Clinical and Radiographic Outcomes of Single Implant-Supported Zirconia Crowns Following a Digital and Conventional Workflow: Four-Year Follow-Up of a Randomized Controlled Clinical Trial
Abstract
1. Introduction
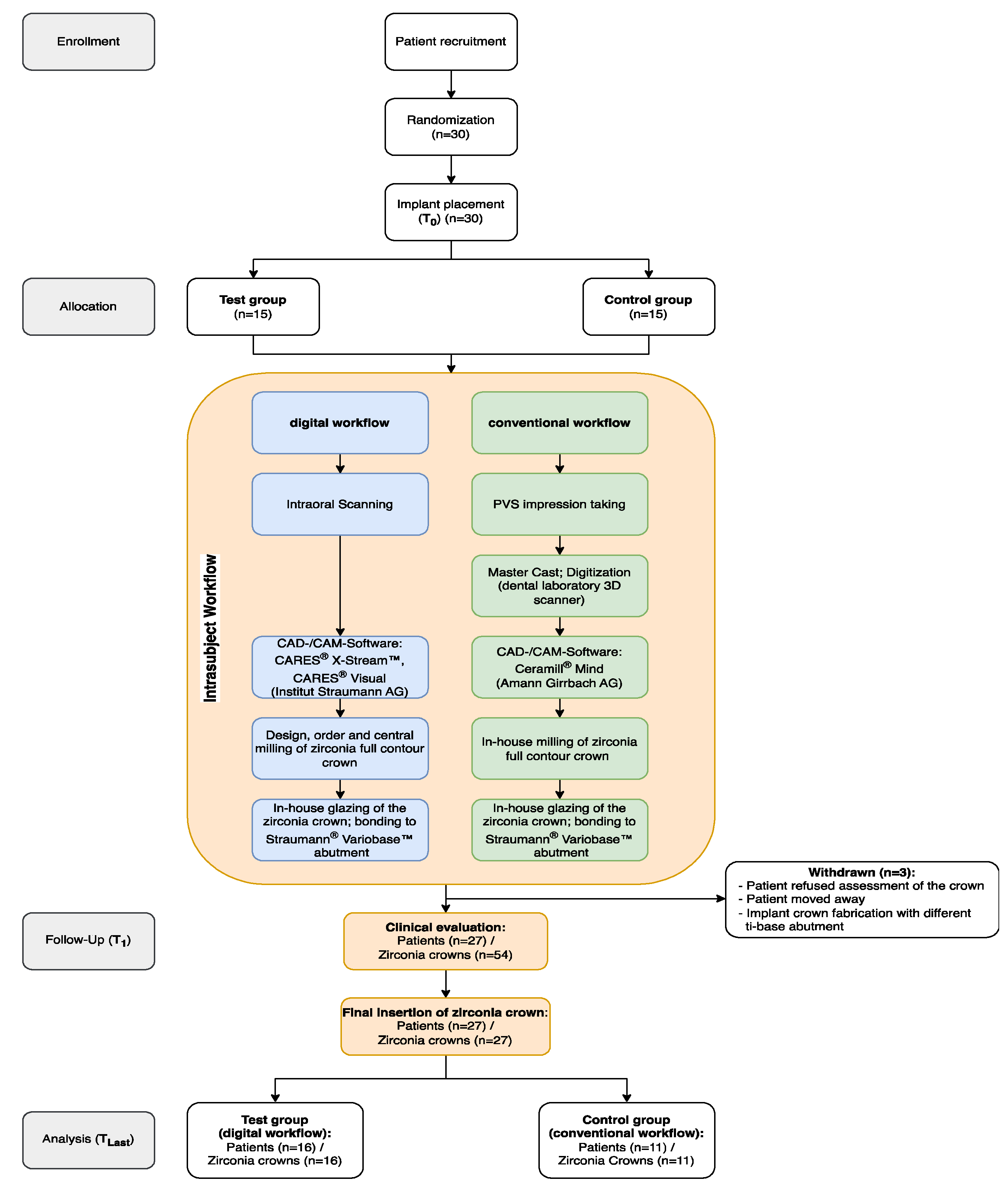
2. Materials and Methods
2.1. Study Design and Population
2.2. Surgical Procedure
2.3. Digital Workflow (Test Group)
2.4. Conventional Workflow (Control Group)
2.5. Outcomes
2.5.1. Clinical Evaluation of the Implant Crown
2.5.2. Patients’ Perception of the Digital/Conventional Impression Taking and the Implant-Supported Solitary Crown (Questionnaire)
2.5.3. Measurement of the Marginal Bone Level (MBL)
2.5.4. Evaluation of Peri-Implant Health
2.5.5. Functional Implant Prosthodontic Score (FIPS)
2.6. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Clinical Adjustment
3.3. Patient Perception (Questionnaire)
3.4. Peri-Implant Health and Technical Complications
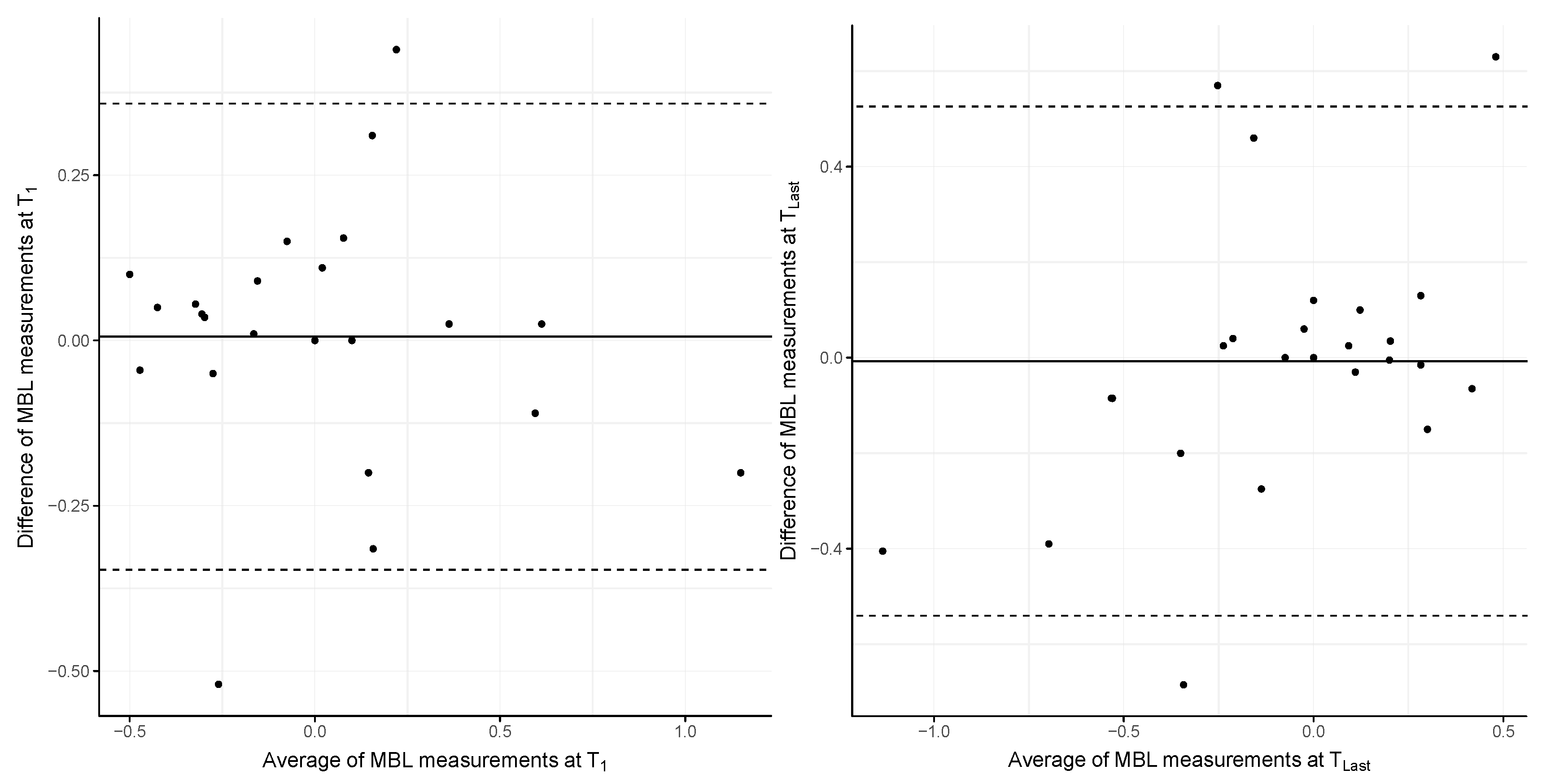
3.5. Marginal Bone Level
3.6. Functional Implant Prosthodontic Score (FIPS)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Joda, T.; Ferrari, M.; Gallucci, G.O.; Wittneben, J.-G.; Brägger, U. Digital technology in fixed implant prosthodontics. Periodontol. 2000 2017, 73, 178–192. [Google Scholar] [CrossRef]
- Suese, K. Progress in digital dentistry: The practical use of intraoral scanners. Dent. Mater. J. 2020, 39, 52–56. [Google Scholar] [CrossRef]
- Flügge, T.; van der Meer, W.J.; Gonzalez, B.G.; Vach, K.; Wismeijer, D.; Wang, P. The accuracy of different dental impression techniques for implant-supported dental prostheses: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29 (Suppl. S16), 374–392. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Vazouras, K.; Chen, Y.-W.; Kotina, E.; Natto, Z.; Kang, K.; Chochlidakis, K. Digital vs Conventional Implant Impressions: A Systematic Review and Meta-Analysis. J. Prosthodont. 2020, 29, 660–678. [Google Scholar] [CrossRef]
- Sanda, M.; Miyoshi, K.; Baba, K. Trueness and precision of digital implant impressions by intraoral scanners: A literature review. Int. J. Implant Dent. 2021, 7, 97. [Google Scholar] [CrossRef]
- Iturrate, M.; Amezua, X.; Garikano, X.; Solaberrieta, E. Use of measuring gauges for in vivo accuracy analysis of intraoral scanners: A pilot study. J. Adv. Prosthodont. 2021, 13, 191–204. [Google Scholar] [CrossRef]
