Utility of Coronary Computed Tomography Angiography in Patients Undergoing Transcatheter Aortic Valve Implantation: A Meta-Analysis and Meta-Regression Based on Published Data from 7458 Patients
Abstract
1. Introduction
2. Methods
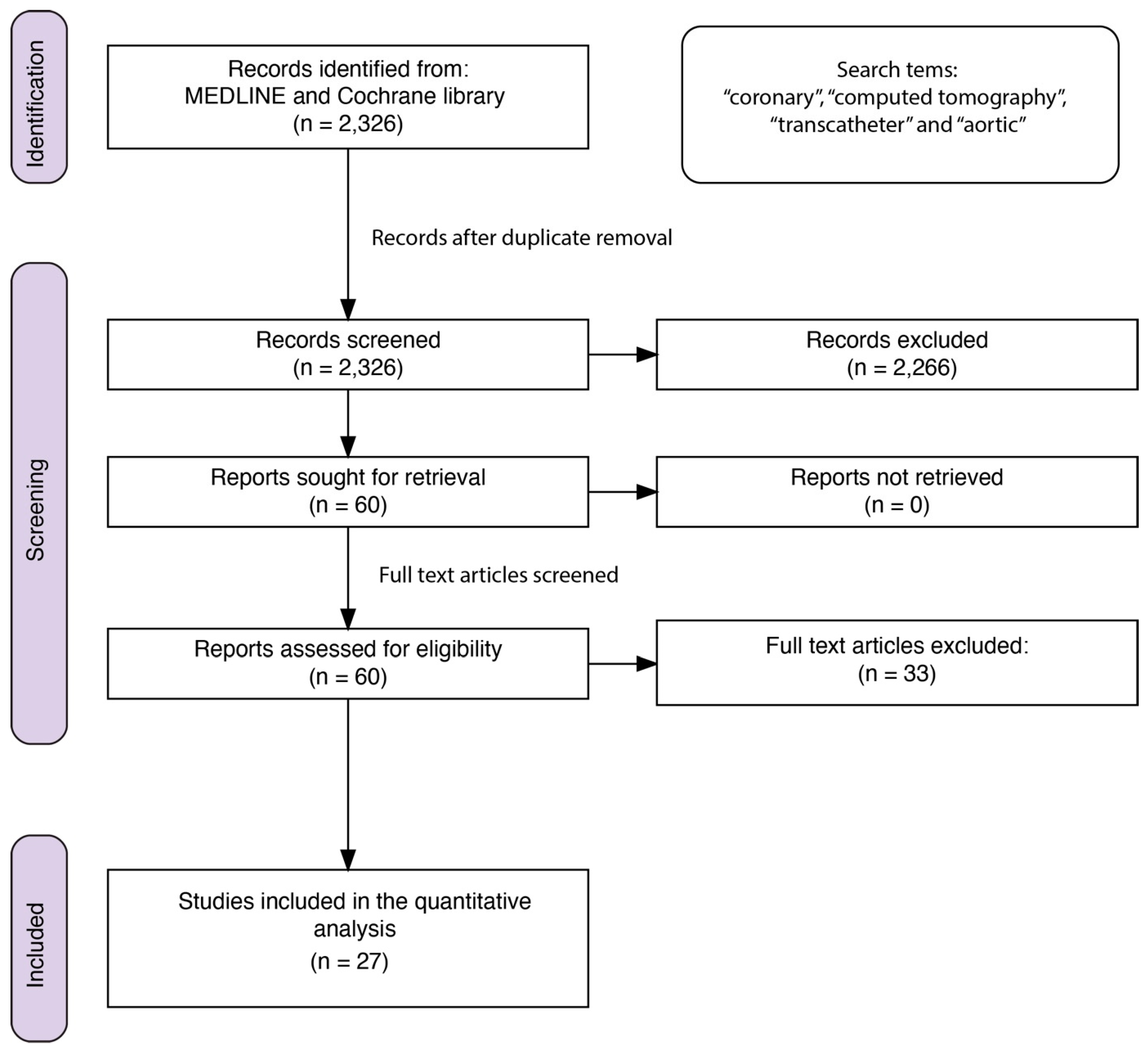
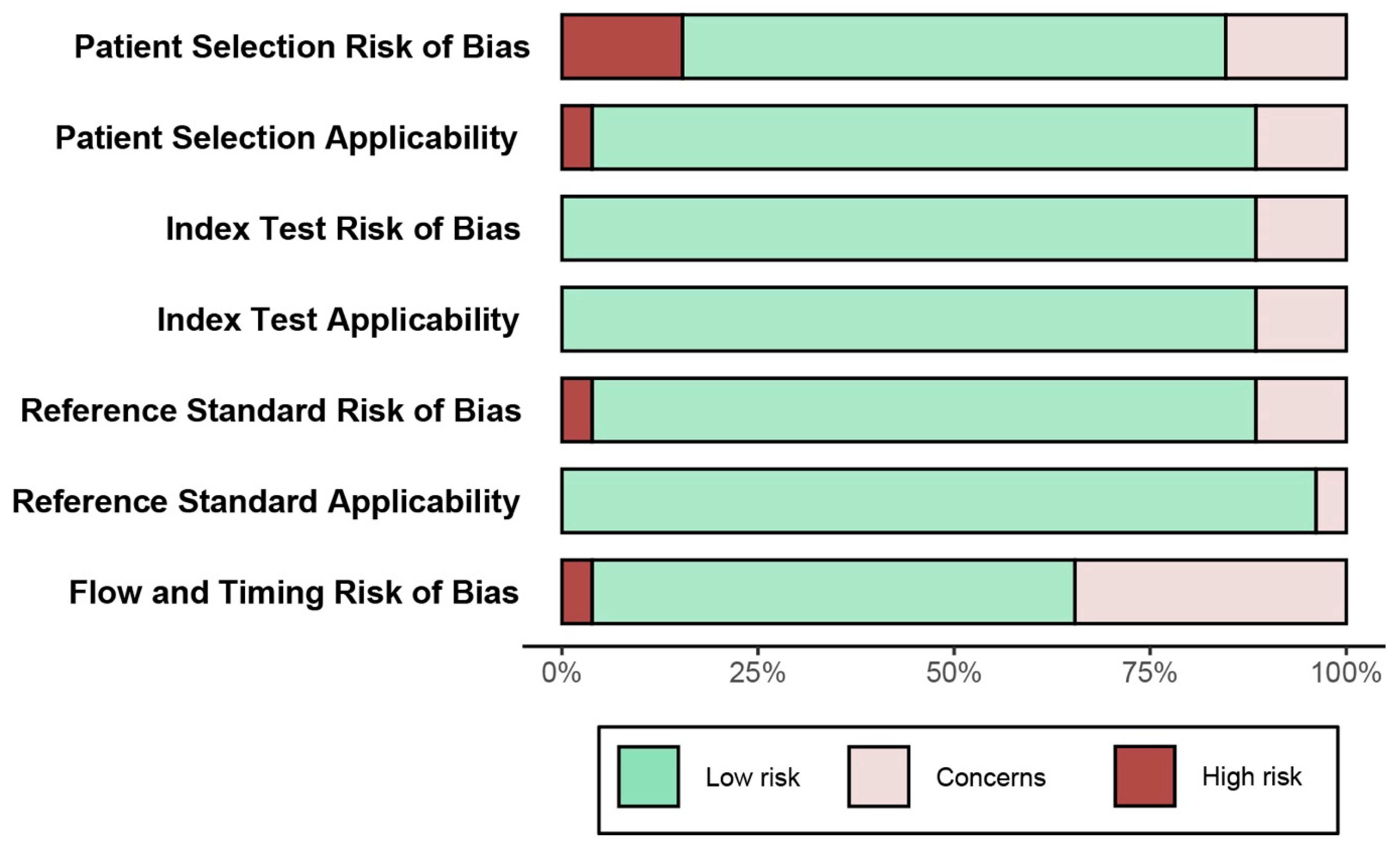
2.1. Study Selection
2.2. Statistical Analysis
3. Results
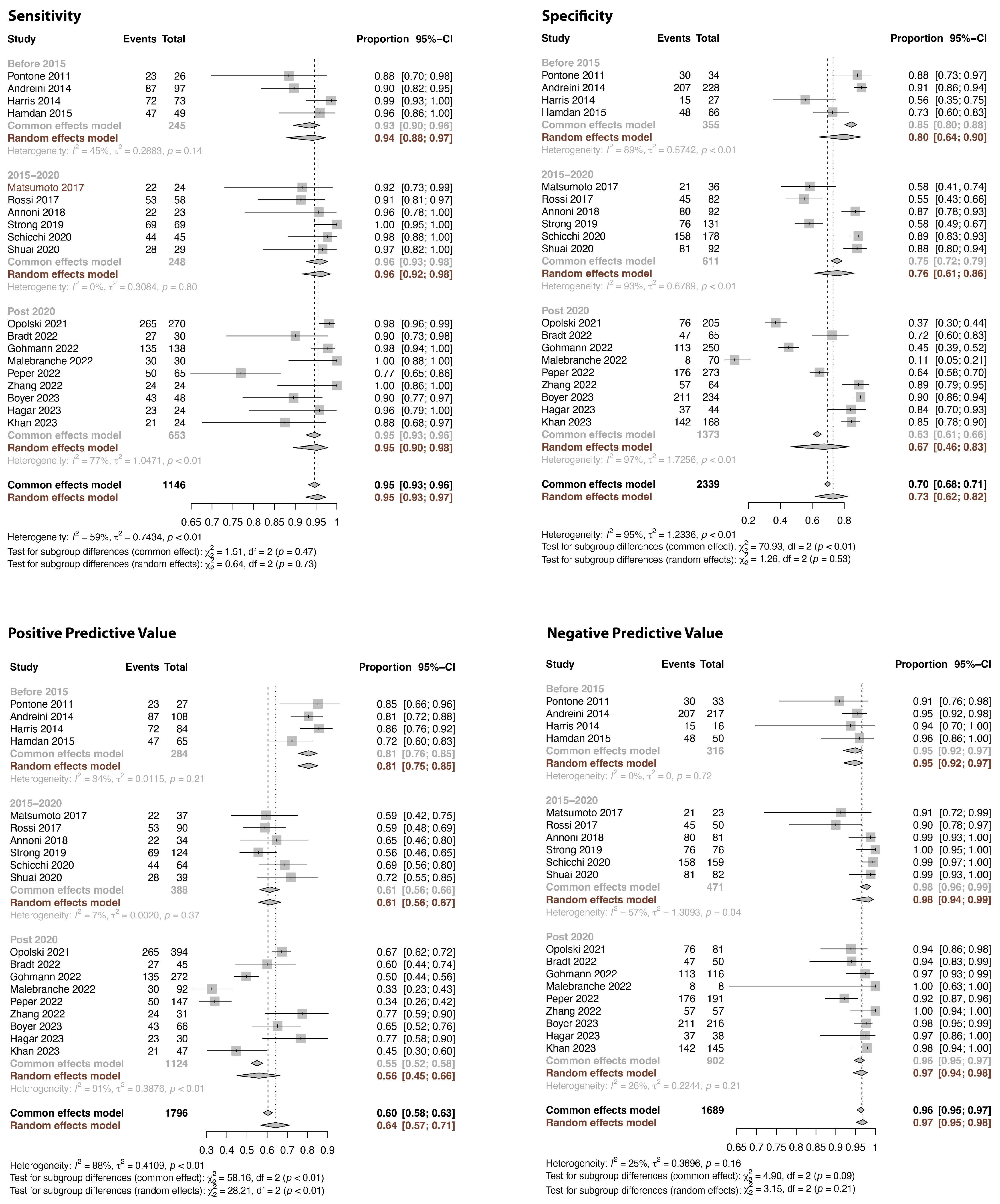
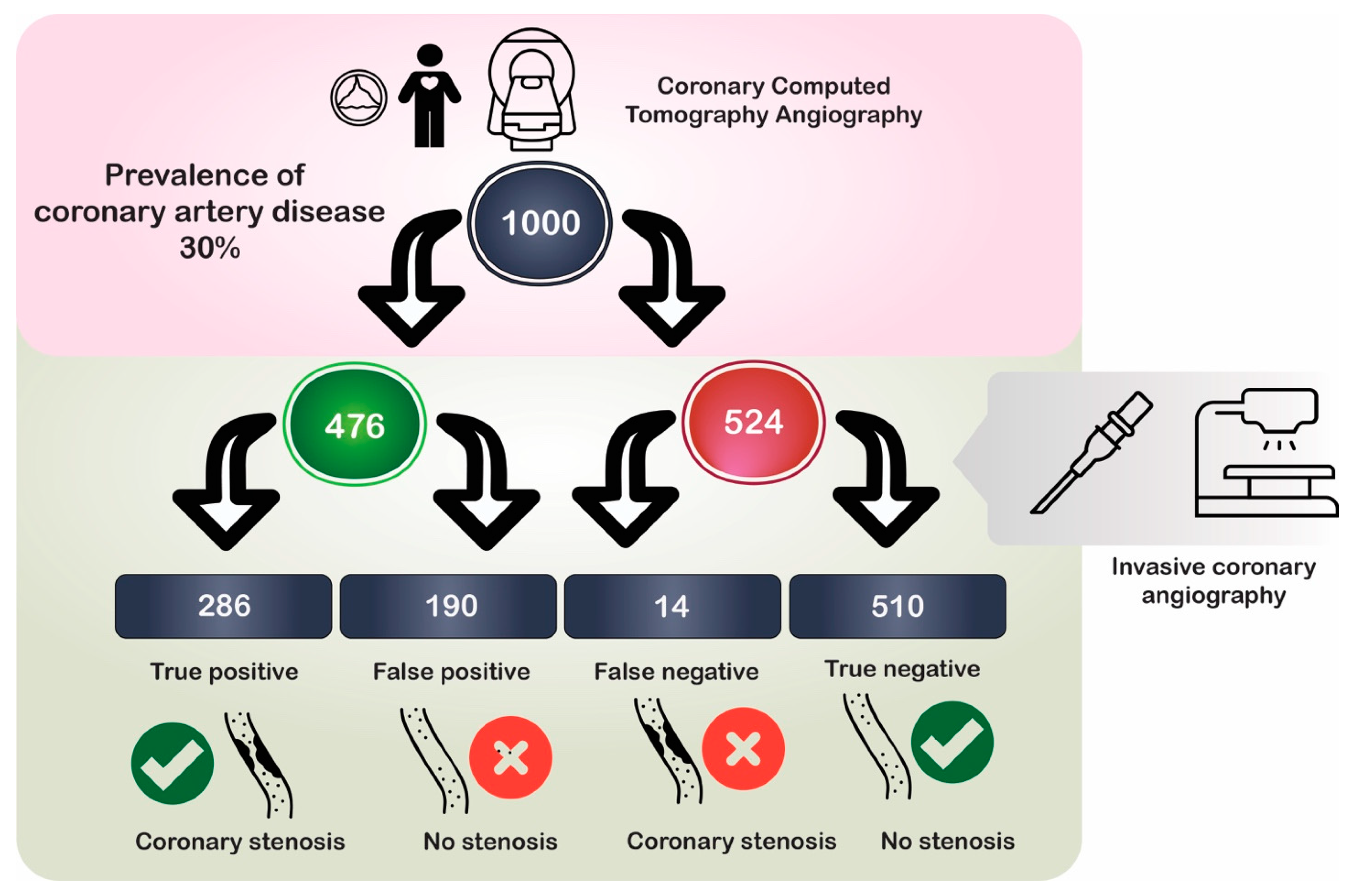
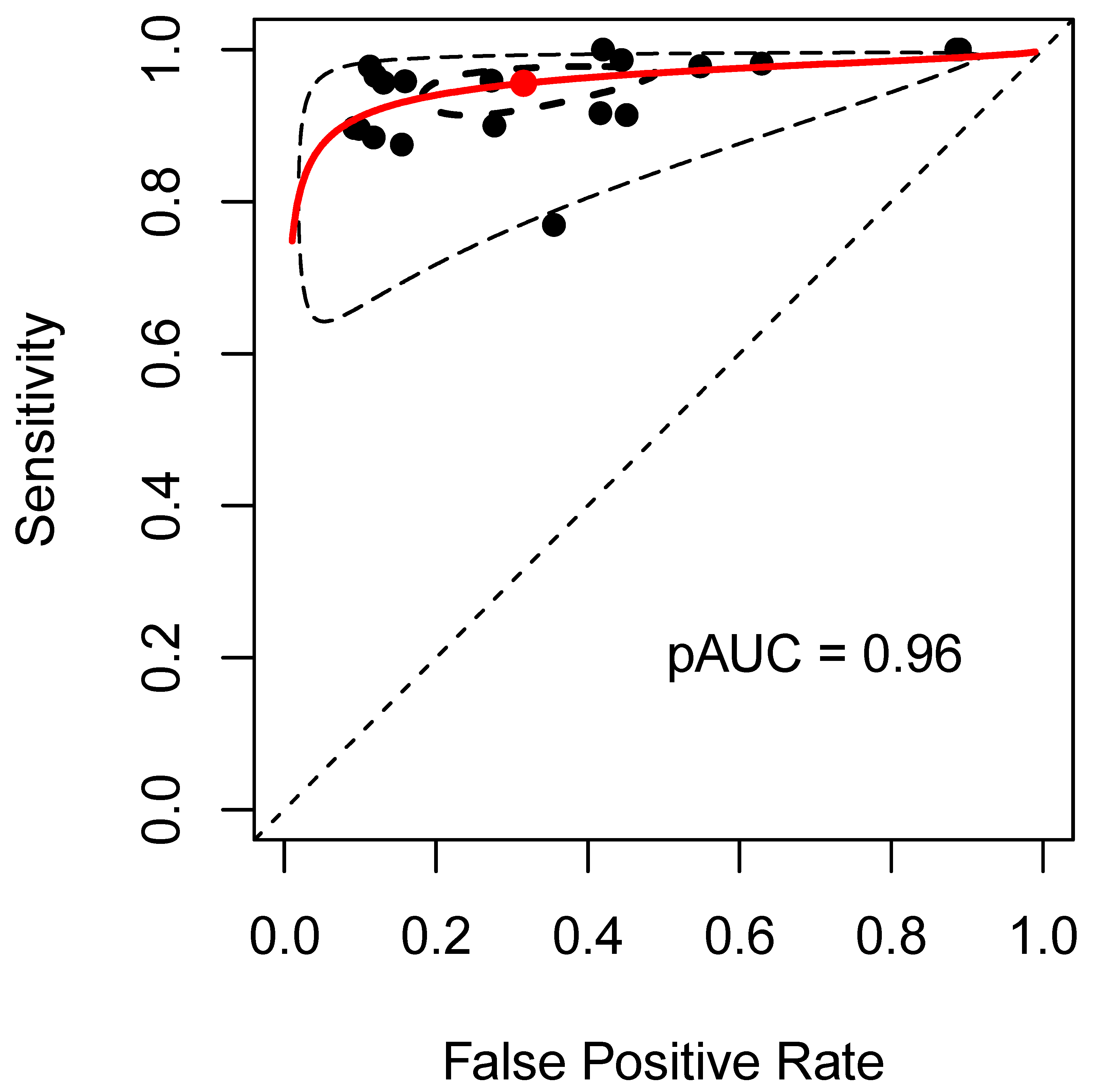
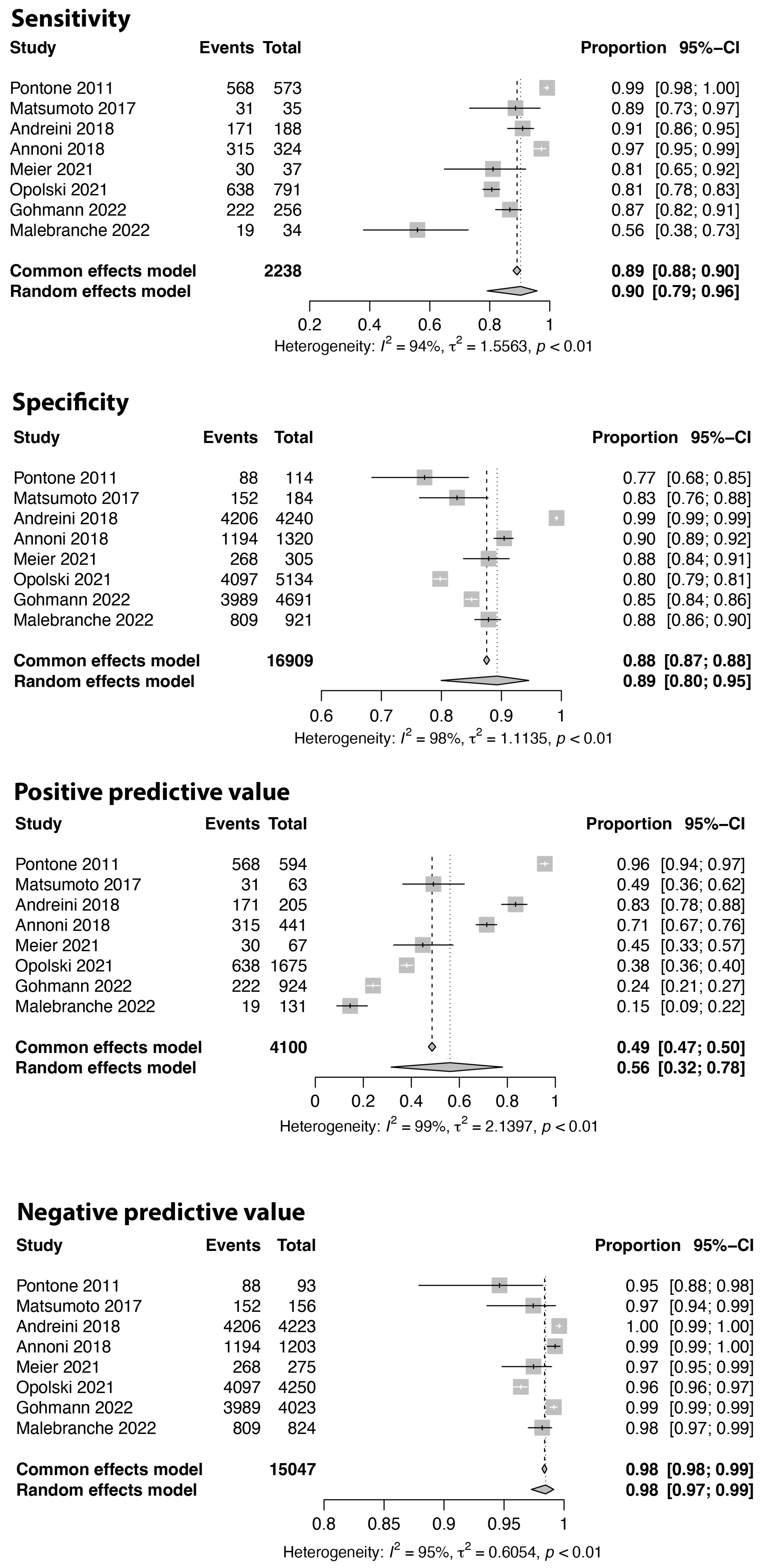
3.1. Per Patient Analysis
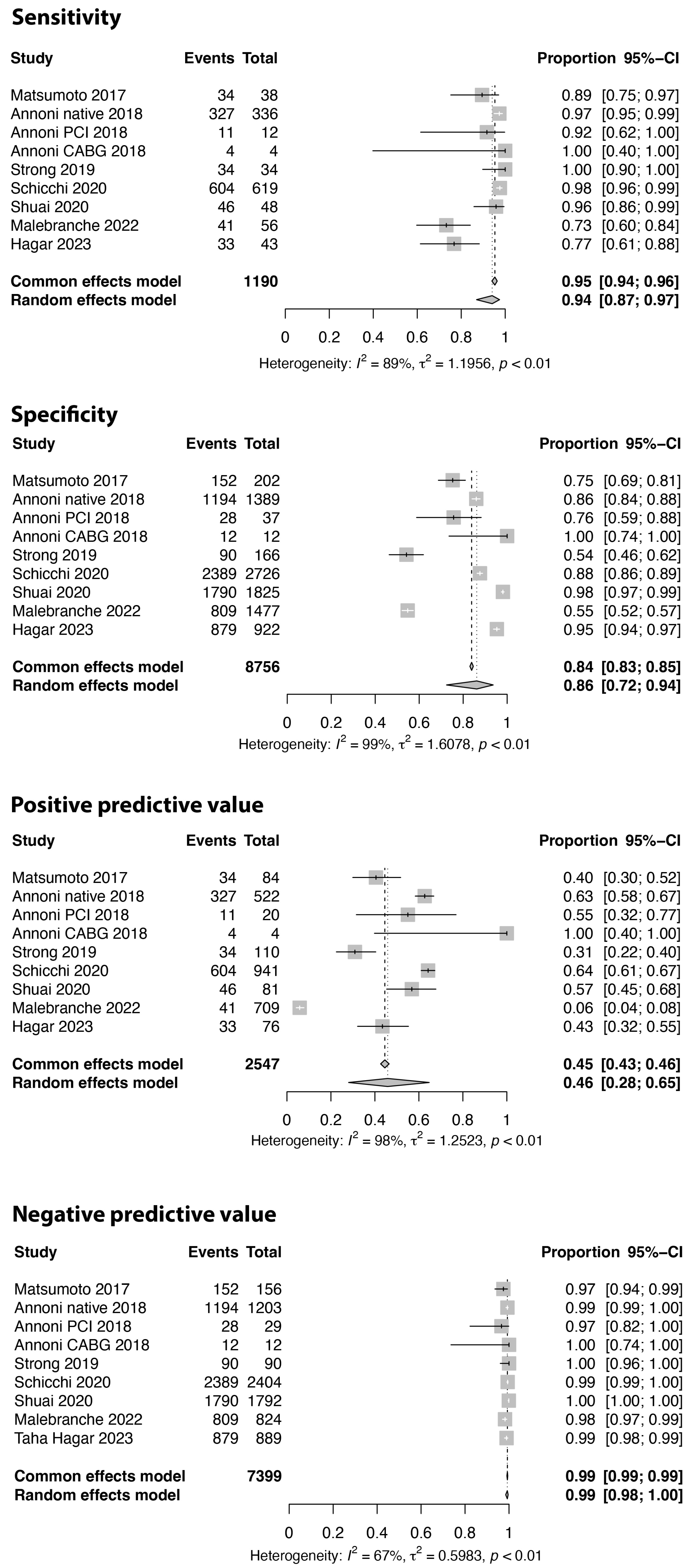
3.2. Per Coronary Segment Analysis
3.3. Analysis of Proximal Coronary Segments and Bypass Grafts
4. Discussion
4.1. Potential and Feasibility of CCTA
4.2. Limitations in Regard to the Evidence
4.3. Limitations of the Current Analysis
4.4. Conclusions and Clinical Implications
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lindman, B.R.; Clavel, M.A.; Mathieu, P.; Iung, B.; Lancellotti, P.; Otto, C.M.; Pibarot, P. Calcific aortic stenosis. Nat. Rev. Dis. Prim. 2016, 2, 16006. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P., 3rd; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA Guideline for the Management of Patients with Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 143, e72–e227. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, H.; Falk, V.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, P.J.; Iung, B.; Lancellotti, P.; Lansac, E.; Rodriguez Munoz, D.; et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart. J. 2017, 38, 2739–2791. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart. J. 2022, 43, 561–632. [Google Scholar] [CrossRef] [PubMed]
- Kalogeropoulos, A.S.; Redwood, S.R.; Allen, C.J.; Hurrell, H.; Chehab, O.; Rajani, R.; Prendergast, B.; Patterson, T. A 20-year journey in transcatheter aortic valve implantation: Evolution to current eminence. Front. Cardiovasc. Med. 2022, 9, 971762. [Google Scholar] [CrossRef]
- Rahhab, Z.; El Faquir, N.; Tchetche, D.; Delgado, V.; Kodali, S.; Mara Vollema, E.; Bax, J.; Leon, M.B.; Van Mieghem, N.M. Expanding the indications for transcatheter aortic valve implantation. Nat. Rev. Cardiol. 2020, 17, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Blanke, P.; Weir-McCall, J.R.; Achenbach, S.; Delgado, V.; Hausleiter, J.; Jilaihawi, H.; Marwan, M.; Norgaard, B.L.; Piazza, N.; Schoenhagen, P.; et al. Computed Tomography Imaging in the Context of Transcatheter Aortic Valve Implantation (TAVI)/Transcatheter Aortic Valve Replacement (TAVR): An Expert Consensus Document of the Society of Cardiovascular Computed Tomography. JACC Cardiovasc. Imaging 2019, 12, 1–24. [Google Scholar] [CrossRef]
- Renker, M.; Schoepf, U.J.; Kim, W.K.; Combined, C.T. Coronary Artery Assessment and TAVI Planning. Diagnostics 2023, 13, 1327. [Google Scholar] [CrossRef]
- Saadi, R.P.; Tagliari, A.P.; Saadi, E.K.; Miglioranza, M.H.; Polanczyck, C.A. Preoperative TAVR Planning: How to Do It. J. Clin. Med. 2022, 11, 2582. [Google Scholar] [CrossRef]
- Postolache, A.; Sperlongano, S.; Lancellotti, P. TAVI after More Than 20 Years. J. Clin. Med. 2023, 12, 5645. [Google Scholar] [CrossRef]
- Leone, P.P.; Scotti, A.; Ho, E.C.; Assafin, M.; Doolittle, J.; Chau, M.; Slipczuk, L.; Levitus, M.; Regazzoli, D.; Mangieri, A.; et al. Prosthesis Tailoring for Patients Undergoing Transcatheter Aortic Valve Implantation. J. Clin. Med. 2023, 12, 338. [Google Scholar] [CrossRef] [PubMed]
- Granger, C.; Guedeney, P. Device Selection for Transcatheter Aortic Valve Implantation. J. Clin. Med. 2022, 12, 284. [Google Scholar] [CrossRef] [PubMed]
