Using Three-Dimensional Printing Technology to Solve Complex Primary Total Hip Arthroplasty Cases: Do We Really Need Custom-Made Guides and Templates? A Critical Systematic Review on the Available Evidence
Abstract
1. Introduction
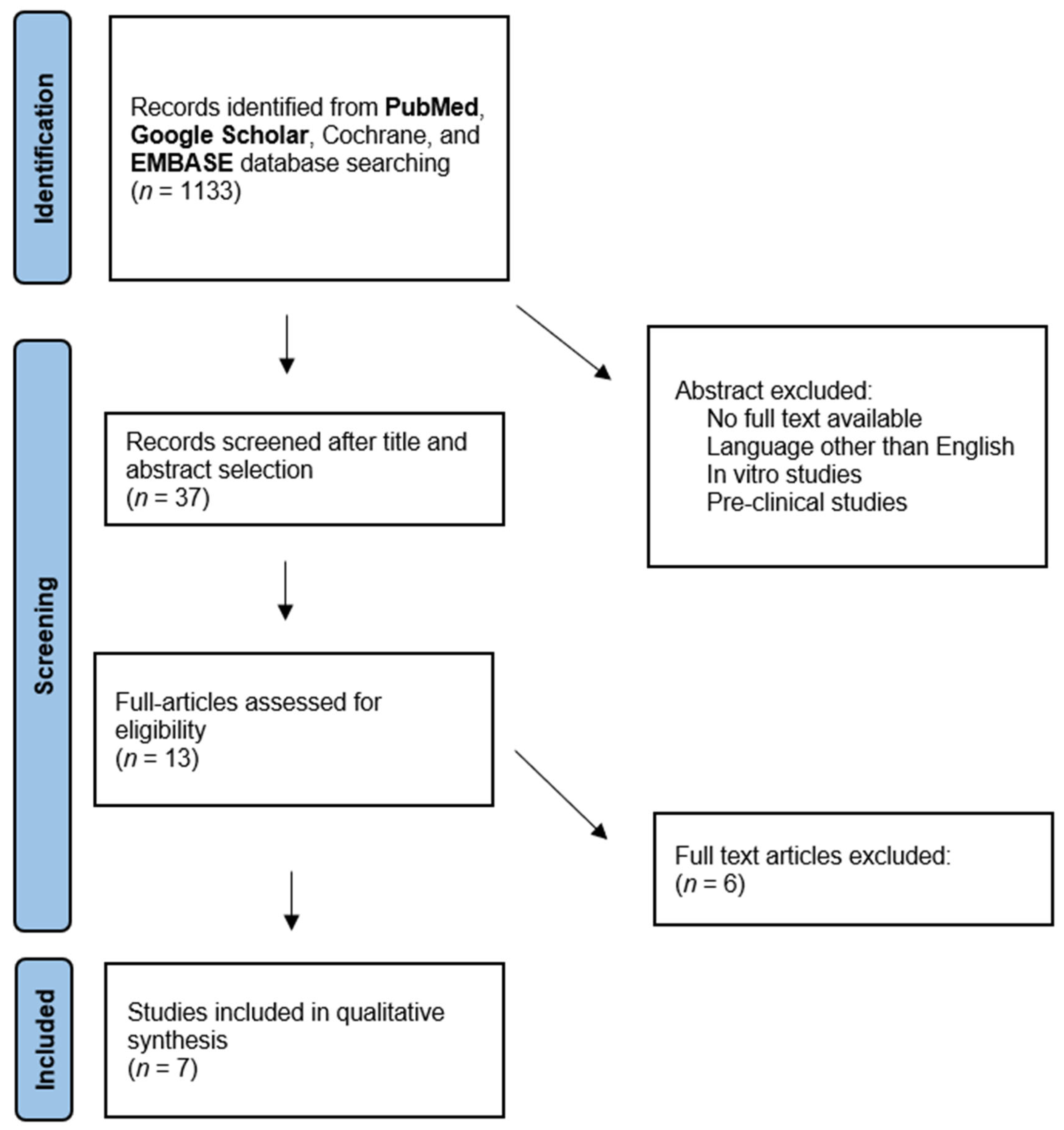
2. Materials and Methods
3. Results
3.1. Quality Assessment of the Retrieved Studies
3.2. 3D-Printed Surgical Guides
3.3. 3D-Printed Models for Surgical Simulations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hall, M.; van der Esch, M.; Hinman, R.S.; Peat, G.; de Zwart, A.; Quicke, J.G.; Runhaar, J.; Knoop, J.; van der Leeden, M.; de Rooij, M.; et al. How Does Hip Osteoarthritis Differ from Knee Osteoarthritis? Osteoarthr. Cartil. 2022, 30, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Li, X.; Zhu, Z.; Wang, H.; Yu, Z.; Bai, X. Effects of Progressive Resistance Training for Early Postoperative Fast-Track Total Hip or Knee Arthroplasty: A Systematic Review and Meta-Analysis. Asian J. Surg. 2021, 44, 1245–1253. [Google Scholar] [CrossRef] [PubMed]
- Scardino, M.; Di Matteo, B.; De Angelis, A.; Anzillotti, G.; Martorelli, F.; Simili, V.; Monteleone, G.; Bovio, M.; Tasso, F.; Laino, M.E.; et al. Clinical Efficacy of Implementing a Patient Blood Management (PBM) Protocol in Joint Replacement Surgery: A Retrospective Cohort Study in a National Referral Center. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 9221–9229. [Google Scholar] [CrossRef] [PubMed]
- Anzillotti, G.; Conte, P.; Di Matteo, B.; Bertolino, E.M.; Marcacci, M.; Kon, E. Injection of Biologic Agents for Treating Severe Knee Osteoarthritis: Is There a Chance for a Good Outcome? A Systematic Review of Clinical Evidence. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 5447–5459. [Google Scholar] [CrossRef]
- Learmonth, I.D.; Young, C.; Rorabeck, C. The Operation of the Century: Total Hip Replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef] [PubMed]
- Lan, R.H.; Yu, J.; Samuel, L.T.; Pappas, M.A.; Brooks, P.J.; Kamath, A.F. How Are We Measuring Cost-Effectiveness in Total Joint Arthroplasty Studies? Systematic Review of the Literature. J. Arthroplast. 2020, 35, 3364–3374. [Google Scholar] [CrossRef]
- Tilbury, C.; Schaasberg, W.; Plevier, J.W.M.; Fiocco, M.; Nelissen, R.G.H.H.; Vliet Vlieland, T.P.M. Return to Work after Total Hip and Knee Arthroplasty: A Systematic Review. Rheumatology 2014, 53, 512–525. [Google Scholar] [CrossRef]
- Ng, N.; Gaston, P.; Simpson, P.M.; Macpherson, G.J.; Patton, J.T.; Clement, N.D. Robotic Arm-Assisted versus Manual Total Hip Arthroplasty: A Systematic Review and Meta-Analysis. Bone Jt. J. 2021, 103-B, 1009–1020. [Google Scholar] [CrossRef]
