Continence Is Not Affected after Sling Revision with Transvaginal Tape Elongation for Post-Sling Voiding Dysfunction
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Clinical Assessment
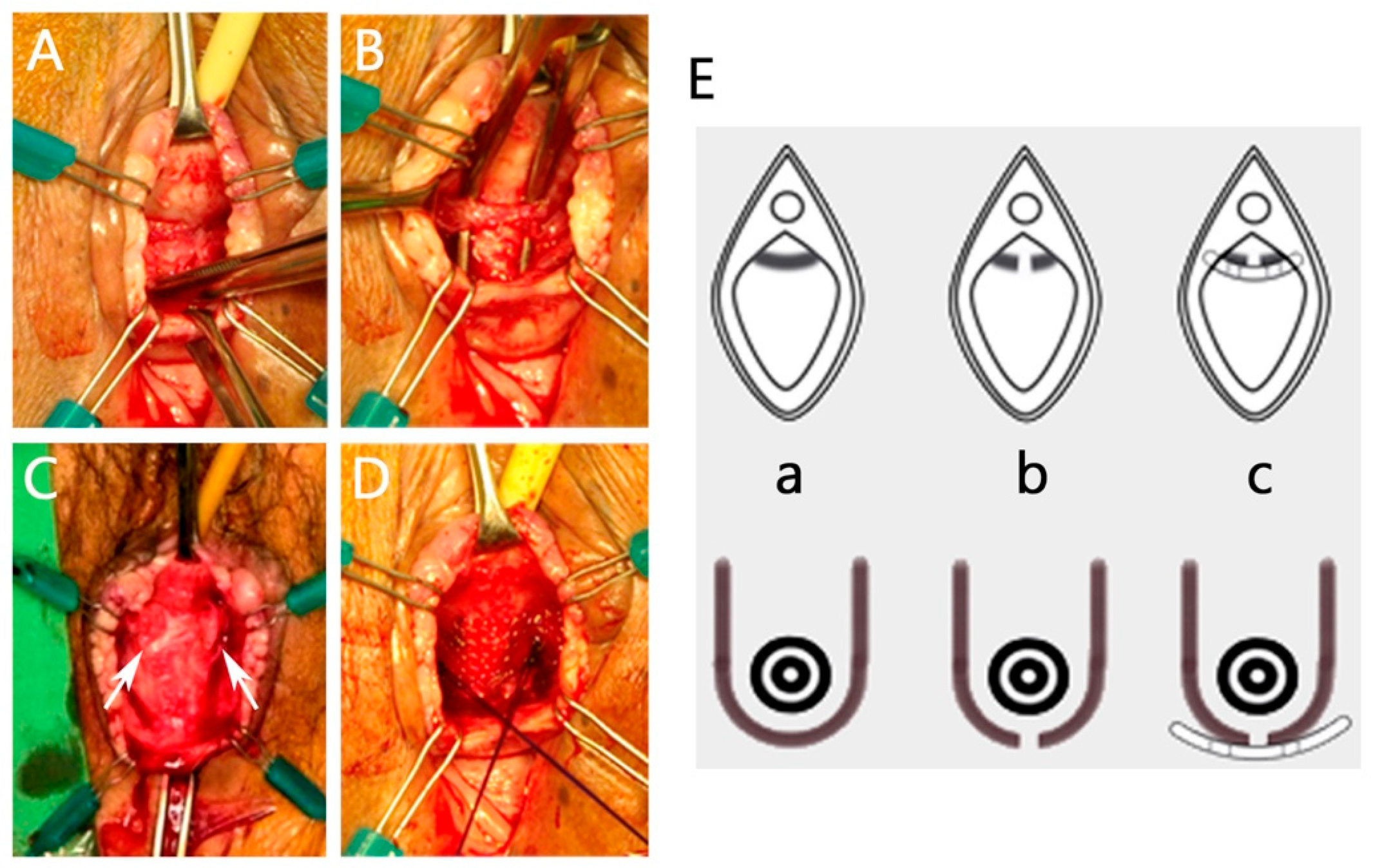
2.3. Surgical Intervention
2.4. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
3.2. Surgical Results
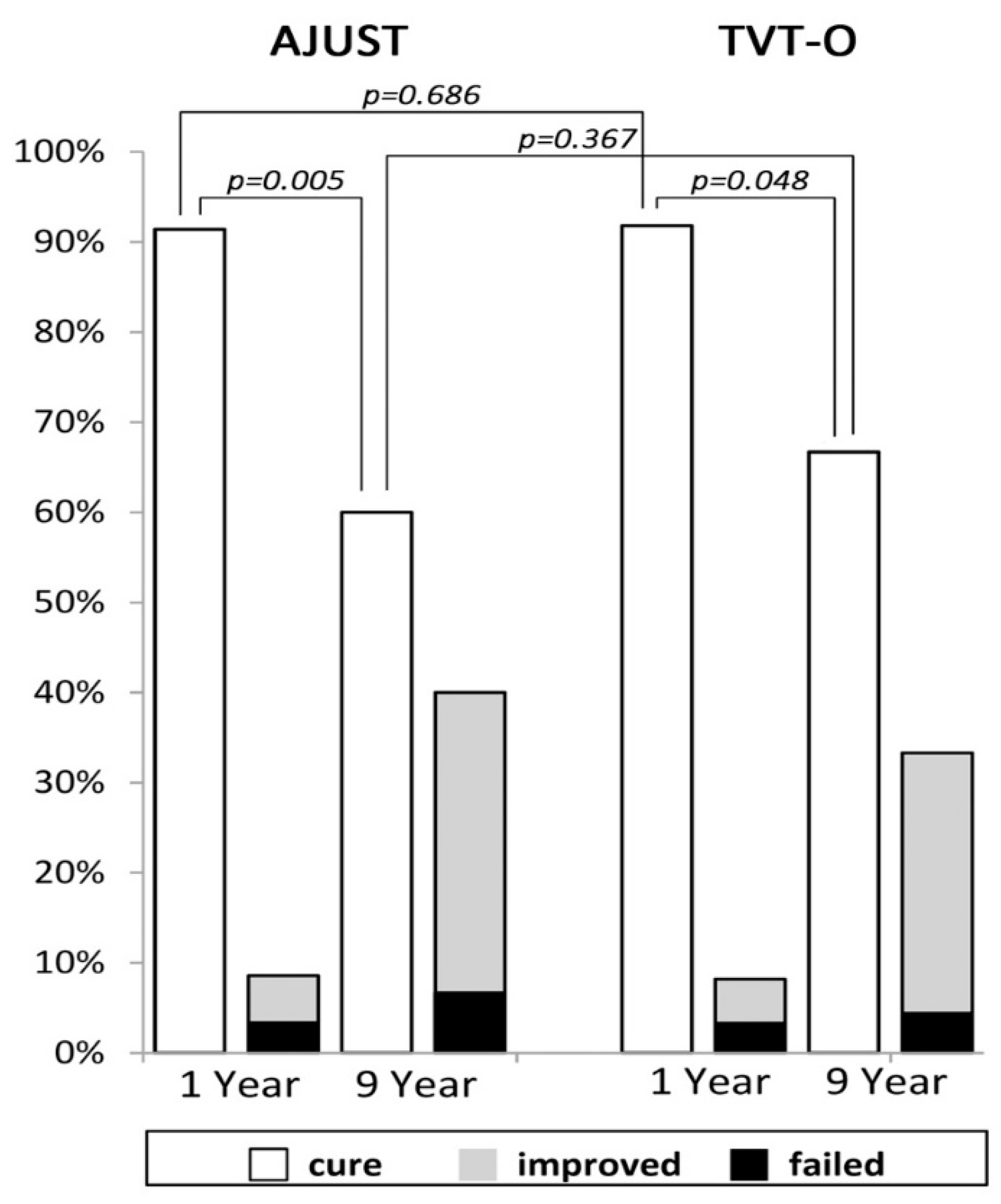
3.3. Long-Term Continence Outcome
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jonsson Funk, M.; Levin, P.J.; Wu, J.M. Trends in the surgical management of stress urinary incontinence. Obstet. Gynecol. 2012, 119, 845–851. [Google Scholar] [CrossRef]
- Urogynecologic Surgical Mesh Update on the Safety and Effectiveness of Transvaginal Placement for Pelvic Organ Prolapse. Available online: https://www.fda.gov/medical-devices/urogynecologic-surgical-mesh-implants/fdas-activities-urogynecologic-surgical-mesh (accessed on 2 January 2024).