- Katchi, F.; Bhatt, D.; Markowitz, S.M.; Szymonifka, J.; Cheng, E.P.; Minutello, R.M.; Bergman, G.W.; Wong, S.C.; Salemi, A.; Truong, Q.A. Impact of Aortomitral Continuity Calcification on Need for Permanent Pacemaker After Transcatheter Aortic Valve Replacement. Circ. Cardiovasc. Imaging 2019, 12, e009570. [Google Scholar] [CrossRef]
- Androshchuk, V.; Chehab, O.; Prendergast, B.; Rajani, R.; Patterson, T.; Redwood, S. Computed tomography derived anatomical predictors of vascular access complications following transfemoral transcatheter aortic valve implantation: A systematic review. Catheter. Cardiovasc. Interv. 2023, 103, 169–185. [Google Scholar] [CrossRef] [PubMed]
- Daghem, M.; Weidinger, F.; Achenbach, S. Computed tomography to guide transcatheter aortic valve implantation. Herz 2023, 48, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Dencker, D.; Pedersen, F.; Engstrom, T.; Kober, L.; Hojberg, S.; Nielsen, M.B.; Schroeder, T.V.; Lonn, L. Major femoral vascular access complications after coronary diagnostic and interventional procedures: A Danish register study. Int. J. Cardiol. 2016, 202, 604–608. [Google Scholar] [CrossRef]
- Louvard, Y.; Benamer, H.; Garot, P.; Hildick-Smith, D.; Loubeyre, C.; Rigattieri, S.; Monchi, M.; Lefevre, T.; Hamon, M.; Group, O.S. Comparison of transradial and transfemoral approaches for coronary angiography and angioplasty in octogenarians (the OCTOPLUS study). Am. J. Cardiol. 2004, 94, 1177–1180. [Google Scholar] [CrossRef]
- Gatti, M.; Gallone, G.; Poggi, V.; Bruno, F.; Serafini, A.; Depaoli, A.; De Filippo, O.; Conrotto, F.; Darvizeh, F.; Faletti, R.; et al. Diagnostic accuracy of coronary computed tomography angiography for the evaluation of obstructive coronary artery disease in patients referred for transcatheter aortic valve implantation: A systematic review and meta-analysis. Eur. Radiol. 2022, 32, 5189–5200. [Google Scholar] [CrossRef]
- van den Boogert, T.P.W.; Vendrik, J.; Claessen, B.; Baan, J.; Beijk, M.A.; Limpens, J.; Boekholdt, S.A.M.; Hoek, R.; Planken, R.N.; Henriques, J.P. CTCA for detection of significant coronary artery disease in routine TAVI work-up: A systematic review and meta-analysis. Neth. Heart. J. 2018, 26, 591–599. [Google Scholar] [CrossRef]
- Andrew, M.; John, H. The challenge of coronary calcium on coronary computed tomographic angiography (CCTA) scans: Effect on interpretation and possible solutions. Int. J. Cardiovasc. Imaging 2015, 31 (Suppl. 2), 145–157. [Google Scholar] [CrossRef]
- Chaikriangkrai, K.; Jhun, H.Y.; Shantha, G.P.S.; Abdulhak, A.B.; Tandon, R.; Alqasrawi, M.; Klappa, A.; Pancholy, S.; Deshmukh, A.; Bhama, J.; et al. Diagnostic Accuracy of Coronary Computed Tomography Before Aortic Valve Replacement: Systematic Review and Meta-Analysis. J. Thorac. Imaging 2018, 33, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell. Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.F.; Rutjes, A.W.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.; Sterne, J.A.; Bossuyt, P.M.; Group, Q. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Wang, N. Conducting Meta-analyses of Proportions in R. J. Behav. Data Sci. 2023, 3, 1–63. [Google Scholar] [CrossRef]
- Patel, A.; Cooper, N.; Freeman, S.; Sutton, A. Graphical enhancements to summary receiver operating characteristic plots to facilitate the analysis and reporting of meta-analysis of diagnostic test accuracy data. Res. Synth. Methods 2021, 12, 34–44. [Google Scholar] [CrossRef]
- Schlattmann, P. Tutorial: Statistical methods for the meta-analysis of diagnostic test accuracy studies. Clin. Chem. Lab Med. 2023, 61, 777–794. [Google Scholar] [CrossRef]
