Comparative Analysis of Heart Rate Variability and Arterial Stiffness in Elite Male Athletes after COVID-19
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Anthropometric Measurements
2.4. Body Composition Analysis
2.5. Pulmonary Function
2.6. Autonomic Regulation
2.7. Arterial Stiffness and Vascular Compliance
2.8. Hemodynamic Monitoring
2.9. Microcirculation and Oxygenation
2.10. Ethical Considerations
2.11. Data Analysis
3. Results
3.1. Anthropometric Measurements
3.2. Pulmonary Function
3.3. Autonomic Regulation
3.4. Arterial Stiffness
3.5. Blood Pressure
3.6. Oxygen Saturation
4. Discussion
4.1. Anthropometric Data and Body Composition
4.2. Spirometric Data
4.3. Autonomic Regulation
4.4. Arterial Stiffness and Vascular Compliance
4.5. Hemodynamics
4.6. Microcirculation and Oxygenation
4.7. Study Limitations
4.8. Recommendations for Future Research
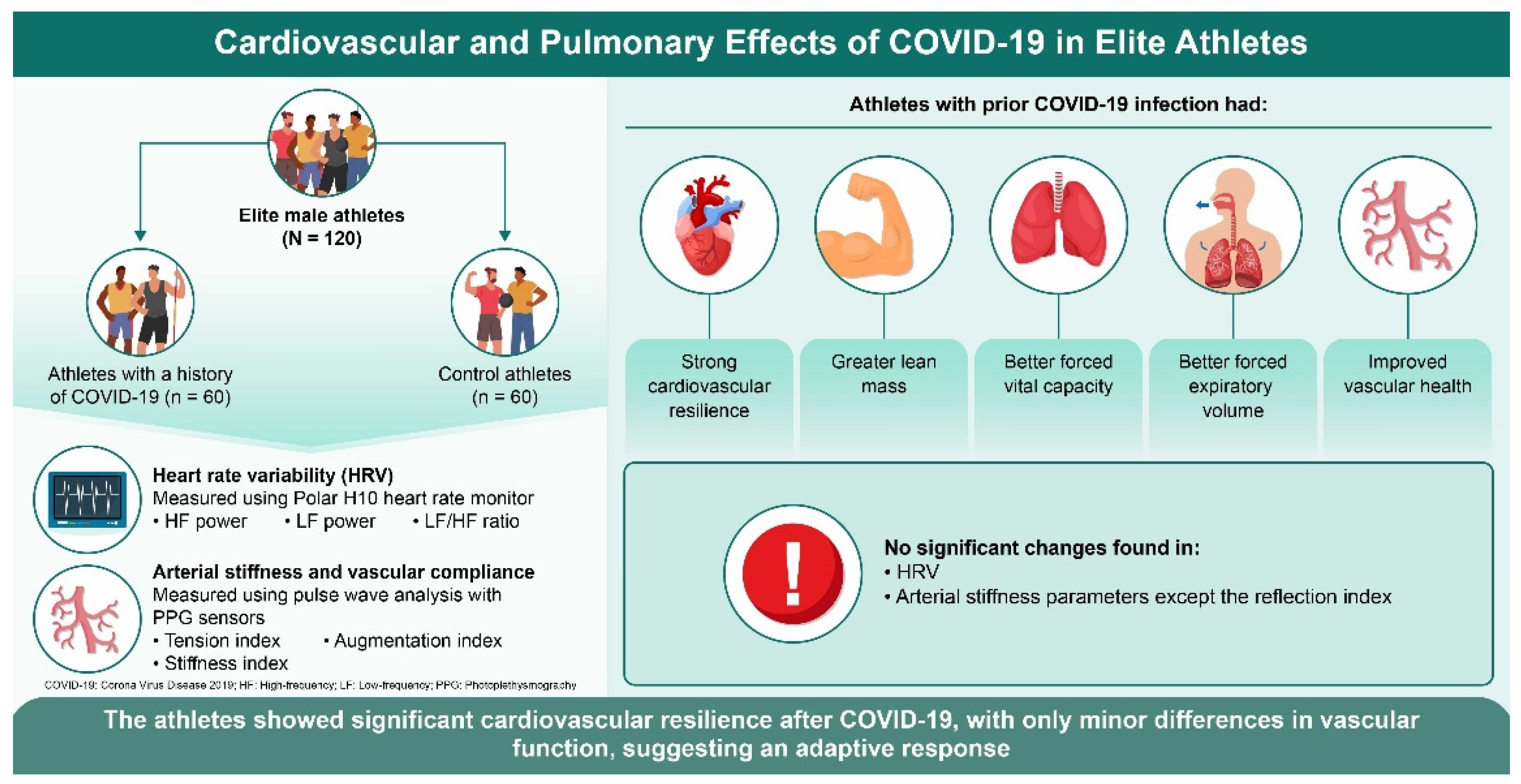
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nishiga, M.; Wang, D.W.; Han, Y.; Lewis, D.B.; Wu, J.C. COVID-19 and cardiovascular disease: From basic mechanisms to clinical perspectives. Nat. Rev. Cardiol. 2020, 17, 543–558. [Google Scholar] [CrossRef] [PubMed]
- Fikenzer, S.; Fikenzer, K.; Laufs, U.; Falz, R.; Pietrek, H.; Hepp, P. Impact of COVID-19 lockdown on endurance capacity of elite handball players. J. Sports Med. Phys. Fitness 2021, 61, 977–982. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Madhavan, M.V.; Sehgal, K.; Nair, N.; Mahajan, S.; Sehrawat, T.S.; Bikdeli, B.; Ahluwalia, N.; Ausiello, J.C.; Wan, E.Y.; et al. Extrapulmonary manifestations of COVID-19. Nat. Med. 2020, 26, 1017–1032. [Google Scholar] [CrossRef] [PubMed]
- Bansal, M. Cardiovascular disease and COVID-19. Diabetes Metab. Syndr. 2020, 14, 247–250. [Google Scholar] [CrossRef] [PubMed]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Bellenger, C.R.; Fuller, J.T.; Thomson, R.L.; Davison, K.; Robertson, E.Y.; Buckley, J.D. Monitoring Athletic Training Status Through Autonomic Heart Rate Regulation: A Systematic Review and Meta-Analysis. Sports Med. 2016, 46, 1461–1486. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J.P. An overview of heart rate variability metrics and norms. Front. Public Health 2017, 5, 290215. [Google Scholar] [CrossRef]
- Asarcikli, L.D.; Hayiroglu, M.I.; Osken, A.; Keskin, K.; Kolak, Z.; Aksu, T. Heart rate variability and cardiac autonomic functions in post-COVID period. J. Interv. Card. Electrophysiol. 2022, 63, 715–721. [Google Scholar] [CrossRef]
- Marques, K.C.; Quaresma, J.A.S.; Falcão, L.F.M. Cardiovascular autonomic dysfunction in “Long COVID”: Pathophysiology, heart rate variability, and inflammatory markers. Front. Cardiovasc. Med. 2023, 10, 1256512. [Google Scholar] [CrossRef]