- Moerenhout, K.; Derome, P.; Laflamme, G.Y.; Leduc, S.; Gaspard, H.S.; Benoit, B. Direct Anterior versus Posterior Approach for Total Hip Arthroplasty: A Multicentre, Prospective, Randomized Clinical Trial. Can. J. Surg. 2020, 63, E412–E417. [Google Scholar] [CrossRef]
- Jamari, J.; Ammarullah, M.I.; Saad, A.P.M.; Syahrom, A.; Uddin, M.; van der Heide, E.; Basri, H. The Effect of Bottom Profile Dimples on the Femoral Head on Wear in Metal-on-Metal Total Hip Arthroplasty. J. Funct. Biomater. 2021, 12, 38. [Google Scholar] [CrossRef]
- Ammarullah, M.I.; Hartono, R.; Supriyono, T.; Santoso, G.; Sugiharto, S.; Permana, M.S. Polycrystalline Diamond as a Potential Material for the Hard-on-Hard Bearing of Total Hip Prosthesis: Von Mises Stress Analysis. Biomedicines 2023, 11, 951. [Google Scholar] [CrossRef] [PubMed]
- Tauviqirrahman, M.; Ammarullah, M.I.; Jamari, J.; Saputra, E.; Winarni, T.I.; Kurniawan, F.D.; Shiddiq, S.A.; van der Heide, E. Analysis of Contact Pressure in a 3D Model of Dual-Mobility Hip Joint Prosthesis under a Gait Cycle. Sci. Rep. 2023, 13, 3564. [Google Scholar] [CrossRef] [PubMed]
- Tack, P.; Victor, J.; Gemmel, P.; Annemans, L. 3D-Printing Techniques in a Medical Setting: A Systematic Literature Review. Biomed. Eng. Online 2016, 15, 115. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Zhu, H.; Gao, C. A Systematic Review and Meta-Analysis of 3D Printing Technology for the Treatment of Acetabular Fractures. BioMed Res. Int. 2021, 2021, 5018791. [Google Scholar] [CrossRef] [PubMed]
- Papotto, G.; Testa, G.; Mobilia, G.; Perez, S.; Dimartino, S.; Giardina, S.M.C.; Sessa, G.; Pavone, V. Use of 3D Printing and Pre-Contouring Plate in the Surgical Planning of Acetabular Fractures: A Systematic Review. Orthop. Traumatol. Surg. Res. 2022, 108, 103111. [Google Scholar] [CrossRef] [PubMed]
- Aman, Z.S.; DePhillipo, N.N.; Peebles, L.A.; Familiari, F.; LaPrade, R.F.; Dekker, T.J. Improved Accuracy of Coronal Alignment Can Be Attained Using 3D-Printed Patient-Specific Instrumentation for Knee Osteotomies: A Systematic Review of Level III and IV Studies. Arthroscopy 2022, 38, 2741–2758. [Google Scholar] [CrossRef]
- Duan, X.; Wang, B.; Yang, L.; Kadakia, A.R. Applications of 3D Printing Technology in Orthopedic Treatment. BioMed Res. Int. 2021, 2021, 9892456. [Google Scholar] [CrossRef]
- Jiang, M.; Coles-Black, J.; Chen, G.; Alexander, M.; Chuen, J.; Hardidge, A. 3D Printed Patient-Specific Complex Hip Arthroplasty Models Streamline the Preoperative Surgical Workflow: A Pilot Study. Front. Surg. 2021, 8, 687379. [Google Scholar] [CrossRef]