- Andreini, D.; Pontone, G.; Mushtaq, S.; Bartorelli, A.L.; Ballerini, G.; Bertella, E.; Segurini, C.; Conte, E.; Annoni, A.; Baggiano, A.; et al. Diagnostic accuracy of multidetector computed tomography coronary angiography in 325 consecutive patients referred for transcatheter aortic valve replacement. Am. Heart. J. 2014, 168, 332–339. [Google Scholar] [CrossRef]
- Annoni, A.D.; Andreini, D.; Pontone, G.; Mancini, M.E.; Formenti, A.; Mushtaq, S.; Baggiano, A.; Conte, E.; Guglielmo, M.; Muscogiuri, G.; et al. CT angiography prior to TAVI procedure using third-generation scanner with wide volume coverage: Feasibility, renal safety and diagnostic accuracy for coronary tree. Br. J. Radiol. 2018, 91, 20180196. [Google Scholar] [CrossRef]
- Boyer, J.; Bartoli, A.; Deharo, P.; Vaillier, A.; Ferrara, J.; Barral, P.A.; Jaussaud, N.; Morera, P.; Porto, A.; Collart, F.; et al. Feasibility of Non-Invasive Coronary Artery Disease Screening with Coronary CT Angiography before Transcatheter Aortic Valve Implantation. J. Clin. Med. 2023, 12, 2285. [Google Scholar] [CrossRef]
- Brandt, V.; Schoepf, U.J.; Aquino, G.J.; Bekeredjian, R.; Varga-Szemes, A.; Emrich, T.; Bayer, R.R., 2nd; Schwarz, F.; Kroencke, T.J.; Tesche, C.; et al. Impact of machine-learning-based coronary computed tomography angiography-derived fractional flow reserve on decision-making in patients with severe aortic stenosis undergoing transcatheter aortic valve replacement. Eur. Radiol. 2022, 32, 6008–6016. [Google Scholar] [CrossRef]
- Chava, S.; Gentchos, G.; Abernethy, A.; Leavitt, B.; Terrien, E.; Dauerman, H.L. Routine CT angiography to detect severe coronary artery disease prior to transcatheter aortic valve replacement. J. Thromb. Thrombolysis 2017, 44, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Gohmann, R.F.; Pawelka, K.; Seitz, P.; Majunke, N.; Heiser, L.; Renatus, K.; Desch, S.; Lauten, P.; Holzhey, D.; Noack, T.; et al. Combined cCTA and TAVR Planning for Ruling Out Significant CAD: Added Value of ML-Based CT-FFR. JACC Cardiovasc. Imaging 2022, 15, 476–486. [Google Scholar] [CrossRef] [PubMed]
- Hachulla, A.L.; Noble, S.; Ronot, M.; Guglielmi, G.; de Perrot, T.; Montet, X.; Vallee, J.P. Low Iodine Contrast Injection for CT Acquisition Prior to Transcatheter Aortic Valve Replacement: Aorta Assessment and Screening for Coronary Artery Disease. Acad. Radiol. 2019, 26, e150–e160. [Google Scholar] [CrossRef] [PubMed]
- Hagar, M.T.; Soschynski, M.; Saffar, R.; Rau, A.; Taron, J.; Weiss, J.; Stein, T.; Faby, S.; von Zur Muehlen, C.; Ruile, P.; et al. Accuracy of Ultrahigh-Resolution Photon-counting CT for Detecting Coronary Artery Disease in a High-Risk Population. Radiology 2023, 307, e223305. [Google Scholar] [CrossRef] [PubMed]
- Hamdan, A.; Wellnhofer, E.; Konen, E.; Kelle, S.; Goitein, O.; Andrada, B.; Raanani, E.; Segev, A.; Barbash, I.; Klempfner, R.; et al. Coronary CT angiography for the detection of coronary artery stenosis in patients referred for transcatheter aortic valve replacement. J. Cardiovasc. Comput. Tomogr. 2015, 9, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Harris, B.S.; De Cecco, C.N.; Schoepf, U.J.; Steinberg, D.H.; Bayer, R.R.; Krazinski, A.W.; Dyer, K.T.; Sandhu, M.K.; Zile, M.R.; Meinel, F.G. Dual-source CT imaging to plan transcatheter aortic valve replacement: Accuracy for diagnosis of obstructive coronary artery disease. Radiology 2015, 275, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Gedela, S.; Frost, O.M.T.; Galinato, M.; Crawford, I.; Smith, S.; Fawaz, S.; Simpson, R.; Singh, A.; Karamasis, G.V.; et al. Noncoronary Gated Transcatheter Aortic Valve Replacement Computed Tomography Scans Can Safely Replace Invasive Coronary Angiography Pre-Transcatheter Aortic Valve Replacement. Struct. Heart. 2023, 7, 100123. [Google Scholar] [CrossRef]
