The Role of Different Feedback Devices in the Survival of Patients in Cardiac Arrest: Systematic Review with Meta-Analysis
Abstract
1. Introduction
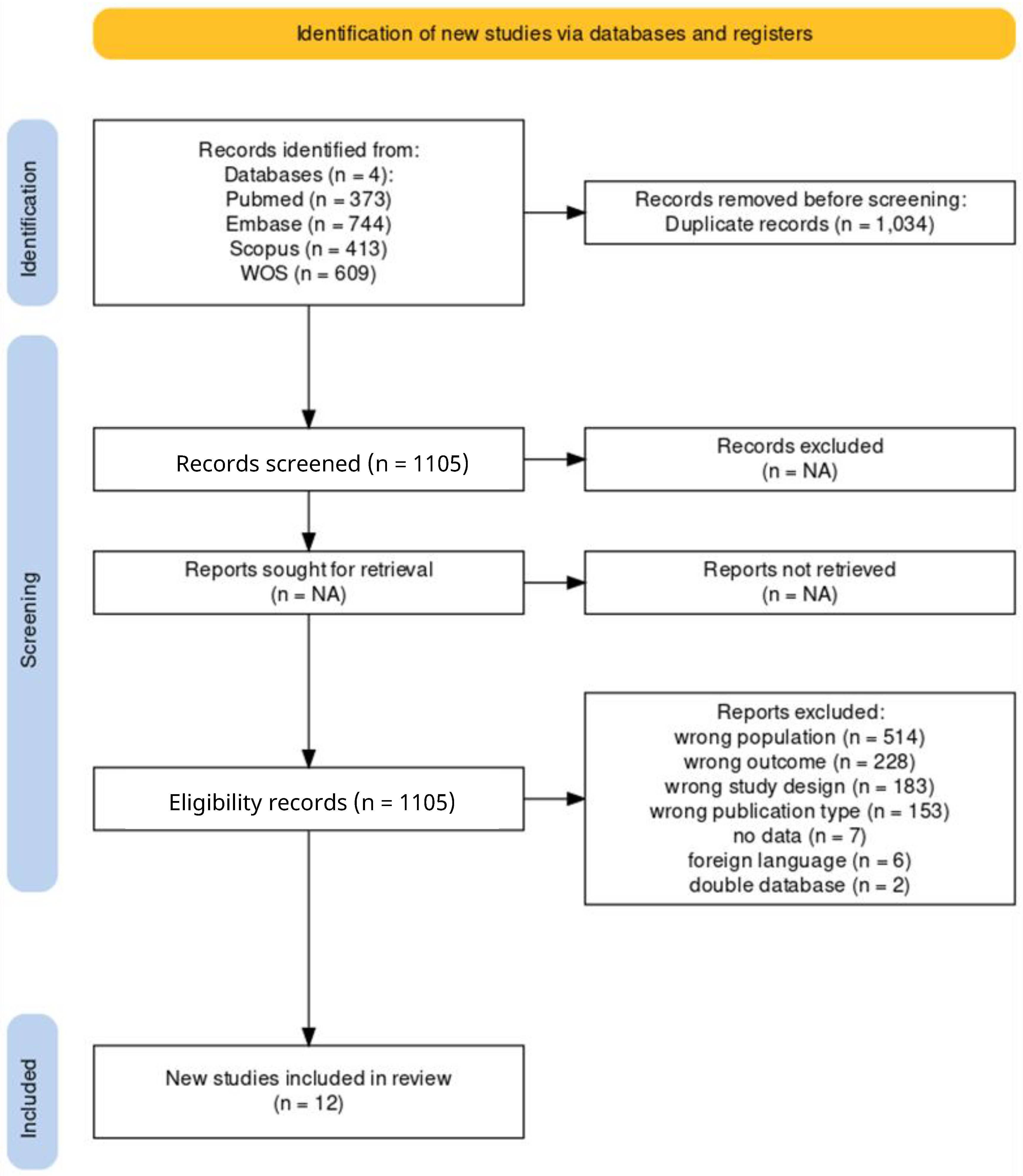
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search String
2.3. Selection of Studies
2.4. Effect Measurement
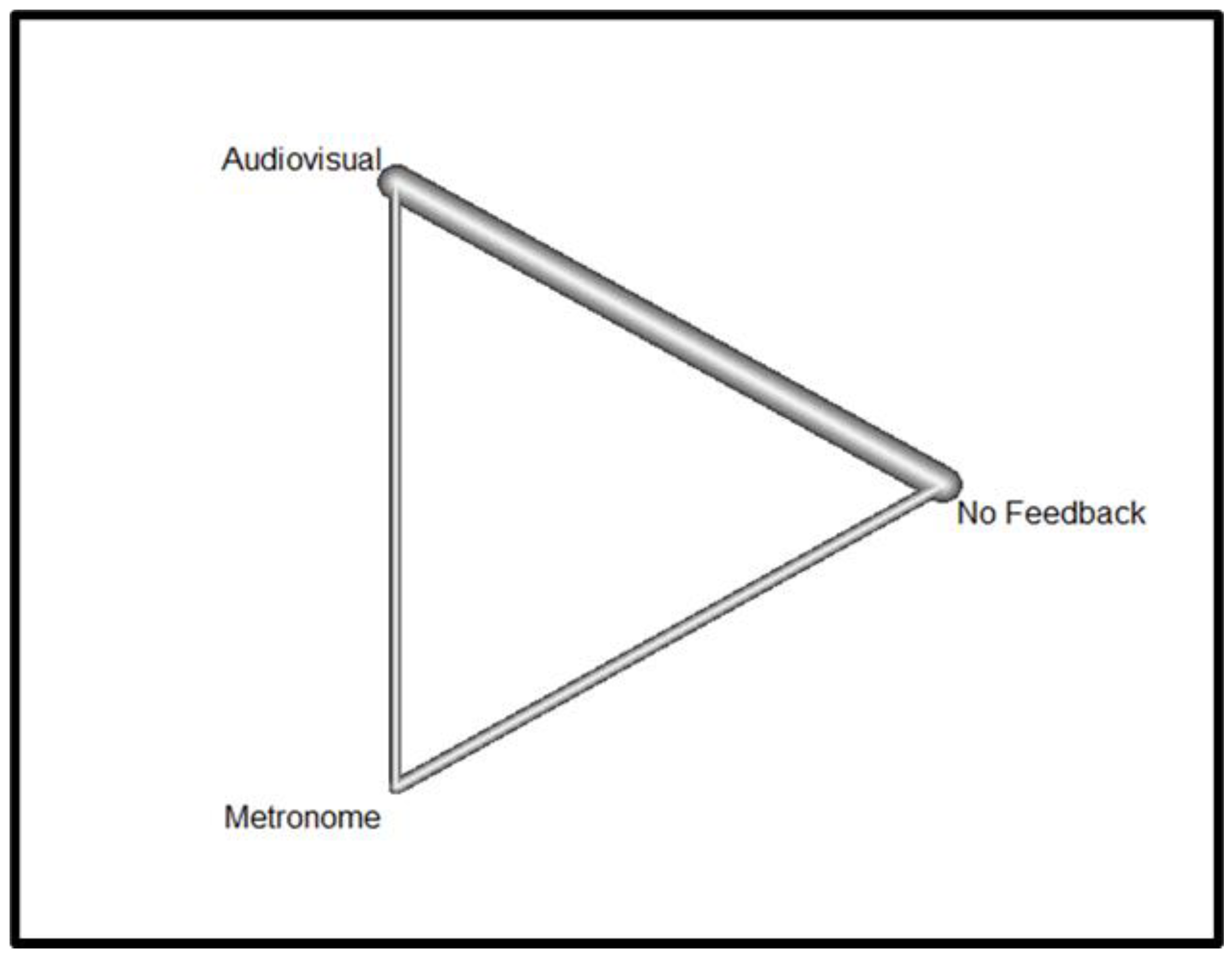
2.5. Synthesis Method
3. Results
3.1. ROSC
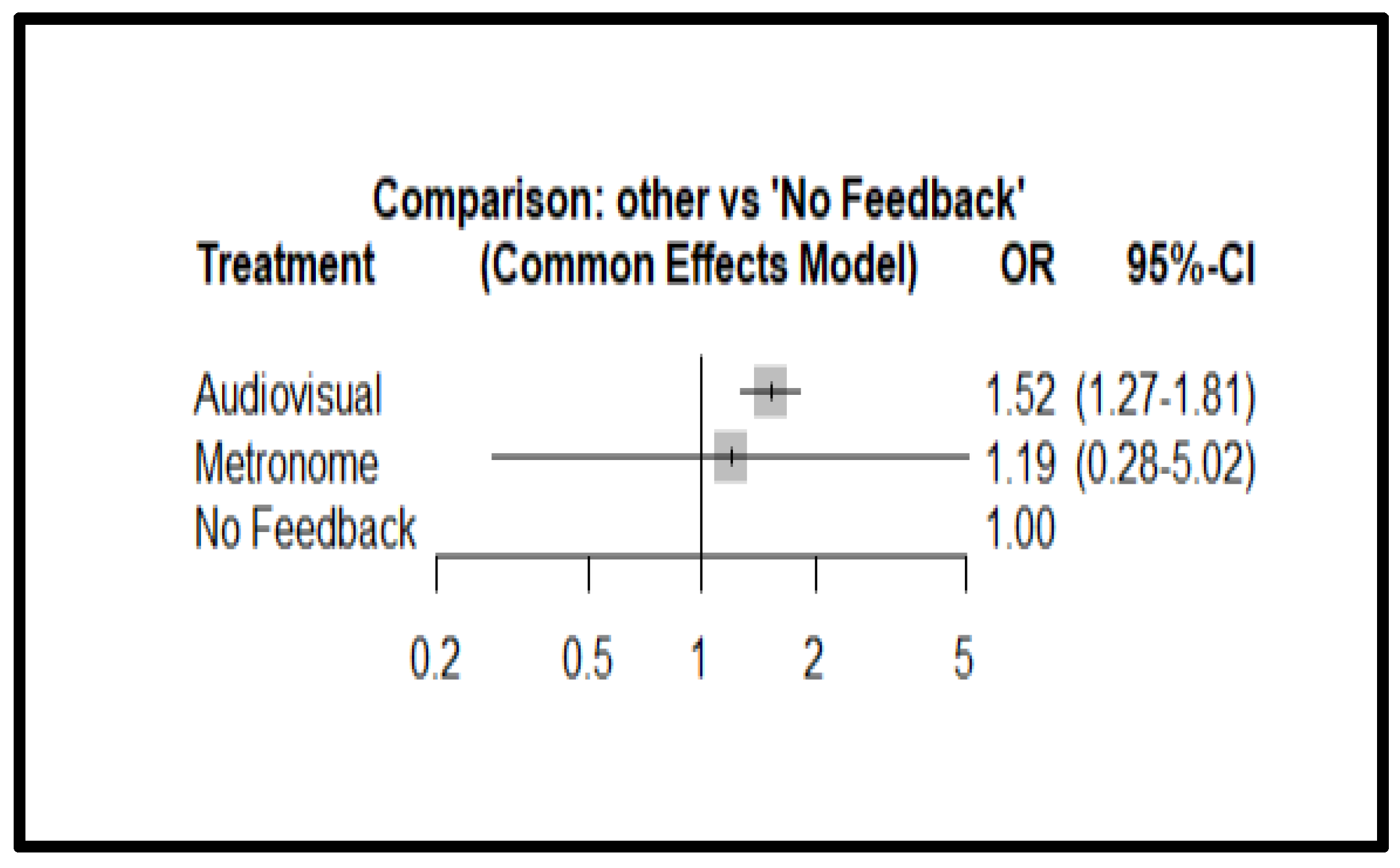
3.2. Survival
3.3. Good Neurological Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stirparo, G.; Andreassi, A.; Sechi, G.M.; Signorelli, C. Spring, It’s Time to ROSC. J. Prev. Med. Hyg. 2023, 64, E87–E91. [Google Scholar] [CrossRef] [PubMed]
- Bellini, L.; Fagoni, N.; Andreassi, A.; Sechi, G.M.; Bonora, R.; Stirparo, G. Effectiveness of Cardiopulmonary Resuscitation at the Workplace. Med. Lav. Work Environ. Health 2023, 114, e2023010. [Google Scholar] [CrossRef]
- Gräsner, J.-T.; Lefering, R.; Koster, R.W.; Masterson, S.; Böttiger, B.W.; Herlitz, J.; Wnent, J.; Tjelmeland, I.B.M.; Ortiz, F.R.; Maurer, H.; et al. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: A Prospective One Month Analysis of out-of-Hospital Cardiac Arrest Outcomes in 27 Countries in Europe. Resuscitation 2016, 105, 188–195. [Google Scholar] [CrossRef]
- Gräsner, J.-T.; Wnent, J.; Herlitz, J.; Perkins, G.D.; Lefering, R.; Tjelmeland, I.; Koster, R.W.; Masterson, S.; Rossell-Ortiz, F.; Maurer, H.; et al. Survival after Out-of-Hospital Cardiac Arrest in Europe—Results of the EuReCa TWO Study. Resuscitation 2020, 148, 218–226. [Google Scholar] [CrossRef]
- Andersen, L.W.; Holmberg, M.J.; Berg, K.M.; Donnino, M.W.; Granfeldt, A. In-Hospital Cardiac Arrest: A Review. JAMA 2019, 321, 1200–1210. [Google Scholar] [CrossRef] [PubMed]
- Barros, A.J.; Enfield, K.B. In-Hospital Cardiac Arrest. Emerg. Med. Clin. N. Am. 2023, 41, 455–464. [Google Scholar] [CrossRef]
- Honarmand, K.; Mepham, C.; Ainsworth, C.; Khalid, Z. Adherence to Advanced Cardiovascular Life Support (ACLS) Guidelines during in-Hospital Cardiac Arrest Is Associated with Improved Outcomes. Resuscitation 2018, 129, 76–81. [Google Scholar] [CrossRef]
