Abstract
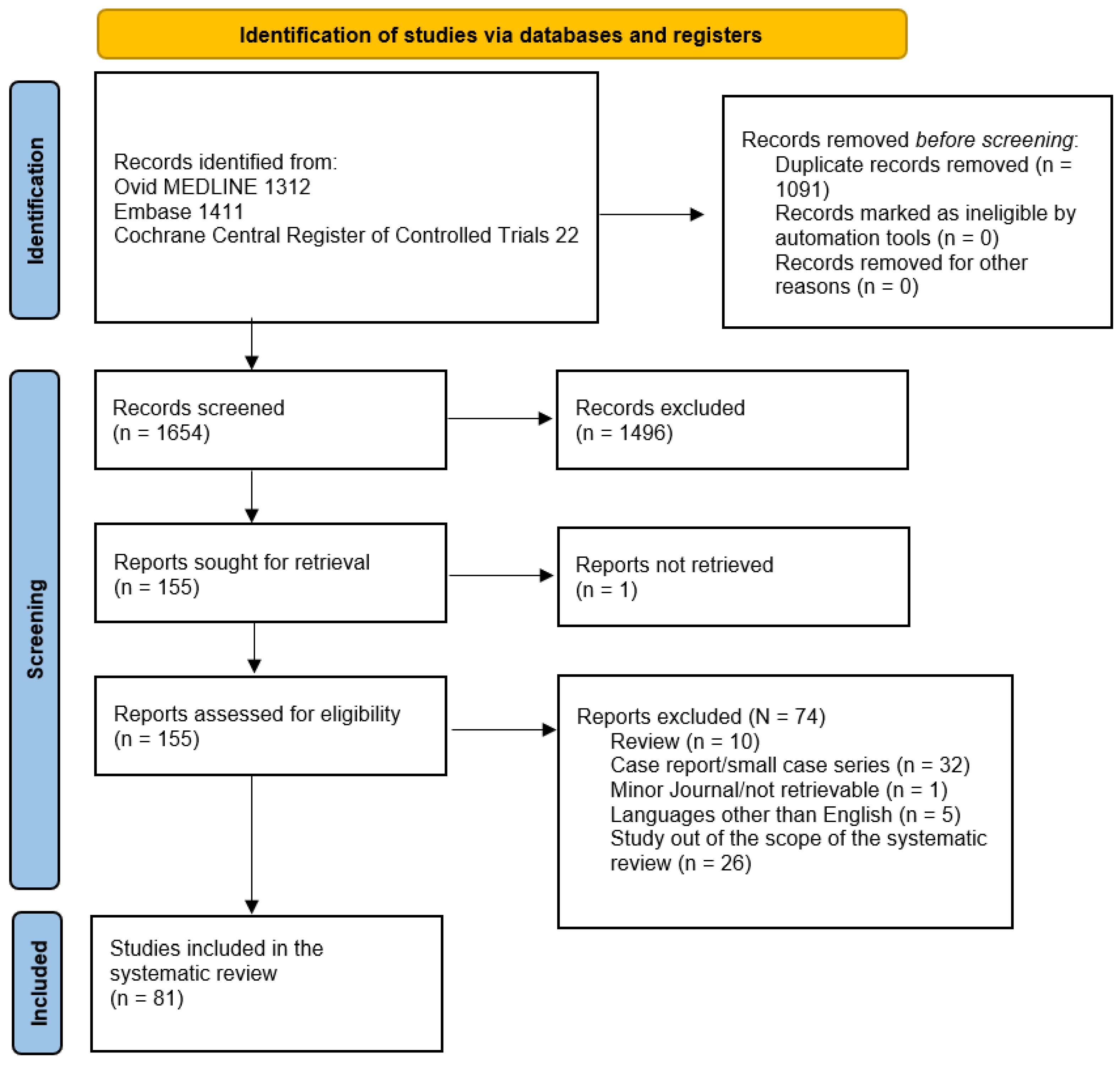
Background: Subretinal macular hemorrhage (SRMH) secondary to age-related macular degeneration (AMD) is a relatively rare condition in ophthalmology characterized by blood collection between the neurosensory retina and the retinal pigment epithelium (RPE). Without prompt treatment, visual prognosis is poor. A plethora of treatment approaches have been tried over the past years ranging from intravitreal anti-vascular endothelial growth factor (anti-VEGF) monotherapy to direct subretinal surgery, with no conclusive superiority of one over the other. Materials and Methods: We conducted a systematic review of the outcomes and treatment modalities of SRMH from inception to 14 June 2022, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA). The level of evidence was assessed for all included articles according to the quality of evidence according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system. Results: A total of 2745 articles were initially extracted, out of which 1654 articles were obtained after duplicates were removed and their abstracts screened. A total of 155 articles were included for full-text review. Finally, 81 articles remained that fulfilled the inclusion criteria. Conclusions: Even though there are solid results supporting a variety of treatments for SRMH, the best treatment modality has still not been conclusively demonstrated and further research is needed.
1. Introduction
Retinal hemorrhage is among the most common clinical signs in retinal disease and consists of a spectrum of blood collection differing in location, size, distribution, and etiology [1]. Fovea-involving subretinal macular hemorrhage (SRMH) is a sight-threatening condition defined as blood collection between the neurosensory retina and the retinal pigment epithelium (RPE) [2]. SRMH can be caused by a plethora of eye disorders, including neovascular age-related macular degeneration (n-AMD) and its variants such as polypoid choroidal vasculopathy (PCV), but also pathologic myopia, ruptured retinal artery macroaneurysms, presumed ocular histoplasmosis syndrome, and trauma [3,4,5,6,7]. SRMH can cause irreversible damage to the photoreceptors; if left untreated, a blood clot under the retina usually turns into a scar, causing permanent loss of central vision [8,9,10].
AMD is the leading cause of legal blindness in the industrialized world [11]. The real incidence of SRMH among patients with n-AMD is unknown [12], even though n-AMD has long been known to be a risk factor for submacular bleeding [8,13].
SRMHs larger than one disc diameter (DD) across in size have been reported in 24 people per million per year, according to a population-based study conducted in two UK centers, while SRMHs larger than two DDs have been reported in only 5.4 people per million per year in a study by a Scottish Ophthalmic Surveillance Unit (SOSU) [14,15]. Nevertheless, the population in many countries is ageing and the disease prevalence for AMD, and therefore SRMHs, is supposed to increase significantly in the coming years [16].
SRMH generally results in a severe and irreversible loss of vision, ranging from 6/30 to light perception, if left untreated [17]. Moreover, only 11% of the eyes in the control group of a submacular surgery study achieve a final best-corrected visual acuity (BCVA) higher than 6/60 [10]. The functional outcome may also be influenced by the duration and size of SRMH, as well as the etiology and location of the bleeding source. Persistent SRMH damages the photoreceptors through three main mechanisms: iron-related toxicity, impairment of diffusion of oxygen and nutrition, and mechanical damage due to clot contraction [18,19,20,21,22,23]. The natural history of SRMH typically leads to a central scotoma with a fibrotic macular scar (38%), atrophy (25%), or RPE rupture (22%) [17].
A variety of approaches have been employed in the treatment of SRMH, and even though ample literature exists, this is dispersive and predominantly made up of small, single-center outcome reports that do not encompass all the therapeutic techniques that have been described.
The purpose of this systematic review is to analyze and summarize the current therapeutic approaches in the management of SRMH while evaluating the level and quality of the research included.
2. Materials and Methods
A systematic review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [24]. The review protocol was not recorded in the study design, but a registration number will be available for consultation. The methodology used consisted of a systematic search of all available articles exploring the treatment modalities of SRMH secondary to n-AMD. To identify all relevant published articles, we performed a systematic literature search including papers published from inception until 14 June 2022. These were searched in Ovid Medline, Embase, Cochrane Register of Controlled Trials, and Cochrane Database of Systematic Reviews using controlled vocabulary and text words expressing (subretinal OR submacular) AND (hemorrhage OR haemorrhage OR bleeding). The search was not restricted by publication type, study design, or date of publication. The search was restricted by the English language. The complete search strategy is given in Appendix A.
Subsequently, the reference lists of all identified articles were examined manually to identify any potential study not selected by the electronic searches. After the preparation of the list of all electronic data, a reviewer (FC) examined the titles and abstracts and identified relevant articles. All the studies analyzing outcomes of the available treatment modalities of SRMH in n-AMD were considered as satisfactory for the inclusion criteria. Exclusion criteria were review studies, pilot studies, letters to the editor, case series with ≤12 eyes, case reports, photo essays, and studies written in languages other than English. Moreover, studies performed on animal eyes, cadaveric eyes, and pediatric patients were excluded as well. Exclusion criteria also included studies that were not specifically powered to detect a correlation between the treatment modality of either the anatomical or functional outcomes in SRMH treatment. SRMH secondary to diseases other than n-AMD was also excluded.
The same reviewer registered and selected the studies according to the inclusion and exclusion criteria by examining the full text of the articles. Any doubt was assessed by consensus with a third-party reviewer (GP), who was consulted when necessary. No further unpublished data were obtained from the corresponding authors of all selected articles, which were analyzed to assess the level of evidence according to the quality of evidence according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system [25,26].
3. Results
A total of 2745 articles were initially extracted. Consequently, 1654 articles were obtained after the duplicates were removed and their abstracts were screened. Subsequently, 155 articles were included for the full-text review and more in-depth evaluation of the inclusion/exclusion criteria. Finally, 81 articles remained that fulfilled all the inclusion criteria.
Figure 1 summarizes the research approach applied here in a flowchart.
Figure 1.
Flowchart of the literature search and selection according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA) [24].
The determining reasons for inclusion or exclusion of the full-text reviewed articles are summarized in Appendix B. Furthermore, Appendix C summarizes all the studies extracted from the systematic literature search, with the relevant descriptive information.
In order to summarize the large amount of information derived from the systematic search, Table 1 was created to report on the studies that are prospective or randomized controlled trials (RCTs). These are in fact the most valuable studies, and they are the main source of evidence.

Table 1.
Prospective or RCT studies on subretinal bleeding.
In Table 2, the studies were grouped according to the type of intervention that was applied, which were anti-vascular endothelial growth factor (anti-VEGF) only, intravitreal recombinant tissue plasminogen activator (rt-PA), and/or subretinal rt-PA.

Table 2.
Studies on subretinal bleeding according to treatment strategies: anti-VEGF only vs. IVT rt-PA vs. subretinal rt-PA.
In Table 3, a summary of the studies is provided according to the hemorrhage onset, as the timing of intervention seems to be crucial for the outcome of SRMH patients [55].

Table 3.
Summary of the mean days from onset: less or more than 2 weeks from symptoms’ onset in subretinal bleeding with references.
Finally, Table 4 groups all the included studies on the basis of SRMH size in an attempt to simplify the understanding for prognostic purposes.

Table 4.
Studies on subretinal bleeding according to the size.
4. Discussion
SRMH poses a formidable challenge in the realm of retinal pathology, given its potential to cause irreversible damage to central vision. Despite its clinical significance, the optimal treatment strategy for SRMH remains to be an ongoing debate, largely due to the scarcity of comprehensive prospective studies and the consequent absence of a widely accepted best practice.
This systematic review critically assessed the existing literature on SRMH treatment modalities, focusing on prospective studies to elucidate the current landscape of therapeutic interventions. The number of prospective trials specifically targeting SRMH is limited, thus underscoring the need for further robust investigations to guide evidence-based decision-making. Within the sparse collection of prospective studies, various treatment options have been explored, ranging from conservative observation to surgical interventions. Notably, only retrospective studies by Ueda-Arakawa et al. [103] and Maggio et al. [47] have explored the merits of a watchful waiting approach, positing its suitability for cases marked by minimal visual impairment and self-resolving hemorrhages. Nevertheless, due to the relatively small sample sizes and inherent variability in hemorrhage characteristics, these studies have not been able to definitively establish the superiority of observation over the active therapeutic interventions.
Pneumatic displacement, an innovative approach, has gained attention for its potential to physically displace subretinal hemorrhage away from the macula. The prospective investigations by Gopalakrishan et al. [28] and De Jong et al. [31] unveiled encouraging results, suggesting improved visual outcomes. However, the limited number of patients and the absence of long-term follow-up data cast a shadow over the sustainability of these positive findings.
Anti-VEGF agents, with their established efficacy in various retinal pathologies, have been examined as a potential treatment modality for SRMH. Iacono et al. [29] conducted prospective studies probing the impact of anti-VEGF injections on neovascularization and inflammation associated with SRMH. Despite the promise showcased in this study, the lack of consensus in the treatment regimens and the modest sample sizes hinder the establishment of a definitive therapeutic role for anti-VEGF agents.
Surgical interventions, specifically vitrectomy with or without rt-PA injection, have been a subject of exploration through prospective studies by Wei et al. [30], Mozafarieh et al. [27], Kadonosono et al. [86], Kimura et al. [69], and De Jong et al. [31]. These studies have shed light on the potential benefits of surgical intervention, particularly in cases of larger and dense or recurrent hemorrhage. However, the invasiveness of the procedure, coupled with concerns regarding complications, necessitates judicious patient selection and cautious consideration of risks and benefits.
Photodynamic therapy (PDT), a modality with established efficacy in other retinal conditions, has also found its way into the discourse surrounding SRMH treatment. Notable retrospective studies by Lin et al. [44] have ventured into investigating PDT’s potential role in addressing neovascularization in SRMH. Nevertheless, the existing body of evidence is marked by its infancy and a lack of consistent findings, impeding the establishment of PDT as a definitive treatment avenue.
Our work sums up all the available treatment modalities of SRMH. As the management of this condition is a complex and challenging task, several treatment modalities have been developed to address it, each with its own set of advantages and limitations. We will further highlight the various treatment modalities for SRMH below.
Intravitreal Anti-VEGF Therapy: Intravitreal injection of anti-VEGF agents, such as ranibizumab and bevacizumab, has gained popularity in recent years. These drugs can resolve SRMH by inhibiting abnormal blood vessel growth and leakage in conditions like CNV. The advantages of this approach include its minimal invasiveness and relatively rapid resolution of the hemorrhage. However, it may not be effective in all cases, and multiple injections over an extended period of time may be required. The long-term safety profile of these agents also warrants the ongoing and further research.
Pneumatic displacement involves the injection of expansile gases, such as sulfur hexafluoride or perfluoropropane, into the vitreous cavity. This gas displaces the SRMH, moving it away from the macula, allowing for improved vision. Pneumatic displacement is less invasive than other surgical procedures and can be an effective treatment option. However, it may be associated with complications, such as subretinal blood displacement, which necessitates careful patient selection and follow-up.
Vitrectomy is a surgical intervention that involves the removal of vitreous gel from the eye. This procedure allows direct visualization and access to the subretinal space, enabling the removal of blood and other substances. Vitrectomy is effective in a wide range of cases, particularly when the hemorrhage is extensive, the fibrosis has occurred, or when other treatment modalities have failed. However, it is an invasive procedure with potential surgical risks, longer recovery times, and need for careful postoperative management. Potential complications from pneumatic displacement during vitrectomy can include vitreous or choroidal hemorrhage, hyphema, RPE tear and cataract formation, retinal detachment, increased intraocular pressure/glaucoma, full-thickness macular hole formation, and endophthalmitis (Appendix C).
Subretinal injection of rt-PA followed by the injection of an expansile gas, such as sulfur hexafluoride or perfluoropropane can facilitate the mechanical displacement of the SRMH and potentially improve visual outcomes. However, it is a surgical procedure and requires experienced surgical skills to minimize risks.
The choice of treatment for SRMH should be individualized, considering factors such as the extent and location of the hemorrhage; the patient’s overall health, including blood pressure and cardiac status, use of blood thinners, and INR level where applicable; the visual acuity goals; and the potential risks and benefits associated with each option. A multidisciplinary approach, involving ophthalmologists, vitreoretinal surgeons, and the patient, is often crucial in making the most informed decision.
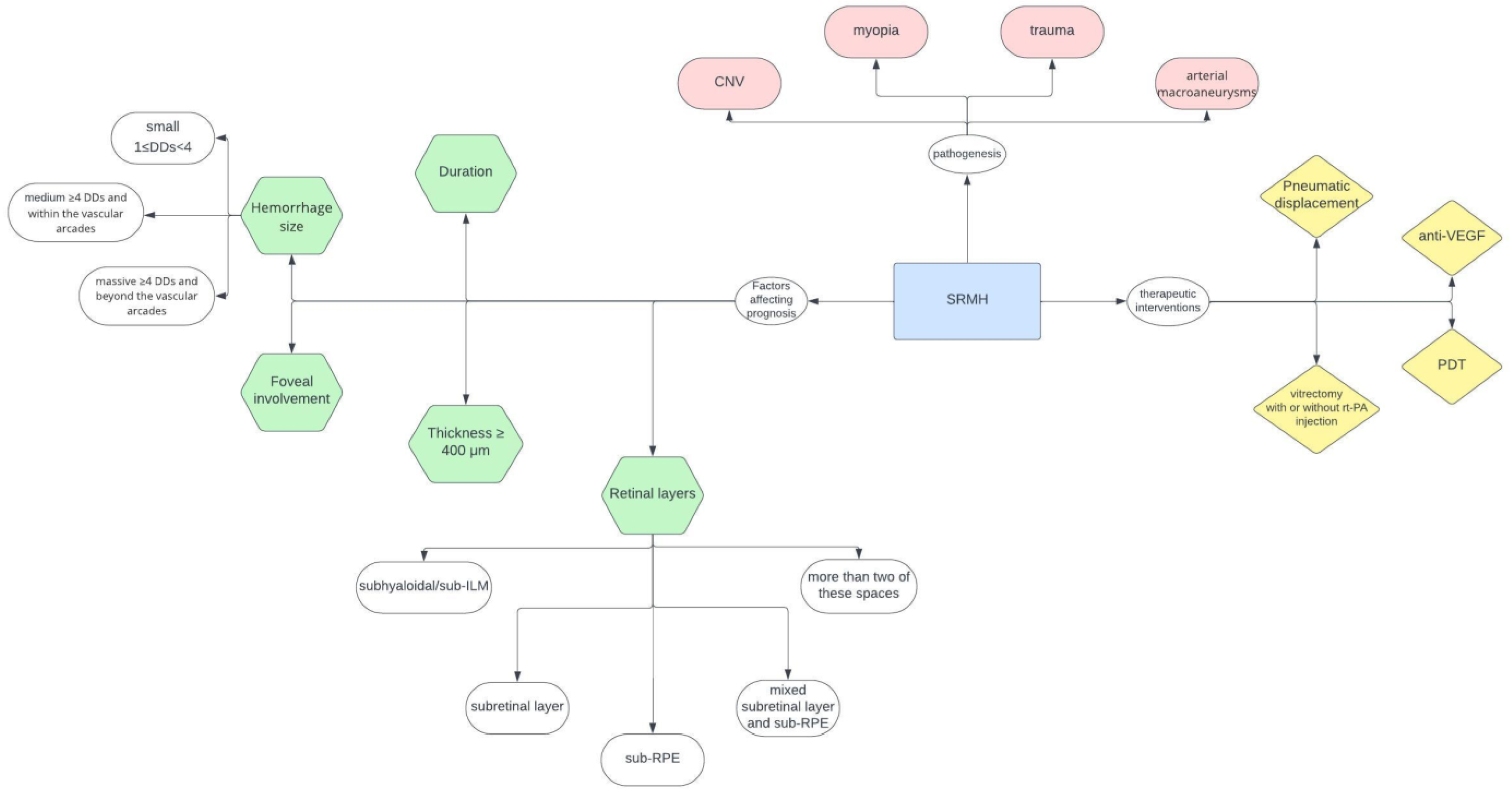
A flow chart on the clinical diagnostics, management, and treatment of patients with acute loss of vision due to suspected SRMH is depicted in Figure 2.
Figure 2.
Flow chart on the clinical diagnostics, management, and treatment of patients with acute loss of vision due to suspected SRMH. Disc diameter (DD); photodynamic therapy (PDT).
As research continues to evolve, new treatment modalities and refinements to existing approaches may emerge, offering hope for improved outcomes and quality of life for individuals affected by SRMH. The optimal approach to managing this condition will depend on the specific characteristics and needs of each patient, and ongoing clinical trials and research will help shape the future of SRMH treatment.
5. Conclusions
In conclusion, the management of subretinal macular hemorrhage presents a complex and challenging clinical scenario. Various treatment modalities have been explored, each with its own set of pros and cons. The choice of treatment should be tailored to the individual patient, taking into consideration the specific characteristics of the hemorrhage, the patient’s overall health, and their visual acuity goals.