- de Abreu, R.M. Cardiac Changes Related to COVID-19 in Athletes: A Brief Review. Curr. Emerg. Hosp. Med. Rep. 2022, 10, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Zacher, J.; Branahl, A.; Predel, H.G.; Laborde, S. Effects of COVID-19 on the autonomic nervous system in elite athletes assessed by heart rate variability. Sport. Sci. Health 2023, 19, 1269–1280. [Google Scholar] [CrossRef]
- Aliani, C.; Rossi, E.; Luchini, M.; Calamai, I.; Deodati, R.; Spina, R.; Lanata, A.; Bocchi, L. Cardiovascular Dynamics in COVID-19: A Heart Rate Variability Investigation. In Proceedings of the 2022 44th Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Glasgow, UK, 11–15 July 2022; IEEE: Piscataway, NJ, USA, 2022. [Google Scholar]
- Gruionu, G.; Gupta, A.; Rattin, M.; Nowak, T.V.; Ward, M.; Everett, T.H. Heart Rate Variability Parameters Indicate Altered Autonomic Tone in Patients with COVID-19. FASEB J. 2022, 36 (Suppl. S1). [Google Scholar] [CrossRef]
- Camargo, S.M.; Silva, B.M.; Pereira, M.W.U.; dos Santos, A.L.G.; Maximo, S.T.; Watanabe, W.T.; Puglisi, J.L.; Goroso, D.G. Assessing Autonomic Nervous System Imbalance in Post-COVID-19 Patients through Heart Rate Variability During Tilt Testing. In Proceedings of the 2023 Computing in Cardiology Conference (CinC), Atlanta, GA, USA, 1–4 October 2023. [Google Scholar]
- Hashimoto, Y.; Okamoto, T. Arterial Stiffness and Left Ventricular Diastolic Function in Endurance Athletes. Int. J. Sports Med. 2020, 42, 497–505. [Google Scholar] [CrossRef] [PubMed]
- Vallee, A. Arterial Stiffness Determinants for Primary Cardiovascular Prevention among Healthy Participants. J. Clin. Med. 2022, 11, 2512. [Google Scholar] [CrossRef] [PubMed]
- Trimarchi, G.; Pizzino, F.; Paradossi, U.; Gueli, I.A.; Palazzini, M.; Gentile, P.; Di Spigno, F.; Ammirati, E.; Garascia, A.; Tedeschi, A. Charting the Unseen: How Non-Invasive Imaging Could Redefine Cardiovascular Prevention. J. Cardiovasc. Dev. Dis. 2024, 11, 245. [Google Scholar] [CrossRef]
- Laurent, S.; Boutouyrie, P. Arterial Stiffness as an Early Marker of Organ Damage, in Special Issues in Hypertension; Springer: Milan, Italy, 2012; pp. 171–179. [Google Scholar]
- Mitchell, G.F.; Hwang, S.J.; Vasan, R.S.; Larson, M.G.; Pencina, M.J.; Hamburg, N.M.; Vita, J.A.; Levy, D.; Benjamin, E.J. Arterial stiffness and cardiovascular events: The Framingham Heart Study. Circulation 2010, 121, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Jud, P.; Gressenberger, P.; Muster, V.; Avian, A.; Meinitzer, A.; Strohmaier, H.; Sourij, H.; Raggam, R.B.; Stradner, M.H.; Demel, U.; et al. Evaluation of Endothelial Dysfunction and Inflammatory Vasculopathy After SARS-CoV-2 Infection-A Cross-Sectional Study. Front. Cardiovasc. Med. 2021, 8, 750887. [Google Scholar] [CrossRef]
- Zhang, J.; Tecson, K.M.; McCullough, P.A. Endothelial dysfunction contributes to COVID-19-associated vascular inflammation and coagulopathy. Rev. Cardiovasc. Med. 2020, 21, 315–319. [Google Scholar] [CrossRef]