- McEvoy, M.D.; Field, L.C.; Moore, H.E.; Smalley, J.C.; Nietert, P.J.; Scarbrough, S.H. The Effect of Adherence to ACLS Protocols on Survival of Event in the Setting of In-Hospital Cardiac Arrest. Resuscitation 2014, 85, 82–87. [Google Scholar] [CrossRef]
- Grunau, B.; Kawano, T.; Scheuermeyer, F.; Tallon, J.; Reynolds, J.; Besserer, F.; Barbic, D.; Brooks, S.; Christenson, J. Early Advanced Life Support Attendance Is Associated with Improved Survival and Neurologic Outcomes after Non-Traumatic out-of-Hospital Cardiac Arrest in a Tiered Prehospital Response System. Resuscitation 2019, 135, 137–144. [Google Scholar] [CrossRef]
- Nehme, Z.; Andrew, E.; Bernard, S.; Smith, K. Impact of Cardiopulmonary Resuscitation Duration on Survival from Paramedic Witnessed Out-of-Hospital Cardiac Arrests: An Observational Study. Resuscitation 2016, 100, 25–31. [Google Scholar] [CrossRef]
- Larribau, R.; Deham, H.; Niquille, M.; Sarasin, F.P. Improvement of Out-of-Hospital Cardiac Arrest Survival Rate after Implementation of the 2010 Resuscitation Guidelines. PLoS ONE 2018, 13, e0204169. [Google Scholar] [CrossRef] [PubMed]
- Berg, K.M.; Bray, J.E.; Ng, K.-C.; Liley, H.G.; Greif, R.; Carlson, J.N.; Morley, P.T.; Drennan, I.R.; Smyth, M.; Scholefield, B.R.; et al. 2023 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Resuscitation 2024, 195, 109992. [Google Scholar] [CrossRef] [PubMed]
- Kurz, M.C.; Schmicker, R.H.; Leroux, B.; Nichol, G.; Aufderheide, T.P.; Cheskes, S.; Grunau, B.; Jasti, J.; Kudenchuk, P.; Vilke, G.M.; et al. Advanced vs. Basic Life Support in the Treatment of Out-of-Hospital Cardiopulmonary Arrest in the Resuscitation Outcomes Consortium. Resuscitation 2018, 128, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Picard, C.; Yang, B.G.; Norris, C.; McIntosh, S.; Douma, M.J. Cardiopulmonary Resuscitation Feedback: A Comparison of Device-Measured and Self-Assessed Chest Compression Quality. J. Emerg. Nurs. 2021, 47, 333–341.e1. [Google Scholar] [CrossRef] [PubMed]