- Mühlemann, S.; Lamperti, S.T.; Stucki, L.; Hämmerle, C.H.F.; Thoma, D.S. Time efficiency and efficacy of a centralized computer-aided-design/computer-aided-manufacturing workflow for implant crown fabrication: A prospective controlled clinical study. J. Dent. 2022, 127, 104332. [Google Scholar] [CrossRef]
- Pan, S.; Guo, D.; Zhou, Y.; Jung, R.E.; Hämmerle, C.H.F.; Mühlemann, S. Time efficiency and quality of outcomes in a model-free digital workflow using digital impression immediately after implant placement: A double-blind self-controlled clinical trial. Clin. Oral Implants Res. 2019, 30, 617–626. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Brägger, U. Time-efficiency analysis of the treatment with monolithic implant crowns in a digital workflow: A randomized controlled trial. Clin. Oral Implant. Res. 2016, 27, 1401–1406. [Google Scholar] [CrossRef] [PubMed]
- Bishti, S.; Tuna, T.; Rittich, A.; Wolfart, S. Patient-reported outcome measures (PROMs) of implant-supported reconstructions using digital workflows: A systematic review and meta-analysis. Clin. Oral Implants Res. 2021, 32 (Suppl. S21), 318–335. [Google Scholar] [CrossRef] [PubMed]
- Glisic, O.; Hoejbjerre, L.; Sonnesen, L. A comparison of patient experience, chair-side time, accuracy of dental arch measurements and costs of acquisition of dental models. Angle Orthod. 2019, 89, 868–875. [Google Scholar] [CrossRef]
- Derksen, W.; Tahmaseb, A.; Wismeijer, D. Randomized Clinical Trial comparing clinical adjustment times of CAD/CAM screw-retained posterior crowns on ti-base abutments created with digital or conventional impressions. One-year follow-up. Clin. Oral Implants Res. 2021, 32, 962–970. [Google Scholar] [CrossRef]
- Delize, V.; Bouhy, A.; Lambert, F.; Lamy, M. Intrasubject comparison of digital vs. conventional workflow for screw-retained single-implant crowns: Prosthodontic and patient-centered outcomes. Clin. Oral Implant. Res. 2019, 30, 892–902. [Google Scholar] [CrossRef]
- Zhang, Y.; Tian, J.; Wei, D.; Di, P.; Lin, Y. Quantitative clinical adjustment analysis of posterior single implant crown in a chairside digital workflow: A randomized controlled trial. Clin. Oral Implant. Res. 2019, 30, 1059–1066. [Google Scholar] [CrossRef]
- Derksen, W.; Wismeijer, D. Three-year follow-up of a Randomized Clinical Trial on screw-retained monolithic zirconia restorations on ti-base abutments based on digital or conventional impression techniques. Int. J. Prosthodont. 2023, 36, 410–415. [Google Scholar] [CrossRef]