- Segaran, N.; Saini, G.; Mayer, J.L.; Naidu, S.; Patel, I.; Alzubaidi, S.; Oklu, R. Application of 3D Printing in Preoperative Planning. J. Clin. Med. 2021, 10, 917. [Google Scholar] [CrossRef]
- Zhang, R.; Lin, J.; Chen, F.; Liu, W.; Chen, M. Clinical and Radiological Outcomes in Three-Dimensional Printing Assisted Revision Total Hip and Knee Arthroplasty: A Systematic Review. J. Orthop. Surg. Res. 2021, 16, 495. [Google Scholar] [CrossRef]
- Yan, L.; Wang, P.; Zhou, H. 3D Printing Navigation Template Used in Total Hip Arthroplasty for Developmental Dysplasia of the Hip. Indian J. Orthop. 2020, 54, 856–862. [Google Scholar] [CrossRef] [PubMed]
- Tu, Q.; Ding, H.-W.; Chen, H.; Shen, J.-J.; Miao, Q.-J.; Liu, B.; Yu, G.-W.; Huang, X.-H.; Zhu, C.-R.; Tang, Y.; et al. Preliminary Application of 3D-Printed Individualised Guiding Templates for Total Hip Arthroplasty in Crowe Type IV Developmental Dysplasia of the Hip. Hip Int. 2022, 32, 334–344. [Google Scholar] [CrossRef]
- Mishra, A.; Verma, T.; Rajkumar Agarwal, G.; Sharma, A.; Maini, L. 3D Printed Patient-Specific Acetabular Jig for Cup Placement in Total Hip Arthroplasty. Indian J. Orthop. 2020, 54, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Hananouchi, T.; Saito, M.; Koyama, T.; Sugano, N.; Yoshikawa, H. Tailor-Made Surgical Guide Reduces Incidence of Outliers of Cup Placement. Clin. Orthop. Relat. Res. 2010, 468, 1088–1095. [Google Scholar] [CrossRef][Green Version]
- Xu, J.; Li, D.; Ma, R.; Barden, B.; Ding, Y. Application of Rapid Prototyping Pelvic Model for Patients with DDH to Facilitate Arthroplasty Planning: A Pilot Study. J. Arthroplast. 2015, 30, 1963–1970. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Guan, J.-Z.; Zhang, Z.; Chen, X.-T.; Ma, X.-D.; Zhao, J.-N.; Zhou, J.-S. Restoring Rotation Center in Total Hip Arthroplasty for Developmental Dysplasia of the Hip with the Assistance of Three Dimensional Printing Technology: A Pilot Study. Orthop. Surg. 2022, 14, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomised Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Palmara, G.; Frascella, F.; Roppolo, I.; Chiappone, A.; Chiadò, A. Functional 3D Printing: Approaches and Bioapplications. Biosens. Bioelectron. 2021, 175, 112849. [Google Scholar] [CrossRef]
- Meng, M.; Wang, J.; Huang, H.; Liu, X.; Zhang, J.; Li, Z. 3D Printing Metal Implants in Orthopedic Surgery: Methods, Applications and Future Prospects. J. Orthop. Transl. 2023, 42, 94–112. [Google Scholar] [CrossRef]
- Ballard, D.H.; Mills, P.; Duszak, R.; Weisman, J.A.; Rybicki, F.J.; Woodard, P.K. Medical 3D Printing Cost-Savings in Orthopedic and Maxillofacial Surgery: Cost Analysis of Operating Room Time Saved with 3D Printed Anatomic Models and Surgical Guides. Acad. Radiol. 2020, 27, 1103–1113. [Google Scholar] [CrossRef] [PubMed]