- Kondoleon, N.P.; Layoun, H.; Spilias, N.; Sipko, J.; Kanaan, C.; Harb, S.; Reed, G.; Puri, R.; Yun, J.; Krishnaswamy, A.; et al. Effectiveness of Pre-TAVR CTA as a Screening Tool for Significant CAD Before TAVR. JACC Cardiovasc. Interv. 2023, 16, 1990–2000. [Google Scholar] [CrossRef]
- Lecomte, A.; Serrand, A.; Marteau, L.; Carlier, B.; Manigold, T.; Letocart, V.; Warin Fresse, K.; Nguyen, J.M.; Serfaty, J.M. Coronary artery assessment on pre transcatheter aortic valve implantation computed tomography may avoid the need for additional coronary angiography. Diagn. Interv. Imaging 2023, 104, 547–551. [Google Scholar] [CrossRef]
- Malebranche, D.; Hoffner, M.K.M.; Huber, A.T.; Cicovic, A.; Spano, G.; Bernhard, B.; Bartkowiak, J.; Okuno, T.; Lanz, J.; Raber, L.; et al. Diagnostic performance of quantitative coronary artery disease assessment using computed tomography in patients with aortic stenosis undergoing transcatheter aortic-valve implantation. BMC Cardiovasc. Disord. 2022, 22, 178. [Google Scholar] [CrossRef]
- Matsumoto, S.; Yamada, Y.; Hashimoto, M.; Okamura, T.; Yamada, M.; Yashima, F.; Hayashida, K.; Fukuda, K.; Jinzaki, M. CT imaging before transcatheter aortic valve implantation (TAVI) using variable helical pitch scanning and its diagnostic performance for coronary artery disease. Eur. Radiol. 2017, 27, 1963–1970. [Google Scholar] [CrossRef] [PubMed]
- Meier, D.; Depierre, A.; Topolsky, A.; Roguelov, C.; Dupre, M.; Rubimbura, V.; Eeckhout, E.; Qanadli, S.D.; Muller, O.; Mahendiran, T.; et al. Computed Tomography Angiography for the Diagnosis of Coronary Artery Disease Among Patients Undergoing Transcatheter Aortic Valve Implantation. J. Cardiovasc. Transl. Res. 2021, 14, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Opolski, M.P.; Kim, W.K.; Liebetrau, C.; Walther, C.; Blumenstein, J.; Gaede, L.; Kempfert, J.; Van Linden, A.; Walther, T.; Hamm, C.W.; et al. Diagnostic accuracy of computed tomography angiography for the detection of coronary artery disease in patients referred for transcatheter aortic valve implantation. Clin. Res. Cardiol. 2015, 104, 471–480. [Google Scholar] [CrossRef] [PubMed]
- Peper, J.; Becker, L.M.; van den Berg, H.; Bor, W.L.; Brouwer, J.; Nijenhuis, V.J.; van Ginkel, D.J.; Rensing, B.; Ten Berg, J.M.; Timmers, L.; et al. Diagnostic Performance of CCTA and CT-FFR for the Detection of CAD in TAVR Work-Up. JACC Cardiovasc. Interv. 2022, 15, 1140–1149. [Google Scholar] [CrossRef] [PubMed]
- Pontone, G.; Andreini, D.; Bartorelli, A.L.; Annoni, A.; Mushtaq, S.; Bertella, E.; Formenti, A.; Cortinovis, S.; Alamanni, F.; Fusari, M.; et al. Feasibility and accuracy of a comprehensive multidetector computed tomography acquisition for patients referred for balloon-expandable transcatheter aortic valve implantation. Am. Heart. J. 2011, 161, 1106–1113. [Google Scholar] [CrossRef] [PubMed]
- Renker, M.; Steinbach, R.; Schoepf, U.J.; Fischer-Rasokat, U.; Choi, Y.H.; Hamm, C.W.; Rolf, A.; Kim, W.K. Comparison of First-generation and Third-generation Dual-source Computed Tomography for Detecting Coronary Artery Disease in Patients Evaluated for Transcatheter Aortic Valve Replacement. J. Thorac. Imaging 2023, 38, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.; De Cecco, C.N.; Kennon, S.R.O.; Zou, L.; Meinel, F.G.; Toscano, W.; Segreto, S.; Achenbach, S.; Hausleiter, J.; Schoepf, U.J.; et al. CT angiography to evaluate coronary artery disease and revascularization requirement before trans-catheter aortic valve replacement. J. Cardiovasc. Comput. Tomogr. 2017, 11, 338–346. [Google Scholar] [CrossRef]