- Zhang, Y.; Wei, D.; Tian, J.; Zhao, Y.; Lin, Y.; Di, P. Clinical evaluation and quantitative occlusal change analysis of posterior implant-supported all-ceramic crowns: A 3-year randomized controlled clinical trial. Clin. Oral Implant. Res. 2023, 34, 1188–1197. [Google Scholar] [CrossRef]
- Schindelin, J.; Arganda-Carreras, I.; Frise, E.; Kaynig, V.; Longair, M.; Pietzsch, T.; Preibisch, S.; Rueden, C.; Saalfeld, S.; Schmid, B.; et al. Fiji: An open-source platform for biological-image analysis. Nat. Methods 2012, 9, 676–682. [Google Scholar] [CrossRef]
- Marconcini, S.; Giammarinaro, E.; Covani, U.; Mijiritsky, E.; Vela, X.; Rodríguez, X. The effect of tapered abutments on marginal bone level: A retrospective cohort study. J. Clin. Med. 2019, 8, 1305. [Google Scholar] [CrossRef]
- Renvert, S.; Persson, G.R.; Pirih, F.Q.; Camargo, P.M. Peri-implant health, peri-implant mucositis, and peri-implantitis: Case definitions and diagnostic considerations. J. Clin. Periodontol. 2018, 45 (Suppl. S20), S278–S285. [Google Scholar] [CrossRef]
- Joda, T.; Zarone, F.; Zitzmann, N.U.; Ferrari, M. The Functional Implant Prosthodontic Score (FIPS): Assessment of reproducibility and observer variability. Clin. Oral Investig. 2018, 22, 2319–2324. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Betensky, R.A.; Gianneschi, G.E.; Gallucci, G.O. Accuracy of digital versus conventional implant impressions. Clin. Oral Implant. Res. 2015, 26, 715–719. [Google Scholar] [CrossRef] [PubMed]
- Guo, D.; Mühlemann, S.; Pan, S.; Zhou, Y.; Jung, R.E. A double-blind randomized within-subject study to evaluate clinical applicability of four digital workflows for the fabrication of posterior single implant crown. Clin. Oral Implants Res. 2023, 34, 1319–1329. [Google Scholar] [CrossRef]
- Edher, F.; Hannam, A.G.; Tobias, D.L.; Wyatt, C.C.L. The accuracy of virtual interocclusal registration during intraoral scanning. J. Prosthet. Dent. 2018, 120, 904–912. [Google Scholar] [CrossRef] [PubMed]
- Abdulateef, S.; Edher, F.; Hannam, A.G.; Tobias, D.L.; Wyatt, C.C.L. Clinical accuracy and reproducibility of virtual interocclusal records. J. Prosthet. Dent. 2020, 124, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Beck, F.; Lettner, S.; Zupancic Cepic, L.; Schedle, A. Comparison of Virtual Intersection and Occlusal Contacts between Intraoral and Laboratory Scans: An In-Vivo Study. J. Clin. Med. 2023, 12, 996. [Google Scholar] [CrossRef]