Intravitreal injection of anti-VEGF agents has emerged as a promising non-invasive option for some patients. Its advantages include rapid resolution of hemorrhage, minimal invasiveness, and a potential for improved visual outcomes. However, it may not be effective in all cases, especially in instances of massive hemorrhage or when fibrotic changes have already occurred. Additionally, the need for multiple injections and the long-term safety profile of these drugs require ongoing research.
Surgical interventions, such as pneumatic displacement and vitrectomy, offer the advantage of direct visualization and removal of the hemorrhage. These procedures can be effective in a wider range of cases and may yield significant improvements in vision. Nevertheless, they come with the risk of surgical complications, prolonged recovery periods, and potential long-term anatomical changes. The choice of surgery should be made carefully, considering the individual patient’s surgical risk profile and the likelihood of postoperative complications.
The use of subretinal tPA and gas injection, while it may achieve faster resolution compared to observation alone, it is still an invasive procedure like traditional vitrectomy. This technique is, however, not suitable for all cases and requires experienced surgical hands to minimize risks.
Ultimately, the decision on the most appropriate treatment modality for subretinal macular hemorrhage should be made through a multidisciplinary approach involving the ophthalmologist, the patient, and other healthcare providers. It is imperative to weigh the potential benefits against the risks and limitations of each approach while considering the patient’s individual circumstances and preferences. Ongoing research and clinical trials will continue to refine our understanding of these treatment modalities and potentially lead to further advancements in the management of this challenging condition. As we move forward, it is crucial that clinicians remain vigilant in their pursuit of improved therapies, with the goal of optimizing visual outcomes and enhancing the quality of life for patients with subretinal macular hemorrhage.
Author Contributions
Conceptualization, F.C.; methodology, F.C., G.B., X.L. and G.P.; software, V.F., G.B., G.P. and F.C.; validation, G.B., F.C., V.F., A.D.M., B.É.P., J.L.V.G., P.V., A.R. and G.P.; formal analysis, G.B.; investigation, F.C., V.F., A.D.M., G.B., X.L. and G.P.; resources, F.C., X.L., G.P., A.D.M. and G.B.; data curation, F.C., V.F., A.D.M., G.B. and G.P.; writing—original draft preparation, A.D.M., G.B. and F.C.; writing—review and editing, all authors; supervision, X.L., G.P. and F.C.; project administration, G.P. and F.C.; funding acquisition, F.C., V.F., A.D.M., G.B., X.L. and G.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available on reasonable request to the corresponding authors.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
Documentation on the literature search for:
Subretinal haemorrhage
Search date: 14 June 2022
The following databases were searched:
| Database | Number of Retrieved References |
| Ovid Medline | 1312 |
| Embase | 1411 |
| Cochrane Central Register of Controlled Trials | 22 |
| Cochrane Database of Systematic Reviews | 0 |
| Number of references before deduplication: | 2745 |
| Number of references after deduplication: | 1654 |
Search syntax:
| / | After an index term indicates a subject heading was selected |
| .ti,ab,kf. | Search for a term in title, abstract, and author keywords |
| * | At the end of a term indicates that this term has been truncated; hemorrhag* retrieves haemorrhage, haemorrhages |
| Adj2 | ADJ = adjacent operator in the Ovid databases. Adj2: search for two terms next to each other, in any order, up to 2 words in between. |
| NEAR/3 | NEAR = proximity operator in the Cochrane Database of Systematic Reviews. NEAR/3: search for two terms next to each other, in any order, up to 2 words in between. |
Search strategies:
Ovid MEDLINE(R) ALL 1946 to 8 June 2022
| # | Searches | Results |
| 1 | ((subretin* or sub-retin* or submacula* or sub-macula*) adj2 (hemorrhag* or haemorrhag* or bleed*)).ti,ab,kf. | 1346 |
| 2 | Retinal Haemorrhage/ | 5523 |
| 3 | (subretin* or sub-retin* or submacula* or sub-macula*).ti,ab,kf. | 11,699 |
| 4 | 1 or (2 and 3) | 1509 |
| 5 | limit 4 to english language | 1312 |
Embase Classic + Embase 1947 to 8 June 2022
| # | Searches | Results |
| 1 | ((subretin* or sub-retin* or submacula* or sub-macula*) adj2 (hemorrhag* or haemorrhag* or bleed*)).ti,ab,kf. | 1672 |
| 2 | retina haemorrhage/ or retina macula haemorrhage/ | 10,977 |
| 3 | (subretin* or sub-retin* or submacula* or sub-macula*).ti,ab,kf. | 16,004 |
| 4 | 1 or (2 and 3) | 2098 |
| 5 | limit 4 to conference abstracts | 234 |
| 6 | 4 not 5 | 1864 |
| 7 | limit 6 to (article or review) | 1725 |
| 8 | limit 7 to english language | 1411 |
Cochrane Central Register of Controlled Trials
| 1 | ((subretin* or sub-retin* or submacula* or sub-macula*) AND (hemorrhag* or haemorrhag* or bleed*)): in Record Title | 22 |
Cochrane Database of Systematic Reviews
| 1 | ((subretin* or sub-retin* or submacula* or sub-macula*) NEAR/3 (hemorrhag* or haemorrhag* or bleed*)): in ti,ab,kw. | 0 |
Appendix B
Summary of the 155 records screened for inclusion/exclusion and the determining reasons behind each choice.
| Title | Included (N. of Eyes) | Excluded | Explanation for Exclusion (or Comments) | |
| 1 | Olivier S, Chow DR, Packo KH, MacCumber MW, Awh CC. Subretinal recombinant tissue plasminogen activator injection and pneumatic displacement of thick submacular haemorrhage in Age-Related macular degeneration. Ophthalmology. 2004 Jun;111(6):1201–8. doi: 10.1016/j.ophtha.2003.10.020. Erratum in: Ophthalmology. 2004 Sep;111(9):1640. PMID: 15177972. | 1 included (29 eyes) | ||
| 2 | Woo, J. John M.D.; Lou, Peter L. M.D.; Ryan, Edward A. M.D.; Kroll, Arnold J. M.D. Surgical Treatment of Submacular Haemorrhage in Age-Related Macular Degeneration. International Ophthalmology Clinics: Winter 2004-Volume 44-Issue 1-p 43–50 | Excluded | Review | |
| 3 | Chan, W.-M., Liu, D.T., Lai, T.Y., Li, H., Tong, J.-P. and Lam, D.S. (2005), Extensive submacular haemorrhage in polypoidal choroidal vasculopathy managed by sequential gas displacement and photodynamic therapy: a pilot study of one-year follow up. Clinical & Experimental Ophthalmology, 33: 611–618. https://doi-org.ezproxy.uio.no/10.1111/j.1442-9071.2005.01105.x | Excluded | Pilot study, 6 eyes | |
| 4 | Puchta, Koch, F., & Hattenbach, L. (2005). Prospektive, randomisierte Studie zur intravitrealen Gabe von rt-PA mit SF6-Gas vs. SF6-Gas in der Behandlung von submakulären Blutungen bei AMD. Klinische Monatsblätter für Augenheilkunde. https://doi.org/10.1055/s-2005-922145 | Excluded | Languages other than English | |
| 5 | Ratanasukon, M., Kittantong, A. Results of intravitreal tissue plasminogen activator and expansile gas injection for submacular haemorrhage in Thais. Eye 19, 1328–1332 (2005). https://doi.org/10.1038/sj.eye.6701769 | 2 included (24 eyes) | ||
| 6 | Thompson JT, Sjaarda RN. Vitrectomy for the treatment of submacular haemorrhages from macular degeneration: a comparison of submacular haemorrhage/membrane removal and submacular tissue plasminogen activator-assisted pneumatic displacement. Trans Am Ophthalmol Soc. 2005;103:98–107; discussion 107. PMID: 17057793; PMCID: PMC1447564. | 3 included (42 eyes) | ||
| 7 | Wu TT, Sheu SJ. Intravitreal tissue plasminogen activator and pneumatic displacement of submacular haemorrhage secondary to retinal artery macroaneurysm. J Ocul Pharmacol Ther. 2005 Feb;21(1):62–7. doi: 10.1089/jop.2005.21.62. PMID: 15718829. | Excluded | Case series of only 6 eyes | |
| 8 | Yang PM, Kuo HK, Kao ML, Chen YJ, Tsai HH. Pneumatic displacement of a dense submacular haemorrhage with or without tissue plasminogen activator. Chang Gung Med J. 2005 Dec;28(12):852–9. PMID: 16515019. | 4 included (24 eyes) | ||
| 9 | Mozaffarieh M, Heinzl H, Sacu S, Wedrich A. In-patient management and treatment satisfaction after intravitreous plasminogen activator injection. Graefes Arch Clin Exp Ophthalmol. 2006 Nov;244(11):1421–8. doi: 10.1007/s00417-005-0232-z. Epub 2006 Apr 5. PMID: 16596407. | 5 included (101 eyes) | (No anatomical parameters) | |
| 10 | Oie Y, Emi K. Surgical excision of retinal macroaneurysms with submacular haemorrhage. Jpn J Ophthalmol. 2006 Nov-Dec;50(6):550–553. doi: 10.1007/s10384-006-0369-2. Epub 2006 Dec 18. PMID: 17180532. | Excluded | Only 2 patients | |
| 11 | Singh RP, Patel C, Sears JE. Management of subretinal macular haemorrhage by direct administration of tissue plasminogen activator. Br J Ophthalmol. 2006 Apr;90(4):429–31. doi: 10.1136/bjo.2005.085001. PMID: 16547320; PMCID: PMC1856980. | 6 included (17 eyes) | ||
| 12 | Chen CY, Hooper C, Chiu D, Chamberlain M, Karia N, Heriot WJ. Management of submacular haemorrhage with intravitreal injection of tissue plasminogen activator and expansile gas. Retina. 2007 Mar;27(3):321–8. doi: 10.1097/01.iae.0000237586.48231.75. PMID: 17460587. | 7 included (104 eyes) | ||
| 13 | Gopalakrishan M, Giridhar A, Bhat S, Saikumar SJ, Elias A, N S. Pneumatic displacement of submacular haemorrhage: safety, efficacy, and patient selection. Retina. 2007 Mar;27(3):329–34. doi: 10.1097/01.iae.0000231544.43093.40. PMID: 17460588. | 8 included (20 eyes) | ||
| 14 | Hasler PW, la Cour M, Villumsen J. Pneumatic displacement and intravitreal bevacizumab in the management of subretinal haemorrhage caused by choroidal neovascularization. Acta Ophthalmol Scand. 2007 Aug;85(5):577–9. doi: 10.1111/j.1600-0420.2007.00914.x. Epub 2007 Jun 8. PMID: 17559558. | Excluded | Case report | |
| 15 | Oshima Y, Ohji M, Tano Y. Pars plana vitrectomy with peripheral retinotomy after injection of preoperative intravitreal tissue plasminogen activator: a modified procedure to drain massive subretinal haemorrhage. Br J Ophthalmol. 2007 Feb;91(2):193–8. doi: 10.1136/bjo.2006.101444. Epub 2006 Aug 17. PMID: 16916872; PMCID: PMC1857597. | Excluded | Surgical technique | |
| 16 | Ron Y, Ehrlich R, Axer-Siegel R, Rosenblatt I, Weinberger D. Pneumatic displacement of submacular haemorrhage due to age-related macular degeneration. Ophthalmologica. 2007;221(1):57–61. doi: 10.1159/000096524. PMID: 17183203. | 9 included (24 eyes) | ||
| 17 | Stifter E, Michels S, Prager F, Georgopoulos M, Polak K, Hirn C, Schmidt-Erfurth U. Intravitreal bevacizumab therapy for neovascular age-related macular degeneration with large submacular haemorrhage. Am J Ophthalmol. 2007 Dec;144(6):886–892. doi: 10.1016/j.ajo.2007.07.034. Epub 2007 Oct 4. PMID: 17916314. | 10 included (21 eyes) | ||
| 18 | Liu, W. Current management of submacular haemorrhage in age-related macular degeneration. International Journal of Ophthalmology-Volume 8, Issue 0, pp. 867–870-published 2008-01-01 | Excluded | Review | |
| 19 | Meyer CH, Scholl HP, Eter N, Helb HM, Holz FG. Combined treatment of acute subretinal haemorrhages with intravitreal recombined tissue plasminogen activator, expansile gas and bevacizumab: a retrospective pilot study. Acta Ophthalmol. 2008 Aug;86(5):490–4. doi: 10.1111/j.1600-0420.2007.01125.x. Epub 2008 Jan 24. PMID: 18221499. | 11 included (19 eyes) | ||
| 20 | Nakamura H, Hayakawa K, Sawaguchi S, Gaja T, Nagamine N, Medoruma K. Visual outcome after vitreous, sub-internal limiting membrane, and/or submacular haemorrhage removal associated with ruptured retinal arterial macroaneurysms. Graefes Arch Clin Exp Ophthalmol. 2008 May;246(5):661–9. doi: 10.1007/s00417-007-0724-0. Epub 2007 Dec 11. PMID: 18071732. | Excluded | SRMH secondary to RAM | |
| 21 | Chawla S, Misra V, Khemchandani M. Pneumatic displacement and intravitreal bevacizumab: a new approach for management of submacular haemorrhage in choroidal neovascular membrane. Indian J Ophthalmol. 2009 Mar-Apr;57(2):155–7. doi: 10.4103/0301-4738.45511. PMID: 19237795; PMCID: PMC2684421. | Excluded | Only 4 cases | |
| 22 | Fang IM, Lin YC, Yang CH, Yang CM, Chen MS. Effects of intravitreal gas with or without tissue plasminogen activator on submacular haemorrhage in age-related macular degeneration. Eye (Lond). 2009 Feb;23(2):397–406. doi: 10.1038/sj.eye.6703017. Epub 2007 Nov 2. PMID: 17975562. | 12 included (53 eyes) | ||
| 23 | Gibran SK, Romano MR, Wong D. Surgical management of massive submacular haemorrhage associated with age-related macular degeneration. Retin Cases Brief Rep. 2009 Fall;3(4):391–4. doi: 10.1097/ICB.0b013e31818a470e. PMID: 25389857. | Excluded | 6 eyes | |
| 24 | Kamei M, Tano Y. Tissue plasminogen activator-assisted vitrectomy: surgical drainage of submacular haemorrhage. Dev Ophthalmol. 2009;44:82–88. doi: 10.1159/000223948. Epub 2009 Jun 3. PMID: 19494655. | Excluded | 12 eyes | |
| 25 | Arias L, Monés J. Transconjunctival sutureless vitrectomy with tissue plasminogen activator, gas and intravitreal bevacizumab in the management of predominantly hemorrhagic age-related macular degeneration. Clin Ophthalmol. 2010 Feb 18;4:67–72. doi: 10.2147/opth.s8635. PMID: 20186279; PMCID: PMC2827187. | 13 included (15 eyes) | ||
| 26 | Cakir M, Cekiç O, Yilmaz OF. Pneumatic displacement of acute submacular haemorrhage with and without the use of tissue plasminogen activator. Eur J Ophthalmol. 2010 May-Jun;20(3):565–71. doi: 10.1177/112067211002000305. PMID: 20037915. | 14 included (21 eyes) | ||
| 27 | Fine HF, Iranmanesh R, Del Priore LV, Barile GR, Chang LK, Chang S, Schiff WM. Surgical outcomes after massive subretinal haemorrhage secondary to age-related macular degeneration. Retina. 2010 Nov-Dec;30(10):1588–94. doi: 10.1097/IAE.0b013e3181e2263c. PMID: 20856172. | 15 included (15 eyes) | ||
| 28 | Hillenkamp J, Surguch V, Framme C, Gabel VP, Sachs HG. Management of submacular haemorrhage with intravitreal versus subretinal injection of recombinant tissue plasminogen activator. Graefes Arch Clin Exp Ophthalmol. 2010 Jan;248(1):5–11. doi: 10.1007/s00417-009-1158-7. Epub 2009 Aug 11. PMID: 19669780. | 16 included (18 + 29 eyes) | ||
| 29 | Höhn F, Mirshahi A, Hattenbach LO. Kombinierte intravitreale Injektion von Bevacizumab und SF(6)-Gas bei AMD-assoziierter, submakulärer Hämorrhagie [Combined intravitreal injection of bevacizumab and SF6 gas for treatment of submacular haemorrhage secondary to age-related macular degeneration]. Ophthalmologe. 2010 Apr;107(4):328–32. German. doi: 10.1007/s00347-009-2004-3. PMID: 19669150. | Excluded | Language other than English | |
| 30 | Kung YH, Wu TT, Hong MC, Sheu SJ. Intravitreal tissue plasminogen activator and pneumatic displacement of submacular haemorrhage. J Ocul Pharmacol Ther. 2010 Oct;26(5):469–74. doi: 10.1089/jop.2010.0066. PMID: 20925578. | 17 included (46 eyes) | ||
| 31 | McAllister IL, Chen SD, Patel JI, Fleming BL, Yu DY. Management of submacular haemorrhage in age-related macular degeneration with intravitreal tenecteplase. Br J Ophthalmol. 2010 Feb;94(2):260–1. doi: 10.1136/bjo.2009.158170. PMID: 20139293. | Excluded | 8 eyes | |
| 32 | McKibbin M, Papastefanou V, Matthews B, Cook H, Downey L. Ranibizumab monotherapy for sub-foveal haemorrhage secondary to choroidal neovascularisation in age-related macular degeneration. Eye (Lond). 2010 Jun;24(6):994–8. doi: 10.1038/eye.2009.271. Epub 2009 Nov 13. PMID: 19911016. | Excluded | 12 eyes | |
| 33 | Sandhu SS, Manvikar S, Steel DH. Displacement of submacular haemorrhage associated with age-related macular degeneration using vitrectomy and submacular rt-PA injection followed by intravitreal ranibizumab. Clin Ophthalmol. 2010 Jul 21;4:637–42. doi: 10.2147/opth.s10060. PMID: 20668667; PMCID: PMC2909894. | 18 included (16 eyes) | ||
| 34 | Treumer F, Klatt C, Roider J, Hillenkamp J. Subretinal coapplication of recombinant tissue plasminogen activator and bevacizumab for neovascular age-related macular degeneration with submacular haemorrhage. Br J Ophthalmol. 2010 Jan;94(1):48–53. doi: 10.1136/bjo.2009.164707. Epub 2009 Nov 27. PMID: 19946027. | Excluded | 12 eyes | |
| 35 | Georgalas I, Papaconstantinou D, Karagiannis D, Ladas I. Pneumatic displacement of acute submacular haemorrhage with and without the use of rt-PA. Eur J Ophthalmol. 2011 Mar-Apr;21(2):220; author reply 221. doi: 10.5301/ejo.2010.5685. PMID: 20853260. | Excluded | Comment to the editor | |
| 36 | Guthoff R, Guthoff T, Meigen T, Goebel W. Intravitreous injection of bevacizumab, tissue plasminogen activator, and gas in the treatment of submacular haemorrhage in age-related macular degeneration. Retina. 2011 Jan;31(1):36–40. doi: 10.1097/IAE.0b013e3181e37884. PMID: 20921929. | 19 included (38 eyes) | ||