- Sasaki, S.; Kawamori, H.; Toba, T.; Takeshige, R.; Fukuyama, Y.; Hiromasa, T.; Fujii, H.; Hamana, T.; Osumi, Y.; Iwane, S.; et al. Diagnostic Accuracy of Pre-Transcatheter Aortic Valve Replacement Nitroglycerin-Free Fractional Flow Reserve-Computed Tomography-Based Physiological Assessment in Patients with Severe Aortic Stenosis for Predicting Post-Transcatheter Aortic Valve Replacement Ischemia. Circ. J. 2023. [Google Scholar] [CrossRef]
- Schicchi, N.; Fogante, M.; Pirani, P.E.; Agliata, G.; Piva, T.; Tagliati, C.; Marcucci, M.; Francioso, A.; Giovagnoni, A. Third generation dual source CT with ultra-high pitch protocol for TAVI planning and coronary tree assessment: Feasibility, image quality and diagnostic performance. Eur. J. Radiol. 2020, 122, 108749. [Google Scholar] [CrossRef]
- Shuai, T.; Li, W.; You, Y.; Deng, L.; Li, J.; Peng, L.; Li, Z. Combined Coronary CT Angiography and Evaluation of Access Vessels for TAVR Patients in Free-Breathing with Single Contrast Medium Injection Using a 16-cm-Wide Detector CT. Acad. Radiol. 2021, 28, 1662–1668. [Google Scholar] [CrossRef]
- Strong, C.; Ferreira, A.; Teles, R.C.; Mendes, G.; Abecasis, J.; Cardoso, G.; Guerreiro, S.; Freitas, P.; Santos, A.C.; Saraiva, C.; et al. Diagnostic accuracy of computed tomography angiography for the exclusion of coronary artery disease in candidates for transcatheter aortic valve implantation. Sci. Rep. 2019, 9, 19942. [Google Scholar] [CrossRef] [PubMed]
- van den Boogert, T.P.W.; Claessen, B.; Opolski, M.P.; Kim, W.K.; Hamdan, A.; Andreini, D.; Pugliese, F.; Mollmann, H.; Delewi, R.; Baan, J.; et al. DEtection of ProxImal Coronary stenosis in the work-up for Transcatheter aortic valve implantation using CTA (from the DEPICT CTA collaboration). Eur. Radiol. 2022, 32, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Li, Z.; You, Y.; Peng, L.; Li, J.; Shuai, T. Image quality and diagnostic performance evaluation in transcatheter aortic valve implantation candidates with atrial fibrillation using a whole-heart coverage CT scanner. Eur. Radiol. 2022, 32, 1034–1043. [Google Scholar] [CrossRef] [PubMed]
- Michail, M.; Ihdayhid, A.R.; Comella, A.; Thakur, U.; Cameron, J.D.; McCormick, L.M.; Gooley, R.P.; Nicholls, S.J.; Mathur, A.; Hughes, A.D.; et al. Feasibility and Validity of Computed Tomography-Derived Fractional Flow Reserve in Patients with Severe Aortic Stenosis: The CAST-FFR Study. Circ. Cardiovasc. Interv. 2021, 14, e009586. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.K.; Vollema, E.M.; Stassen, J.; van Rosendael, A.; Gegenava, T.; van der Kley, F.; Knuuti, J.; Marsan, N.A.; Delgado, V.; Bax, J.J. Comparison of the Quantity of Calcium in the Aortic Valve and the Coronary Arteries in Men Versus Women Who Underwent Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2022, 182, 83–88. [Google Scholar] [CrossRef]
- Schlattmann, P.; Schuetz, G.M.; Dewey, M. Influence of coronary artery disease prevalence on predictive values of coronary CT angiography: A meta-regression analysis. Eur. Radiol. 2011, 21, 1904–1913. [Google Scholar] [CrossRef] [PubMed]
- Di Carli, M.F.; Gupta, A. Estimating Pre-Test Probability of Coronary Artery Disease: Battle of the Scores in an Evolving CAD Landscape. JACC Cardiovasc. Imaging 2019, 12, 1401–1404. [Google Scholar] [CrossRef]