- Meng, J.C.; Nagy, W.W.; Wirth, C.G.; Buschang, P.H. The effect of equilibrating mounted dental stone casts on the occlusal harmony of cast metal complete crowns. J. Prosthet. Dent. 2010, 104, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Pariente, L.; Dada, K.; Daas, M.; Linder, S.; Dard, M. Evaluation of the Treatment of Partially Edentulous Patients with Bone Level Tapered Implants: 24-Month Clinical and Radiographic Follow-Up. J. Oral Implantol. 2020, 46, 407–413. [Google Scholar] [CrossRef]
- Joda, T.; Bragger, U.; Zitzmann, N.U. CAD/CAM implant crowns in a digital workflow: Five-year follow-up of a prospective clinical trial. Clin. Implant. Dent. Relat. Res. 2019, 21, 169–174. [Google Scholar] [CrossRef]
- Kunavisarut, C.; Jarangkul, W.; Pornprasertsuk-Damrongsri, S.; Joda, T. Patient-reported outcome measures (PROMs) comparing digital and conventional workflows for treatment with posterior single-unit implant restorations: A randomized controlled trial. J. Dent. 2022, 117, 103875. [Google Scholar] [CrossRef]
- Yavuz, A.; Büyükerkmen, E.B. Fracture Resistance of CAD/CAM Monolithic Zirconia Crowns Supported by Titanium and Ti-Base Abutments: The Effect of Chewing Simulation and Thermocyclic Aging. Int. J. Oral Maxillofac. Implant. 2023, 38, 328–333. [Google Scholar] [CrossRef]
- Sailer, I.; Karasan, D.; Todorovic, A.; Ligoutsikou, M.; Pjetursson, B.E. Prosthetic failures in dental implant therapy. Periodontol. 2000 2022, 88, 130–144. [Google Scholar] [CrossRef]
- Revilla-León, M.; Barmak, A.B.; Tohme, H.; Yilmaz, B.; Kois, J.C.; Gómez-Polo, M. Factors that influence the accuracy of maxillomandibular relationship at maximum intercuspation acquired by using intraoral scanners: A systematic review. J. Dent. 2023, 138, 104718. [Google Scholar] [CrossRef]


| Question | Outcome | p-Value | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Preference of impression technique | Digital (n = 9) | Conventional (n = 7) | No opinion (n = 11) | 0.375 | |||||||||||||||||||||
| (2) Satisfaction with implant crown’s esthetics | Yes (n = 26) | No (n = 1) | 0.407 | ||||||||||||||||||||||
| (3) Perform future impressions digitally | Yes (n = 10) | No (n = 2) | Maybe (n = 2) | n/a (n = 13) | 0.162 | ||||||||||||||||||||