| 37 | Mizutani T, Yasukawa T, Ito Y, Takase A, Hirano Y, Yoshida M, Ogura Y. Pneumatic displacement of submacular haemorrhage with or without tissue plasminogen activator. Graefes Arch Clin Exp Ophthalmol. 2011 Aug;249(8):1153–7. doi: 10.1007/s00417-011-1649-1. Epub 2011 Mar 29. PMID: 21445629. | 20 included (53 eyes) | ||
| 38 | Moriyama M, Ohno-Matsui K, Shimada N, Hayashi K, Kojima A, Yoshida T, Tokoro T, Mochizuki M. Correlation between visual prognosis and fundus autofluorescence and optical coherence tomographic findings in highly myopic eyes with submacular haemorrhage and without choroidal neovascularization. Retina. 2011 Jan;31(1):74–80. doi: 10.1097/IAE.0b013e3181e91148. PMID: 21187733. | Excluded | Macular hemorrhage secondary to pathologic myopia | |
| 39 | Shultz RW, Bakri SJ. Treatment for submacular haemorrhage associated with neovascular age-related macular degeneration. Semin Ophthalmol. 2011 Nov;26(6):361–71. doi: 10.3109/08820538.2011.585368. PMID: 22044334. | Excluded | Review | |
| 40 | Steel DH, Sandhu SS. Submacular haemorrhages associated with neovascular age-related macular degeneration. Br J Ophthalmol. 2011 Aug;95(8):1051–7. doi: 10.1136/bjo.2010.182253. Epub 2010 Sep 2. PMID: 20813746. | Excluded | Review | |
| 41 | Tognetto D, Skiadaresi E, Cecchini P, Ravalico G. Subretinal recombinant tissue plasminogen activator and pneumatic displacement for the management of subretinal haemorrhage occurring after anti-VEGF injections for wet AMD. Clin Ophthalmol. 2011;5:459–63. doi: 10.2147/OPTH.S15864. Epub 2011 Apr 13. PMID: 21573092; PMCID: PMC3090299. | Excluded | 3 cases | |
| 42 | Treumer F, Roider J, Hillenkamp J. Long-term outcome of subretinal coapplication of rt-PA and bevacizumab followed by repeated intravitreal anti-VEGF injections for neovascular AMD with submacular haemorrhage. Br J Ophthalmol. 2012 May;96(5):708–13. doi: 10.1136/bjophthalmol-2011-300655. Epub 2011 Dec 15. PMID: 22174095. | 21 included (41 eyes) | ||
| 43 | Wu TT, Kung YH, Hong MC. Vitreous haemorrhage complicating intravitreal tissue plasminogen activator and pneumatic displacement of submacular haemorrhage. Retina. 2011 Nov;31(10):2071–7. doi: 10.1097/IAE.0b013e31822528c8. PMID: 21817964. | Excluded | Aim out of the scope: to evaluate the clinical factors associated with vitreous hemorrhage | |
| 44 | Hesgaard HB, Torkashvand M, la Cour M. Failure to detect an effect of pneumatic displacement in the management of submacular haemorrhage secondary to age-related macular degeneration: a retrospective case series. Acta Ophthalmol. 2012 Sep;90(6):e498–500. doi: 10.1111/j.1755-3768.2011.02352.x. Epub 2012 Jan 23. PMID: 22268661. | Excluded | Letter to the editor | |
| 45 | Hesse, L. Intravitreale Injektionen. Ophthalmologe 109, 644–647 (2012). https://doi.org/10.1007/s00347-012-2565-4 | Excluded | Language other than English | |
| 46 | Hillenkamp J, Klettner A, Puls S, Treumer F, Roider J. Subretinale Koapplikation von rt-PA und Bevacizumab bei exsudativer altersbedingter Makuladegeneration mit submakulärer Blutung. Kompatibilität der Wirkstoffe und klinische Langzeitergebnisse [Subretinal co-application of rt-PA and bevacizumab for exudative AMD with submacular haemorrhage. Compatibility and clinical long-term results]. Ophthalmologe. 2012 Jul;109(7):648–56. German. doi: 10.1007/s00347-012-2564-5. PMID: 22752624. | Excluded | Language other than English | |
| 47 | Cochrane Central Register of Controlled Trials Intravitreal versus submacular injection of rt-PA for acute submacular haemorrhages NTR3359 https://trialsearch.who.int/Trial2.aspx?TrialID=NTR3359, 2012 | added to CENTRAL: 31 March 2019 | 2019 Issue 3 accessed on 1 July 2023. | Excluded | Trial protocol | |
| 48 | Sonmez K, Ozturk F, Ozcan PY. Treatment of multilevel macular haemorrhage secondary to retinal arterial macroaneurysm with submacular tissue plasminogen activator. Eur J Ophthalmol. 2012 Nov-Dec;22(6):1026–31. doi: 10.5301/ejo.5000140. Epub 2012 Mar 20. PMID: 22467586. | Excluded | SRMH secondary to RAM | |
| 49 | Szurman P. Subretinale Chirurgie bei Massenblutung [Subretinal surgery for massive haemorrhage]. Ophthalmologe. 2012 Jul;109(7):657–64. German. doi: 10.1007/s00347-012-2566-3. PMID: 22814924. | Excluded | Language other than English | |
| 50 | Tsymanava A, Uhlig CE. Intravitreal recombinant tissue plasminogen activator without and with additional gas injection in patients with submacular haemorrhage associated with age-related macular degeneration. Acta Ophthalmol. 2012 Nov;90(7):633–8. doi: 10.1111/j.1755-3768.2011.02115.x. Epub 2011 Feb 18. PMID: 21332673. | 22 included (110 eyes) | ||
| 51 | Ueda-Arakawa N, Tsujikawa A, Yamashiro K, Ooto S, Tamura H, Yoshimura N. Visual prognosis of eyes with submacular haemorrhage associated with exudative age-related macular degeneration. Jpn J Ophthalmol. 2012 Nov;56(6):589–98. doi: 10.1007/s10384-012-0191-y. Epub 2012 Oct 4. PMID: 23053632. | 23 included (31 eyes) | ||
| 52 | Injection of Lucentis (Ranibizumab) in the vitreous body of the eye after eye surgery and application of recombinant tissue plasminogen activator (rt-PA) in patients with submacular bleeding complications suffering from wet age-related macular degeneration (AMD) EUCTR2010-018637-21-DE https://trialsearch.who.int/Trial2.aspx?TrialID=EUCTR2010-018637-21-DE, 2013 | added to CENTRAL: 31 March 2019 | 2019 Issue 3 | Excluded | Protocol clinical trial | |
| 53 | Intravitreal rt-PA and C3F8 for the Treatment of Submacular Haemorrhage as a Complication of Neovascular Age-related Macular Degeneration NCT01835067 https://clinicaltrials.gov/show/NCT01835067, 2013 | added to CENTRAL: 31 May 2018 | 2018 Issue 5 | Excluded | Protocol clinical trial | |
| 54 | Cheung CM, Bhargava M, Xiang L, Mathur R, Mun CC, Wong D, Wong TY. Six-month visual prognosis in eyes with submacular haemorrhage secondary to age-related macular degeneration or polypoidal choroidal vasculopathy. Graefes Arch Clin Exp Ophthalmol. 2013 Jan;251(1):19–25. doi: 10.1007/s00417-012-2029-1. Epub 2012 May 26. PMID: 22638617. | Excluded | ||
| 55 | Cho HJ, Koh KM, Kim HS, Lee TG, Kim CG, Kim JW. Anti-vascular endothelial growth factor monotherapy in the treatment of submacular haemorrhage secondary to polypoidal choroidal vasculopathy. Am J Ophthalmol. 2013 Sep;156(3):524–531.e1. doi: 10.1016/j.ajo.2013.04.029. Epub 2013 Jun 13. PMID: 23769197. | 24 included (27 eyes) | ||
| 56 | Cho HJ, Koh KM, Kim HS, Lee TG, Kim CG, Kim JW. Anti-vascular endothelial growth factor monotherapy in the treatment of submacular haemorrhage secondary to polypoidal choroidal vasculopathy. Am J Ophthalmol. 2013 Sep;156(3):524–531.e1. doi: 10.1016/j.ajo.2013.04.029. Epub 2013 Jun 13. PMID: 23769197. | 25 included (17 eyes) | ||
| 57 | Han L, Ma Z, Wang C, Dou H, Hu Y, Feng X, Xu Y, Yin Z, Wang X. Autologous transplantation of simple retinal pigment epithelium sheet for massive submacular haemorrhage associated with pigment epithelium detachment. Invest Ophthalmol Vis Sci. 2013 Jul 24;54(7):4956–63. doi: 10.1167/iovs.13-11957. PMID: 23744996. | 26 included (14 eyes) | ||
| 58 | Jain S, Kishore K, Sharma YR. Intravitreal anti-VEGF monotherapy for thick submacular haemorrhage of less than 1 week duration secondary to neovascular age-related macular degeneration. Indian J Ophthalmol. 2013 Sep;61(9):490–6. doi: 10.4103/0301-4738.119432. PMID: 24104707; PMCID: PMC3831764. | 27 included (14 eyes) | ||
| 59 | Kapran Z, Ozkaya A, Uyar OM. Hemorrhagic age-related macular degeneration managed with vitrectomy, subretinal injection of tissue plasminogen activator, gas tamponade, and upright positioning. Ophthalmic Surg Lasers Imaging Retina. 2013 Sep-Oct;44(5):471–6. doi: 10.3928/23258160-20130909-09. PMID: 24044710. | Excluded | 10 eyes | |
| 60 | Lumi X, Sulak M. Treatment of submacular haemorrhage in patients with neovascular age related macular degeneration. Coll Antropol. 2013 Apr;37 Suppl 1:223–6. PMID: 23837248. | Excluded | 9 patients | |
| 61 | Martel JN, Mahmoud TH. Subretinal pneumatic displacement of subretinal haemorrhage. JAMA Ophthalmol. 2013 Dec;131(12):1632–5. doi: 10.1001/jamaophthalmol.2013.5464. PMID: 24337559. | Excluded | Surgical technique | |
| 62 | Mayer WJ, Hakim I, Haritoglou C, Gandorfer A, Ulbig M, Kampik A, Wolf A. Efficacy and safety of recombinant tissue plasminogen activator and gas versus bevacizumab and gas for subretinal haemorrhage. Acta Ophthalmol. 2013 May;91(3):274–8. doi: 10.1111/j.1755-3768.2011.02264.x. Epub 2011 Sep 22. PMID: 21952010. | 28 included (45 eyes) | ||
| 63 | Papavasileiou E, Steel DH, Liazos E, McHugh D, Jackson TL. Intravitreal tissue plasminogen activator, perfluoropropane (C3F8), and ranibizumab or photodynamic therapy for submacular haemorrhage secondary to wet age-related macular degeneration. Retina. 2013 Apr;33(4):846–53. doi: 10.1097/IAE.0b013e318271f278. PMID: 23400079. | Excluded | 7 eyes | |
| 64 | Rishi E, Gopal L, Rishi P, Sengupta S, Sharma T. Submacular haemorrhage: a study amongst Indian eyes. Indian J Ophthalmol. 2012 Nov-Dec;60(6):521–5. doi: 10.4103/0301-4738.103779. PMID: 23202390; PMCID: PMC3545128. | 29 included (46 eyes) | ||
| 65 | Mark Sherman, Charles Barr, Shlomit Schaal; Functional and Anatomical Outcomes of Tissue Plasminogen Activator (rt-PA) Treatment for Submacular Haemorrhage Associated with Exudative Macular Degeneration (ExAMD): A Comparative Analysis Between Intra-vitreal and Sub-retinal rt-PA injected Patients. Invest. Ophthalmol. Vis. Sci. 2013;54(15):3304. | Excluded | Meeting abstract | |
| 66 | Shienbaum G, Garcia Filho CA, Flynn HW Jr, Nunes RP, Smiddy WE, Rosenfeld PJ. Management of submacular haemorrhage secondary to neovascular age-related macular degeneration with anti-vascular endothelial growth factor monotherapy. Am J Ophthalmol. 2013 Jun;155(6):1009–13. doi: 10.1016/j.ajo.2013.01.012. Epub 2013 Mar 7. PMID: 23465269. | 30 included (19 eyes) | ||
| 67 | van Zeeburg EJ, Cereda MG, van Meurs JC. Recombinant tissue plasminogen activator, vitrectomy, and gas for recent submacular haemorrhage displacement due to retinal macroaneurysm. Graefes Arch Clin Exp Ophthalmol. 2013 Mar;251(3):733–40. doi: 10.1007/s00417-012-2116-3. Epub 2012 Aug 4. PMID: 22865261. | Excluded | SRMH secondary to RAM | |
| 68 | van Zeeburg EJ, van Meurs JC. Literature review of recombinant tissue plasminogen activator used for recent-onset submacular haemorrhage displacement in age-related macular degeneration. Ophthalmologica. 2013;229(1):1–14. doi: 10.1159/000343066. Epub 2012 Oct 12. PMID: 23075629. | Excluded | Review | |
| 69 | Chang W, Garg SJ, Maturi R, Hsu J, Sivalingam A, Gupta SA, Regillo CD, Ho AC. Management of thick submacular haemorrhage with subretinal tissue plasminogen activator and pneumatic displacement for age-related macular degeneration. Am J Ophthalmol. 2014 Jun;157(6):1250–7. doi: 10.1016/j.ajo.2014.02.007. Epub 2014 Feb 13. PMID: 24531021. | 31 included (101 eyes) | ||
| 70 | Dewilde E, Delaere L, Vaninbroukx I, Van Calster J, Stalmans P. Subretinal tissue plasminogen activator injection to treat submacular haemorrhage during age-related macular degeneration. Acta Ophthalmol. 2014 Sep;92(6):e497–8. doi: 10.1111/aos.12458. Epub 2014 Jun 18. PMID: 24943231. | Excluded | Letter to the editor | |
| 71 | Iacono P, Parodi MB, Introini U, La Spina C, Varano M, Bandello F. Intravitreal ranibizumab for choroidal neovascularization with large submacular haemorrhage in age-related macular degeneration. Retina. 2014 Feb;34(2):281–7. doi: 10.1097/IAE.0b013e3182979e33. PMID: 23851632. | 32 included (23 eyes) | ||
| 72 | Kitahashi M, Baba T, Sakurai M, Yokouchi H, Kubota-Taniai M, Mitamura Y, Yamamoto S. Pneumatic displacement with intravitreal bevacizumab for massive submacular haemorrhage due to polypoidal choroidal vasculopathy. Clin Ophthalmol. 2014 Mar 3;8:485–92. doi: 10.2147/OPTH.S55413. PMID: 24623972; PMCID: PMC3949732. | 33 included (32 eyes) | ||
| 73 | Gerard F McGowan, David Steel, David Yorston; AMD with submacular haemorrhage: new insights from a population-based study. Invest. Ophthalmol. Vis. Sci. 2014;55(13):662. | Excluded | Meeting abstract | |
| 74 | Moisseiev E, Ben Ami T, Barak A. Vitrectomy and subretinal injection of tissue plasminogen activator for large submacular haemorrhage secondary to AMD. Eur J Ophthalmol. 2014 Nov-Dec;24(6):925–31. doi: 10.5301/ejo.5000500. Epub 2014 Jun 12. PMID: 24966031. | 34 included (31 eyes) | ||
| 75 | Dimopoulos S, Leitritz MA, Ziemssen F, Voykov B, Bartz-Schmidt KU, Gelisken F. Submacular predominantly hemorrhagic choroidal neovascularization: resolution of bleedings under anti-VEGF therapy. Clin Ophthalmol. 2015 Aug 24;9:1537–41. doi: 10.2147/OPTH.S87919. PMID: 26346691; PMCID: PMC4554429. | 35 included (46 eyes) | ||
| 76 | Hirashima T, Moriya T, Bun T, Utsumi T, Hirose M, Oh H. Optical coherence tomography findings and surgical outcomes of tissue plasminogen activator-assisted vitrectomy for submacular haemorrhage secondary to age-related macular degeneration. Retina. 2015 Oct;35(10):1969–78. doi: 10.1097/IAE.0000000000000574. PMID: 26079475. | Excluded | 9 eyes | |
| 77 | Inoue M, Shiraga F, Shirakata Y, Morizane Y, Kimura S, Hirakata A. Subretinal injection of recombinant tissue plasminogen activator for submacular haemorrhage associated with ruptured retinal arterial macroaneurysm. Graefes Arch Clin Exp Ophthalmol. 2015 Oct;253(10):1663–9. doi: 10.1007/s00417-014-2861-6. Epub 2014 Nov 25. PMID: 25418034. | Excluded | RAM | |
| 78 | Prospective intervention study for drainage of subretinal haemorrhage using tissue plasminogen activator Authors: Jprn, Umin; Journal: https://trialsearch.who.int/Trial2.aspx?TrialID=JPRN-UMIN000019668 | Excluded | Clinical trial protocol | |
| 79 | Kadonosono K, Arakawa A, Yamane S, Inoue M, Yamakawa T, Uchio E, Yanagi Y. Displacement of submacular haemorrhages in age-related macular degeneration with subretinal tissue plasminogen activator and air. Ophthalmology. 2015 Jan;122(1):123–8. doi: 10.1016/j.ophtha.2014.07.027. Epub 2014 Sep 4. PMID: 25200400. | 36 included (13 eyes) | ||
| 80 | Kim HS, Cho HJ, Yoo SG, Kim JH, Han JI, Lee TG, Kim JW. Intravitreal anti-vascular endothelial growth factor monotherapy for large submacular haemorrhage secondary to neovascular age-related macular degeneration. Eye (Lond). 2015 Sep;29(9):1141–51. doi: 10.1038/eye.2015.131. Epub 2015 Aug 14. PMID: 26272443; PMCID: PMC4565949. | 37 included (49 eyes) | ||
| 81 | Kimura S, Morizane Y, Hosokawa M, Shiode Y, Kawata T, Doi S, Matoba R, Hosogi M, Fujiwara A, Inoue Y, Shiraga F. Submacular haemorrhage in polypoidal choroidal vasculopathy treated by vitrectomy and subretinal tissue plasminogen activator. Am J Ophthalmol. 2015 Apr;159(4):683–9. doi: 10.1016/j.ajo.2014.12.020. Epub 2014 Dec 30. PMID: 25555798. | 38 included (15 eyes) | ||
| 82 | Nayak S, Padhi TR, Basu S, Das T. Pneumatic displacement and intra-vitreal bevacizumab in management of sub-retinal and sub-retinal pigment epithelial haemorrhage at macula in polypoidal choroidal vasculopathy (PCV): rationale and outcome. Semin Ophthalmol. 2015 Jan;30(1):53–5. doi: 10.3109/08820538.2013.807849. Epub 2013 Aug 15. PMID: 23947424. | Excluded | 3 eyes | |
| 83 | Schaal, S.; Apenbrinck, E.; Barr, C. C.; Management of thick submacular haemorrhage with subretinal tissue plasminogen activator and pneumatic displacement for age-related macular degeneration. February 2015American Journal of Ophthalmology 159(2) DOI: 10.1016/j.ajo.2014.10.024 | Excluded | Correspondence article | |
| 84 | Shin JY, Lee JM, Byeon SH. Anti-vascular endothelial growth factor with or without pneumatic displacement for submacular haemorrhage. Am J Ophthalmol. 2015 May;159(5):904–14.e1. doi: 10.1016/j.ajo.2015.01.024. Epub 2015 Jan 28. PMID: 25637179. | 39 included (82 eyes) | ||
| 85 | Wei Y, Zhang Z, Jiang X, Li F, Zhang T, Qiu S, Yang Y, Zhang S. A surgical approach to large subretinal haemorrhage using pars plana vitrectomy and 360° retinotomy. Retina. 2015 Aug;35(8):1631–9. doi: 10.1097/IAE.0000000000000501. PMID: 26214315. | 40 included (21 eyes) | ||
| 86 | Abdelkader E, Yip KP, Cornish KS. Pneumatic displacement of submacular haemorrhage. Saudi J Ophthalmol. 2016 Oct-Dec;30(4):221–226. doi: 10.1016/j.sjopt.2016.10.002. Epub 2016 Oct 13. PMID: 28003779; PMCID: PMC5161816. | Excluded | 12 eyes, 9 with SRMH secondary to AMD | |
| 87 | Araújo J, Sousa C, Faria PA, Carneiro Â, Rocha-Sousa A, Falcão-Reis F. Intravitreal injection of recombinant tissue plasminogen activator in submacular haemorrhage: case series. Eur J Ophthalmol. 2016 Apr 12;26(3):e49–51. doi: 10.5301/ejo.5000682. PMID: 26428222. | Excluded | 6 eyes | |