- Jannasz, I.; Pruc, M.; Rahnama-Hezavah, M.; Targowski, T.; Olszewski, R.; Feduniw, S.; Petryka, K.; Szarpak, L. The Impact of COVID-19 on Carotid-Femoral Pulse Wave Velocity: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 5747. [Google Scholar] [CrossRef]
- Luck, J.C.; Blaha, C.; Cauffman, A.; Gao, Z.; Arnold, A.C.; Cui, J.; Sinoway, L.I. Autonomic and vascular function testing in collegiate athletes following SARS-CoV-2 infection: An exploratory study. Front. Physiol. 2023, 14, 1225814. [Google Scholar] [CrossRef] [PubMed]
- Ratchford, S.M.; Stickford, J.L.; Province, V.M.; Stute, N.; Augenreich, M.A.; Koontz, L.K.; Bobo, L.K.; Stickford, A.S.L. Vascular alterations among young adults with SARS-CoV-2. Am. J. Physiol. Heart Circ. Physiol. 2021, 320, H404–H410. [Google Scholar] [CrossRef] [PubMed]
- Pereira, T.; Lira, F.; Caseiro, A.; Castanheira, J.; Coelho-e-Silva, M. COVID-19 and Arterial Stiffness in Vaccinated Young Adults without Prior Co-Morbidities. A Cross-Sectional Analysis of the Fit@4covid Cohort Study. J. Hypertens. 2023, 41 (Suppl. S3), e31. [Google Scholar] [CrossRef]
- Jetté, M.; Sidney, K.; Blümchen, G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin. Cardiol. 1990, 13, 555–565. [Google Scholar] [CrossRef] [PubMed]
- Mansoubi, M.; Pearson, N.; Clemes, S.A.; Biddle, S.J.; Bodicoat, D.H.; Tolfrey, K.; Edwardson, C.L.; Yates, T. Energy expenditure during common sitting and standing tasks: Examining the 1.5 MET definition of sedentary behaviour. BMC Public Health 2015, 15, 516. [Google Scholar] [CrossRef] [PubMed]
- Cunha, E.F.D.; Silveira, M.S.; Milan-Mattos, J.C.; Cavalini, H.F.S.; Ferreira, Á.A.; Batista, J.d.S.; Uzumaki, L.C.; Guimarães, J.P.C.; Roriz, P.I.L.; Dantas, F.M.d.N.A. Cardiac Autonomic Function and Functional Capacity in Post-COVID-19 Individuals with Systemic Arterial Hypertension. J. Pers. Med. 2023, 13, 1391. [Google Scholar] [CrossRef]
- Skazkina, V.V.; Krasikova, N.S.; Borovkova, E.I.; Gorshkov, A.Y.; Korolev, A.; Dadaeva, V.; Fedorovich, A.; Kuligin, A.; Drapkina, O.; Karavaev, A. Synchronization of autonomic control loops of blood circulation in patients with COVID-19. Russ. Open Med. J. 2021, 10, 307. [Google Scholar] [CrossRef]
- Bosy-Westphal, A.; Later, W.; Hitze, B.; Sato, T.; Kossel, E.; Gluer, C.C.; Heller, M.; Muller, M.J. Accuracy of bioelectrical impedance consumer devices for measurement of body composition in comparison to whole body magnetic resonance imaging and dual X-ray absorptiometry. Obes. Facts 2008, 1, 319–324. [Google Scholar] [CrossRef]
- Kyle, U.G.; Schutz, Y.; Dupertuis, Y.M.; Pichard, C. Body composition interpretation. Nutrition 2003, 19, 597–604. [Google Scholar] [CrossRef]