- Chen, H. Application Progress of Artificial Intelligence and Augmented Reality in Orthopaedic Arthroscopy Surgery. J. Orthop. Surg. Res. 2023, 18, 775. [Google Scholar] [CrossRef] [PubMed]
- Crowe, J.F.; Mani, V.J.; Ranawat, C.S. Total Hip Replacement in Congenital Dislocation and Dysplasia of the Hip. J. Bone Jt. Surg. Am. 1979, 61, 15–23. [Google Scholar] [CrossRef]
- Loppini, M.; Longo, U.G.; Caldarella, E.; Rocca, A.D.; Denaro, V.; Grappiolo, G. Femur First Surgical Technique: A Smart Non-Computer-Based Procedure to Achieve the Combined Anteversion in Primary Total Hip Arthroplasty. BMC Musculoskelet. Disord. 2017, 18, 331. [Google Scholar] [CrossRef] [PubMed]
- Mouri, K.; Madachi, A.; Karita, T. Intraoperative Pelvic Tilt and Axial Rotation During Total Hip Arthroplasty Through the Direct Anterior Approach Is Affected by the Acetabular Retractor and Cup Impactor. Arthroplast. Today 2023, 24, 101251. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.L.; Kurtz, S.M.; Lau, E.; Bozic, K.J.; Berry, D.J.; Parvizi, J. Prosthetic Joint Infection Risk after Total Hip Arthroplasty in the Medicare Population. J. Arthroplast. 2009, 24, 105–109. [Google Scholar] [CrossRef]
- Phillips, J.E.; Crane, T.P.; Noy, M.; Elliott, T.S.J.; Grimer, R.J. The Incidence of Deep Prosthetic Infections in a Specialist Orthopaedic Hospital: A 15-Year Prospective Survey. J. Bone Jt. Surg. Br. 2006, 88, 943–948. [Google Scholar] [CrossRef]
- Blom, A.W.; Taylor, A.H.; Pattison, G.; Whitehouse, S.; Bannister, G.C. Infection after Total Hip Arthroplasty. The Avon Experience. J. Bone Jt. Surg. Br. 2003, 85, 956–959. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Lau, E.C.; Son, M.-S.; Chang, E.T.; Zimmerli, W.; Parvizi, J. Are We Winning or Losing the Battle With Periprosthetic Joint Infection: Trends in Periprosthetic Joint Infection and Mortality Risk for the Medicare Population. J. Arthroplast. 2018, 33, 3238–3245. [Google Scholar] [CrossRef]
- Premkumar, A.; Kolin, D.A.; Farley, K.X.; Wilson, J.M.; McLawhorn, A.S.; Cross, M.B.; Sculco, P.K. Projected Economic Burden of Periprosthetic Joint Infection of the Hip and Knee in the United States. J. Arthroplast. 2021, 36, 1484–1489.e3. [Google Scholar] [CrossRef]
| Risk of Bias Domains | |||||||
|---|---|---|---|---|---|---|---|
| D1 | D2 | D3 | D4 | D5 | Overall | ||
| Study | Yan et al. (2020) [21] |  |  |  |  |  |  |
| Mishra et al. (2020) [23] |  |  |  |  |  |  | |
 , Some concerns;
, Some concerns;  , Low.