| 88 | Bae K, Cho GE, Yoon JM, Kang SW. Optical Coherence Tomographic Features and Prognosis of Pneumatic Displacement for Submacular Haemorrhage. PLoS One. 2016 Dec 19;11(12):e0168474. doi: 10.1371/journal.pone.0168474. PMID: 27992524; PMCID: PMC5167395. | 41 included (37 eyes) | ||
| 89 | de Jong JH, van Zeeburg EJ, Cereda MG, van Velthoven ME, Faridpooya K, Vermeer KA, van Meurs JC. Intravitreal versus subretinal administration of recombinant tissue plasminogen activator combined with gas for acute submacular haemorrhages due to age-related macular degeneration: An Exploratory Prospective Study. Retina. 2016 May;36(5):914–25. doi: 10.1097/IAE.0000000000000954. PMID: 26807631. | 42 included (24 eyes) | ||
| 90 | de Silva SR, Bindra MS. Early treatment of acute submacular haemorrhage secondary to wet AMD using intravitreal tissue plasminogen activator, C3F8, and an anti-VEGF agent. Eye (Lond). 2016 Jul;30(7):952–7. doi: 10.1038/eye.2016.67. Epub 2016 Apr 15. PMID: 27080482; PMCID: PMC4941069. | Excluded | 8 eyes | |
| 91 | Dhawan, B.; Vig, V.; Singh, P.; Singh, R.; Management of sub macular haemorrhage with intravitreal injection of tissue plasminogen activator and sulfur hexafluoride. Journal Retina-Vitreus | Excluded | Not retrievable | |
| 92 | Fassbender JM, Sherman MP, Barr CC, Schaal S. Tissue plasminogen activator for subfoveal haemorrhage due to age-related macular degeneration: Comparison of 3 Treatment Modalities. Retina. 2016 Oct;36(10):1860–5. doi: 10.1097/IAE.0000000000001030. PMID: 26945238. | 43 included (39 eyes) | ||
| 93 | González-López JJ, McGowan G, Chapman E, Yorston D. Vitrectomy with subretinal tissue plasminogen activator and ranibizumab for submacular haemorrhages secondary to age-related macular degeneration: retrospective case series of 45 consecutive cases. Eye (Lond). 2016 Jul;30(7):929–35. doi: 10.1038/eye.2016.65. Epub 2016 Apr 8. PMID: 27055681; PMCID: PMC4941067. | 44 included (45 eyes) | ||
| 94 | Isizaki E, Morishita S, Sato T, Fukumoto M, Suzuki H, Kida T, Ueki M, Ikeda T. Treatment of massive subretinal hematoma associated with age-related macular degeneration using vitrectomy with intentional giant tear. Int Ophthalmol. 2016 Apr;36(2):199–206. doi: 10.1007/s10792-015-0102-6. Epub 2015 Jul 28. PMID: 26216161. | Excluded | 12 eyes | |
| 95 | Kitagawa Y, Shimada H, Mori R, Tanaka K, Yuzawa M. Intravitreal Tissue Plasminogen Activator, Ranibizumab, and Gas Injection for Submacular Haemorrhage in Polypoidal Choroidal Vasculopathy. Ophthalmology. 2016 Jun;123(6):1278–86. doi: 10.1016/j.ophtha.2016.01.035. Epub 2016 Mar 2. PMID: 26949121. | 45 included (20 eyes) | ||
| 96 | Kumar A, Roy S, Bansal M, Tinwala S, Aron N, Temkar S, Pujari A. Modified Approach in Management of Submacular Haemorrhage Secondary to Wet Age-Related Macular Degeneration. Asia Pac J Ophthalmol (Phila). 2016 Mar-Apr;5(2):143–6. doi: 10.1097/APO.0000000000000130. PMID: 26302314. | Excluded | 10 eyes | |
| 97 | Lee JP, Park JS, Kwon OW, You YS, Kim SH. Management of Acute Submacular Haemorrhage with Intravitreal Injection of Tenecteplase, Anti-vascular Endothelial Growth Factor and Gas. Korean J Ophthalmol. 2016 Jun;30(3):192–7. doi: 10.3341/kjo.2016.30.3.192. Epub 2016 May 18. PMID: 27247518; PMCID: PMC4878979. | 46 included (25 eyes) | ||
| 98 | Lin TC, Hwang DK, Lee FL, Chen SJ. Visual prognosis of massive submacular haemorrhage in polypoidal choroidal vasculopathy with or without combination treatment. J Chin Med Assoc. 2016 Mar;79(3):159–65. doi: 10.1016/j.jcma.2015.11.004. Epub 2016 Jan 8. PMID: 26775600. | 47 included (20 eyes) | ||
| 99 | Liu H, Zhang LY, Li XX, Wu MQ. 23-Gauge vitrectomy with external drainage therapy as a novel procedure to displace massive submacular haemorrhage secondary to polypoidal choroidal vasculopathy. Medicine (Baltimore). 2016 Aug;95(32):e4192. doi: 10.1097/MD.0000000000004192. PMID: 27512837; PMCID: PMC4985292. | Excluded | 4 eyes | |
| 100 | Sadeghi Y, Elalouf M, Mantel I, Pournaras JA. Vitrectomy with Gas Tamponade and anti-VEGF Injections for the Management of Submacular Haemorrhage. Klin Monbl Augenheilkd. 2016 Apr;233(4):500–2. English. doi: 10.1055/s-0042-102567. Epub 2016 Apr 26. PMID: 27116519. | Excluded | Case report | |
| 101 | Stanescu-Segall D, Balta F, Jackson TL. Submacular haemorrhage in neovascular age-related macular degeneration: A synthesis of the literature. Surv Ophthalmol. 2016 Jan-Feb;61(1):18–32. doi: 10.1016/j.survophthal.2015.04.004. Epub 2015 Jul 23. PMID: 26212151. | Excluded | Review | |
| 102 | Waizel M, Todorova MG, Kazerounian S, Rickmann A, Blanke BR, Szurman P. Efficacy of Vitrectomy Combined with Subretinal Recombinant Tissue Plasminogen Activator for Subretinal versus Subpigment Epithelial versus Combined Haemorrhages. Ophthalmologica. 2016;236(3):123–132. doi: 10.1159/000449172. Epub 2016 Sep 16. PMID: 27631507. | 48 included (19 eyes) | ||
| 103 | Bell JE, Shulman JP, Swan RJ, Teske MP, Bernstein PS. Intravitreal Versus Subretinal Tissue Plasminogen Activator Injection for Submacular Haemorrhage. Ophthalmic Surg Lasers Imaging Retina. 2017 Jan 1;48(1):26–32. doi: 10.3928/23258160-20161219-04. PMID: 28060391. | 49 included (18 eyes) | ||
| 104 | Fleissig E, Barak A, Goldstein M, Loewenstein A, Schwartz S. Massive subretinal and subretinal pigment epithelial haemorrhage displacement with perfluorocarbon liquid using a two-step vitrectomy technique. Graefes Arch Clin Exp Ophthalmol. 2017 Jul;255(7):1341–1347. doi: 10.1007/s00417-017-3648-3. Epub 2017 Apr 15. PMID: 28412773. | Excluded | 7 eyes | |
| 105 | Fotis K, Garcia-Cabrera R, Ohn M, Chandra A. Anatomical and Functional Outcome of Pars Plana Vitrectomy and Subretinal Recombinant Tissue Plasminogen Activator for a Macular Subpigment Epithelial Haemorrhage. Ophthalmologica. 2017;238(1–2):106–108. doi: 10.1159/000475891. Epub 2017 May 24. PMID: 28535542. | Excluded | Case report | |
| 106 | Gok M, Karabaş VL, Aslan MS, Kara Ö, Karaman S, Yenihayat F. Tissue plasminogen activator-assisted vitrectomy for submacular haemorrhage due to age-related macular degeneration. Indian J Ophthalmol. 2017 Jun;65(6):482–487. doi: 10.4103/ijo.IJO_129_16. PMID: 28643713; PMCID: PMC5508459. | 50 included (17 eyes) | ||
| 107 | Kimura S, Morizane Y, Matoba R, Hosokawa M, Shiode Y, Hirano M, Doi S, Toshima S, Takahashi K, Hosogi M, Fujiwara A, Shiraga F. Retinal sensitivity after displacement of submacular haemorrhage due to polypoidal choroidal vasculopathy: effectiveness and safety of subretinal tissue plasminogen activator. Jpn J Ophthalmol. 2017 Nov;61(6):472–478. doi: 10.1007/s10384-017-0530-0. Epub 2017 Aug 23. PMID: 28836011. | Excluded | 11 eyes | |
| 108 | Amy Q. Lu, Jay G. Prensky, Paul S. Baker, Ingrid U. Scott, Tamer H. Mahmoud, Bozho Todorich. (2020) Update on medical and surgical management of submacular haemorrhage. Expert Review of Ophthalmology 15:1, pages 43–57. | Excluded | Review | |
| 109 | Tan, C.S., Lim, L.W. & Ngo, W.K. Treatment of massive subretinal haemorrhage from polypoidal choroidal vasculopathy and age-related macular degeneration. Int Ophthalmol 37, 779–780 (2017). https://doi.org/10.1007/s10792-016-0351-z | Excluded | Letter to the editor | |
| 110 | Waizel M, Todorova MG, Rickmann A, Blanke BR, Szurman P. Efficacy of Vitrectomy Combined with Subretinal rt-PA Injection with Gas or Air Tamponade. Klin Monbl Augenheilkd. 2017 Apr;234(4):487–492. English. doi: 10.1055/s-0042-121575. Epub 2017 Jan 31. PMID: 28142164. | 51 included (85 eyes) | ||
| 111 | Waizel M, Todorova MG, Rickmann A, Blanke BR, Szurman P. Structural and Functional Outcome of Vitrectomy Combined with Subretinal Recombinant Tissue Plasminogen Activator for Isolated Subpigment Epithelial Haemorrhages. Ophthalmologica. 2017;238(1–2):109. doi: 10.1159/000475892. Epub 2017 May 24. PMID: 28535505. | Excluded | Letter to the editor | |
| 112 | Cochrane Central Register of Controlled Trials Impacts of pneumatic displacement of submacular haemorrhage secondary to age-related macular degeneration on retinal pigment epithelial detachment UMIN000031065 https://trialsearch.who.int/Trial2.aspx?TrialID=JPRN-UMIN000031065, 2018 | added to CENTRAL: 31 March 2019 | 2019 Issue 3 Sourced from: ICTRP Links: WHO ICTRP | Excluded | Trial registration | |
| 113 | Bardak H, Bardak Y, Erçalık Y, Erdem B, Arslan G, Timlioglu S. Sequential tissue plasminogen activator, pneumatic displacement, and anti-VEGF treatment for submacular haemorrhage. Eur J Ophthalmol. 2018 May;28(3):306–310. doi: 10.5301/ejo.5001074. PMID: 29148027. | 52 included (16 eyes) | ||
| 114 | Juncal VR, Hanout M, Altomare F, Chow DR, Giavedoni LR, Muni RH, Wong DT, Berger AR. Surgical management of submacular haemorrhage: experience at an academic Canadian centre. Can J Ophthalmol. 2018 Aug;53(4):408–414. doi: 10.1016/j.jcjo.2017.10.010. Epub 2017 Dec 23. PMID: 30119797. | 53 included (99 eyes) | ||
| 115 | Kim JH, Chang YS, Lee DW, Kim CG, Kim JW. Quantification of retinal changes after resolution of submacular haemorrhage secondary to polypoidal choroidal vasculopathy. Jpn J Ophthalmol. 2018 Jan;62(1):54–62. doi: 10.1007/s10384-017-0549-2. Epub 2017 Nov 29. PMID: 29188462. | 54 included (21 eyes) | ||
| 116 | Management of Submacular Haemorrhage in Age-Related Macular Degeneration Authors: Kim, L. A.; Eliott, D.; Journal: Ophthalmology Retina-Volume 2, Issue 3, pp. 177–179-published 2018-01-01 | Excluded | Review | |
| 117 | Kimura M, Yasukawa T, Shibata Y, Kato A, Hirano Y, Uemura A, Yoshida M, Ogura Y. Flattening of retinal pigment epithelial detachments after pneumatic displacement of submacular haemorrhages secondary to age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2018 Oct;256(10):1823–1829. doi: 10.1007/s00417-018-4059-9. Epub 2018 Jul 1. PMID: 29961921. | 55 included (33 eyes) | ||
| 118 | Ozkaya A, Erdogan G, Tarakcioglu HN. Submacular haemorrhage secondary to age-related macular degeneration managed with vitrectomy, subretinal injection of tissue plasminogen activator, haemorrhage displacement with liquid perfluorocarbon, gas tamponade, and face-down positioning. Saudi J Ophthalmol. 2018 Oct-Dec;32(4):269–274. doi: 10.1016/j.sjopt.2018.08.002. Epub 2018 Aug 15. PMID: 30581295; PMCID: PMC6300785. | Excluded | 9 eyes | |
| 119 | Sharma S, Kumar JB, Kim JE, Thordsen J, Dayani P, Ober M, Mahmoud TH. Pneumatic Displacement of Submacular Haemorrhage with Subretinal Air and Tissue Plasminogen Activator: Initial United States Experience. Ophthalmol Retina. 2018 Mar;2(3):180–186. doi: 10.1016/j.oret.2017.07.012. Epub 2017 Sep 28. PMID: 31047581. | 56 included (24 eyes) | ||
| 120 | Adrean SD, Chaili S, Pirouz A, Grant S. Rapid displacement of subretinal haemorrhage from a choroidal neovascular membrane with intravitreal C3F8 gas and face-down positioning. Am J Ophthalmol Case Rep. 2019 Mar 14;14:79–82. doi: 10.1016/j.ajoc.2019.03.003. PMID: 30949612; PMCID: PMC6428934. | Excluded | Case report | |
| 121 | Balughatta P, Kadri V, Braganza S, Jayadev C, Mehta RA, Nakhate V, Yadav NK, Shetty R. Pneumatic displacement of limited traumatic submacular haemorrhage without tissue plasminogen activator: a case series. Retin Cases Brief Rep. 2019 Winter;13(1):34–38. doi: 10.1097/ICB.0000000000000525. PMID: 28079650. | Excluded | Case report | |
| 122 | Gujral GS, Agarwal M, Mayor R, Shroff D, Chhablani J, Shanmugam MP. Clinical profile and management outcomes of traumatic submacular haemorrhage. J Curr Ophthalmol. 2019 Oct 22;31(4):411–415. doi: 10.1016/j.joco.2019.09.001. PMID: 31844792; PMCID: PMC6896465. | Excluded | Traumatic SRMH | |
| 123 | Li ZX, Hu YJ, Atik A, Lu L, Hu J. Long-term observation of vitrectomy without subretinal haemorrhage management for massive vitreous haemorrhage secondary to polypoidal choroidal vasculopathy. Int J Ophthalmol. 2019 Dec 18;12(12):1859–1864. doi: 10.18240/ijo.2019.12.07. PMID: 31850169; PMCID: PMC6901888. | Excluded | Vitreous hemorrhage without SRMH | |
| 124 | Plemel DJA, Lapere SRJ, Rudnisky CJ, Tennant MTS. VITRECTOMY WITH SUBRETINAL TISSUE PLASMINOGEN ACTIVATOR AND GAS TAMPONADE FOR SUBFOVEAL HAEMORRHAGE: Prognostic Factors and Clinical Outcomes. Retina. 2019 Jan;39(1):172–179. doi: 10.1097/IAE.0000000000001931. PMID: 29135798. | 57 included (78 eyes) | ||
| 125 | Erdogan G, Kirmaci A, Perente I, Artunay O. Gravitational displacement of submacular haemorrhage in patients with age-related macular disease. Eye (Lond). 2020 Jun;34(6):1136–1141. doi: 10.1038/s41433-019-0720-8. Epub 2019 Dec 2. PMID: 31792350; PMCID: PMC7253466. | Excluded | 9 eyes | |
| 126 | Helaiwa K, Paez LR, Szurman P, Januschowski K. Combined Administration of Preoperative Intravitreal and Intraoperative Subretinal Recombinant Tissue Plasminogen Activator in Acute Hemorrhagic Age-related Macular Degeneration. Cureus. 2020 Mar 10;12(3):e7229. doi: 10.7759/cureus.7229. PMID: 32190528; PMCID: PMC7065728. | 58 included (14 eyes) | ||
| 127 | Jeong S, Park DG, Sagong M. Management of a Submacular Haemorrhage Secondary to Age-Related Macular Degeneration: A Comparison of Three Treatment Modalities. J Clin Med. 2020 Sep 24;9(10):3088. doi: 10.3390/jcm9103088. PMID: 32987903; PMCID: PMC7601376. | 59 included (77 eyes) | ||
| 128 | Karamitsos A, Papastavrou V, Ivanova T, Cottrell D, Stannard K, Karachrysafi S, Cheristanidis S, Ziakas N, Papamitsou T, Hillier R. Management of acute submacular haemorrhage using intravitreal injection of tissue plasminogen activator and gas: A case series. SAGE Open Med Case Rep. 2020 Nov 13;8:2050313X20970337. doi: 10.1177/2050313X20970337. PMID: 33240500; PMCID: PMC7675899. | 60 included (28 eyes) | ||
| 129 | Kim JH, Kim CG, Lee DW, Yoo SJ, Lew YJ, Cho HJ, Kim JY, Lee SH, Kim JW. Intravitreal aflibercept for submacular haemorrhage secondary to neovascular age-related macular degeneration and polypoidal choroidal vasculopathy. Graefes Arch Clin Exp Ophthalmol. 2020 Jan;258(1):107–116. doi: 10.1007/s00417-019-04474-0. Epub 2019 Nov 18. PMID: 31741044. | 61 included (29 eyes) | ||
| 130 | Lee K, Park YG, Park YH. Visual prognosis after pneumatic displacement of submacular haemorrhage according to age-related macular degeneration subtypes. Retina. 2020 Dec;40(12):2304–2311. doi: 10.1097/IAE.0000000000002762. PMID: 31985556. | 62 included (67 eyes) | ||
| 131 | Amy Q. Lu, Jay G. Prensky, Paul S. Baker, Ingrid U. Scott, Tamer H. Mahmoud & Bozho Todorich (2020) Update on medical and surgical management of submacular haemorrhage, Expert Review of Ophthalmology, 15:1, 43–57, DOI: 10.1080/17469899.2020.1725474 | Excluded | Review | |
| 132 | Maggio E, Peroglio Deiro A, Mete M, Sartore M, Polito A, Prigione G, Guerriero M, Pertile G. Intravitreal Recombinant Tissue Plasminogen Activator and Sulphur Hexafluoride Gas for Submacular Haemorrhage Displacement in Age-Related Macular Degeneration: Looking behind the Blood. Ophthalmologica. 2020;243(3):224–235. doi: 10.1159/000505752. Epub 2020 Jan 7. PMID: 31905361. | 63 included (96) | ||
| 133 | Onder Tokuc, E.; Levent Karabas, V.; Surgical management of subretinal haemorrhage. Journal: Retina-Vitreus-Volume 29, Issue 0, pp. 1–9-published 2020-01-01 | Excluded | Review | |
| 134 | Sun, T.; Wan, Z.; Gao, Y.; Zhang, L.; Peng, Q. Fundus imaging features of massive hemorrhaging in polypoidal choroidal vasculopathy after treatment. International Journal of Clinical and Experimental Medicine-Volume 13, Issue 0, pp. 5736–5744-published 2020-01-01 | Excluded | Case series of 9 eyes | |
| 135 | Wilkins CS, Mehta N, Wu CY, Barash A, Deobhakta AA, Rosen RB. Outcomes of pars plana vitrectomy with subretinal tissue plasminogen activator injection and pneumatic displacement of fovea-involving submacular haemorrhage. BMJ Open Ophthalmol. 2020 Mar 16;5(1):e000394. doi: 10.1136/bmjophth-2019-000394. PMID: 32201733; PMCID: PMC7076260. | 64 included (37 eyes) | ||
| 136 | Ali Said Y, Dewilde E, Stalmans P. Visual Outcome after Vitrectomy with Subretinal rt-PA Injection to Treat Submacular Haemorrhage Secondary to Age-Related Macular Degeneration or Macroaneurysm. J Ophthalmol. 2021 Dec 30;2021:3160963. doi: 10.1155/2021/3160963. PMID: 35003789; PMCID: PMC8736698. | 65 included (93 eyes) | ||
| 137 | Avcı R, Mavi Yıldız A, Çınar E, Yılmaz S, Küçükerdönmez C, Akalp FD, Avcı E. Subretinal Coapplication of Tissue Plasminogen Activator and Bevacizumab with Concurrent Pneumatic Displacement for Submacular Haemorrhages Secondary to Neovascular Age-Related Macular Degeneration. Turk J Ophthalmol. 2021 Feb 25;51(1):38–44. doi: 10.4274/tjo.galenos.2020.72540. PMID: 33631914; PMCID: PMC7931654. | 66 included (30 patients) | ||