- Selberg, O.; Selberg, D. Norms and correlates of bioimpedance phase angle in healthy human subjects, hospitalized patients, and patients with liver cirrhosis. Eur. J. Appl. Physiol. 2002, 86, 509–516. [Google Scholar] [CrossRef]
- Graham, B.L.; Steenbruggen, I.; Miller, M.R.; Barjaktarevic, I.Z.; Cooper, B.G.; Hall, G.L.; Hallstrand, T.S.; Kaminsky, D.A.; McCarthy, K.; McCormack, M.C.; et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 2019, 200, e70–e88. [Google Scholar] [CrossRef] [PubMed]
- Roca, J. References values for forced spirometry. Group of the European Community Respiratory Health Survey. Eur. Respir. J. 1998, 11, 1354–1362. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, F.; McCraty, R.; Zerr, C.L. A healthy heart is not a metronome: An integrative review of the heart’s anatomy and heart rate variability. Front. Psychol. 2014, 5, 1040. [Google Scholar] [CrossRef] [PubMed]
- Allen, J. Photoplethysmography and its application in clinical physiological measurement. Physiol. Meas. 2007, 28, R1–R39. [Google Scholar] [CrossRef] [PubMed]
- Millasseau, S.C.; Guigui, F.G.; Kelly, R.P.; Prasad, K.; Cockcroft, J.R.; Ritter, J.M.; Chowienczyk, P.J. Noninvasive assessment of the digital volume pulse. Comparison with the peripheral pressure pulse. Hypertension 2000, 36, 952–956. [Google Scholar] [CrossRef]
- Elgendi, M. On the analysis of fingertip photoplethysmogram signals. Curr. Cardiol. Rev. 2012, 8, 14–25. [Google Scholar] [CrossRef]
- Laurent, S. European Network for Non-invasive Investigation of Large Arteries. Expert consensus document on arterial stiffness: Methodological issues and clinical applications. Eur. Heart J. 2006, 27, 2588–2605. [Google Scholar] [CrossRef]
- Wilkinson, I.B.; MacCallum, H.; Flint, L.; Cockcroft, J.R.; Newby, D.E.; Webb, D.J. The influence of heart rate on augmentation index and central arterial pressure in humans. J. Physiol. 2000, 525 Pt 1, 263–270. [Google Scholar] [CrossRef]
- Vlachopoulos, C.; Aznaouridis, K.; Stefanadis, C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010, 55, 1318–1327. [Google Scholar] [CrossRef]
- Muntner, P.; Shimbo, D.; Carey, R.M.; Charleston, J.B.; Gaillard, T.; Misra, S.; Myers, M.G.; Ogedegbe, G.; Schwartz, J.E.; Townsend, R.R.; et al. Measurement of Blood Pressure in Humans: A Scientific Statement from the American Heart Association. Hypertension 2019, 73, E35–E66. [Google Scholar] [CrossRef]
- Charloux, A.; Lonsdorfer-Wolf, E.; Richard, R.; Lampert, E.; Oswald-Mammosser, M.; Mettauer, B.; Geny, B.; Lonsdorfer, J. A new impedance cardiograph device for the non-invasive evaluation of cardiac output at rest and during exercise: Comparison with the “direct” Fick method. Eur. J. Appl. Physiol. 2000, 82, 313–320. [Google Scholar] [CrossRef]