- Lo, T.-S.; Tan, Y.L. Use of vaginal mesh; an Asian perspective footnote from the pan-Asia meeting. Int. Urogynecol. J. 2020, 31, 675–677. [Google Scholar] [CrossRef]
- Devan, W.J.; Rodriguez, D.; Munarriz, R.; Ng, L.; Bose, S. Would Surgeons opt for Polypropylene Mesh if They Hypothetically Had Stress Urinary Incontinence or Pelvic Organ Prolapse? Urol. Pract. 2022, 9, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Goldman, H.B. Joint position statement on midurethral slings for stress urinary incontinence. Neurourol. Urodyn. 2022, 41, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Malacarne, D.R.; Nitti, V.W. Post-sling urinary retention in women. Curr. Urol. Rep. 2016, 17, 83. [Google Scholar] [CrossRef]
- Tran, H.; Rutman, M. Female Outlet Obstruction After Anti-Incontinence Surgery. Urology 2018, 112, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Bazi, T.; Kerkhof, M.H.; Takahashi, S.I.; Abdel-Fattah, M.; IUGA Research and Development Committee. Management of post-midurethral sling voiding dysfunction. International Urogynecological Association research and development committee opinion. Int. Urogynecol. J. 2018, 29, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Peyronnet, B.; Lapitan, M.C.; Tzelves, L.; O’Connor, E.; Nic An Riogh, A.; Manso, M.; Yuhong Yuan, C.; Arlandis, S.; Bo, K.; Costantini, E.; et al. Benefits and Harms of Conservative, Pharmacological, and Surgical Management Options for Women with Bladder Outlet Obstruction: A Systematic Review from the European Association of Urology Non-neurogenic Female LUTS Guidelines Panel. Eur. Urol. Focus 2022, 8, 1340–1361. [Google Scholar] [CrossRef]
- Hsiao, S.M.; Kuo, H.C. Predictors of further anti-incontinence interventions or transvaginal urethrolysis after a pubovaginal sling procedure in women with and without neurologic disorders. J. Formos. Med. Assoc. 2021, 120, 1464–1477. [Google Scholar] [CrossRef]
- South, M.M.T.; Wu, J.M.; Webster, G.D.; Weidner, A.C.; Roelands, J.J.; Amundsen, C.L. Early vs. late midline sling lysis results in greater improvement in lower urinary tract symptoms. Am. J. Obstet. Gynecol. 2009, 200, 564.e1–564.e5. [Google Scholar] [CrossRef]
- Crescenze, I.M.; Abraham, N.; Li, J.; Goldman, H.B.; Vasavada, S. Urgency Incontinence before and after Revision of a Synthetic Mid Urethral Sling. J. Urol. 2016, 196, 478–483. [Google Scholar] [CrossRef]
- Ross, J.; Avvakoumova, L.; Yassein, A.; Payne, M.; Maciejewski, C.; Mallick, R.; Breau, R.H.; Vigil, H.; Hickling, D. Prevalence and Predictors of Bladder Outlet Obstruction in Women with Chronic Urinary Symptoms and a History of Urethral Sling Surgery. J. Urol. 2023, 209, 384–390. [Google Scholar] [CrossRef]