| 138 | Caporossi T, Bacherini D, Governatori L, Oliverio L, Di Leo L, Tartaro R, Rizzo S. Management of submacular massive haemorrhage in age-related macular degeneration: comparison between subretinal transplant of human amniotic membrane and subretinal injection of tissue plasminogen activator. Acta Ophthalmol. 2022 Aug;100(5):e1143–e1152. doi: 10.1111/aos.15045. Epub 2021 Oct 5. PMID: 34609787. | 67 included (44 eyes) | ||
| 139 | Iannetta D, De Maria M, Bolletta E, Mastrofilippo V, Moramarco A, Fontana L. Subretinal Injection of Recombinant Tissue Plasminogen Activator and Gas Tamponade to Displace Acute Submacular Haemorrhages Secondary to Age-Related Macular Degeneration. Clin Ophthalmol. 2021;15:3649–3659 https://doi.org/10.2147/OPTH.S324091 | 68 included (25 eyes) | ||
| 140 | Iyer PG, Brooks HL Jr, Flynn HW Jr. Long-Term Favorable Visual Outcomes in Patients with Large Submacular Haemorrhage. Clin Ophthalmol. 2021;15:1189–1192 https://doi.org/10.2147/OPTH.S300662 | Excluded | Case series (2 eyes) | |
| 141 | Aslı Kırmacı Kabakcı, Gürkan Erdoğan, Burcu Kemer Atik, İrfan Perente. Outcomes of Surgical Treatment in Cases with Submacular Haemorrhage. | 69 included (54 eyes) | ||
| 142 | Kawakami S, Wakabayashi Y, Umazume K, Usui Y, Muramatsu D, Agawa T, Yamamoto K, Goto H. Long-Term Outcome of Eyes with Vitrectomy for Submacular and/or Vitreous Haemorrhage in Neovascular Age-Related Macular Degeneration. J Ophthalmol. 2021 Nov 2;2021:2963822. doi: 10.1155/2021/2963822. PMID: 34765261; PMCID: PMC8577947. | 70 included (25 eyes) | ||
| 143 | Kishikova L, Saad AAA, Vaideanu-Collins D, Isac M, Hamada D, El-Haig WM. Comparison between different techniques for treatment of submacular haemorrhage due to Age-Related Macular Degeneration. Eur J Ophthalmol. 2021 Sep;31(5):2621–2624. doi: 10.1177/1120672120959551. Epub 2020 Sep 29. PMID: 32993349. | 71 included (29 eyes) | ||
| 144 | Pierre M, Mainguy A, Chatziralli I, Pakzad-Vaezi K, Ruiz-Medrano J, Bodaghi B, Loewenstein A, Ambati J, de Smet MD, Tadayoni R, Touhami S. Macular Haemorrhage Due to Age-Related Macular Degeneration or Retinal Arterial Macroaneurysm: Predictive Factors of Surgical Outcome. J Clin Med. 2021 Dec 10;10(24):5787. doi: 10.3390/jcm10245787. PMID: 34945083; PMCID: PMC8703651. | 72 included (65 eyes) | ||
| 145 | Matsuo Y, Haruta M, Ishibashi Y, Ishibashi K, Furushima K, Kato N, Murotani K, Yoshida S. Visual Outcomes and Prognostic Factors of Large Submacular Haemorrhages Secondary to Polypoidal Choroidal Vasculopathy. Clin Ophthalmol. 2021 Aug 24;15:3557–3562. doi: 10.2147/OPTH.S327138. PMID: 34465976; PMCID: PMC8403222. | 73 included (30 eyes) | ||
| 146 | Rickmann A, Paez LR, Della Volpe Waizel M, Bisorca-Gassendorf L, Schulz A, Vandebroek AC, Szurman P, Januschowski K. Functional and structural outcome after vitrectomy combined with subretinal rt-PA Injection with or without additional intravitreal Bevacizumab injection for submacular haemorrhages. PLoS ONE. 2021 Apr 30;16(4):e0250587. doi: 10.1371/journal.pone.0250587. PMID: 33930041; PMCID: PMC8087026. | 74 included (31 eyes) | ||
| 147 | Saito-Uchida S, Inoue M, Koto T, Kato Y, Hirakata A. Vitrectomy combined with subretinal injection of tissue plasminogen activator for successful treatment of massive subretinal haemorrhage. Eur J Ophthalmol. 2021 Sep;31(5):2588–2595. doi: 10.1177/1120672120970404. Epub 2020 Nov 4. PMID: 33148019. | Excluded | 11 eyes | |
| 148 | Sniatecki JJ, Ho-Yen G, Clarke B, Barbara R, Lash S, Papathomas T, Antonakis S, Gupta B. Treatment of submacular haemorrhage with tissue plasminogen activator and pneumatic displacement in age-related macular degeneration. Eur J Ophthalmol. 2021 Mar;31(2):643–648. doi: 10.1177/1120672119891625. Epub 2019 Dec 9. PMID: 31813290. | 75 included (54 eyes) | ||
| 149 | Tranos P, Tsiropoulos GN, Koronis S, Vakalis A, Asteriadis S, Stavrakas P. Comparison of subretinal versus intravitreal injection of recombinant tissue plasminogen activator with gas for submacular haemorrhage secondary to wet age-related macular degeneration: treatment outcomes and brief literature review. Int Ophthalmol. 2021 Dec;41(12):4037–4046. doi: 10.1007/s10792-021-01976-x. Epub 2021 Jul 30. PMID: 34331185. | 76 included (25 eyes) | ||
| 150 | Fukuda Y, Nakao S, Kohno RI, Ishikawa K, Shimokawa S, Shiose S, Takeda A, Morizane Y, Sonoda KH. Postoperative follow-up of submacular haemorrhage displacement treated with vitrectomy and subretinal injection of tissue plasminogen activator: ultrawide-field fundus autofluorescence imaging in gas-filled eyes. Jpn J Ophthalmol. 2022 May;66(3):264–270. doi: 10.1007/s10384-022-00910-7. Epub 2022 Mar 9. PMID: 35260984. | 77 included (24 eyes) | ||
| 151 | Jackson, T.L., Bunce, C., Desai, R. et al. Vitrectomy, subretinal Tissue plasminogen activator and Intravitreal Gas for submacular haemorrhage secondary to Exudative Age-Related macular degeneration (TIGER): study protocol for a phase 3, pan-European, two-group, non-commercial, active-control, observer-masked, superiority, randomised controlled surgical trial. Trials 23, 99 (2022). https://doi.org/10.1186/s13063-021-05966-3 | Excluded | Study protocol | |
| 152 | Kitagawa Y, Shimada H, Mori R, Tanaka K, Wakatsuki Y, Onoe H, Kaneko H, Machida Y, Nakashizuka H. One-Year Outcome of Intravitreal Tissue Plasminogen Activator, Ranibizumab, and Gas Injections for Submacular Haemorrhage in Polypoidal Choroidal Vasculopathy. J Clin Med. 2022 Apr 13;11(8):2175. doi: 10.3390/jcm11082175. PMID: 35456268; PMCID: PMC9032067. | 78 included (64 eyes) | ||
| 153 | Mehta A, Steel DH, Muldrew A, Peto T, Reeves BC, Evans R, Chakravarthy U; IVAN Study Investigators. Associations and Outcomes of Patients with Submacular Haemorrhage Secondary to Age-related Macular Degeneration in the IVAN Trial. Am J Ophthalmol. 2022 Apr;236:89–98. doi: 10.1016/j.ajo.2021.09.033. Epub 2021 Oct 6. PMID: 34626573. | 79 included (535 eyes) | ||
| 154 | Tiosano A, Gal-Or O, Fradkin M, Elul R, Dotan A, Hadayer A, Brody J, Ehrlich R. Visual acuity outcome in patients with subretinal haemorrhage-office procedure vs. surgical treatment. Eur J Ophthalmol. 2022 May 9:11206721221098208. doi: 10.1177/11206721221098208. Epub ahead of print. PMID: 35532042. | 80 included (107 eyes) | ||
| 155 | Ura S, Miyata M, Ooto S, Yasuhara S, Tamura H, Ueda-Arakawa N, Muraoka Y, Miyake M, Takahashi A, Wakazono T, Uji A, Yamashiro K, Tsujikawa A. Contrast-to-noise ratio is a useful predictor of early displacement of large submacular haemorrhage by intravitreal sf6 gas injection. Retina. 2022 Apr 1;42(4):661–668. doi: 10.1097/IAE.0000000000003360. PMID: 35350046. | 81 included (16 eyes) |
Appendix C
| Author (et al.) | Year | Study Design | Study Sample (Eyes) | Type of Surgery | Mean Size of the Bleeding | Outcome Final BCVA | Mean Days from Onset | Complications | GRADE 1 |
| Olivier [85] | 2004 | Retrospective, noncomparative, interventional case series | 29 | PPV + subretinal rt-PA + air | N/A | 17 eyes (59%) gained more than 2 lines; 3 eyes (10%) lost more than 2 lines at 3 months | 23 | 2 vitreous hemorrhages and 1 relapse | Very low |
| Ratanasukon [56] | 2005 | Retrospective, noncomparative, interventional case series | 19 | Intravitreal rt-PA + expansile gas | More than 3 disc diameters | BCVA improved 2 lines or greater in 12 eyes (63.2%), stabilized in 6 eyes (31.6%), and worsened in 1 (5.2%) (at 13 months) | 13.1 | 3 vitreous hemorrhages, 3 cataracts, and 2 retinal detachments | Very low |
| Thompson [90] | 2005 | Retrospective, comparative, interventional case series | 42 | PPV + removal of subretinal hemorrhage versus PPV + subretinal rt-PA | 12 disc diameters or less | From 20/1000–1 to 20/640–2 at 3 months | N/A | 1 RD, 1 hyphema, 2 VH | Low |
| Yang [58] | 2005 | Retrospective, comparative, interventional case series | 24 | Intravitreal injection of expansile gas, with or without adjunctive commercial rt-PA solution | N/A | BCVA improved two or more lines in 11 (45.8%) of the 24 eyes, and measured 20/100 or better in 10 (41.7%) of the 11 eyes | N/A | 2 recurrent SRMH, 7 VH, 1 massive VH | Very low |
| Mozafarieh [27] | 2006 | Longitudinal prospective study | 101 | Intravitreous plasminogen activator injection | At least one disc diameter | - | Less than 4 weeks | None | Moderate |
| Singh [57] | 2006 | Retrospective, noncomparative, interventional case series | 17 | PPV + subretinal rt-PA + air | N/A | Improvement was made in all but five patients | Mean duration before surgery was 11.9 days | 3 rebleeds, 1 RD | Very low |
| Chen [58] | 2007 | Retrospective, noncomparative, interventional case series | 85 | PPV + subretinal rt-PA + gas | N/A | 52 eyes (64%) achieved 2 Snellen acuity lines or better improvement at 3 months | Mean duration of symptoms before surgery was 9.3 days | Vitreous hemorrhage in 8 eyes (8%) and retinal detachment in 3 eyes | Low |
| Gopalakrishan [28] | 2007 | Prospective, consecutive, single-center, noncomparative, interventional case series | 20 | Intravitreal C3F8 injection without rt-PA | N/A | Mean BCVA improved from 1.6 to 0.72 LogMAR | Range from 1 to 30 days | 4 VH | Moderate |
| Ron [91] | 2007 | Retrospective, noncomparative, interventional case series | 24 | PPV + subretinal rt-PA + gas (SF 6 and C3F8) | At least 3 disc diameters | SF6 used in 13 patients (54.2%). Seven (53.8%) showed improvement of 2 lines on the Snellen chart. C3F8 was injected in 11 patients (45.8%). Four of them (36.3%) showed an improvement of 2 lines on the Snellen chart | Range from 1 to 30 days | No complications | Low |
| Stifter [59] | 2007 | Retrospective, noncomparative, interventional case series | 21 | Intravitreal bevacizumab | At least 3 disc diameters | VA improved in 48% (10/21) of the treated eyes with a mean VA gain of 0.2 0.16, was stable in 9% (2/21), and decreased in 43% (9/21) of the treated eyes with a mean VA loss of 0.1 0.06 | The mean period between symptomatic onset of submacular hemorrhage and the time of initial presentation was 12.9 days | N/A | Very low |
| Meyer [92] | 2008 | Retrospective, noncomparative, interventional case series | 19 | Intravitreal injections of recombined tissue plasminogen activator (rt-PA), expansile gas and bevacizumab | 1–3 disc diameters | VA improved two or more lines in 19% of the surgery group compared to 17% of the observation group at 3 months | Onset < 3 months | 5 High IOP > 30 mmHg | Very low |
| Fang [93] | 2009 | Retrospective, noncomparative, interventional case series | 53 | PPV with or without subretinal rt-PA + Gas | N/A | Best visual acuity improvement was significantly higher in the rt-PA and gas group than in the gas-alone group (60.7 vs. 32.0%; p = 0.037) | Duration < 14 days or > 14 days | VH and endophthalmitis | Low |
| Arias [60] | 2010 | Retrospective, noncomparative, interventional case series | 15 | PPV with intravitreal or subretinal rt-PA + Gas SF6 + intravitreal bevacizumab | 1–3 disc diameters | The mean VA (ETDRS) improved from 9.4 letters to 28.2 letters with a mean change of +18.7 letters | Within 5 days from symptoms’ onset | 3 VH and 1 RPE tear | Very low |
| Cakir [61] | 2010 | Retrospective, noncomparative, interventional case series | 21 | C3 F8 gas-assisted pneumatic displacement, with and without intravitreal rt-PA | N/A | Visual acuity in all patients either improved at least one Snellen line (n = 13) or remained the same (n = 8) | Up to 10 days | 2 recurrences | Very low |
| Fine [94] | 2010 | Retrospective, noncomparative, interventional case series | 15 | Subretinal injection of rt-PA (15 of 15) + gas tamponade (12 of 15), oil tamponade (3 of 15) | At least two quadrants | LogMAR 2.77 at baseline vs. 1.95 at 12 months follow-up | Less than 3 weeks after the onset | 6 vitreous hemorrhages, 2 RD, 1 glaucoma, 1 cataract, 1 aphakia | Very low |
| Hillenkamp [35] | 2010 | Nonrandomized, retrospective, interventional, comparative consecutive series | 47 | PPV with intravitreal injection of rt-PA and SF6 (Group A) versus PPV with subretinal injection of rt-PA and intravitreal injection of SF6 (Group B) | N/A | The difference in BCVA change between Group A and Group B was not statistically significant | 6.6 days (Group A), 5.9 days (Group B) | Group A: 1 vitreous hemorrhage and 1 recurrence; Group B: 3 RD, 2 vitreous hemorrhages | Low |
| Kung [62] | 2010 | Retrospective, interventional case series | 46 | rt-PA + C3F8 | From 0.5 to 35 disc areas (median, 8 disc areas) | Postoperative BCVA improved by 2 Snellen lines or greater in 21 of 45 eyes (46.67%) | 10 | 9 vitreous hemorrhages | Low |
| Sandhu [63] | 2010 | Retrospective, interventional case series | 16 | PPV + submacular rt-PA injection + pneumatic displacement with air followed by postoperative intravitreal ranibizumab (RZB) (12 patients) | 6 disc diameters (range 3–12) | At 6 months, 10 of 16 patients had improved by 2 lines; 10 of the 12 patients treated with RZB improved by 2, and all improved by at least 1 line. The mean number of lines of improvement was 3.4 | 12.5 | 2 recurrences (treated with another RZB injection) | Very low |
| Guthoff [36] | 2011 | Nonrandomized, retrospective, interventional, comparative consecutive series | 38 | Group A: intravitreal rt-PA + SF6 (26 patients) vs. Group B: intravitreal bevacizumab + rt-PA + SF6 (12 patients) | More than 1 disc diameter | After 7 months, BCVA was significantly higher in the bevacizumab/rt-PA/gas group (B) | 1–31 days | No complications | Low |
| Mizutani [95] | 2011 | Nonrandomized, retrospective, interventional, comparative consecutive series | 53 | Intravitreal injection SF6 with/without rt-PA | N/A | Intravitreal SF6 + rt-PA have good visual outcomes and no remarkable complications for treating submacular hemorrhage secondary to AMD. rt-PA is not recommended for ruptured retinal arterial macroaneurysms, because of a higher incidence of subsequent vitreous hemorrhage | N/A | All eyes with macroaneurysms have recurrence. 5 postoperative transient ocular hypertensions | Low |
| Treumer [64] | 2011 | Retrospective, consecutive, interventional case series | 41 | PPV + subretinal rt-PA and bevacizumab + SF6 | Mean 4.5 disc diameters (range 1.5–12) | LogMAR BCVA improved significantly from the preoperative value 1.7 (3.0–0.5) to 0.8 (1.6–0.2) | Maximum 2 weeks | 8 recurrences | Low |
| Tsymanava [37] | 2012 | Retrospective, non-randomized, comparative case study | 110 | rt-PA injection without gas injection (group A1: 50 µg of rt-PA; A2: 100 µg; A3: 200 µg) and with gas injection (group B1: 50 µg of rt-PA; B2: 100 µg; B3: 200 µg) | 12.5 (1–38) | BCVA was better in B1 and B2 groups | 10.0 (0.5–180.0) | 2 endophthalmitis, 10 vitreous hemorrhages, 3 increased intraocular pressure | Low |
| Ueda-Arakawa [103] | 2012 | Nonrandomized, retrospective, comparative consecutive series | 31 | None, the study valued the retinal structural changes associated with submacular hemorrhage and their relationships with visual prognosis | 6.0 ± 3.1 disc areas | The initial OCT detection of the IS/OS just beneath the fovea may predict good visual outcomes | 3.7 ± 2.3 months | N/A | Low |
| Cho [65] | 2013 | Retrospective, interventional case series | 27 | Anti-VEGF injection with an initial 3 loading injections by month, followed by an as-needed reinjection in patients with PCV | 18.2 ± 13.8 mm2 | LogMAR visual acuity at baseline was 1.02 ± 0.51 and improved significantly to 0.76 ± 0.48 at 12 months | 9.8 ± 7.5 days | 3 vitreous hemorrhages | Very low |
| Han [96] | 2013 | Retrospective, interventional case series | 14 | 180° peripheral temporal retinotomy, choroidal neovascular membrane (CNVM) excision, and transplantation of an autologous simple RPE sheet developed from the PED region outside the CNVM lesion | Massive submacular hemorrhage (extending to at least one temporal vessel arch) | Mean ETDRS score increased from 14.0 ± 23.4 preoperatively to 31.9 ± 23.8 at 18 months | Less than 6 months | 1 RD, 1 delayed recurrent submacular hemorrhage | Very low |
| Jain [66] | 2013 | Retrospective chart review | 14 | Anti-VEGF monotherapy | More than 2 disc areas | Mean change in VA from baseline at final follow-up was −0.58 LogMAR (range −1.6 to +1, Snellen range 20/30–20/400, median 20/60; p = 0.0022) | 4 (range 1–7) | N/A | Very low |
| Mayer [38] | 2013 | Nonrandomized, retrospective, interventional, comparative consecutive series | 45 | Group A: rt-PA (50 µg⁄0.05 mL) + SF6. Group B: bevacizumab (1.25 mg⁄0.05 mL) + SF6. Thereafter, all patients received bevacizumab | From 1 to 5 disc areas | Better VA in the rt-PA and gas group (14 letters improvement) compared with VA increase in the bevacizumab and gas group (8 letters improvement) from baseline to 12 months follow-up (p < 0.03) | N/A | 10 vitreous hemorrhages | Low |