, Low.| Author (Year Pub) | Baseline Confounding | Selection of Participants | Classification of Intervention | Deviation from Intended Intervention | Missing Data | Measurement of Outcomes | Selection of Reported Results | Overall Risk of Bias |
|---|---|---|---|---|---|---|---|---|
| Tu et al. [22] (2020) | Low | Low | Low | Low | No information | Low | Low | Low |
| Hananouchi et al. [24] (2010) | Moderate | Moderate | Moderate | Low | Low | Moderate | Moderate | Serious |
| Zhang et al. [26] (2021) | Low | Low | Low | Low | No information | Moderate | Low | Moderate |
| Jiang et al. [18] (2021) | Moderate | Serious | Low | Low | No information | Low | Moderate | Low |
| Xu et al. [25] (2015) | Low | Moderate | Low | Low | No information | Low | Moderate | Moderate |
| Author (Year) | Design | Number of Patients | Type of 3D-Printed Device | Disease | Follow-Up | Outcome Measures | Results |
|---|---|---|---|---|---|---|---|
| Yan et al. [21] 2020 | RCT | 12 with 3D-printed guides vs. 13 without | PLA 3D-printed acetabular guiding | DDH (Crowe II–IV) | 1.6 years (1.2–3.8) | Operation time, intraoperative hemorrhage, postoperative drainage, infection, loosening, HHS acetabular position with CT scan, distance from COR to ischial tuberosity | Lower operation time, blood loss *, and higher HHS at 6 months in the 3D-printed group. More precise replication of contralateral acetabular angles in the 3D-printed group |
| Tu et al. [22] 2020 | Prospective | 12 | Resin 3D-printed guiding template for cup position and femoral osteotomy | DDH (Crowe IV) | 72.42 months (38–135) | HHS, leg length discrepancy, visual analog scale scores | Improvements in HHS *, LLD *, and VAS * |
| Mishra et al. [23] 2020 | RCT | 36: 18 3D-aided vs. 18 conventional cup placement | PLA 3D-printed acetabular jig for guiding cup placement | Complex anatomy | - | Blood loss, total surgical duration, surgical duration of cup placementCup angle of inclination, angle of anteversion, differences in acetabular offset and hip length | No significant differences in blood loss and surgical timings No significant differences in accuracy of cup placement but less variability and outliers in 3D-aided group |
| Hananouchi et al. [24] 2010 | Case–control | 31 with surgical guides vs. 38 without | Resin 3D-printed surgical guide | OA | - | Alignment accuracy, operating time, total blood loss | The surgical guide provided more reliable cup insertion compared with conventional techniques. No differences in total blood loss or operating time |
| Author (Year) | Material | Cost of Software | Costs Cost of the 3D Printer | Cost of Material/Case |
|---|---|---|---|---|
| Yan et al. [21] 2020 | PLA 3D-printed acetabular guides | - | - | - |
| Tu et al. [22] 2020 | Resin 3D-printed guiding template for cup positioning and femoral osteotomy | - | - | USD 100 |
| Mishra et al. [23] 2020 | PLA 3D-printed acetabular jig for cup placement | - | - | USD 4–USD 6 |
| Hananouchi et al. [24] 2010 | Resin 3D-printed surgical guide | USD 15,000–USD 30,000 | USD 120,000 | USD 50–USD 100 |
| Zhang et al. [26] 2021 | PLA life-sized 3D-printed template for surgical simulation | - | - | - |
| Jiang et al. [18] 2021 | Plaster, resin, and nylon 3D-printed acetabular models | Outsourced | Outsourced | Plaster: USD 200 Resin: USD 1500 Nylon: USD 100 |