- Diamond, G.A.; Forrester, J.S. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N. Engl. J. Med. 1979, 300, 1350–1358. [Google Scholar] [CrossRef]
- Natanzon, S.S.; Fardman, A.; Mazin, I.; Barbash, I.; Segev, A.; Konen, E.; Goitein, O.; Guetta, V.; Raanani, E.; Maor, E.; et al. Usefulness of Coronary Artery Calcium Score to Rule Out Obstructive Coronary Artery Disease Before Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2022, 183, 70–77. [Google Scholar] [CrossRef]
- Kotronias, R.A.; Kwok, C.S.; George, S.; Capodanno, D.; Ludman, P.F.; Townend, J.N.; Doshi, S.N.; Khogali, S.S.; Genereux, P.; Herrmann, H.C.; et al. Transcatheter Aortic Valve Implantation with or without Percutaneous Coronary Artery Revascularization Strategy: A Systematic Review and Meta-Analysis. J. Am. Heart. Assoc. 2017, 6, e005960. [Google Scholar] [CrossRef]
- Patterson, T.; Clayton, T.; Dodd, M.; Khawaja, Z.; Morice, M.C.; Wilson, K.; Kim, W.K.; Meneveau, N.; Hambrecht, R.; Byrne, J.; et al. ACTIVATION (PercutAneous Coronary inTervention prIor to transcatheter aortic VAlve implantaTION): A Randomized Clinical Trial. JACC Cardiovasc. Interv. 2021, 14, 1965–1974. [Google Scholar] [CrossRef] [PubMed]
- Rheude, T.; Costa, G.; Ribichini, F.L.; Pilgrim, T.; Amat Santos, I.J.; De Backer, O.; Kim, W.K.; Ribeiro, H.B.; Saia, F.; Bunc, M.; et al. Comparison of different percutaneous revascularisation timing strategies in patients undergoing transcatheter aortic valve implantation. EuroIntervention 2023, 19, 589–599. [Google Scholar] [CrossRef] [PubMed]
- Mancini, G.B.J.; Leipsic, J.; Budoff, M.J.; Hague, C.J.; Min, J.K.; Stevens, S.R.; Reynolds, H.R.; O’Brien, S.M.; Shaw, L.J.; Manjunath, C.N.; et al. CT Angiography Followed by Invasive Angiography in Patients with Moderate or Severe Ischemia-Insights From the ISCHEMIA Trial. JACC Cardiovasc. Imaging 2021, 14, 1384–1393. [Google Scholar] [CrossRef] [PubMed]
- Schuetz, G.M.; Schlattmann, P.; Achenbach, S.; Budoff, M.; Garcia, M.J.; Roehle, R.; Pontone, G.; Meijboom, W.B.; Andreini, D.; Alkadhi, H.; et al. Individual patient data meta-analysis for the clinical assessment of coronary computed tomography angiography: Protocol of the Collaborative Meta-Analysis of Cardiac CT (CoMe-CCT). Syst. Rev. 2013, 2, 13. [Google Scholar] [CrossRef]
- Deeks, J.J.; Macaskill, P.; Irwig, L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J. Clin. Epidemiol. 2005, 58, 882–893. [Google Scholar] [CrossRef]


| Study | Year | Patients | Age | Males (%) | BMI | D.M. | AF | Hyperchol. | HT | PCI | CABG | Betablocker | CT Slices |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pontone | 2011 | 60 | 80.0 ± 8.0 | 63.3% | 25.0 ± 5.0 | 13.0% | 0.0% | 40.0% | 67.0% | 24.0% | 16.0% | ivabradine | 64 |
| Andreini | 2014 | 325 | 81.1 ± 6.6 | 40.6% | 25.6 ± 4.4 | 30.0% | 0.0% | 53.0% | 74.0% | 15.1% | 12.9% | ivabradine | 64 |
| Harris | 2014 | 100 | 79.6 ± 9.9 | 61.0% | - | 24.0% | 36.0% | 72.0% | 92.0% | 16.0% | 41.0% | no | 128 |
| Hamdan | 2015 | 115 | 80.4 | 43.6% | 26.8 | 30.4% | 7.8% | 70.4% | 85.2% | 69.6% | 20.0% | yes | 256 |
| Matsumoto | 2017 | 60 | 84.4 ± 4.6 | 28.3% | 22.3 ± 3.6 | - | - | - | - | 10.0% | 3.3% | - | 320 |
| Rossi | 2017 | 140 | 82.3 ± 7.7 | 48.6% | 27.1 ± 5.3 | 21.0% | 31.0% | 59.0% | 75.0% | 0.0% | 0.0% | no | 128 |
| Annoni | 2018 | 115 | 82.5 ± 6.2 | 55.7% | 26.7 ± 3.6 | 18.3% | 13.0% | 68.7% | 71.3% | 14.8% | 13.9% | no | 256 |
| Hachulla | 2019 | 84 | 84.8 | 47.6% | 26.9 | - | - | - | - | - | - | no | 128 |
| Strong | 2019 | 200 | 83.4 ± 5.9 | 40.0% | 26.6 ± 4.7 | 28.0% | 33.5% | 73.5% | 92.5% | 0.0% | 0.0% | no | 64 |
| Schicchi | 2020 | 223 | 79.2 ± 4.9 | - | - | - | 19.7% | - | - | 35.0% | 16.6% | no | 192 |