| Rishi [39] | 2012 | Retrospective, single-center study | 46 | PPV + subretinal rt-PA (group 1); pneumatic displacement with intravitreal rt-PA and gas (group 2); pneumatic displacement with intraocular gas (group 3) | 5.6 ± 3.4 disc areas | No statistically significant difference amongst groups | 10 | 4 cataracts, 4 RD, 2 secondary glaucoma, 2 vitreous hemorrhages | Low |
| Shienbaum [97] | 2013 | Retrospective, interventional, consecutive case series | 19 | Anti-VEGF monotherapy | 39.0 mm2 (range 4.3–170.2 mm2 | The mean change in approximate ETDRS letter score from baseline was +12 letters at 3 months (p < 0.003), +18 letters at 6 months (p < 0.001), and +17 letters at 12 months follow-up (p < 0.02) | N/A | No adverse ocular or systemic events | Very low |
| Chang [98] | 2014 | Retrospective, comparative, interventional case series | 101 | PPV + subretinal rt-PA + gas tamponade with and without postsurgical antiVEGF injection | N/A | BCVA of the group that received post-operative anti-VEGF injection showed greater visual acuity improvement 6 months postoperatively compared to the group that did not receive post-operative anti-VEGF | N/A | 6 recurrences, 4 RD, 2 vitreous hemorrhages | Low |
| Iacono [29] | 2014 | Prospective interventional case series | 23 | Intravitreal ranibizumab | Occult choroidal neovascularization with flat large submacular hemorrhage > 50% of the entire lesion | At 12-months mean visual acuity improved significantly to 0.68 ± 0.41 (p = 0.04) | N/A | None | Very low |
| Kitahashi [40] | 2014 | Retrospective, comparative, interventional case series | 32 | Pneumatic displacement (SF6) + intravitreal bevacizumab vs. pneumatic displacement (SF6) alone | More than 2 disc areas | Mean BCVA in the SF6 + IVB group was significantly better than that in the SF6 group at 1, 3, and 6 months postoperatively (p 0.001, p 0.001 and p 0.001, respectively) | Less than 10 days | 1 RD | Low |
| Moisseiev [67] | 2014 | Retrospective, noncomparative, interventional case series | 31 | PPV + subretinal rt-PA | N/A | Patients who improved by at least one line in VA (change in LogMAR −0.41 ± 0.17) had worse VA at presentation and better final VA than those who did not improve (change in LogMAR 0.37 ± 0.18) | 13.4 ± 12.4 (range 1–60) days | 6 RD, 2 recurrences, 2 elevated IOP following surgery | Low |
| Dimopoulos [41] | 2015 | Retrospective, noncomparative, interventional case series | 46 | Intravitreal bevacizumab in group A (from 1 to 4 disc area), group B (from 4 to 9 DA), group C (more than 9 DA) | 6 DA | The mean BCVA increased from 0.81 LogMAR (Snellen 20/125) at baseline to 0.75 LogMAR (20/125) after 1 year. Amongst the three groups, improvement of the BCVA was found in 57% (13/23), 53% (8/15), and 38% (3/8) of eyes, respectively. | 11.5 ± 19 days (range: 1–45 days) | None | Low |
| Kadonosono [86] | 2015 | Prospective, consecutive, interventional case series | 13 | 25-gauge vitrectomy and submacular injection of rt-PA and air | N/A | Mean ETDRS score improvement was 19.4 letters at 1 month and 23.3 letters at 3 months | 19 days (range 7–40) | 1 FTMH, 1 VH | Moderate |
| Kim [68] | 2015 | Retrospective, noncomparative, interventional case series | 49 | Intravitreal anti-VEGF injection | 13.9 ± 8.8 disc areas | Mean BCVA improved from 1.14 ± 0.61 LogMAR (20/276, Snellen equivalent) to 0.82 ± 0.53 LogMAR (20/132) at 12 months | 7.25 ± 5.9 days | 10 VH | Low |
| Kimura [69] | 2015 | Prospective, noncomparative, interventional case series | 15 | PPV + subretinal rt-PA injection + air tamponade, followed by intravitreal antiVEGF injection | 5.6 ± 4.7 disc diameters (range, 1.5–20 disc diameters) | Mean BCVA at baseline (0.98 ± 0.44) had improved significantly both 1 month after surgery (0.41 ± 0.25) and at final visit (0.23 ± 0.25) | 9.5 ± 4.5 (range 5–21) days | None | Moderate |
| Shin [42] | 2015 | Retrospective, comparative, interventional case series | 82 | Pneumatic displacement (SF6 or C3F8) + intravitreal anti-VEGF vs. anti-VEGF monotherapy | N/A | Improvement in BCVA was not significantly different between the 2 groups at baseline, 3 months, or 6 months after initial treatment, but the combination therapy group showed better visual acuity at 1 month after initial treatment compared with the monotherapy group | 11.4 ± 10.4 days in the combination therapy group and 13.8 ± 11.5 days in the monotherapy group | 6 recurrences, 12 RPE tears, 5 VH, 2 RRD, 1 HRD with choroidal hemorrhage | Low |
| Wei [30] | 2015 | Prospective, nonrandomized, and noncomparative case series study | 21 | PPV + 360° retinotomy + silicon oil (Oxane 5700) tamponade | N/A | The mean BCVA in LogMAR (Snellen equivalent) significantly improved from preoperatively 2.64 (hand movement) to 1.73 (7/400), 1.50 (6/200), 1.51 (6/200), and 1.45 (7/200) at 1 month, 3 months, 6 months after the initial surgery, and final follow-up | N/A | 10 mild subretinal fibrosis | Moderate |
| Bae [105] | 2016 | Retrospective, interventional case series | 37 | Pneumatic displacement + laser or anti-VEGF | 12.9 ± 8.3 DA | The mean BCVA was 1.08 ± 0.55 at baseline, 0.74 ± 0.57 at 3 months, and 0.63 ± 0.58 at 6 months. The mean BCVA of PCV patients was significantly better than that of typical exudative AMD patients | 16.1 ± 12.5 | None | Low |
| De Jong [31] | 2016 | Prospective, noncomparative, interventional case series | 24 | Group A: PPV + gas + subretinal rt-PA; Group B: intravitreal rt-PA + gas | Group A: 11.1 DA (range 0.5–31.0); Group B: 9.7 DA (range 2.9–20.2) | Median visual acuity improvement in ETDRS lines at Week 4, 6, and 12 shows no significant differences between groups | Group A: 5 (range 1–11), Group B: 6 (range 1–14 | Group A: 3 increased IOP > 50 mmHg, 2 VH, 1 RD, 1 recurrence. Group B: 2 RD, 2 recurrences | Very low |
| Fassbender [43] | 2016 | Retrospective case series | 39 | Group A: PPV + subretinal (rt-PA) injection; Group B: pneumatic displacement (PD) + intravitreal rt-PA; Group C: PD without rt-PA | Group A: 9.1 mm2; Group B: 8.1 mm2; Group C: 9.1 mm2 | Final visual acuity improved significantly in both the vitrectomy and subretinal rt-PA injection group and the intravitreal rt-PA injection group, but not with PD alone | Group A: 5 ± 4.6; Group B: 6 ± 4.2; Group C: 6 ± 2.2 | None | Low |
| Gonzàlez-Lòpez [70] | 2016 | Retrospective, nonrandomized, and noncomparative case series study | 45 | Small gauge PPV + subretinal rt-PA + ranibizumab | 40.64 ± 20.20 mm2 | Visual acuity improved −0.59 ± 0.61 LogMAR between presentation and last follow-up | 6.98 ± 5.70 | N/A | Low |
| Kitagawa [32] | 2016 | Prospective, interventional, consecutive case series | 20 | Intravitreal rt-PA + ranibizumab + gas without vitrectomy | 11.1 ± 8.7 disc diameters (range, 2–31 disc diameters) | Mean change in ETDRS score from baseline was +13 letters | 9.9 ± 9.8 days (range 2–30 days) | 3 VH, 1 RD | Very low |
| Lee [71] | 2016 | Retrospective clinical case series | 25 | Intravitreal injections of tenecteplase, antiVEGF, and expansile gas | 7.5 ± 5.0 disc areas (range, 1.5 to 19) | BCVA improved from 1.09 ± 0.77 LogMAR at baseline to 0.52 ± 0.60 LogMAR at 12 months | 7.2 ± 8.2 days (range, 1 to 30 days) | 1 VH, 1 RPE tear | Very low |
| Lin [44] | 2016 | Retrospective, comparative, interventional case series | 20 | Group A: subretinal rt-PA + PPV; Group B: or intravitreal rt-PA + gas to achieve pneumatic displacement. Additionally, combination treatment with either (PDT) or intravitreal injection of anti-VEGF was performed | 17.8 ± 19.2 disc diameter (DD) compared (2.64 DD) | Combination treatment with PDT showed significant efficacy in the improvement of BCVA | 14.3 ± 16.6 days | 2 VH | Very low |
| Waizel [72] | 2016 | Observational analysis | 83 | PPV + rt-PA + gas for subretinal hemorrhages (SRH), subpigment epithelial hemorrhages (SPH), and combined subretinal and subpigment epithelial hemorrhages (CH). 68.7% received additional anti-VEGF | N/A | Vitrectomy combined with subretinal rt-PA injection and gas or air tamponade has a strong functional and anatomical effect on both SRH and CH and also seems to slightly improve the anatomical outcome in SPH | 13.4 ± 13.4 in CH; 8.3 ± 10.3 in SRH; 4.9 ± 8.0 in SPH | 1 FTMH, 1 RD, 3 recurrences | Low |
| Bell [45] | 2017 | Retrospective chart review | 18 | Pneumatic displacement followed by intravitreal rt-PA if needed vs. PPV with subretinal rt-PA | N/A | The percentage of patients achieving three lines or greater improvement at 1 year was 46% and 18% in these groups; the difference was not statistically significant | N/A | 1 recurrence | Very low |
| Gok [73] | 2017 | Retrospective, nonrandomized, consecutive case series | 17 | PPV + subretinal rt-PA + SF6 | 8.6 ± 5.3 disc areas | Improvement from initial VA (mean LogMAR, 1.8 ± 0.3) and the final BCVA (mean LogMAR, 0.97 ± 0.52) | 12.8 ± 18.2 days | 1 recurrence, 1 RRD | Very low |
| Waizel [74] | 2017 | Retrospective observational study | 85 | PPV with rt-PA combined with gas or air tamponade | N/A | In air tamponade group, mean VA improved from LogMAR 1.42 ± 0.52 to LogMAR 1.25 ± 0.51 (20/530 to 20/355 Snellen equivalent, average gain in visual acuity of 1.7 lines). In gas tamponade group, VA improved from LogMAR 1.37 ± 0.42 to LogMAR 1.29 ± 0.39 (20/471 to 20/394 Snellen equivalent, average gain in visual acuity of 0.8 lines) | 13.5 ± 12.3 days in gas tamponade; 10.9 ± 15.2 days in air tamponade | 1 FTMH, 3 recurrences | Low |
| Bardak [75] | 2018 | Retrospective pilot study | 16 | Intravitreal rt-PA + pneumatic displacement + anti-VEGF | N/A | Mean BCVA was 2.08 ± 0.79 LogMAR at baseline, 1.09 ± 0.73 LogMAR at the last follow up | 7.9 ± 3.6 days | 1 retinal pigment epithelium tear | Very low |
| Juncal [84] | 2018 | Retrospective case series | 99 | PPV + subretinal rt-PA + pneumatic displacement | 15.7% 1–5 DA; 18.6% 6–10 DA; 65.7% > 10 DA | Mean LogMAR BCVA improved from 2.03 ± 0.81 (Snellen 20/2143) at baseline to 1.80 ± 1.00 (Snellen 20/1262) at final follow-up | 19.6 ± 29.1 (2–160) | 13 VH, 8 RD, 4 RPE tears, 2 expulsive choroidal hemorrhages, 12 recurrences | Low |
| Kim [87] | 2017 | Retrospective observational study | 21 | Anti-VEGF monotherapy | 19.3 ± 9.1 mm2 (range: 5.6 to 32.3 mm2) | From 0.86 ± 0.39 LogMAR at baseline to 0.53 ± 0.43 LogMAR after resolution of the hemorrhage | 16.0 ± 10.1 | N/A | Very low |
| Kimura [99] | 2018 | Retrospective analysis | 33 | Pneumatic displacement with SF6 with or without rt-PA | N/A | The BCVAs improved significantly in eyes with PCV compared with eyes with typical AMD | N/A | 4 persistent PED | Low |
| Sharma [76] | 2017 | Retrospective, noncomparative, interventional case series | 24 | PPV + subretinal air injection in combination with rt-PA + partial fluid–gas exchange and preoperative, intraoperative, or postoperative anti-VEGF | Small (does not reach arcades) in 6 patients (25%), large (extending to the arcades) in 2 patients (8.3%), extensive (extending past the arcades) in 9 patients (37.5%), and massive (extending to 2 quadrants, past the equator, or both) in 7 patients (29.2%) | Mean preoperative VA was 1.95 (Snellen equivalent, 20/1783), mean postoperative VA was 0.85 LogMAR (Snellen equivalent, 20/141) | 11.3 days (range, 1–59 days; median, 9 days) | 5 recurrences, 3 VH, 2 RD, 1 FTMH | Very low |
| Plemel [100] | 2019 | Retrospective, noncomparative, interventional case series | 78 | PPV + subretinal rt-PA + gas tamponade | 13.6 DA | Visual acuity improved from 20/1449 preoperatively to 20/390 after a mean follow-up time of 6.3 months, corresponding to approximately 5 lines of Snellen acuity improvement | N/A | 9 recurrences | Low |
| Helaiwa [101] | 2020 | Single-center, case series report | 14 | Intravitreal rt-PA + (next day) PPV + subretinal rt-PA + air tamponade | 21.6 ± 17.8 mm2 | Significant (p = 0.01) overall improvement in the visual acuity post-treatment (from 1.4 ± 0.5 log MAR to 0.9 ± 0.4) | N/A | None | Very low |
| Jeong [46] | 2020 | Retrospective chart review | 77 | Group A: anti-VEGF monotherapy, Group B: PD + anti-VEGF; Group C: PPV + subretinal rt-PA and gas tamponade | Three groups according to the dimensions: small-sized (optic disc diameter (ODD) ≥1 to <4), medium-sized (ODD ≥ 4 within the temporal arcade) and large-sized (ODD ≥ 4, exceeding the temporal arcade) | In the small-sized group, all treatment modalities showed a gradual BCVA improvement. In the medium-sized group, PD and surgery were associated with better BCVA than anti-VEGF monotherapy (67% and 83%, respectively, vs. 33%). In the large-sized group, surgery showed a better visual improvement with a higher displacement rate than PD (86% vs. 25%) | 14.3 ± 25.8 | 1 recurrence, 1 RPE rip, 1 FTMH | Low |
| Karamitsos [77] | 2020 | Retrospective case series | 28 | Intravitreal rt-PA + gas ± anti-VEGF | 4.9 mm in patients with no anatomical displacement; 4.5 ± 1.4 mm in patients with anatomical displacement | The mean improvement of all patients with anatomical displacement of the hemorrhage in visual acuity was 0.7 ± 0.5 (LogMAR) in 1 month | 3.5 ± 2.1 days in patients with no anatomical displacement and 3.4 ± 3.6 days in patients with anatomical displacement | 2 VH, 1 RD | Very low |
| Kim [104] | 2019 | Retrospective, nonrandomized, and noncomparative case series study | 29 | Intravitreal aflibercept | 6.2 ± 4.8 DA | BCVA significantly improved from 52.9 ± 17.8 ETDRS letters at week 0 to 71.8 ± 16.1 letters at week 56 | ≤7 days in 18 patients (62.1%), >7 days but ≤1 month in 7 patients (24.1%), and >1 month but <3 months in 4 patients (13.8%) | 8 reactivations | Very low |
| Lee [78] | 2020 | Retrospective, comparative, interventional case series | 67 | Pneumatic displacement among patients with different subtypes of age-related macular degeneration (AMD): typical AMD, polypoidal choroidal vasculopathy (PCV), and retinal angiomatous proliferation (RAP) | 6.63 ± 4.66 DA in typical AMD; 5.95 ± 4.58 DA in PCV; 8.35 ± 4.00 DA in RAP | The proportion of eyes with improved visual acuity was highest in the PCV subtype and lowest in the RAP subtype | 7.85 ± 6.89 | N/A | Low |
| Maggio [47] | 2020 | Retrospective, noncomparative, interventional case series | 96 | Intravitreal rt-PA + SF6 for guiding the selection of additional treatments (anti-VEGF, PDT, or submacular surgery) or observation (CNV) | At least 3 DA involving the fovea | BCVA improved from 1.8 (SD = 0.96) LogMAR to BCVA significantly improved to 1.29 (SD = 0.78) LogMAR at 3 months | Less than 14 days | 7 recurrences, 2 VH | Low |
| Wilkins [102] | 2020 | Retrospective, interventional case series | 37 | PPV + subretinal rt-PA + pneumatic displacement | N/A | Median preoperative VA was 20/2000, at postoperative month 3 was 20/152 | N/A | 5 VH, 4 recurrent H, 3 RD, 1 blood stained cornea, 1 glaucoma, 1 phthisis | Low |
| Ali Said [79] | 2021 | Retrospective analysis | 93 | PPV + subretinal rt-PA + air | N/A | Mean BCVA at baseline was 0.06 Snellen; after the surgery, BCVA improved to 0.16 Snellen; at 8 months, decreased to 0.08 Snellen | The majority of eyes were operated within two days after the onset of the hemorrhage (60, 2%), 90.3% of eyes within one week, and all 93 eyes within 14 days | 2 RPE tears, 7 VH, 4 hyphema, 6 RD, 2 subchoroidal hemorrhages | Low |
| Avci [80] | 2021 | Retrospective study | 30 | PPV + C3F8 5% + subretinal rt-PA + anti-VEGF | 61.95 ± 43.47 (range: 10.75–176.42) mm2 | Mean VA improved from LogMAR 2.11 ± 0.84 at baseline to LogMAR 1.32 ± 0.91, 0.94 ± 0.66, 1.13 ± 0.84, and 1.00 ± 0.70 at postoperative month 1, 2, 3, and 6, respectively | 13.70 ± 8.05 (range: 2–30) days | 2 recurrences | Low |
| Caporossi [88] | 2022 | Retrospective, consecutive, comparative, non-randomized interventional study | 44 | Group A: PPV + massive submacular hemorrhage and neovascular membrane removal + hAM subretinal implant + silicone oil; Group B: PPV + subretinal rt-PA + SF6 20% | N/A | Mean preoperative BCVA was 1.9 LogMARin the amniotic membrane group and 2 LogMAR in the rt-PA group. The mean final BCVA values were 1.25 and 1.4 LogMAR, respectively, with a statistically significant difference | 25.9 ± 36 days (range, 1–150 days) | 2 VH, 2 RD | Low |
| Iannetta [81] | 2021 | Single-center, retrospective, case series | 25 | PPV + subretinal rt-PA + SF6 20% | 68.34 ± 42.42 mm2 | BCVA significantly improved from 1.81 ± 0.33 to 1.37 ± 0.52 LogMAR at 12 months from surgery | 9.24 (±3.37) | 2 recurrences, 1 RD | Very low |