- Tonelli, A.R.; Alnuaimat, H.; Li, N.; Carrie, R.; Mubarak, K.K. Value of Impedance Cardiography in Patients Studied for Pulmonary Hypertension. Lung 2011, 189, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Schrading, W.; McCafferty, B.; Grove, J.; Page, D. Portable, consumer-grade pulse oximeters are accurate for home and medical use: Implications for use in the COVID-19 pandemic and other resource-limited environments. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1450–1458. [Google Scholar] [CrossRef] [PubMed]
- Bassett, D.R.; Howley, E.T. Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med. Sci. Sports Exerc. 2000, 32, 70–84. [Google Scholar] [CrossRef] [PubMed]
- Poole, D.C.; Behnke, B.J.; Padilla, D.J. Dynamics of muscle microcirculatory oxygen exchange. Med. Sci. Sports Exerc. 2005, 37, 1559–1566. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Taylor and Francis: Hoboken, NJ, USA, 2013; pp. 23–26. [Google Scholar]
- Hull, J.H.; Wootten, M.; Moghal, M.; Heron, N.; Martin, R.; Walsted, E.S.; Biswas, A.; Loosemore, M.; Elliott, N.; Ranson, C. Clinical patterns, recovery time and prolonged impact of COVID-19 illness in international athletes: The UK experience. Br. J. Sports Med. 2022, 56, 4–11. [Google Scholar] [CrossRef]
- Morley, J.E.; Kalantar-Zadeh, K.; Anker, S.D. COVID-19: A major cause of cachexia and sarcopenia? J. Cachexia Sarcopenia Muscle 2020, 11, 863–865. [Google Scholar] [CrossRef]
- Czeck, M.A.; Roelofs, E.J.; Evanoff, N.G.; Dengel, D.R. No Changes in Body Composition in NCAA Division I Collegiate Football Players because of COVID-19 Restrictions. J. Strength. Cond. Res. 2022, 36, 1749–1752. [Google Scholar] [CrossRef]
- Bila, W.C.; Silva, A.M.e.; Bicalho, L.G.; Cândido, R.; Costa, J.R.S.; Salgado, J.V.V.; Campos, C.G.; Café, A.C.C.; Amaral, P.C.d.; Novais, R.L.R.; et al. Body Composition and Level of Physical Activity in Post-COVID-19 Patients. Arch. Curr. Res. Int. 2023, 23, 95–103. [Google Scholar] [CrossRef]
- Rosa, B.V.; Maldonado, A.J.; de Araujo, A.O.; Neves, L.M.; Rossi, F.E. Impact of the COVID-19 Lockdown on the Body Composition and Physical Performance of Athletes: A Systematic Review with Meta-Analysis and Meta-Regression. Healthcare 2023, 11, 2319. [Google Scholar] [CrossRef] [PubMed]
- Mohr, M.; Nassis, G.P.; Brito, J.; Randers, M.B.; Castagna, C.; Parnell, D.; Krustrup, P. Return to elite football after the COVID-19 lockdown. Manag. Sport. Leis. 2020, 27, 172–180. [Google Scholar] [CrossRef]
- Komici, K.; Bianco, A.; Perrotta, F.; Dello Iacono, A.; Bencivenga, L.; D’Agnano, V.; Rocca, A.; Bianco, A.; Rengo, G.; Guerra, G. Clinical Characteristics, Exercise Capacity and Pulmonary Function in Post-COVID-19 Competitive Athletes. J. Clin. Med. 2021, 10, 3053. [Google Scholar] [CrossRef] [PubMed]
- Nissanka, W.; Jayasekara, R.T.; Karunanayake, R.; Ekanayake, L.; Chathurantha, S.; Wijesinghe, N.; Fernando, A. Impact of COVID 19 Infection on Cardiopulmonary Functions of a Cohort of National Level Athletes in Sri Lanka. In 01.05—Clinical Respiratory Physiology, Exercise and Functional Imaging; European Respiratory Society: Brussels, Belgium, 2022. [Google Scholar]