| (4) Nausea during conventional impressions (NRS) | 1 (n = 13) | 2 (n = 2) | 3 (n = 4) | 5 (n = 1) | 6 (n = 4) | 7 (n = 2) | 8 (n = 1) | 0.372 | |||||||||||||||||
| (5) Discomfort in clinical step(s) (from implant placement to insertion of the crown) | None (n = 22) | Analog impression (n = 1) | Insertion of crown (n = 1) | Implant placement/ Impression (n = 1) | Implant placement/ impression/ insertion of crown (n = 1) | Other (n = 1) | 0.316 | ||||||||||||||||||
| (6) Importance of single posterior tooth gap rehabilitation (NRS) | 1 (n = 2) | 5 (n = 4) | 8 (n = 1) | 9 (n = 2) | 10 (n = 18) | 0.888 | |||||||||||||||||||
| (7) Recommendation of implant-supported zirconia crowns to friends | Yes (n = 26) | No (n = 1) | 0.407 | ||||||||||||||||||||||
| (8) Type of impression technique recommended to friends | Digital (n = 16) | Conventional (n = 7) | Both (n = 3) | None (n = 1) | 0.503 | ||||||||||||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beck, F.; Zupancic Cepic, L.; Lettner, S.; Moritz, A.; Ulm, C.; Zechner, W.; Schedle, A. Clinical and Radiographic Outcomes of Single Implant-Supported Zirconia Crowns Following a Digital and Conventional Workflow: Four-Year Follow-Up of a Randomized Controlled Clinical Trial. J. Clin. Med. 2024, 13, 432. https://doi.org/10.3390/jcm13020432
Beck F, Zupancic Cepic L, Lettner S, Moritz A, Ulm C, Zechner W, Schedle A. Clinical and Radiographic Outcomes of Single Implant-Supported Zirconia Crowns Following a Digital and Conventional Workflow: Four-Year Follow-Up of a Randomized Controlled Clinical Trial. Journal of Clinical Medicine. 2024; 13(2):432. https://doi.org/10.3390/jcm13020432
Chicago/Turabian StyleBeck, Florian, Lana Zupancic Cepic, Stefan Lettner, Andreas Moritz, Christian Ulm, Werner Zechner, and Andreas Schedle. 2024. "Clinical and Radiographic Outcomes of Single Implant-Supported Zirconia Crowns Following a Digital and Conventional Workflow: Four-Year Follow-Up of a Randomized Controlled Clinical Trial" Journal of Clinical Medicine 13, no. 2: 432. https://doi.org/10.3390/jcm13020432
APA StyleBeck, F., Zupancic Cepic, L., Lettner, S., Moritz, A., Ulm, C., Zechner, W., & Schedle, A. (2024). Clinical and Radiographic Outcomes of Single Implant-Supported Zirconia Crowns Following a Digital and Conventional Workflow: Four-Year Follow-Up of a Randomized Controlled Clinical Trial. Journal of Clinical Medicine, 13(2), 432. https://doi.org/10.3390/jcm13020432