| Asli [48] | Retrospective case series | 54 | - 21 eyes PPV + submacular rt-PA + 20% SF6 or 14% C3F8; - 14 eyes PPV + submacular rt-PA + 20% SF6 or 14% C3F8 + antiVEGF; - 10 eyes PPV + subretinal rt-PA without gas; - 4 eyes intravitreal gas + rt-PA; - 3 eyes PPV + subretinal rt-PA + drainage; - 2 eyes intravitreal gas + intravitreal antiVEGF | 31.5 ± 26.5 (2.8–145.3) mm2 | BCVA improved from 2.0 ± 0.8 (0.3–3) at presentation to 1.67 ± 0.87 (0.22–3) LogMAR on postoperative month 1, 1.65 ± 0.79 (0.40–3) LogMAR on month 3, 1.76 ± 0.88 (0.22–3) LogMAR on month 6, 1.71 ± 0.85 (0.30–3) LogMAR at year 1, and 1.76 ± 0.81 (0.22–3) LogMAR at final visit | 13.7 ± 16.3 (1–95) days | 6 RD, 3 VH, 2 FTMH, 4 recurrences | Low | |
| Kawakami [82] | 2021 | Retrospective case series | 25 | PPV ± anti-VEGF (2 eyes in SMH group) | 4.0 ± 1.6 (range 2.0–6.7) disc diameters | BCVA improved in eyes with SMH at 6 and 12 months after PPV, and the BCVA was maintained until the end of the study (24 months) | 9.3 ± 4.6 (range 4–17) | 2 FTMH | Very low |
| Kishikova [49] | 2020 | Retrospective analysis | 29 | Group 1: intravitreal rt-PA + SF6 Group 2: PPV + subretinal rt-PA + SF6 with (2A) or without (2B) subretinal air | 9.45 DD ± 2.34 in Group 1 and 9.72 DD ± 2.02 in Group 2 | The mean BCVA at presentation was 0.0068 in Group 1 and 0.0067 in Group 2. The mean postoperative BCVA at 6 months was 0.31 in Group 1 and 0.58 in Group 2. Subgroup analysis of Group 2 did not show statistically significant difference in outcome when adding subretinal air to the vitrectomy procedure | N/A | 3 high IOP, 2 RD, 3 cataracts | Very low |
| Pierre [13] | 2021 | Multicentric retrospective case series | 65 | PPV + subretinal rt-PA + gas | 5441.3 ± 1323.1 microns in AMD group; 5085.2 ± 3012.3 microns in RAM group | BCVA improved from 20/500 to 20/125 at month 1 and month 6 | 7.1 ± 6.7 days (range 0–30 days) | 7 VH, 5 RRD, 7 recurrences | Low |
| Matsuo [50] | 2021 | Retrospective study | 30 | 13 eyes underwent pneumatic displacement, 22 eyes received anti-VEGF therapy, and four eyes underwent PPV | 17.0 ± 4.8 disc areas | The mean BCVA at the development, 1 month, and 1 year after the development of large SMHs, and at the final visit were LogMAR 0.88 ± 0.61 (Snellen equivalent 20/151), LogMAR 1.12 ± 0.82 (Snellen equivalent 20/263), LogMAR 0.84 ± 0.72 (Snellen equivalent 20/138), and LogMAR 0.88 ± 0.75 (Snellen equivalent 20/152), respectively | N/A | 2 VH, 1 RRD | Low |
| Rickmann [51] | 2021 | Retrospective, consecutive case series | 31 | PPV + subretinal rt-PA + air displacement with (group +B) or without Group − B) intravitreal bevacizumab | 11.78 ± 3.04 mm2 in +B; 14.75 ± 3.98 mm2 in −B | The mean visual acuity improved significantly in both groups, from 1.37 ± 0.39 to 1.03 ± 0.57 LogMAR in +B and from 1.48 ± 0.48 to 1.01 ± 0.38 LogMAR in group B | 3.3 ± 1.6 in +B; 3.4 ± 1.5 in −B | 1 FTMH, 2 RD, 1 recurrence | Low |
| Sniatecki [52] | 2019 | Retrospective study | 54 | PPV + subretinal rt-PA + pneumatic displacement vs. antiVEGF monotherapy | In rt-PA group, 5.0 DA; in anti-VEGF group, 4.2 DA | Mean LogMAR in rt-PA group at baseline was 1.56, and it was improved at 1 year to 1.07. Mean BCVA in anti-VEGF group at baseline was 1.22 LogMAR with no significant improvement (1.36 at 1 year) | 5 days (range 1–13) | 2 RD, 3 VH, 7 cataracts | Low |
| Tranos [53] | 2021 | Retrospective, comparative, interventional case series | 25 | Group A: PPV + subretinal rt-PA + gas; Group B: intravitreal rt-PA + gas | 4.604 ± 2079 µm | BCVA improved significantly but did not differ between the 2 groups | 8.2 (±7.3) days | N/A | Very low |
| Fukuda [83] | 2022 | Retrospective, consecutive case series | 24 | PPV + subretinal rt-PA | N/A | BCVAs at baseline (1.16 ± 0.52) had improved significantly at the final visit (0.52 ± 0.39) | 11.5 ± 6.6 days | N/A | Very low |
| Kitagawa [33] | 2022 | Extended study of a previous prospective study | 64 | Intravitreal rt-PA + ranibizumab + gas injection | 8 ± 6 (range, 2–27) disc diameters | Mean ETDRS score increased from 58 at baseline to 64 letters | 7 ± 7 (range, 1–30) days | 46 recurrences | Low |
| Mehta [34] | 2021 | Secondary analyses of a randomized, controlled trial of image and clinical data | 535 | Randomly divided into monthly ranibizumab, as-needed ranibizumab, monthly bevacizumab or as-needed bevacizumab | 89% were smaller than 1 standard disc area | SMH at baseline was associated with worse baseline BCVA compared with eyes with no SMH (median letters, 62 vs. 68; p < 0.001; estimate of difference 6 letters, 95% CI, 4–8 letters). By month 12, the BCVA had improved in both groups (median letters 71 vs. 75) and was not significantly associated with the presence of baseline SMH (p = 0.570) | N/A | 1 RPE tear, 28 fibrosis, 10 atrophic scars, 6 geographic atrophies, 7 epiretinal membranes | Moderate |
| Tiosano [54] | 2022 | Retrospective study | 107 | Group A: intravitreal injection of rt-PA + gas; Group B: PPV | 767 microns in Group A and 962.5 microns in Group B | Visual acuity (in LogMAR) was similar in the two groups prior to the diagnosis of subretinal hemorrhage but better in the rt-PA and gas group at the end of follow-up | N/A | N/A | Low |
| Ura [89] | 2022 | Retrospective study | 16 | Investigate predictors of early displacement of submacular hemorrhage by simple intravitreal SF6 gas injections before inception of subretinal rt-PA | 33.10 ± 13.98 mm2 | LogMAR BCVA at 1 week after the injection showed no statistically significant association with any of the measured parameters | 20.6 ± 44.2 days | N/A | Very low |
| 1 Grading of Recommendations Assessment, Development and Evaluation (GRADE) system [25,26]. | |||||||||
References
- Kanukollu, V.M.; Ahmad, S.S. Retinal Haemorrhage; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Shukla, U.V.; Kaufman, E.J. Intraocular Haemorrhage; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Ohji, M.; Saito, Y.; Hayashi, A.; Lewis, J.M.; Tano, Y. Pneumatic Displacement of Subretinal Haemorrhage without Tissue Plasminogen Activator. Arch. Ophthalmol. 1998, 116, 1326–1332. [Google Scholar] [CrossRef]
- Nayak, S.; Padhi, T.R.; Basu, S.; Das, T. Pneumatic Displacement and Intra-Vitreal Bevacizumab in Management of Sub-Retinal and Sub-Retinal Pigment Epithelial Haemorrhage at Macula in Polypoidal Choroidal Vasculopathy (PCV): Rationale and Outcome. Semin. Ophthalmol. 2015, 30, 53–55. [Google Scholar] [CrossRef]
- Thuruthumaly, C.; Yee, D.C.; Rao, P.K. Presumed Ocular Histoplasmosis. Curr. Opin. Ophthalmol. 2014, 25, 508–512. [Google Scholar] [CrossRef]
- Moriyama, M.; Ohno-Matsui, K.; Shimada, N.; Hayashi, K.; Kojima, A.; Yoshida, T.; Tokoro, T.; Mochizuki, M. Correlation between Visual Prognosis and Fundus Autofluorescence and Optical Coherence Tomographic Findings in Highly Myopic Eyes with Submacular Haemorrhage and without Choroidal Neovascularization. Retina 2011, 31, 74–80. [Google Scholar] [CrossRef]
- Nakamura, H.; Hayakawa, K.; Sawaguchi, S.; Gaja, T.; Nagamine, N.; Medoruma, K. Visual Outcome after Vitreous, Sub-Internal Limiting Membrane, and/or Submacular Haemorrhage Removal Associated with Ruptured Retinal Arterial Macroaneurysms. Graefes Arch. Clin. Exp. Ophthalmol. 2008, 246, 661–669. [Google Scholar] [CrossRef]
- Avery, R.L.; Fekrat, S.; Hawkins, B.S.; Bressler, N.M. Natural History of Subfoveal Subretinal Haemorrhage in Age-Related Macular Degeneration. Retina 1996, 16, 183–189. [Google Scholar] [CrossRef]
- Stevens, T.S.; Bressler, N.M.; Maguire, M.G.; Bressler, S.B.; Fine, S.L.; Alexander, J.; Phillips, D.A.; Margherio, R.R.; Murphy, P.L.; Schachat, A.P. Occult Choroidal Neovascularization in Age-Related Macular Degeneration. A Natural History Study. Arch. Ophthalmol. 1997, 115, 345–350. [Google Scholar] [CrossRef]
- Bressler, N.M.; Bressler, S.B.; Childs, A.L.; Haller, J.A.; Hawkins, B.S.; Lewis, H.; MacCumber, M.W.; Marsh, M.J.; Redford, M.; Sternberg, P.; et al. Surgery for Hemorrhagic Choroidal Neovascular Lesions of Age-Related Macular Degeneration: Ophthalmic Findings: SST Report No. 13. Ophthalmology 2004, 111, 1993–2006. [Google Scholar] [CrossRef]
- Fleckenstein, M.; Keenan, T.D.L.; Guymer, R.H.; Chakravarthy, U.; Schmitz-Valckenberg, S.; Klaver, C.C.; Wong, W.T.; Chew, E.Y. Age-Related Macular Degeneration. Nat. Rev. Dis. Primer 2021, 7, 31. [Google Scholar] [CrossRef]
- Steel, D.H.W.; Sandhu, S.S. Submacular Haemorrhages Associated with Neovascular Age-Related Macular Degeneration. Br. J. Ophthalmol. 2011, 95, 1051–1057. [Google Scholar] [CrossRef]
- Pierre, M.; Mainguy, A.; Chatziralli, I.; Pakzad-Vaezi, K.; Ruiz-Medrano, J.; Bodaghi, B.; Loewenstein, A.; Ambati, J.; de Smet, M.D.; Tadayoni, R.; et al. Macular Haemorrhage Due to Age-Related Macular Degeneration or Retinal Arterial Macroaneurysm: Predictive Factors of Surgical Outcome. J. Clin. Med. 2021, 10, 5787. [Google Scholar] [CrossRef]
- Al-Hity, A.; Steel, D.H.; Yorston, D.; Gilmour, D.; Koshy, Z.; Young, D.; Hillenkamp, J.; McGowan, G. Incidence of Submacular Haemorrhage (SMH) in Scotland: A Scottish Ophthalmic Surveillance Unit (SOSU) Study. Eye 2019, 33, 486–491. [Google Scholar] [CrossRef]
- McGowan, G.F.; Steel, D.; Yorston, D. AMD with Submacular Haemorrhage: New Insights from a Population-Based Study. Investig. Ophthalmol. Vis. Sci. 2014, 55, 662. [Google Scholar]
- A Historic Shift: More Elderly than Children and Teenagers. Available online: https://www.ssb.no/en/befolkning/artikler-og-publikasjoner/a-historic-shift-more-elderly-than-children-and-teenagers (accessed on 16 August 2022).
- Scupola, A.; Coscas, G.; Soubrane, G.; Balestrazzi, E. Natural History of Macular Subretinal Haemorrhage in Age-Related Macular Degeneration. Ophthalmologica 1999, 213, 97–102. [Google Scholar] [CrossRef]
- Glatt, H.; Machemer, R. Experimental Subretinal Haemorrhage in Rabbits. Am. J. Ophthalmol. 1982, 94, 762–773. [Google Scholar] [CrossRef]
- Papanikolaou, G.; Pantopoulos, K. Iron Metabolism and Toxicity. Toxicol. Appl. Pharmacol. 2005, 202, 199–211. [Google Scholar] [CrossRef]
- Imam, M.U.; Zhang, S.; Ma, J.; Wang, H.; Wang, F. Antioxidants Mediate Both Iron Homeostasis and Oxidative Stress. Nutrients 2017, 9, 671. [Google Scholar] [CrossRef]
- Hochman, M.A.; Seery, C.M.; Zarbin, M.A. Pathophysiology and Management of Subretinal Haemorrhage. Surv. Ophthalmol. 1997, 42, 195–213. [Google Scholar] [CrossRef]
- Hassan, A.S.; Johnson, M.W.; Schneiderman, T.E.; Regillo, C.D.; Tornambe, P.E.; Poliner, L.S.; Blodi, B.A.; Elner, S.G. Management of Submacular Haemorrhage with Intravitreous Tissue Plasminogen Activator Injection and Pneumatic Displacement. Ophthalmology 1999, 106, 1900–1906; discussion 1906–1907. [Google Scholar] [CrossRef]
- Balughatta, P.; Kadri, V.; Braganza, S.; Jayadev, C.; Mehta, R.A.; Nakhate, V.; Yadav, N.K.; Shetty, R. Pneumatic displacement of limited traumatic submacular haemorrhage without tissue plasminogen activator: A case series. Retin. Cases Brief Rep. 2019, 13, 34–38. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Howick, J.; Glasziou, P.; Aronson, J.K. Evidence-Based Mechanistic Reasoning. J. R. Soc. Med. 2010, 103, 433–441. [Google Scholar] [CrossRef]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; deBeer, H.; et al. GRADE Guidelines: 1. Introduction—GRADE Evidence Profiles and Summary of Findings Tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef]
- Mozaffarieh, M.; Heinzl, H.; Sacu, S.; Wedrich, A. In-Patient Management and Treatment Satisfaction after Intravitreous Plasminogen Activator Injection. Graefes Arch. Clin. Exp. Ophthalmol. 2006, 244, 1421–1428. [Google Scholar] [CrossRef]
- Gopalakrishan, M.; Giridhar, A.; Bhat, S.; Saikumar, S.J.; Elias, A.; Sandhya, N. Pneumatic Displacement of Submacular Haemorrhage: Safety, Efficacy, and Patient Selection. Retina 2007, 27, 329–334. [Google Scholar] [CrossRef]
- Iacono, P.; Parodi, M.B.; Introini, U.; La Spina, C.; Varano, M.; Bandello, F. Intravitreal Ranibizumab for Choroidal Neovascularization with Large Submacular Haemorrhage in Age-Related Macular Degeneration. Retina 2014, 34, 281–287. [Google Scholar] [CrossRef]
- Wei, Y.; Zhang, Z.; Jiang, X.; Li, F.; Zhang, T.; Qiu, S.; Yang, Y.; Zhang, S. A surgical approach to large subretinal haemorrhage using pars plana vitrectomy and 360° retinotomy. Retina 2015, 35, 1631–1639. [Google Scholar] [CrossRef]
- De Jong, J.H.; van Zeeburg, E.J.; Cereda, M.G.; van Velthoven, M.E.; Faridpooya, K.; Vermeer, K.A.; van Meurs, J.C. Intravitreal versus subretinal administration of recombinant tissue plasminogen activator combined with gas for acute submacular haemorrhages due to age-related macular degeneration: An Exploratory Prospective Study. Retina 2016, 36, 914–925. [Google Scholar] [CrossRef]
- Kitagawa, Y.; Shimada, H.; Mori, R.; Tanaka, K.; Yuzawa, M. Intravitreal Tissue Plasminogen Activator, Ranibizumab, and Gas Injection for Submacular Haemorrhage in Polypoidal Choroidal Vasculopathy. Ophthalmology 2016, 123, 1278–1286. [Google Scholar] [CrossRef]
- Kitagawa, Y.; Shimada, H.; Mori, R.; Tanaka, K.; Wakatsuki, Y.; Onoe, H.; Kaneko, H.; Machida, Y.; Nakashizuka, H. One-Year Outcome of Intravitreal Tissue Plasminogen Activator, Ranibizumab, and Gas Injections for Submacular Haemorrhage in Polypoidal Choroidal Vasculopathy. J. Clin. Med. 2022, 11, 2175. [Google Scholar] [CrossRef]
- Mehta, A.; Steel, D.H.; Muldrew, A.; Peto, T.; Reeves, B.C.; Evans, R.; Chakravarthy, U.; IVAN Study Investigators. Associations and Outcomes of Patients with Submacular Haemorrhage Secondary to Age-Related Macular Degeneration in the IVAN Trial. Am. J. Ophthalmol. 2022, 236, 89–98. [Google Scholar] [CrossRef]
- Hillenkamp, J.; Surguch, V.; Framme, C.; Gabel, V.P.; Sachs, H.G. Management of Submacular Haemorrhage with Intravitreal versus Subretinal Injection of Recombinant Tissue Plasminogen Activator. Graefes Arch. Clin. Exp. Ophthalmol. 2010, 248, 5–11. [Google Scholar] [CrossRef]
- Guthoff, R.; Guthoff, T.; Meigen, T.; Goebel, W. Intravitreous Injection of Bevacizumab, Tissue Plasminogen Activator, and Gas in the Treatment of Submacular Haemorrhage in Age-Related Macular Degeneration. Retina 2011, 31, 36–40. [Google Scholar] [CrossRef]
- Tsymanava, A.; Uhlig, C.E. Intravitreal Recombinant Tissue Plasminogen Activator without and with Additional Gas Injection in Patients with Submacular Haemorrhage Associated with Age-Related Macular Degeneration. Acta Ophthalmol. 2012, 90, 633–638. [Google Scholar] [CrossRef]
- Mayer, W.J.; Hakim, I.; Haritoglou, C.; Gandorfer, A.; Ulbig, M.; Kampik, A.; Wolf, A. Efficacy and Safety of Recombinant Tissue Plasminogen Activator and Gas versus Bevacizumab and Gas for Subretinal Haemorrhage. Acta Ophthalmol. 2013, 91, 274–278. [Google Scholar] [CrossRef]
- Rishi, E.; Gopal, L.; Rishi, P.; Sengupta, S.; Sharma, T. Submacular Haemorrhage: A Study amongst Indian Eyes. Indian J Ophthalmol. 2012, 60, 521–525. [Google Scholar] [CrossRef]
- Kitahashi, M.; Baba, T.; Sakurai, M.; Yokouchi, H.; Kubota-Taniai, M.; Mitamura, Y.; Yamamoto, S. Pneumatic Displacement with Intravitreal Bevacizumab for Massive Submacular Haemorrhage Due to Polypoidal Choroidal Vasculopathy. Clin. Ophthalmol. 2014, 8, 485–492. [Google Scholar] [CrossRef]
- Dimopoulos, S.; Leitritz, M.A.; Ziemssen, F.; Voykov, B.; Bartz-Schmidt, K.U.; Gelisken, F. Submacular Predominantly Hemorrhagic Choroidal Neovascularization: Resolution of Bleedings under Anti-VEGF Therapy. Clin. Ophthalmol. 2015, 9, 1537–1541. [Google Scholar] [CrossRef]
- Shin, J.Y.; Lee, J.M.; Byeon, S.H. Anti-Vascular Endothelial Growth Factor with or without Pneumatic Displacement for Submacular Haemorrhage. Am. J. Ophthalmol. 2015, 159, 904–914.E1. [Google Scholar] [CrossRef]
- Fassbender, J.M.; Sherman, M.P.; Barr, C.C.; Schaal, S. Tissue plasminogen activator for subfoveal haemorrhage due to age-related macular degeneration: Comparison of 3 Treatment Modalities. Retina 2016, 36, 1860–1865. [Google Scholar] [CrossRef]
- Lin, T.C.; Hwang, D.K.; Lee, F.L.; Chen, S.J. Visual Prognosis of Massive Submacular Haemorrhage in Polypoidal Choroidal Vasculopathy with or without Combination Treatment. J. Chin. Med. Assoc. 2016, 79, 159–165. [Google Scholar] [CrossRef]
- Bell, J.E.; Shulman, J.P.; Swan, R.J.; Teske, M.P.; Bernstein, P.S. Intravitreal Versus Subretinal Tissue Plasminogen Activator Injection for Submacular Haemorrhage. Ophthalmic Surg. Lasers Imaging Retina 2017, 48, 26–32. [Google Scholar] [CrossRef]
- Jeong, S.; Park, D.G.; Sagong, M. Management of a Submacular Haemorrhage Secondary to Age-Related Macular Degeneration: A Comparison of Three Treatment Modalities. J. Clin. Med. 2020, 9, 3088. [Google Scholar] [CrossRef]