- Hostler, D.; Everson-Stewart, S.; Rea, T.D.; Stiell, I.G.; Callaway, C.W.; Kudenchuk, P.J.; Sears, G.K.; Emerson, S.S.; Nichol, G. Resuscitation Outcomes Consortium Investigators Effect of Real-Time Feedback during Cardiopulmonary Resuscitation Outside Hospital: Prospective, Cluster-Randomised Trial. BMJ 2011, 342, d512. [Google Scholar] [CrossRef] [PubMed]
- Lakomek, F.; Lukas, R.-P.; Brinkrolf, P.; Mennewisch, A.; Steinsiek, N.; Gutendorf, P.; Sudowe, H.; Heller, M.; Kwiecien, R.; Zarbock, A.; et al. Real-Time Feedback Improves Chest Compression Quality in out-of-Hospital Cardiac Arrest: A Prospective Cohort Study. PLoS ONE 2020, 15, e0229431. [Google Scholar] [CrossRef]
- Martin, P.; Theobald, P.; Kemp, A.; Maguire, S.; Maconochie, I.; Jones, M. Real-Time Feedback Can Improve Infant Manikin Cardiopulmonary Resuscitation by up to 79%—A Randomised Controlled Trial. Resuscitation 2013, 84, 1125–1130. [Google Scholar] [CrossRef]
- Kiyohara, K.; Kitamura, Y.; Ayusawa, M.; Nitta, M.; Iwami, T.; Nakata, K.; Sobue, T.; Kitamura, T. Dissemination of Chest Compression-Only Cardiopulmonary Resuscitation by Bystanders for Out-of-Hospital Cardiac Arrest in Students: A Nationwide Investigation in Japan. J. Clin. Med. 2022, 11, 928. [Google Scholar] [CrossRef]
- Nassar, B.S.; Kerber, R. Improving CPR Performance. Chest 2017, 152, 1061–1069. [Google Scholar] [CrossRef]
- Leo, W.Z.; Chua, D.; Tan, H.C.; Ho, V.K. Chest Compression Quality and Patient Outcomes with the Use of a CPR Feedback Device: A Retrospective Study. Sci. Rep. 2023, 13, 19852. [Google Scholar] [CrossRef]
- Stirparo, G.; Di Fronzo, P.; Solla, D.; Bottignole, D.; Gambolò, L. Are Italian Newly Licensed Nurses Ready? A Study on Self-Perceived Clinical Autonomy in Critical Care Scenarios. Healthcare 2024, 12, 809. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Vahedian-Azimi, A.; Hajiesmaeili, M.; Amirsavadkouhi, A.; Jamaati, H.; Izadi, M.; Madani, S.J.; Hashemian, S.M.R.; Miller, A.C. Effect of the Cardio First AngelTM Device on CPR Indices: A Randomized Controlled Clinical Trial. Crit. Care 2016, 20, 147. [Google Scholar] [CrossRef] [PubMed]