- Rodrigues, P.; Hering, F.; Dias, E.C. Female obstruction after incontinence surgery may present different urodynamic patterns. Int. Urogynecol. J. 2013, 24, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Aponte, M.M.; Shah, S.R.; Hickling, D.; Brucker, B.M.; Rosenblum, N.; Nitti, V.W. Urodynamics for clinically suspected obstruction after anti-incontinence surgery in women. J. Urol. 2013, 190, 598–602. [Google Scholar] [CrossRef] [PubMed]
- Karram, M.M.; Segal, J.L.; Vassallo, B.J.; Kleeman, S.D. Complications and untoward effects of the tension-free vaginal tape procedure. Obstet. Gynecol. 2003, 101, 929–932. [Google Scholar] [PubMed]
- Moksnes, L.R.; Svenningsen, R.; Schiøtz, H.A.; Moe, K.; Staff, A.C.; Kulseng-Hanssen, S. Sling mobilization in the management of urinary retention after mid-urethral sling surgery. Neurourol. Urodyn. 2017, 36, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Lo, T.S.; Chua, S.; Tseng, L.H.; Long, C.Y.; Kao, C.C.; Hsieh, W.C. Clinical outcomes on tension-releasing suture appendage on single-incision sling devices for postoperative voiding dysfunction involving undue tape tension. Int. Urogynecol. J. 2019, 30, 1509–1517. [Google Scholar] [CrossRef]
- Baekelandt, F.; Van Oyen, P.; Ghysel, C.; Van der Aa, F.; Ampe, J. Long-term functional results after unilateral mid-urethral sling transection for voiding dysfunction. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016, 207, 89–93. [Google Scholar] [CrossRef]
- Brennand, E.A.; Tang, S.; Birch, C.; Robert, M.; Kim-Fine, S. Early voiding dysfunction after midurethral sling surgery: Comparison of two management approaches. Int. Urogynecol. J. 2017, 28, 1515–1526. [Google Scholar] [CrossRef]
- Hung, M.J.; Liu, F.S.; Shen, P.S.; Chen, G.D.; Lin, L.Y.; Ho, E.S.C. Analysis of two sling procedures using polypropylene mesh for treatment of stress urinary incontinence. Int. J. Gynecol. Obstet. 2004, 84, 133–141. [Google Scholar] [CrossRef]
- McLennan, M.T.; Bent, A.E. Sling incision with associated vaginal wall interposition for obstructed voiding secondary to suburethral sling procedure. Int. Urogynecol. J. 1997, 8, 168–172. [Google Scholar] [CrossRef]
- Spelzini, F.; Frigerio, M.; Regini, C.; Palmieri, S.; Manodoro, S.; Milani, R. Learning curve for the single-incision suburethral sling procedure for female stress urinary incontinence. Int. J. Gynaecol. Obstet. 2017, 139, 363–367. [Google Scholar] [CrossRef]
- Moalli, P.A.; Papas, N.; Menefee, S.; Albo, M.; Meyn, L.; Abramowitch, S.D. Tensile properties of five commonly used mid-urethral slings relative to the TVT. Int. Urogynecol. J. 2008, 19, 655–663. [Google Scholar] [CrossRef]
- Lenz, F.; Doll, S.; Sohn, C.; Brocker, K.A. Single-Incision Mini-Slings: Obturator Complex Pull-Out-Force Measurements. Gynecol. Obstet. Investig. 2017, 82, 376–381. [Google Scholar] [CrossRef]
