobladder Reconstruction After Radical Cystectomy: Results From a Prospective Italian Multicenter Observational Study. Urology 2015, 86, 974–979. [Google Scholar] [CrossRef] [PubMed]
- Crozier, J.; Hennessey, D.; Sengupta, S.; Bolton, D.; Lawrentschuk, N. A Systematic Review of Ileal Conduit and Neobladder Outcomes in Primary Bladder Cancer. Urology 2016, 96, 74–79. [Google Scholar] [CrossRef]
- Yang, L.S.; Shan, B.L.; Shan, L.L.; Chin, P.; Murray, S.; Ahmadi, N.; Saxena, A. A systematic review and meta-analysis of quality of life outcomes after radical cystectomy for bladder cancer. Surg. Oncol. 2016, 25, 281–297. [Google Scholar] [CrossRef]
- Kretschmer, A.; Grimm, T.; Buchner, A.; Stief, C.G.; Karl, A. Prognostic features for quality of life after radical cystectomy and orthotopic neobladder. Int. Braz. J. Urol. 2016, 42, 1109–1120. [Google Scholar] [CrossRef]
- Kretschmer, A.; Grimm, T.; Buchner, A.; Jokisch, F.; Ziegelmüller, B.; Casuscelli, J.; Schulz, G.; Stief, C.G.; Karl, A. Midterm Health-related Quality of Life After Radical Cystectomy: A Propensity Score-matched Analysis. Eur. Urol. Focus 2020, 6, 704–710. [Google Scholar] [CrossRef]
- Novara, G.; Ficarra, V.; Minja, A.; De Marco, V.; Artibani, W. Functional results following vescica ileale Padovana (VIP) neobladder: Midterm follow-up analysis with validated questionnaires. Eur. Urol. 2010, 57, 1045–1051. [Google Scholar] [CrossRef]
- Veskimäe, E.; Neuzillet, Y.; Rouanne, M.; MacLennan, S.; Lam, T.B.L.; Yuan, Y.; Compérat, E.; Cowan, N.C.; Gakis, G.; van der Heijden, A.G.; et al. Systematic review of the oncological and functional outcomes of pelvic organ-preserving radical cystectomy (RC) compared with standard RC in women who undergo curative surgery and orthotopic neobladder substitution for bladder cancer. BJU Int. 2017, 120, 12–24. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Overall, n = 120 | Increase in GHS, n = 80 | Decrease in GHS, n = 40 | p-Value |
|---|---|---|---|---|
| Male | 97 (81%) | 65 (81%) | 32 (80%) | >0.99 |
| Age (years) | 66 ± 9.6 | 66 ± 9.7 | 66 ± 9.6 | >0.99 |
| BMI (kg/m2) | 27 ± 4.3 | 27 ± 4.3 | 27 ± 4.3 | 0.63 |
| Smokers | 75 (65%) | 47 (61%) | 28 (72%) | 0.35 |
| Alcohol consumption | 48 (41%) | 30 (38%) | 18 (46%) | 0.55 |
| Hypertension | 54 (45%) | 37 (46%) | 17 (43%) | 0.85 |
| Diabetes | 33 (28%) | 16 (20%) | 17 (43%) | 0.017 |
| Coronary heart disease | 18 (15%) | 12 (15%) | 6 (15%) | >0.99 |
| ASA score | 0.23 | |||
| 1 | 4 (3.4%) | 2 (2.5%) | 2 (5.3%) | |
| 2 | 40 (34%) | 31 (39%) | 9 (24%) | |
| 3 | 74 (63%) | 47 (59%) | 27 (71%) | |
| Operative time (minutes) | 222 ± 53 | 222 ± 52 | 222 ± 55 | >0.99 |
| Blood loss (ml) | 417 ± 367 | 401 ± 370 | 449 ± 365 | 0.5 |
| Histology | 54 (45%) | 37 (46%) | 17 (43%) | 0.85 |
| Urothelial cancer | 113 (95%) | 73 (92%) | 40 (100%) | |
| Variant histology | 6 (5%) | 6 (7.6%) | 0 (0%) | |
| T after cystectomy | 0.94 | |||
| ≤T2 | 86 (72%) | 58 (73%) | 28 (70%) | |
| ≥T3 | 34 (28%) | 22 (28%) | 12 (30%) | |
| Positive lymph nodes | 18 (16%) | 13 (17%) | 5 (13%) | 0.82 |
| Clavien–Dindo complications | 0.3 | |||
| 1 | 2 (9.5%) | 2 (12%) | 0 (0%) | |
| 2 | 8 (38%) | 5 (29%) | 3 (75%) | |
| 3 | 5 (24%) | 4 (24%) | 1 (25%) | |
| 4 | 6 (29%) | 6 (35%) | 0 (0%) | |
| Hospital stay (days) | 21 ± 6.4 | 21 ± 6.2 | 22 ± 6.8 | 0.55 |
| GHS preoperatively | 64 ± 23 | 58 ± 24 | 76 ± 16 | <0.001 |
| GHS 3 months | 64 ± 20 | 67 ± 19 | 57 ± 22 | 0.045 |
| GHS 12 months | 68 ± 23 | 77 ± 16 | 50 ± 26 | <0.001 |