- Couper, K.; Kimani, P.K.; Abella, B.S.; Chilwan, M.; Cooke, M.W.; Davies, R.P.; Field, R.A.; Gao, F.; Quinton, S.; Stallard, N.; et al. The System-Wide Effect of Real-Time Audiovisual Feedback and Postevent Debriefing for In-Hospital Cardiac Arrest: The Cardiopulmonary Resuscitation Quality Improvement Initiative. Crit. Care Med. 2015, 43, 2321–2331. [Google Scholar] [CrossRef]
- Kramer-Johansen, J.; Myklebust, H.; Wik, L.; Fellows, B.; Svensson, L.; Sørebø, H.; Steen, P.A. Quality of Out-of-Hospital Cardiopulmonary Resuscitation with Real Time Automated Feedback: A Prospective Interventional Study. Resuscitation 2006, 71, 283–292. [Google Scholar] [CrossRef]
- Goharani, R.; Vahedian-Azimi, A.; Pourhoseingholi, M.A.; Amanpour, F.; Rosano, G.M.C.; Sahebkar, A. Survival to Intensive Care Unit Discharge among In-hospital Cardiac Arrest Patients by Applying Audiovisual Feedback Device. ESC Heart Fail. 2021, 8, 4652–4660. [Google Scholar] [CrossRef]
- Obling, L.; Hassager, C.; Blomberg, S.N.; Folke, F. Inverse Association Between Bystander Use of Audiovisual Feedback From an Automated External Defibrillator and Return of Spontaneous Circulation. J. Am. Heart Assoc. 2022, 11, e023232. [Google Scholar] [CrossRef] [PubMed]
- Lukas, R.-P.; Gräsner, J.T.; Seewald, S.; Lefering, R.; Weber, T.P.; Van Aken, H.; Fischer, M.; Bohn, A. Chest Compression Quality Management and Return of Spontaneous Circulation: A Matched-Pair Registry Study. Resuscitation 2012, 83, 1212–1218. [Google Scholar] [CrossRef]
- Abella, B.S.; Edelson, D.P.; Kim, S.; Retzer, E.; Myklebust, H.; Barry, A.M.; O’Hearn, N.; Hoek, T.L.V.; Becker, L.B. CPR Quality Improvement during In-Hospital Cardiac Arrest Using a Real-Time Audiovisual Feedback System. Resuscitation 2007, 73, 54–61. [Google Scholar] [CrossRef]
- de Oliveira Botelho, R.M.; Campanharo, C.R.V.; Lopes, M.C.B.T.; Okuno, M.F.P.; de Góis, A.F.T.; Batista, R.E.A. The Use of a Metronome during Cardiopulmonary Resuscitation in the Emergency Room of a University Hospital. Rev. Lat. Am. Enferm. 2016, 24, e2829. [Google Scholar] [CrossRef][Green Version]
- Leis, C.C.; González, V.A.; Hernández, R.D.E.; Sánchez, Ó.E.; Martín, J.L.M.; Hermosa, E.J.M.; Torres, E.C. Feedback on Chest Compression Quality Variables and Their Relationship to Rate of Return of Spontaneous Circulation. Emergencias 2013, 25, 99–104. [Google Scholar]