| Shuai | 2020 | 121 | 73.3 ± 6.4 | 47.1% | 22.6 ± 3.9 | 26.4% | 27.2% | 12.0% | 37.1% | 0.0% | 0.0% | no | 256 |
| Meier | 2021 | 127 | 82.3 ± 7.3 | 38.6% | 26.5 ± 5.1 | 36.0% | - | 54.3% | 77.2% | 16.5% | 0.0% | no | 64 |
| Opolski | 2021 | 475 | 82.6 ± 6.0 | 41.0% | 27.5 ± 5,1 | 32.0% | 19.0% | 48.0% | 95.0% | 48.0% | 19.0% | no | 64 |
| van den Boogert * | 2021 | 1060 | 81.7 ± 6.6 | 51.4% | 26.8 ± 4.9 | 21.3% | 15.5% | 51.8% | 84.0% | 29.8% | 16.1% | yes | various |
| Bradt | 2022 | 95 | 78.6 ± 8.8 | 47.4% | 28.2 ± 6.6 | 30.5% | 35.8% | 74.7% | 96.8% | 9.4% | 0.0% | yes | 128 |
| Gohmann | 2022 | 460 | 79.6 ± 7.4 | 57.0% | 29.4 | - | - | - | - | 0.0% | 0.0% | no | 128 |
| Malebranche | 2022 | 100 | 82.3 ± 6.5 | 30.0% | 25.5 ± 5.6 | 20.0% | 14.0% | - | 84.0% | 0.0% | 0.0% | no | 128 |
| Peper | 2022 | 338 | 81.0 ± 6.5 | 42.3% | 26.6 ± 5.0 | 25.4% | - | 29.3% | 71.3% | 0.0% | 0.0% | yes | 64 and 256 |
| Zhang | 2022 | 88 | 74.0 ± 6.0 | 56.8% | 22.4 ± 4.1 | 9.1% | 100.0% | - | 27.3% | 0.0% | 0.0% | no | 256 |
| Boyer | 2023 | 282 | 82.1 ± 7.2 | 43.3% | 26.6 ± 5.1 | 28.7% | 28.4% | 39.0% | 70.9% | 0.0% | 0.0% | yes | 256 |
| Hagar | 2023 | 68 | 81.0 ± 7.0 | 47.1% | 26.6 ± 4.5 | 22.0% | - | 63.0% | 82.0% | 22.0% | 1.0% | no | 288 |
| Khan | 2023 | 192 | 82.0 ± 6.0 | 61.0% | - | - | - | - | - | 2.6% | 21.0% | - | 64 |
| Kondoleon | 2023 | 2211 | 79.2 ± 8.5 | 53.4% | 29.0 ± 7.4 | 33.3% | 39.3% | - | 87.6% | 0.0% | 16.1% | - | max. 256 |
| Lecomte | 2023 | 206 | 80.6 ± 6.1 | 44.7% | 26.7 ± 4.6 | - | 20.0% | - | - | 0.0% | 0.0% | no | 256 |
| Renker | 2023 | 192 | 81.9 | 36.5% | 26.8 | 26.6% | 42.2% | 25.0% | 94.8% | 0.0% | 0.0% | no | 64 and 192 |
| Sasaki | 2023 | 21 | 86.0 ± 4.0 | 38.0% | 21.6 ± 3.1 | 38.1% | - | 57.1% | 95.2% | 14.3% | 0.0% | no | 192 |
| Study | Year | N | TPs | TNs | FPs | FNs |
|---|---|---|---|---|---|---|
| Pontone | 2011 | 60 | 23 | 30 | 4 | 3 |
| Andreini | 2014 | 325 | 87 | 207 | 21 | 10 |
| Harris | 2014 | 100 | 72 | 15 | 12 | 1 |
| Hamdan | 2015 | 115 | 47 | 48 | 18 | 2 |
| Matsumoto | 2017 | 60 | 22 | 21 | 15 | 2 |
| Rossi | 2017 | 140 | 53 | 45 | 37 | 5 |
| Annoni | 2018 | 115 | 22 | 80 | 12 | 1 |
| Strong | 2019 | 200 | 69 | 76 | 55 | 0 |
| Schicchi | 2020 | 223 | 44 | 158 | 20 | 1 |
| Shuai | 2020 | 121 | 28 | 81 | 11 | 1 |
| Opolski | 2021 | 475 | 265 | 76 | 129 | 5 |
| van den Boogert * | 2021 | 1060 | 296 | 536 | 217 | 11 |
| Bradt | 2022 | 95 | 27 | 47 | 18 | 3 |
| Gohmann | 2022 | 388 | 135 | 113 | 137 | 3 |
| Malebranche | 2022 | 100 | 30 | 8 | 62 | 0 |
| Peper | 2022 | 338 | 50 | 176 | 97 | 15 |
| Zhang | 2022 | 88 | 24 | 57 | 7 | 0 |
| Boyer | 2023 | 282 | 43 | 211 | 23 | 5 |
| Hagar | 2023 | 68 | 23 | 37 | 7 | 1 |
| Khan | 2023 | 192 | 21 | 142 | 26 | 3 |
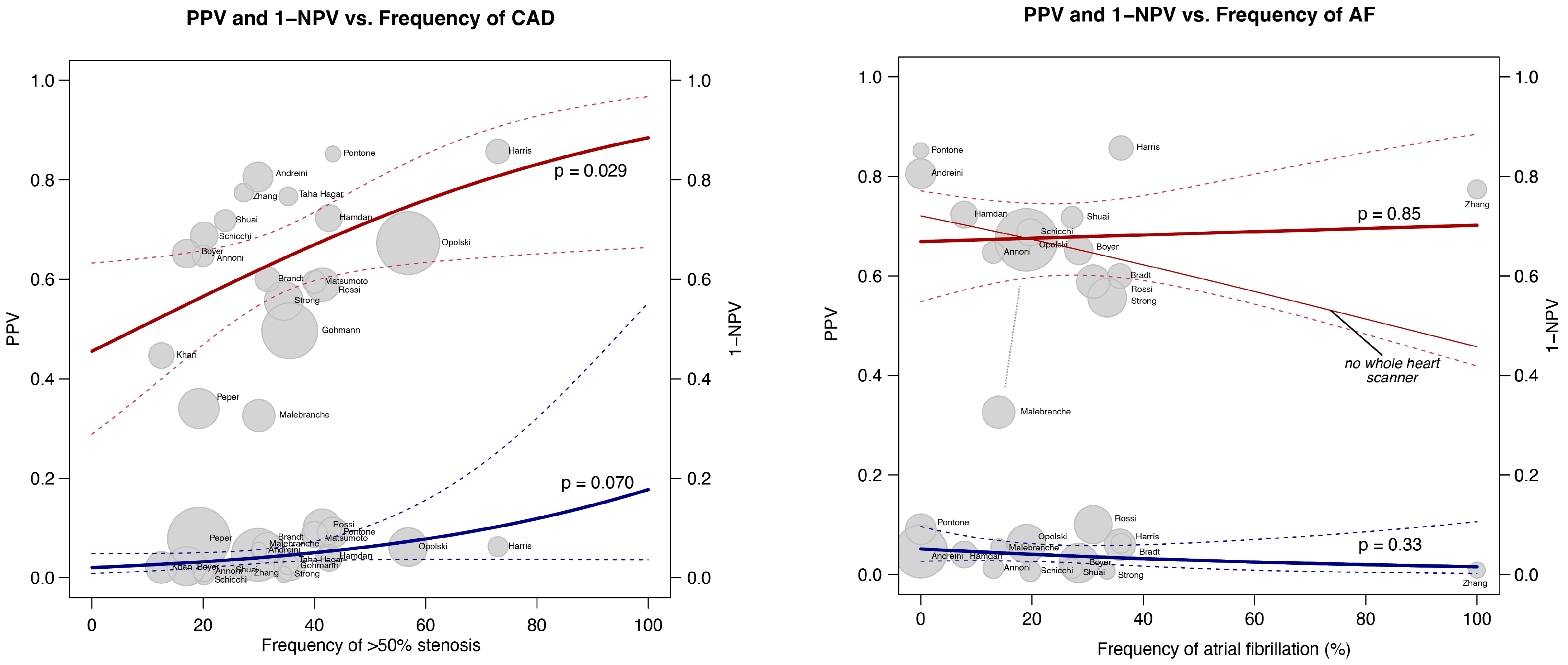
| Variable | Sens Estimate | Sens p-Value | Spec Estimate | Spec p-Value | PPV Estimate | PPV p-Value | NPV Estimate | NPV p-Value |
|---|---|---|---|---|---|---|---|---|
| Study Year | 0.043 | 0.912 | −0.772 | 0.572 | −2.616 | 0.001 | 0.323 | 0.157 |
| Frequency of >50% stenosis | 0.181 | 0.006 | −0.800 | 0.013 | 0.473 | 0.029 | −0.122 | 0.070 |
| Prev. PCI (0/1) | 0.073 | 0.143 | 0.047 | 0.860 | 0.309 | 0.046 | −0.008 | 0.841 |
| Prev. CABG (0/1) | 0.108 | 0.280 | 0.143 | 0.745 | 0.635 | 0.007 | 0.010 | 0.886 |
| Atrial fibrillation (0/1) | 0.049 | 0.315 | 0.085 | 0.752 | 0.033 | 0.845 | 0.035 | 0.328 |
| Males (%) | 0.020 | 0.898 | 1.023 | 0.062 | 0.633 | 0.120 | 0.083 | 0.341 |
| Age (years) | −0.319 | 0.552 | −2.747 | 0.074 | −1.956 | 0.134 | −0.403 | 0.167 |
| BMI (kg/m2) | 0.325 | 0.708 | −3.672 | 0.141 | −2.264 | 0.257 | −0.048 | 0.923 |