- Besson, C.; Guex, K.; Schmitt, L.; Gojanovic, B.; Gremeaux, V. Successful Return to Performance After COVID-19 Infection in an Elite Athlete. Int. J. Sports Physiol. Perform. 2022, 17, 667–670. [Google Scholar] [CrossRef] [PubMed]
- Bhati, P.; Moiz, J.A.; Menon, G.R.; Hussain, M.E. Does resistance training modulate cardiac autonomic control? A systematic review and meta-analysis. Clin. Auton. Res. 2019, 29, 75–103. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.G.; Hull, J.H.; Rogers, J.; Pollock, N.; Dodd, M.; Haines, J.; Harris, S.; Loosemore, M.; Malhotra, A.; Pieles, G.; et al. Cardiorespiratory considerations for return-to-play in elite athletes after COVID-19 infection: A practical guide for sport and exercise medicine physicians. Br. J. Sports Med. 2020, 54, 1157–1161. [Google Scholar] [CrossRef]
- Sollazzo, F.; Morra, L.; Zanotto, A.; Monti, R.; Bianco, M.; Modica, G.; Penza, V.M.; Skittel, O.; Zeppilli, P.; Palmieri, V. Effect Effect of Sars-CoV-2 infection on heart rate variability of young competitive athletes. Med. Sport. 2023, 76, 353–362. [Google Scholar] [CrossRef]
- Pla, R.; Bosquet, L.; McGibbon, K.; Mujika, I.; Aubry, A. Heart rate variability in elite swimmers before, during and after COVID-19 lockdown: A brief report on time domain analysis. Appl. Sci. 2021, 11, 8106. [Google Scholar] [CrossRef]
- Menezes Junior, A.D.S.; Schroder, A.A.; Botelho, S.M.; Resende, A.L. Cardiac Autonomic Function in Long COVID-19 Using Heart Rate Variability: An Observational Cross-Sectional Study. J. Clin. Med. 2022, 12, 100. [Google Scholar] [CrossRef]
- Michael, S.; Graham, K.S.; Davis, G.M.O. Cardiac Autonomic Responses during Exercise and Post-exercise Recovery Using Heart Rate Variability and Systolic Time Intervals-A Review. Front. Physiol. 2017, 8, 301. [Google Scholar] [CrossRef] [PubMed]
- Chirinos, J.A.; Segers, P.; Hughes, T.; Townsend, R. Large-Artery Stiffness in Health and Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019, 74, 1237–1263. [Google Scholar] [CrossRef] [PubMed]
- Nagele, M.P.; Haubner, B.; Tanner, F.C.; Ruschitzka, F.; Flammer, A.J. Endothelial dysfunction in COVID-19: Current findings and therapeutic implications. Atherosclerosis 2020, 314, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Kar, M. Vascular Dysfunction and Its Cardiovascular Consequences During and After COVID-19 Infection: A Narrative Review. Vasc. Health Risk Manag. 2022, 18, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Zota, I.M.; Statescu, C.; Sascau, R.A.; Roca, M.; Anghel, L.; Mastaleru, A.; Leon-Constantin, M.M.; Ghiciuc, C.M.; Cozma, S.R.; Dima-Cozma, L.C.; et al. Acute and Long-Term Consequences of COVID-19 on Arterial Stiffness-A Narrative Review. Life 2022, 12, 781. [Google Scholar] [CrossRef]