- Agerskov, M.; Hansen, M.B.; Nielsen, A.M.; Møller, T.P.; Wissenberg, M.; Rasmussen, L.S. Return of Spontaneous Circulation and Long-Term Survival According to Feedback Provided by Automated External Defibrillators. Acta Anaesthesiol. Scand. 2017, 61, 1345–1353. [Google Scholar] [CrossRef] [PubMed]
- Idris, A.H.; Guffey, D.; Pepe, P.E.; Brown, S.P.; Brooks, S.C.; Callaway, C.W.; Christenson, J.; Davis, D.P.; Daya, M.R.; Gray, R.; et al. Chest Compression Rates and Survival Following Out-of-Hospital Cardiac Arrest. Crit. Care Med. 2015, 43, 840–848. [Google Scholar] [CrossRef]
- Oermann, M.H.; Kardong-Edgren, S.E.; Odom-Maryon, T. Competence in CPR. AJN Am. J. Nurs. 2012, 112, 43–46. [Google Scholar] [CrossRef]
- Stirparo, G.; Bellini, L.; Solla, D.; Stirparo, P.; Fagoni, N.; Gambolò, L. Should Basic Life Support–Defibrillator Training Be Compulsory for Newly Licensed Italian Physicians? An Observational Study. J. Cardiovasc. Med. 2024, 25, 632–636. [Google Scholar] [CrossRef]
- Gugelmin-Almeida, D.; Tobase, L.; Polastri, T.F.; Peres, H.H.C.; Timerman, S. Do Automated Real-Time Feedback Devices Improve CPR Quality? A Systematic Review of Literature. Resusc. Plus 2021, 6, 100108. [Google Scholar] [CrossRef]


| Author | Year | Sample | Outcome | Feedback Type |
|---|---|---|---|---|
| Vahedian-Azimi et al. [25] | 2016 | 80 | -ROSC | Audiovisual |
| Couper et al. [26] | 2015 | 634 | -ROSC -SURVIVAL -NEUROLOGICAL OUTCOME | Audiovisual |
| Kramer-Johansen et al. [27] | 2006 | 358 | -ROSC -SURVIVAL | Audiovisual |
| Goharani et al. [28] | 2019 | 900 | -ROSC -SURVIVAL | Audiovisual |
| Obling et al. [29] | 2022 | 325 | -ROSC -SURVIVAL | Audiovisual, Metronome |
| Hostler et al. [15] | 2011 | 1586 | -ROSC -SURVIVAL -NEUROLOGICAL OUTCOME | Audiovisual |
| Lukas et al. [30] | 2012 | 638 | -ROSC | Audiovisual |
| Abella et al. [31] | 2007 | 156 | -ROSC -SURVIVAL | Audiovisual |
| Botelho et al. [32] | 2016 | 111 | -ROSC -SURVIVAL | Metronome |
| Camacho Leis et al. [33] | 2012 | 892 | -ROSC | Audiovisual |
| Lakomek et al. [16] | 2020 | 292 | -ROSC | Audiovisual |