- Nambiar, A.; Cody, J.D.; Jeffery, S.T.; Aluko, P. Single-incision sling operations for urinary incontinence in women. Cochrane Database Syst. Rev. 2017, 7, CD008709. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.M.; Yang, S.H.; Huang, W.C.; Tzeng, C.R. Correlation of tape location and tension with surgical outcome after transobturator suburethral tape procedures. Ultrasound Obstet. Gynecol. 2012, 39, 458–465. [Google Scholar] [CrossRef]
- Taithongchai, A.; Pandeva, I.; Sultan, A.H.; Thakar, R. Association between 3D endovaginal and 2D perineal pelvic floor ultrasound findings and symptoms in women presenting with mid-urethral sling complications. Ultrasound Obstet. Gynecol. 2021, 57, 639–646. [Google Scholar] [CrossRef]
- Grigoryan, B.; Shadyan, G.; Kasyan, G.; Pushkar, D. Adjustable slings versus other surgical methods in female stress urinary incontinence: A systematic review and meta-analysis. Int. Urogynecol. J. 2023, 34, 1351–1367. [Google Scholar] [CrossRef]
- O’Leary, B.D.; McCreery, A.; Redmond, A.E.; Keane, D.P. The efficacy and complications of retropubic tension-free vaginal tapes after 20 years: A prospective observational study. BJOG 2023, 130, 107–113. [Google Scholar] [CrossRef]
- Offiah, I.; Freeman, R.; MONARC™ Study Group. Long-term efficacy and complications of a multicentre randomised controlled trial comparing retropubic and transobturator mid-urethral slings: A prospective observational study. BJOG 2021, 128, 2191–2199. [Google Scholar] [CrossRef]
- Manso, M.; Botelho, F.; Silva, C.; Cruz, F. Mini-Slings: Do They Stand the Test of Time? A 10-Year Cohort. Urol. Int. 2021, 105, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Hung, M.J.; Ho, E.S.; Shen, P.S.; Sun, M.J.; Lin, A.T.; Chen, G.D.; Taiwan OAB Club. Urgency is the core symptom of female overactive bladder syndrome, as demonstrated by a statistical analysis. J. Urol. 2006, 176, 636–640. [Google Scholar] [CrossRef] [PubMed]
- Irwin, D.E.; Milsom, I.; Hunskaar, S.; Reilly, K.; Kopp, Z.; Herschorn, S.; Coyne, K.; Kelleher, C.; Hampel, C.; Artibani, W.; et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: Results of the EPIC study. Eur. Urol. 2006, 50, 1306–1315. [Google Scholar] [CrossRef]
| AJUST (N = 58) | TVT-O (N = 61) | ||||
|---|---|---|---|---|---|
| Characteristics | Value | Range | Value | Rage | p Value |
| General data | |||||
| Mean age (year) | 54.4 ± 9.4 | (37~82) | 57.4 ± 12.1 | (37~92) | 0.296 * |
| Median parity | 3 | (1~5) | 3 | (1~4) | 0.125 * |
| Mean body mass index (kg/m2) | 24.6 ± 3.3 | (19.4~33.7) | 25.7 ± 3.5 | (18.8–32.2) | 0.225 * |
| % Menopause | 56.9 | (33/58) | 59 | (36/61) | 0.705 # |
| % Diabetes mellitus | 6.9 | (4/58) | 9.8 | (6/61) | 0.744 # |
| % Hypertension | 24.1 | (14/58) | 31.1 | (19/61) | 0.420 # |
| % previous hysterectomy | 8.6 | (8/58) | 18 | (11/61) | 0.620 # |
| Urodynamics (filling and voiding CMG) | |||||