- Maggio, E.; Peroglio Deiro, A.; Mete, M.; Sartore, M.; Polito, A.; Prigione, G.; Guerriero, M.; Pertile, G. Intravitreal Recombinant Tissue Plasminogen Activator and Sulphur Hexafluoride Gas for Submacular Haemorrhage Displacement in Age-Related Macular Degeneration: Looking behind the Blood. Ophthalmologica 2020, 243, 224–235. [Google Scholar] [CrossRef]
- Kabakcı, A.K.; Erdoğan, G.; Atik, B.K.; Perente, İ. Outcomes of Surgical Treatment in Cases with Submacular Haemorrhage. Retin.-Vitr. J. Retin.-Vitr. 2021, 30, 2. [Google Scholar]
- Kishikova, L.; Saad, A.A.A.; Vaideanu-Collins, D.; Isac, M.; Hamada, D.; El-Haig, W.M. Comparison between Different Techniques for Treatment of Submacular Haemorrhage Due to Age-Related Macular Degeneration. Eur. J. Ophthalmol. 2021, 31, 2621–2624. [Google Scholar] [CrossRef]
- Matsuo, Y.; Haruta, M.; Ishibashi, Y.; Ishibashi, K.; Furushima, K.; Kato, N.; Murotani, K.; Yoshida, S. Visual Outcomes and Prognostic Factors of Large Submacular Haemorrhages Secondary to Polypoidal Choroidal Vasculopathy. Clin. Ophthalmol. 2021, 15, 3557–3562. [Google Scholar] [CrossRef]
- Rickmann, A.; Paez, L.R.; Della Volpe Waizel, M.; Bisorca-Gassendorf, L.; Schulz, A.; Vandebroek, A.C.; Szurman, P.; Januschowski, K. Functional and Structural Outcome after Vitrectomy Combined with Subretinal Rt-PA Injection with or without Additional Intravitreal Bevacizumab Injection for Submacular Haemorrhages. PLoS ONE 2021, 16, E0250587. [Google Scholar] [CrossRef]
- Sniatecki, J.J.; Ho-Yen, G.; Clarke, B.; Barbara, R.; Lash, S.; Papathomas, T.; Antonakis, S.; Gupta, B. Treatment of Submacular Haemorrhage with Tissue Plasminogen Activator and Pneumatic Displacement in Age-Related Macular Degeneration. Eur. J. Ophthalmol. 2021, 31, 643–648. [Google Scholar] [CrossRef]
- Tranos, P.; Tsiropoulos, G.N.; Koronis, S.; Vakalis, A.; Asteriadis, S.; Stavrakas, P. Comparison of Subretinal versus Intravitreal Injection of Recombinant Tissue Plasminogen Activator with Gas for Submacular Haemorrhage Secondary to Wet Age-Related Macular Degeneration: Treatment Outcomes and Brief Literature Review. Int. Ophthalmol. 2021, 41, 4037–4046. [Google Scholar] [CrossRef]
- Tiosano, A.; Gal-Or, O.; Fradkin, M.; Elul, R.; Dotan, A.; Hadayer, A.; Brody, J.; Ehrlich, R. Visual Acuity Outcome in Patients with Subretinal Haemorrhage—Office Procedure vs. Surgical Treatment. Eur. J. Ophthalmol. 2022, 33, 506–513. [Google Scholar] [CrossRef]
- Confalonieri, F.; Stene-Johansen, I.; Lumi, X.; Petrovski, G. Intravitreal RT-PA Injection and Pneumatic Displacement for Submacular Retinal Haemorrhage: A Case Series. Case Rep. Ophthalmol. 2022, 13, 630–637. [Google Scholar] [CrossRef]
- Ratanasukon, M.; Kittantong, A. Results of Intravitreal Tissue Plasminogen Activator and Expansile Gas Injection for Submacular Haemorrhage in Thais. Eye 2005, 19, 1328–1332. [Google Scholar] [CrossRef]
- Singh, R.P.; Patel, C.; Sears, J.E. Management of Subretinal Macular Haemorrhage by Direct Administration of Tissue Plasminogen Activator. Br. J. Ophthalmol. 2006, 90, 429–431. [Google Scholar] [CrossRef]
- Yang, P.-M.; Kuo, H.-K.; Kao, M.-L.; Chen, Y.-J.; Tsai, H.-H. Pneumatic Displacement of a Dense Submacular Haemorrhage with or without Tissue Plasminogen Activator. Chang. Gung Med. J. 2005, 28, 852–859. [Google Scholar]
- Stifter, E.; Michels, S.; Prager, F.; Georgopoulos, M.; Polak, K.; Hirn, C.; Schmidt-Erfurth, U. Intravitreal Bevacizumab Therapy for Neovascular Age-Related Macular Degeneration with Large Submacular Haemorrhage. Am. J. Ophthalmol. 2007, 144, 886–892.e2. [Google Scholar] [CrossRef]
- Arias, L.; Monés, J. Transconjunctival Sutureless Vitrectomy with Tissue Plasminogen Activator, Gas and Intravitreal Bevacizumab in the Management of Predominantly Hemorrhagic Age-Related Macular Degeneration. Clin. Ophthalmol. 2010, 4, 67–72. [Google Scholar]
- Cakir, M.; Cekiç, O.; Yilmaz, O.F. Pneumatic Displacement of Acute Submacular Haemorrhage with and without the Use of Tissue Plasminogen Activator. Eur. J. Ophthalmol. 2010, 20, 565–571. [Google Scholar] [CrossRef]
- Kung, Y.H.; Wu, T.T.; Hong, M.C.; Sheu, S.J. Intravitreal Tissue Plasminogen Activator and Pneumatic Displacement of Submacular Haemorrhage. J. Ocul. Pharmacol Ther. 2010, 26, 469–474. [Google Scholar] [CrossRef]
- Sandhu, S.S.; Manvikar, S.; Steel, D.H. Displacement of Submacular Haemorrhage Associated with Age-Related Macular Degeneration Using Vitrectomy and Submacular RT-PA Injection Followed by Intravitreal Ranibizumab. Clin. Ophthalmol. 2010, 4, 637–642. [Google Scholar] [CrossRef]
- Treumer, F.; Roider, J.; Hillenkamp, J. Long-Term Outcome of Subretinal Coapplication of Rt-PA and Bevacizumab Followed by Repeated Intravitreal Anti-VEGF Injections for Neovascular AMD with Submacular Haemorrhage. Br. J. Ophthalmol. 2012, 96, 708–713. [Google Scholar] [CrossRef]
- Cho, H.J.; Koh, K.M.; Kim, H.S.; Lee, T.G.; Kim, C.G.; Kim, J.W. Anti-Vascular Endothelial Growth Factor Monotherapy in the Treatment of Submacular Haemorrhage Secondary to Polypoidal Choroidal Vasculopathy. Am. J. Ophthalmol. 2013, 156, 524–531.E1. [Google Scholar] [CrossRef]
- Jain, S.; Kishore, K.; Sharma, Y.R. Intravitreal Anti-VEGF Monotherapy for Thick Submacular Haemorrhage of Less than 1 Week Duration Secondary to Neovascular Age-Related Macular Degeneration. Indian J. Ophthalmol. 2013, 61, 490–496. [Google Scholar] [CrossRef]
- Moisseiev, E.; Ben Ami, T.; Barak, A. Vitrectomy and Subretinal Injection of Tissue Plasminogen Activator for Large Submacular Haemorrhage Secondary to AMD. Eur. J. Ophthalmol. 2014, 24, 925–931. [Google Scholar] [CrossRef]
- Kim, H.S.; Cho, H.J.; Yoo, S.G.; Kim, J.H.; Han, J.I.; Lee, T.G.; Kim, J.W. Intravitreal Anti-Vascular Endothelial Growth Factor Monotherapy for Large Submacular Haemorrhage Secondary to Neovascular Age-Related Macular Degeneration. Eye 2015, 29, 1141–1151. [Google Scholar] [CrossRef]
- Kimura, S.; Morizane, Y.; Hosokawa, M.; Shiode, Y.; Kawata, T.; Doi, S.; Matoba, R.; Hosogi, M.; Fujiwara, A.; Inoue, Y.; et al. Submacular Haemorrhage in Polypoidal Choroidal Vasculopathy Treated by Vitrectomy and Subretinal Tissue Plasminogen Activator. Am. J. Ophthalmol. 2015, 159, 683–689. [Google Scholar] [CrossRef]
- González-López, J.J.; McGowan, G.; Chapman, E.; Yorston, D. Vitrectomy with Subretinal Tissue Plasminogen Activator and Ranibizumab for Submacular Haemorrhages Secondary to Age-Related Macular Degeneration: Retrospective Case Series of 45 Consecutive Cases. Eye 2016, 30, 929–935. [Google Scholar] [CrossRef]
- Lee, J.P.; Park, J.S.; Kwon, O.W.; You, Y.S.; Kim, S.H. Management of Acute Submacular Haemorrhage with Intravitreal Injection of Tenecteplase, Anti-Vascular Endothelial Growth Factor and Gas. Korean J. Ophthalmol. 2016, 30, 192–197. [Google Scholar] [CrossRef]
- Waizel, M.; Todorova, M.G.; Kazerounian, S.; Rickmann, A.; Blanke, B.R.; Szurman, P. Efficacy of Vitrectomy Combined with Subretinal Recombinant Tissue Plasminogen Activator for Subretinal versus Subpigment Epithelial versus Combined Haemorrhages. Ophthalmologica 2016, 236, 123–132. [Google Scholar] [CrossRef]
- Gok, M.; Karabaş, V.L.; Aslan, M.S.; Kara, Ö.; Karaman, S.; Yenihayat, F. Tissue Plasminogen Activator-Assisted Vitrectomy for Submacular Haemorrhage Due to Age-Related Macular Degeneration. Indian J. Ophthalmol. 2017, 65, 482–487. [Google Scholar] [CrossRef]
- Waizel, M.; Todorova, M.G.; Rickmann, A.; Blanke, B.R.; Szurman, P. Efficacy of Vitrectomy Combined with Subretinal Rt-PA Injection with Gas or Air Tamponade. Klin. Monbl. Augenheilkd. 2017, 234, 487–492. (In English) [Google Scholar] [CrossRef]
- Bardak, H.; Bardak, Y.; Erçalık, Y.; Erdem, B.; Arslan, G.; Timlioglu, S. Sequential Tissue Plasminogen Activator, Pneumatic Displacement, and Anti-VEGF Treatment for Submacular Haemorrhage. Eur. J. Ophthalmol. 2018, 28, 306–310. [Google Scholar] [CrossRef]
- Sharma, S.; Kumar, J.B.; Kim, J.E.; Thordsen, J.; Dayani, P.; Ober, M.; Mahmoud, T.H. Pneumatic Displacement of Submacular Haemorrhage with Subretinal Air and Tissue Plasminogen Activator: Initial United States Experience. Ophthalmol. Retina 2018, 2, 180–186. [Google Scholar] [CrossRef]
- Karamitsos, A.; Papastavrou, V.; Ivanova, T.; Cottrell, D.; Stannard, K.; Karachrysafi, S.; Cheristanidis, S.; Ziakas, N.; Papamitsou, T.; Hillier, R. Management of Acute Submacular Haemorrhage Using Intravitreal Injection of Tissue Plasminogen Activator and Gas: A Case Series. SAGE Open Med. Case Rep. 2020, 8, 2050313X20970337. [Google Scholar] [CrossRef]
- Lee, K.; Park, Y.G.; Park, Y.H. Visual prognosis after pneumatic displacement of submacular haemorrhage according to age-related macular degeneration subtypes. Retina 2020, 40, 2304–2311. [Google Scholar] [CrossRef]
- Ali Said, Y.; Dewilde, E.; Stalmans, P. Visual Outcome after Vitrectomy with Subretinal RT-PA Injection to Treat Submacular Haemorrhage Secondary to Age-Related Macular Degeneration or Macroaneurysm. J. Ophthalmol. 2021, 2021, 3160963. [Google Scholar] [CrossRef]
- Avcı, R.; Mavi Yıldız, A.; Çınar, E.; Yılmaz, S.; Küçükerdönmez, C.; Akalp, F.D.; Avcı, E. Subretinal Coapplication of Tissue Plasminogen Activator and Bevacizumab with Concurrent Pneumatic Displacement for Submacular Haemorrhages Secondary to Neovascular Age-Related Macular Degeneration. Turk. J. Ophthalmol. 2021, 51, 38–44. [Google Scholar] [CrossRef]
- Iannetta, D.; De Maria, M.; Bolletta, E.; Mastrofilippo, V.; Moramarco, A.; Fontana, L. Subretinal Injection of Recombinant Tissue Plasminogen Activator and Gas Tamponade to Displace Acute Submacular Haemorrhages Secondary to Age-Related Macular Degeneration. Clin. Ophthalmol. 2021, 15, 3649–3659. [Google Scholar] [CrossRef]
- Kawakami, S.; Wakabayashi, Y.; Umazume, K.; Usui, Y.; Muramatsu, D.; Agawa, T.; Yamamoto, K.; Goto, H. Long-Term Outcome of Eyes with Vitrectomy for Submacular and/or Vitreous Haemorrhage in Neovascular Age-Related Macular Degeneration. J. Ophthalmol. 2021, 2021, 2963822. [Google Scholar] [CrossRef]
- Fukuda, Y.; Nakao, S.; Kohno, R.I.; Ishikawa, K.; Shimokawa, S.; Shiose, S.; Takeda, A.; Morizane, Y.; Sonoda, K.H. Postoperative Follow-up of Submacular Haemorrhage Displacement Treated with Vitrectomy and Subretinal Injection of Tissue Plasminogen Activator: Ultrawide-Field Fundus Autofluorescence Imaging in Gas-Filled Eyes. Jpn. J. Ophthalmol. 2022, 66, 264–270. [Google Scholar] [CrossRef]
- Juncal, V.R.; Hanout, M.; Altomare, F.; Chow, D.R.; Giavedoni, L.R.; Muni, R.H.; Wong, D.T.; Berger, A.R. Surgical Management of Submacular Haemorrhage: Experience at an Academic Canadian Centre. Can. J. Ophthalmol. 2018, 53, 408–414. [Google Scholar] [CrossRef]
- Olivier, S.; Chow, D.R.; Packo, K.H.; MacCumber, M.W.; Awh, C.C. Subretinal Recombinant Tissue Plasminogen Activator Injection and Pneumatic Displacement of Thick Submacular Haemorrhage in Age-Related Macular Degeneration. Ophthalmology 2004, 111, 1201–1208. [Google Scholar] [CrossRef]
- Kadonosono, K.; Arakawa, A.; Yamane, S.; Inoue, M.; Yamakawa, T.; Uchio, E.; Yanagi, Y. Displacement of Submacular Haemorrhages in Age-Related Macular Degeneration with Subretinal Tissue Plasminogen Activator and Air. Ophthalmology 2015, 122, 123–128. [Google Scholar] [CrossRef]
- Kim, J.H.; Chang, Y.S.; Lee, D.W.; Kim, C.G.; Kim, J.W. Quantification of Retinal Changes after Resolution of Submacular Haemorrhage Secondary to Polypoidal Choroidal Vasculopathy. Jpn. J. Ophthalmol. 2018, 62, 54–62. [Google Scholar] [CrossRef]
- Caporossi, T.; Bacherini, D.; Governatori, L.; Oliverio, L.; Di Leo, L.; Tartaro, R.; Rizzo, S. Management of Submacular Massive Haemorrhage in Age-Related Macular Degeneration: Comparison between Subretinal Transplant of Human Amniotic Membrane and Subretinal Injection of Tissue Plasminogen Activator. Acta Ophthalmol. 2022, 100, E1143–E1152. [Google Scholar] [CrossRef]
- Ura, S.; Miyata, M.; Ooto, S.; Yasuhara, S.; Tamura, H.; Ueda-Arakawa, N.; Muraoka, Y.; Miyake, M.; Takahashi, A.; Wakazono, T.; et al. Contrast-to-noise ratio is a useful predictor of early displacement of large submacular haemorrhage by intravitreal sf6 gas injection. Retina 2022, 42, 661–668. [Google Scholar] [CrossRef]
- Thompson, J.T.; Sjaarda, R.N. Vitrectomy for the treatment of submacular haemorrhages from macular degeneration: A comparison of submacular haemorrhage/membrane removal and submacular tissue plasminogen activator–assisted pneumatic displacement. Trans. Am. Ophthalmol. Soc. 2005, 103, 98–107. [Google Scholar]
- Ron, Y.; Ehrlich, R.; Axer-Siegel, R.; Rosenblatt, I.; Weinberger, D. Pneumatic Displacement of Submacular Haemorrhage Due to Age-Related Macular Degeneration. Ophthalmologica 2006, 221, 57–61. [Google Scholar] [CrossRef]
- Meyer, C.H.; Scholl, H.P.; Eter, N.; Helb, H.-M.; Holz, F.G. Combined Treatment of Acute Subretinal Haemorrhages with Intravitreal Recombined Tissue Plasminogen Activator, Expansile Gas and Bevacizumab: A Retrospective Pilot Study. Acta Ophthalmol. 2008, 86, 490–494. [Google Scholar] [CrossRef]
- Fang, I.-M.; Lin, Y.-C.; Yang, C.-H.; Yang, C.-M.; Chen, M.-S. Effects of Intravitreal Gas with or without Tissue Plasminogen Activator on Submacular Haemorrhage in Age-Related Macular Degeneration. Eye 2009, 23, 397–406. [Google Scholar] [CrossRef]
- Fine, H.F.; Iranmanesh, R.; Del Priore, L.V.; Barile, G.R.; Chang, L.K.; Chang, S.; Schiff, W.M. Surgical Outcomes after Massive Subretinal Haemorrhage Secondary to Age-Related Macular Degeneration. Retina 2010, 30, 1588–1594. [Google Scholar] [CrossRef]
- Mizutani, T.; Yasukawa, T.; Ito, Y.; Takase, A.; Hirano, Y.; Yoshida, M.; Ogura, Y. Pneumatic Displacement of Submacular Haemorrhage with or without Tissue Plasminogen Activator. Graefes Arch. Clin. Exp. Ophthalmol. 2011, 249, 1153–1157. [Google Scholar] [CrossRef]
- Han, L.; Ma, Z.; Wang, C.; Dou, H.; Hu, Y.; Feng, X.; Xu, Y.; Yin, Z.; Wang, X. Autologous Transplantation of Simple Retinal Pigment Epithelium Sheet for Massive Submacular Haemorrhage Associated with Pigment Epithelium Detachment. Investig. Ophthalmol. Vis. Sci. 2013, 54, 4956–4963. [Google Scholar] [CrossRef]
- Shienbaum, G.; Garcia Filho, C.A.; Flynn, H.W., Jr.; Nunes, F.; Smiddy, W.E.; Rosenfeld, P.J. Management of Submacular Haemorrhage Secondary to Neovascular Age-Related Macular Degeneration with Anti-Vascular Endothelial Growth Factor Monotherapy. Am. J. Ophthalmol. 2013, 155, 1009–1013. [Google Scholar] [CrossRef]
- Chang, W.; Garg, S.J.; Maturi, R.; Hsu, J.; Sivalingam, A.; Gupta, S.A.; Regillo, C.D.; Ho, A.C. Management of Thick Submacular Haemorrhage with Subretinal Tissue Plasminogen Activator and Pneumatic Displacement for Age-Related Macular Degeneration. Am. J. Ophthalmol. 2014, 157, 1250–1257. [Google Scholar] [CrossRef]
- Kimura, M.; Yasukawa, T.; Shibata, Y.; Kato, A.; Hirano, Y.; Uemura, A.; Yoshida, M.; Ogura, Y. Flattening of Retinal Pigment Epithelial Detachments after Pneumatic Displacement of Submacular Haemorrhages Secondary to Age-Related Macular Degeneration. Graefes Arch. Clin. Exp. Ophthalmol. 2018, 256, 1823–1829. [Google Scholar] [CrossRef]
- Plemel, D.J.A.; Lapere, S.R.J.; Rudnisky, C.J.; Tennant, M.T.S. Vitrectomy with subretinal tissue plasminogen activator and gas tamponade for subfoveal haemorrhage: Prognostic Factors and Clinical Outcomes. Retina 2019, 39, 172–179. [Google Scholar] [CrossRef]
- Helaiwa, K.; Paez, L.R.; Szurman, P.; Januschowski, K. Combined Administration of Preoperative Intravitreal and Intraoperative Subretinal Recombinant Tissue Plasminogen Activator in Acute Hemorrhagic Age-Related Macular Degeneration. Cureus 2020, 12, E7229. [Google Scholar] [CrossRef]
- Wilkins, C.S.; Mehta, N.; Wu, C.Y.; Barash, A.; Deobhakta, A.A.; Rosen, R.B. Outcomes of Pars Plana Vitrectomy with Subretinal Tissue Plasminogen Activator Injection and Pneumatic Displacement of Fovea-Involving Submacular Haemorrhage. BMJ Open Ophthalmol. 2020, 5, E000394. [Google Scholar] [CrossRef]
- Ueda-Arakawa, N.; Tsujikawa, A.; Yamashiro, K.; Ooto, S.; Tamura, H.; Yoshimura, N. Visual Prognosis of Eyes with Submacular Haemorrhage Associated with Exudative Age-Related Macular Degeneration. Jpn. J. Ophthalmol. 2012, 56, 589–598. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, C.G.; Lee, D.W.; Yoo, S.J.; Lew, Y.J.; Cho, H.J.; Kim, J.Y.; Lee, S.H.; Kim, J.W. Intravitreal Aflibercept for Submacular Haemorrhage Secondary to Neovascular Age-Related Macular Degeneration and Polypoidal Choroidal Vasculopathy. Graefes Arch. Clin. Exp. Ophthalmol. 2020, 258, 107–116. [Google Scholar] [CrossRef]
- Bae, K.; Cho, G.E.; Yoon, J.M.; Kang, S.W. Optical Coherence Tomographic Features and Prognosis of Pneumatic Displacement for Submacular Haemorrhage. PLoS ONE 2016, 11, E0168474. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).