| Agerskov et al. [34] | 2017 | 196 | -ROSC -SURVIVAL | Audiovisual |
| Study | Outcome | Feedback | Event | Total |
|---|---|---|---|---|
| Couper et al., 2015 [26] | GOOD NEUROLOGICAL OUTCOME | Audiovisual | 82 | 513 |
| Couper et al., 2015 [26] | GOOD NEUROLOGICAL OUTCOME | No Feedback | 17 | 121 |
| Hostler et al., 2011 [15] | GOOD NEUROLOGICAL OUTCOME | Audiovisual | 35 | 815 |
| Hostler et al., 2011 [15] | GOOD NEUROLOGICAL OUTCOME | No Feedback | 29 | 771 |
| Couper et al., 2015 [26] | SURVIVAL | No Feedback | 21 | 121 |
| Couper et al., 2015 [26] | SURVIVAL | Audiovisual | 90 | 513 |
| Kramer-Johansen et al., 2006 [27] | SURVIVAL | No Feedback | 7 | 241 |
| Kramer-Johansen et al., 2006 [27] | SURVIVAL | Audiovisual | 5 | 117 |
| Goharani et al., 2019 [28] | SURVIVAL | No Feedback | 128 | 450 |
| Goharani et al., 2019 [28] | SURVIVAL | Audiovisual | 243 | 450 |
| Hostler et al., 2011 [15] | SURVIVAL | No Feedback | 96 | 771 |
| Hostler et al., 2011 [15] | SURVIVAL | Audiovisual | 92 | 815 |
| Abella et al., 2007 [31] | SURVIVAL | No Feedback | 5 | 55 |
| Abella et al., 2007 [31] | SURVIVAL | Audiovisual | 9 | 101 |
| Botelho et al., 2016 [32] | SURVIVAL | No Feedback | 4 | 60 |
| Botelho et al., 2016 [32] | SURVIVAL | Metronome | 4 | 51 |
| Agerskov et al., 2017 [34] | SURVIVAL | No Feedback | 53 | 134 |
| Agerskov et al., 2017 [34] | SURVIVAL | Audiovisual | 24 | 62 |
| Vahedian-Azimi et al., 2016 [25] | ROSC | Audiovisual | 29 | 40 |
| Vahedian-Azimi et al., 2016 [25] | ROSC | No Feedback | 14 | 40 |
| Couper et al., 2015 [26] | ROSC | Audiovisual | 262 | 513 |
| Couper et al., 2015 [26] | ROSC | No Feedback | 61 | 121 |
| Kramer-Johansen et al., 2006 [27] | ROSC | Audiovisual | 27 | 117 |
| Kramer-Johansen et al., 2006 [27] | ROSC | No Feedback | 42 | 241 |
| Goharani et al., 2019 [28] | ROSC | Audiovisual | 300 | 450 |
| Goharani et al., 2019 [28] | ROSC | No Feedback | 191 | 450 |
| Obling et al., 2022 [29] | ROSC | Audiovisual | 51 | 155 |
| Obling et al., 2022 [29] | ROSC | Metronome | 38 | 77 |
| Obling et al., 2022 [29] | ROSC | No Feedback | 38 | 93 |
| Hostler et al., 2011 [15] | ROSC | Audiovisual | 361 | 815 |