| ALPP (cmH2O) | 63.5 ± 19.1 | (38~110) | 64.3 ± 23.3 | (28~135) | 0.843 * |
| Cystometric capacity (mL) | 314.5 ± 54.7 | (199~410) | 276.0 ± 102.8 | (211~487) | 0.938 * |
| Qmax (mL/min) | 26.0 ± 10.4 | (14~61) | 21.0 ± 8.3 | (12~38) | 0.319 * |
| Qmean (mL/min) | 11.5 ± 4.9 | (6~30) | 12.0 ± 4.5 | (6~22) | 0.460 * |
| Residual urine (mL) | 14.6 ± 25.8 | (0~100) | 15.5 ± 28.4 | (0~100) | 0.976 * |
| One-hour Pad test (gm) | 32.3 ± 14.8 | (10~50) | 33.9 ± 16.1 | (10~50) | 0.134 * |
| AJUST (N = 58) | TVT-O (N = 61) | ||||
|---|---|---|---|---|---|
| Patients’ Characteristics | Value | Range | Value | Rage | p Value |
| Perioperative data | |||||
| Mean hospital stays (days) | 2.9 ± 1.1 | (1~6) | 2.6 ± 0.9 | (1~4) | 0.027 * |
| Mean total operating time (mins) | 63.4 ± 14.4 | (35~95) | 63.2 ± 13.0 | (45~85) | 0.762 * |
| Mean estimated blood loss (mL) | 71.1 ± 40.8 | (50~150) | 64.7 ± 22.3 | (50~100) | 0.874 * |
| Mean Foley drainage (days) | 1.4 ± 0.8 | (1~4) | 1.2 ± 0.5 | (1~3) | 0.220 * |
| Mean PVR at post-op day 1 (mL) | 107.1 ± 171.2 | (0~800) | 61.8 ± 66.5 | (0~250) | 0.468 * |
| Complications | |||||
| % Voiding dysfunction | 17.2 | (10/58) | 3.0 | (2/61) | 0.026 # |
| % De novo UUI | 3.4 | (2/58) | 4.9 | (3/61) | 1.000 # |
| % Groin/Thigh pain | 3.4 | (2/58) | 4.9 | (3/61) | 1.000 # |
| Outcomes of SUI at 1-year | |||||
| % Cure | 91.4 | (53/58) | 91.8 | (56/61) | 1.000 # |
| % Improvement | 5.2 | (3/58) | 4.9 | (3/61) | |
| % Failure | 3.4 | (2/58) | 3.3 | (2/61) | |
| Outcome of SUI at 9-year | |||||
| % Cure | 60.0 | (27/45) | 66.7 | (30/45) | 0.317 # |
| % Improvement | 33.3 | (15/45) | 26.7 | (12/45) | |
| % Failure | 6.7 | (3/45) | 6.7 | (3/45) | |
| Outcomes of UDI-6 & IIQ-7 at 9-year | |||||
| UDI-6 total scores | 1.78 ± 1.77 | (0–5) | 1.84 ± 2.46 | (0–12) | 0.744 * |
| Irritative scores | 0.77 ± 0.87 | (0–2) | 0.67 ± 1.02 | (0–4) | 0.871 * |
| Stress scores | 0.81 ± 0.93 | (0–2) | 0.69 ± 1.00 | (0–4) | 0.791 * |
| Obstructive scores | 0.28 ± 0.45 | (0–1) | 0.49 ± 0.82 | (0–4) | 0.095 * |
| IIQ-7 scores | 1.53 ± 2.76 | (0–11) | 1.80 ± 3.43 | (0–12) | 0.695 * |
| Cases by Slingorder | Sling Type- Series No. | Age | Symptoms | Q Max/Mean (mL/s) | RU | Days to Revision | Sling Position at Revision | Surgical Outcomes of SUI |
|---|---|---|---|---|---|---|---|---|
| 01 | AJUST-03 | 50 | Frequency, groin/thigh pain | 12/7 | 40 | 406 | Distal (unilateral) | failure (immediate recurrence) |
| 02 | AJUST-07 | 49 | Frequency, groin/thigh pain | 38/21 | 60 | 519 | Distal (unilateral) | cured |
| 03 | TVTO-07 | 56 | Slow stream | 10/4 | 30 | 254 | Distal | cured |
| 04 | AJUST-08 | 67 | Urgency | 9/5 | 10 | 84 | Middle | cured |
| 05 | AJUST-09 | 59 | Slow stream, Multiple/positional voiding | 2/2 | 40 | 147 | Middle | cured |
| 06 | AJUST-14 | 51 | Urgency | NA | 40 | 80 | Distal | cured |