| Xu et al. [25] 2015 | 3D-printed model for preoperative surgical simulation made of fluid-binding substances and ink | - | - | USD 400 |
| Author (Year) | Design | Number of Patients | Type of 3D-Printed Device | Disease | Follow-Up | Outcome Measures | Results |
|---|---|---|---|---|---|---|---|
| Zhang et al. [26] 2021 | Retrospective | 17 patients/21 hips | PLA life-sized 3D-printed template for surgical simulation | DDH | 18.35 ± 6.86 months | Preoperative and postoperative hip rotation center data measurement on pelvis plain films, bone defect area, and HHS | High rate of accordance in the sizes of the acetabular component and the bone defect between preoperative planning on the 3D print model and THA. Improvement of HHS * |
| Jiang et al. [18] 2021 | Pilot Study with Surgical Simulation | 7 | Plaster, resin, and nylon 3D-printed acetabular models | Complex pelvic fractures, Perthes disease, DDH, OA with substantial bone loss | - | Changes in cup size, changes in surgical plan, comparison of different materials | Simulation with patient-specific 3D-printed models conferred superior clinical, logistical, and educational outcomes compared to CT and X-rays. Furthermore, it streamlined equipment selection and revealed potential complications |
| Xu et al. [25] 2015 | Prospective | 10 patients (14 hips) | 3D-printed model for preoperative surgical simulation | DDH | 23.1 ± 5.9 months (14–30) | HHS, LLD, cup coverage, hip center location, cup migration, cup sizing coincidence (ICC) | No surgical complications. Improvement of HHS *, no perceptible LLD, 83% average bone coverage, no cup migrations, all implants clinically and radiographically stable. Better sizing prediction in 3D planning compared to 2D planning * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anzillotti, G.; Guazzoni, E.; Conte, P.; Di Matteo, V.; Kon, E.; Grappiolo, G.; Loppini, M. Using Three-Dimensional Printing Technology to Solve Complex Primary Total Hip Arthroplasty Cases: Do We Really Need Custom-Made Guides and Templates? A Critical Systematic Review on the Available Evidence. J. Clin. Med. 2024, 13, 474. https://doi.org/10.3390/jcm13020474
Anzillotti G, Guazzoni E, Conte P, Di Matteo V, Kon E, Grappiolo G, Loppini M. Using Three-Dimensional Printing Technology to Solve Complex Primary Total Hip Arthroplasty Cases: Do We Really Need Custom-Made Guides and Templates? A Critical Systematic Review on the Available Evidence. Journal of Clinical Medicine. 2024; 13(2):474. https://doi.org/10.3390/jcm13020474
Chicago/Turabian StyleAnzillotti, Giuseppe, Edoardo Guazzoni, Pietro Conte, Vincenzo Di Matteo, Elizaveta Kon, Guido Grappiolo, and Mattia Loppini. 2024. "Using Three-Dimensional Printing Technology to Solve Complex Primary Total Hip Arthroplasty Cases: Do We Really Need Custom-Made Guides and Templates? A Critical Systematic Review on the Available Evidence" Journal of Clinical Medicine 13, no. 2: 474. https://doi.org/10.3390/jcm13020474
APA StyleAnzillotti, G., Guazzoni, E., Conte, P., Di Matteo, V., Kon, E., Grappiolo, G., & Loppini, M. (2024). Using Three-Dimensional Printing Technology to Solve Complex Primary Total Hip Arthroplasty Cases: Do We Really Need Custom-Made Guides and Templates? A Critical Systematic Review on the Available Evidence. Journal of Clinical Medicine, 13(2), 474. https://doi.org/10.3390/jcm13020474