| Diab. Mel. (%) | 0.025 | 0.928 | −0.548 | 0.522 | −0.297 | 0.672 | 0.053 | 0.746 |
| Hypercholesterolaemia (%) | 0.169 | 0.153 | −0.251 | 0.353 | 0.134 | 0.553 | 0.011 | 0.852 |
| Hypertension (%) | 8.952 | 0.450 | −53.277 | 0.008 | −14.830 | 0.527 | −6.165 | 0.239 |
| Betablocker (0/1) | −8.206 | 0.001 | 13.269 | 0.177 | 3.300 | 0.687 | −2.081 | 0.149 |
| CT slices | −0.009 | 0.582 | 0.066 | 0.216 | 0.002 | 0.960 | 0.004 | 0.592 |
| CT whole heart coverage (0/1) | −2.493 | 0.354 | 20.937 | 0.020 | 1.853 | 0.804 | 1.271 | 0.400 |
| Prevalence | CT Suggests CAD–ICA Neg. | CT Suggests no CAD–ICA Pos. | CT Suggests CAD–ICA Confirmed | CT Suggests no CAD–ICA Confirmed | % Correct |
|---|---|---|---|---|---|
| 5% | 25.8% (95% CI: 17.7–35.9%) | 0.2% (95% CI: 0.1–0.4%) | 4.8% (95% CI: 4.6–4.9%) | 69.2% (95% CI: 59.1–77.3%) | 74.0% |
| 10% | 24.5% (95% CI: 16.8–34.0%) | 0.5% (95% CI: 0.3–0.7%) | 9.5% (95% CI: 9.3–9.7%) | 65.5% (95% CI: 56.0–73.2%) | 75.0% |
| 20% | 21.7% (95% CI: 14.9–30.2%) | 0.9% (95% CI: 0.6–1.5%) | 19.1% (95% CI: 18.5–19.4%) | 58.3% (95% CI: 49.8–65.1%) | 77.4% |
| 30% | 19.0% (95% CI: 13.0–26.5%) | 1.4% (95% CI: 0.9–2.2%) | 28.6% (95% CI: 27.8–29.1%) | 51.0% (95% CI: 43.5–57.0%) | 79.6% |
| 40% | 16.3% (95% CI: 11.2–22.7%) | 1.8% (95% CI: 1.1–2.9%) | 38.2% (95% CI: 37.1–38.9%) | 43.7% (95% CI: 37.3–48.8%) | 81.9% |
| 50% | 13.6% (95% CI: 9.3–18.9%) | 2.3% (95% CI: 1.4–3.7%) | 47.7% (95% CI: 46.3–48.6%) | 36.4% (95% CI: 31.1–40.7%) | 84.1% |
| 60% | 10.9% (95% CI: 7.5–15.1%) | 2.8% (95% CI: 1.7–4.4%) | 57.2% (95% CI: 55.6–58.3%) | 29.1% (95% CI: 24.9–32.5%) | 86.3% |
| 70% | 8.2% (95% CI: 5.6–11.3%) | 3.2% (95% CI: 2–5.1%) | 66.8% (95% CI: 64.9–68%) | 21.8% (95% CI: 18.7–24.4%) | 88.6% |
| false positives | false negatives | true positives | true negatives |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diller, G.-P.; Gerwing, M.; Boroni Grazioli, S.; De-Torres-Alba, F.; Radke, R.M.; Vormbrock, J.; Baumgartner, H.; Kaleschke, G.; Orwat, S. Utility of Coronary Computed Tomography Angiography in Patients Undergoing Transcatheter Aortic Valve Implantation: A Meta-Analysis and Meta-Regression Based on Published Data from 7458 Patients. J. Clin. Med. 2024, 13, 631. https://doi.org/10.3390/jcm13020631
Diller G-P, Gerwing M, Boroni Grazioli S, De-Torres-Alba F, Radke RM, Vormbrock J, Baumgartner H, Kaleschke G, Orwat S. Utility of Coronary Computed Tomography Angiography in Patients Undergoing Transcatheter Aortic Valve Implantation: A Meta-Analysis and Meta-Regression Based on Published Data from 7458 Patients. Journal of Clinical Medicine. 2024; 13(2):631. https://doi.org/10.3390/jcm13020631
Chicago/Turabian StyleDiller, Gerhard-Paul, Mirjam Gerwing, Simona Boroni Grazioli, Fernando De-Torres-Alba, Robert M. Radke, Julia Vormbrock, Helmut Baumgartner, Gerrit Kaleschke, and Stefan Orwat. 2024. "Utility of Coronary Computed Tomography Angiography in Patients Undergoing Transcatheter Aortic Valve Implantation: A Meta-Analysis and Meta-Regression Based on Published Data from 7458 Patients" Journal of Clinical Medicine 13, no. 2: 631. https://doi.org/10.3390/jcm13020631
APA StyleDiller, G.-P., Gerwing, M., Boroni Grazioli, S., De-Torres-Alba, F., Radke, R. M., Vormbrock, J., Baumgartner, H., Kaleschke, G., & Orwat, S. (2024). Utility of Coronary Computed Tomography Angiography in Patients Undergoing Transcatheter Aortic Valve Implantation: A Meta-Analysis and Meta-Regression Based on Published Data from 7458 Patients. Journal of Clinical Medicine, 13(2), 631. https://doi.org/10.3390/jcm13020631