- van Hattum, J.C.; Spies, J.L.; Verwijs, S.M.; Verwoert, G.C.; Planken, R.N.; Boekholdt, S.M.; Groenink, M.; Malekzadeh, A.; Pinto, Y.M.; Wilde, A.A.M.; et al. Cardiac abnormalities in athletes after SARS-CoV-2 infection: A systematic review. BMJ Open Sport. Exerc. Med. 2021, 7, e001164. [Google Scholar] [CrossRef]
- Rajpal, S.; Tong, M.S.; Borchers, J.; Zareba, K.M.; Obarski, T.P.; Simonetti, O.P.; Daniels, C.J. Cardiovascular Magnetic Resonance Findings in Competitive Athletes Recovering from COVID-19 Infection. JAMA Cardiol. 2021, 6, 116–118. [Google Scholar] [CrossRef]
- Bauer, P.; Kraushaar, L.; Dorr, O.; Keranov, S.; Nef, H.; Hamm, C.W.; Most, A. Vascular alterations among male elite athletes recovering from SARS-CoV-2 infection. Sci. Rep. 2022, 12, 8655. [Google Scholar] [CrossRef]
- Schnaubelt, S.; Oppenauer, J.; Tihanyi, D.; Mueller, M.; Maldonado-Gonzalez, E.; Zejnilovic, S.; Haslacher, H.; Perkmann, T.; Strassl, R.; Anders, S.; et al. Arterial stiffness in acute COVID-19 and potential associations with clinical outcome. J. Intern. Med. 2021, 290, 437–443. [Google Scholar] [CrossRef]
- Green, D.J.; Hopman, M.T.; Padilla, J.; Laughlin, M.H.; Thijssen, D.H. Vascular Adaptation to Exercise in Humans: Role of Hemodynamic Stimuli. Physiol. Rev. 2017, 97, 495–528. [Google Scholar] [CrossRef]
- Naylor, L.H.; Spence, A.L.; Donker, S.C.M.; Thijssen, D.H.J.; Green, D.J. Is there an athlete’s artery? A comparison of brachial and femoral artery structure and function in male strength, power and endurance athletes. J. Sci. Med. Sport. 2021, 24, 635–640. [Google Scholar] [CrossRef] [PubMed]
- Raman, B.; Cassar, M.P.; Tunnicliffe, E.M.; Filippini, N.; Griffanti, L.; Alfaro-Almagro, F.; Okell, T.; Sheerin, F.; Xie, C.; Mahmod, M.; et al. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. EClinicalMedicine 2021, 31, 100683. [Google Scholar] [CrossRef]
- Starekova, J.; Bluemke, D.A.; Bradham, W.S.; Eckhardt, L.L.; Grist, T.M.; Kusmirek, J.E.; Purtell, C.S.; Schiebler, M.L.; Reeder, S.B. Evaluation for Myocarditis in Competitive Student Athletes Recovering from Coronavirus Disease 2019 with Cardiac Magnetic Resonance Imaging. JAMA Cardiol. 2021, 6, 945–950. [Google Scholar] [CrossRef] [PubMed]
- Puntmann, V.O.; Carerj, M.L.; Wieters, I.; Fahim, M.; Arendt, C.; Hoffmann, J.; Shchendrygina, A.; Escher, F.; Vasa-Nicotera, M.; Zeiher, A.M.; et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered from Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 1265–1273. [Google Scholar] [CrossRef] [PubMed]
- Libby, P.; Lüscher, T. COVID-19 is, in the end, an endothelial disease. Eur. Heart J. 2020, 41, 3038–3044. [Google Scholar] [CrossRef] [PubMed]