| 07 | AJUST-15 | 63 | multiple/positional voiding | 7/3 | Minimal | 153 | Distal (unilateral) | Improvement (delayed recurrence) |
| 08 | AJUST-18 | 52 | Slow stream, recurrent UTI | 31/9 | Minimal | 160 | Proximal | Improvement (delayed recurrence) |
| 09 | AJUST-22 | 63 | Frequency, slow stream | 12/4 | Minimal | 267 | Distal | Improvement (delayed recurrence) |
| 10 | AJUST-23 | 48 | Frequency, urgency. | 35/20 | 240 | 3 | Middle | cured |
| 11 | AJUST-27 | 62 | Urgency, urine stream deviation | 19/8 | 40 | 22 | Distal | cured |
| 12 | TVTO-28 | 48 | Intermittent flow, groin/thigh pain | NA | Minimal | 19 | Middle | cured |
| Continent (N = 57) | Incontinent (N = 33) | p Value | |||
|---|---|---|---|---|---|
| Age (years) | 53.0 | (48.0–63.0) | 52.0 | (45.0–60.5) | 0.365 |
| BMI (kg/M2) | 24.7 | (22.5–26.8) | 23.4 | (22.4–28.1) | 0.719 |
| Parity | 3.0 | (2.0–3.0) | 2.0 | (2.0–3.0) | 0.462 |
| ALPP (cmH2O) | 58.5 | (45.0–74.0) | 62.0 | (52.0–79.0) | 0.285 |
| Menopause | 32 | (56.1%) | 16 | (48.5%) | 0.630 |
| MUS procedures | 0.662 | ||||
| % AJUST | 27 | (47.4%) | 18 | (54.5%) | |
| % TVT-O | 30 | (52.6%) | 15 | (45.5%) | |
| Sling Revision | 8 | (14.0%) | 4 | (12.1%) | 0.382 |
| Follow-up (years) | 9.0 | (8.0–10.0) | 9.0 | (8.0–10.0) | 0.472 |
| UDI-6 total scores at 9 years | 0.93 ± 1.49 | (0–7) | 5.36 ± 3.87 | (1–18) | <0.001 |
| Irritative scores | 0.44 ± 0.76 | (0–2) | 1.94 ± 1.84 | (0–6) | <0.001 |
| Stress scores | 0.13 ± 0.34 | (0–1) | 2.61 ± 1.48 | (1–6) | <0.001 |
| Obstructive scores | 0.36 ± 0.78 | (0–2) | 0.82 ± 1.31 | (0–6) | 0.077 |
| IIQ-7 scores at 9 years | 0.72 ± 2.03 | (0–10) | 4.00 ± 4.03 | (0–12) | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, C.-P.; Liu, C.-K.; Yang, E.; Ying, T.-H.; Chen, G.-D.; Hung, M.-J. Continence Is Not Affected after Sling Revision with Transvaginal Tape Elongation for Post-Sling Voiding Dysfunction. J. Clin. Med. 2024, 13, 637. https://doi.org/10.3390/jcm13020637
Tsai C-P, Liu C-K, Yang E, Ying T-H, Chen G-D, Hung M-J. Continence Is Not Affected after Sling Revision with Transvaginal Tape Elongation for Post-Sling Voiding Dysfunction. Journal of Clinical Medicine. 2024; 13(2):637. https://doi.org/10.3390/jcm13020637
Chicago/Turabian StyleTsai, Ching-Pei, Chih-Ku Liu, Evelyn Yang, Tsung-Ho Ying, Gin-Den Chen, and Man-Jung Hung. 2024. "Continence Is Not Affected after Sling Revision with Transvaginal Tape Elongation for Post-Sling Voiding Dysfunction" Journal of Clinical Medicine 13, no. 2: 637. https://doi.org/10.3390/jcm13020637
APA StyleTsai, C.-P., Liu, C.-K., Yang, E., Ying, T.-H., Chen, G.-D., & Hung, M.-J. (2024). Continence Is Not Affected after Sling Revision with Transvaginal Tape Elongation for Post-Sling Voiding Dysfunction. Journal of Clinical Medicine, 13(2), 637. https://doi.org/10.3390/jcm13020637