| Characteristic | Overall, n = 120 | Increase in GHS, n = 80 | Decrease in GHS, n = 40 | p-Value |
|---|---|---|---|---|
| ICIQ Score | 9.0 ± 6.4 | 7.5 ± 6 | 12.2 ± 6.1 | <0.001 |
| Patients with incontinence (≥1 pad/day) | 100 (84%) | 63 (79%) | 37 (95%) | 0.047 |
| Characteristic | Age ≥ 70, n = 46 | Age < 70, n = 74 | p-Value |
|---|---|---|---|
| Male | 39 (85%) | 58 (78%) | 0.53 |
| Age (years) | 75.3 ± 3.1 | 60.5 ± 7.7 | <0.001 |
| BMI (kg/m2) | 26.4 ± 4.1 | 27.0 ± 4.4 | 0.50 |
| Smokers | 32 (71%) | 43 (61%) | 0.34 |
| Alcohol consumption | 22 (50%) | 26 (36%) | 0.18 |
| Hypertension | 25 (54%) | 29 (39%) | 0.15 |
| Diabetes | 15 (33%) | 18 (24%) | 0.44 |
| Coronary heart disease | 13 (28%) | 5 (6.8%) | 0.003 |
| ASA score | 0.018 | ||
| 1 | 0 (0%) | 4 (5.5%) | |
| 2 | 10 (22%) | 30 (41%) | |
| 3 | 35 (78%) | 39 (53%) | |
| Operative time (minutes) | 209.1 ± 47.5 | 229.8 ± 54.9 | 0.033 |
| Blood loss (ml) | 435.6 ± 447.3 | 404.8 ± 310.5 | 0.69 |
| Histology | 0.12 | ||
| Urothelial cancer | 46 (100%) | 67 (92%) | |
| Variant histology | 0 (0%) | 6 (8.2%) | |
| T after cystectomy | >0.99 | ||
| ≤T2 | 33 (72%) | 53 (72%) | |
| ≥T3 | 13 (28%) | 21 (28%) | |
| Positive lymph nodes | 5 (11%) | 13 (18%) | 0.39 |
| Clavien–Dindo complications | 0.40 | ||
| 1 | 1 (10%) | 1 (9.1%) | |
| 2 | 3 (30%) | 5 (45%) | |
| 3 | 4 (40%) | 1 (9.1%) | |
| 4 | 2 (20%) | 4 (36%) | |
| Hospital stay (days) | 22.4 ± 7.0 | 20.5 ± 6.0 | 0.14 |
| ICIQ 12 months | 10.4 ± 6.9 | 8.1 ± 5.9 | 0.068 |
| Functioning Scores | Overall, n = 120 | Age ≥ 70, n = 46 | Age < 70, n = 74 | p-Value |
|---|---|---|---|---|
| Physical functioning | −16.6 ± 29.5 | −19.1 ± 31.2 | −14.8 ± 28.6 | 0.6 |
| Role functioning | −15.2 ± 41.1 | −25.4 ± 40.8 | −7.8 ± 40.4 | 0.12 |
| Social functioning | −13.0 ± 38.1 | −22.7 ± 44.4 | −6.3 ± 32.2 | 0.14 |
| Cognitive functioning | 13.0 ± 30.2 | 18.8 ± 30.7 | 8.9 ± 29.6 | 0.23 |
| Emotional functioning | 27.0 ± 30.8 | 26.5 ± 30.9 | 27.3 ± 31.2 | 0.92 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pyrgidis, N.; Schulz, G.B.; Ebner, B.; Jokisch, F.; Eismann, L.; Karatas, D.; Fouladgar, S.T.; Hermans, J.; Keller, P.; Stief, C.; et al. Radical Cystectomy with Ileal Orthotopic Neobladder after 70 Years Leads to Worse Health-Related Quality of Life. J. Clin. Med. 2024, 13, 6102. https://doi.org/10.3390/jcm13206102
Pyrgidis N, Schulz GB, Ebner B, Jokisch F, Eismann L, Karatas D, Fouladgar ST, Hermans J, Keller P, Stief C, et al. Radical Cystectomy with Ileal Orthotopic Neobladder after 70 Years Leads to Worse Health-Related Quality of Life. Journal of Clinical Medicine. 2024; 13(20):6102. https://doi.org/10.3390/jcm13206102
Chicago/Turabian StylePyrgidis, Nikolaos, Gerald Bastian Schulz, Benedikt Ebner, Friedrich Jokisch, Lennert Eismann, Deniz Karatas, Sarah Takayama Fouladgar, Julian Hermans, Patrick Keller, Christian Stief, and et al. 2024. "Radical Cystectomy with Ileal Orthotopic Neobladder after 70 Years Leads to Worse Health-Related Quality of Life" Journal of Clinical Medicine 13, no. 20: 6102. https://doi.org/10.3390/jcm13206102
APA StylePyrgidis, N., Schulz, G. B., Ebner, B., Jokisch, F., Eismann, L., Karatas, D., Fouladgar, S. T., Hermans, J., Keller, P., Stief, C., & Volz, Y. (2024). Radical Cystectomy with Ileal Orthotopic Neobladder after 70 Years Leads to Worse Health-Related Quality of Life. Journal of Clinical Medicine, 13(20), 6102. https://doi.org/10.3390/jcm13206102