| Hostler et al., 2011 [15] | ROSC | No Feedback | 345 | 771 |
| Lukas et al., 2012 [30] | ROSC | Audiovisual | 165 | 319 |
| Lukas et al., 2012 [30] | ROSC | No Feedback | 151 | 319 |
| Abella et al., 2007 [31] | ROSC | Audiovisual | 45 | 101 |
| Abella et al., 2007 [31] | ROSC | No Feedback | 22 | 55 |
| Botelho et al., 2016 [32] | ROSC | Metronome | 28 | 51 |
| Botelho et al., 2016 [32] | ROSC | No Feedback | 36 | 60 |
| Camacho Leis et al., 2012 [33] | ROSC | Audiovisual | 50 | 104 |
| Camacho Leis et al., 2012 [33] | ROSC | No Feedback | 319 | 788 |
| Lakomek et al., 2020 [16] | ROSC | Audiovisual | 37 | 103 |
| Lakomek et al., 2020 [16] | ROSC | No Feedback | 69 | 189 |
| Agerskov et al., 2017 [34] | ROSC | Audiovisual | 34 | 62 |
| Agerskov et al., 2017 [34] | ROSC | No Feedback | 72 | 134 |
| Study | Treatment 1 | Treatment 2 | OR | 95% CI | Leverage |
|---|---|---|---|---|---|
| Vahedian-Azimi et al., 2016 [25] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.01 |
| Couper et al., 2015 [26] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.08 |
| Kramer-Johansen et al., 2006 [27] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.04 |
| Goharani et al., 2019 [28] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.17 |
| Obling et al., 2022 [29] | Audiovisual | Metronome | 0.84 | [0.55–1.30] | 0.00 |
| Obling et al., 2022 [29] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.00 |
| Obling et al., 2022 [29] | Metronome | No feedback | 1.50 | [0.98–2.30] | 0.00 |
| Hostler et al., 2011 [15] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.32 |
| Lukas et al., 2012 [30] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.13 |
| Abella et al., 2007 [31] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.03 |
| Botelho et al., 2016 [32] | Metronome | No feedback | 1.50 | [0.98–2.30] | 0.32 |
| Camacho Leis et al., 2012 [33] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.08 |
| Lakomek et al., 2020 [16] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.05 |
| Agerskov et al., 2017 [34] | Audiovisual | No feedback | 1.26 | [1.13–1.41] | 0.03 |
| Study | Treatment 1 | Treatment 2 | OR | 95% CI | Leverage |
|---|---|---|---|---|---|
| Couper et al., 2015 [26] | Audiovisual | No feedback | 1.52 | [1.27–1.81] | 0.12 |
| Kramer-Johansen et al., 2006 [27] | Audiovisual | No feedback | 1.52 | [1.27–1.81] | 0.02 |
| Goharani et al., 2019 [28] | Audiovisual | No feedback | 1.52 | [1.27–1.81] | 0.41 |
| Hostler et al., 2011 [15] | Audiovisual | No feedback | 1.52 | [1.27–1.81] | 0.34 |
| Abella et al., 2007 [31] | Audiovisual | No feedback | 1.52 | [1.27–1.81] | 0.02 |
| Botelho et al., 2016 [32] | Metronome | No feedback | 1.19 | [0.28–5.02] | 1.00 |
| Agerskov et al., 2017 [34] | Audiovisual | No feedback | 1.52 | [1.27–1.81] | 0.08 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gambolò, L.; Di Fronzo, P.; Ristagno, G.; Biserni, S.; Milazzo, M.; Socaci, D.M.; Sarli, L.; Artioli, G.; Bonacaro, A.; Stirparo, G. The Role of Different Feedback Devices in the Survival of Patients in Cardiac Arrest: Systematic Review with Meta-Analysis. J. Clin. Med. 2024, 13, 5989. https://doi.org/10.3390/jcm13195989
Gambolò L, Di Fronzo P, Ristagno G, Biserni S, Milazzo M, Socaci DM, Sarli L, Artioli G, Bonacaro A, Stirparo G. The Role of Different Feedback Devices in the Survival of Patients in Cardiac Arrest: Systematic Review with Meta-Analysis. Journal of Clinical Medicine. 2024; 13(19):5989. https://doi.org/10.3390/jcm13195989
Chicago/Turabian StyleGambolò, Luca, Pasquale Di Fronzo, Giuseppe Ristagno, Sofia Biserni, Martina Milazzo, Delia Marta Socaci, Leopoldo Sarli, Giovanna Artioli, Antonio Bonacaro, and Giuseppe Stirparo. 2024. "The Role of Different Feedback Devices in the Survival of Patients in Cardiac Arrest: Systematic Review with Meta-Analysis" Journal of Clinical Medicine 13, no. 19: 5989. https://doi.org/10.3390/jcm13195989
APA StyleGambolò, L., Di Fronzo, P., Ristagno, G., Biserni, S., Milazzo, M., Socaci, D. M., Sarli, L., Artioli, G., Bonacaro, A., & Stirparo, G. (2024). The Role of Different Feedback Devices in the Survival of Patients in Cardiac Arrest: Systematic Review with Meta-Analysis. Journal of Clinical Medicine, 13(19), 5989. https://doi.org/10.3390/jcm13195989