- Dellavechia de Carvalho, C.; Bertucci, D.R.; Ribeiro, F.A.; Costa, G.P.; Toro, D.M.; Camacho-Cardenosa, M.; Brazo-Sayavera, J.; Sorgi, C.A.; Papoti, M.; Trape, A.A. Effects of Moderate-Intensity Training Under Cyclic Hypoxia on Cardiorespiratory Fitness and Hematological Parameters in People Recovered from COVID-19: The AEROBICOVID Study. Sports Health 2023, 15, 558–570. [Google Scholar] [CrossRef]
- Kalliokoski, K.K.; Oikonen, V.; Takala, T.O.; Sipila, H.; Knuuti, J.; Nuutila, P. Enhanced oxygen extraction and reduced flow heterogeneity in exercising muscle in endurance-trained men. Am. J. Physiol. Endocrinol. Metab. 2001, 280, E1015–E1021. [Google Scholar] [CrossRef]
- Lemes, I.R.; Smaira, F.I.; Ribeiro, W.J.D.; Favero, N.K.; Matos, L.; Pinto, A.L.S.; Dolan, E.; Gualano, B.; Coalition, S.-C. Acute and post-acute COVID-19 presentations in athletes: A systematic review and meta-analysis. Br. J. Sports Med. 2022, 56, 941–947. [Google Scholar] [CrossRef]
- Baratto, C.; Caravita, S.; Faini, A.; Perego, G.B.; Senni, M.; Badano, L.P.; Parati, G. Impact of COVID-19 on exercise pathophysiology: A combined cardiopulmonary and echocardiographic exercise study. J. Appl. Physiol. 2021, 130, 1470–1478. [Google Scholar] [CrossRef]
- Scala, I.; Rizzo, P.A.; Bellavia, S.; Brunetti, V.; Colò, F.; Broccolini, A.; Della Marca, G.; Calabresi, P.; Luigetti, M.; Frisullo, G. Autonomic dysfunction during acute SARS-CoV-2 infection: A systematic review. J. Clin. Med. 2022, 11, 3883. [Google Scholar] [CrossRef]
| COVID-19 Group (n = 60) | Control Group (n = 60) | t | p | 95% CI | Effect Size | |
|---|---|---|---|---|---|---|
| Age (years) | 23.4 ± 6.6 | 21.0 ± 9.1 | 1.65 | 0.101 | [−0.46, 5.26] | 0.30 |
| Wt (kg) | 78.4 ± 9.0 | 74.8 ± 12.0 | 1.45 | 0.150 | [−1.31, 8.91] | 0.34 |
| Ht (cm) | 183.4 ± 6.3 | 181.2 ± 9.0 | 1.55 | 0.124 | [−0.08, 0.64] | 0.63 |
| BMI (kg/m2) | 26.6 ± 1.1 | 26.6 ± 1.8 | 0.00 | 1.000 | [−0.54, 0.54] | 0.00 |
| LM (kg) | 68.2 ± 7.4 | 64.7 ± 8.5 | 2.41 | 0.017 | [0.62, 6.38] | 0.44 |
| FM (kg) | 12.9 ± 3.6 | 13.0 ± 5.8 | −0.11 | 0.913 | [−1.84, 1.64] | −0.02 |
| TBW (L) | 63.8 ± 2.7 | 63.7 ± 4.2 | 0.16 | 0.871 | [−1.18, 1.38] | 0.03 |
| MM (kg) | 23.3 ± 2.4 | 23.2 ± 3.4 | 0.19 | 0.849 | [−0.96, 1.16] | 0.03 |
| PhA (degrees) | 7.9 ± 1.2 | 7.7 ± 1.4 | 0.84 | 0.403 | [−0.27, 0.67] | 0.15 |
| Years of training (years) | 13.55 ± 4.22 | 12.8 ± 5.07 | 0.82 | 0.413 | [−0.21, 0.51] | 0.15 |
| Hours of training per week | 15.30 ± 5.19 | 15.89 ± 6.35 | −0.56 | 0.578 | [−0.46, 0.26] | −0.10 |
| COVID-19 Group (n = 60) | Control Group (n = 60) | t-Value | p-Value | 95% CI | Cohen’s d | |
|---|---|---|---|---|---|---|
| FVC (L) | 5.9 ± 0.8 | 5.3 ± 1.1 | 3.40 | 0.001 | [0.24, 0.96] | 0.62 |
| FEV1 (L) | 5.0 ± 0.7 | 4.6 ± 1.0 | 2.75 | 0.007 | [0.10, 0.70] | 0.49 |
| FEV1/FVC (%) | 85.0 ± 6.6 | 86.0 ± 11.5 | −0.55 | 0.584 | [−4.80, 2.80] | −0.10 |
| PEF (l/s) | 8.5 ± 1.5 | 8.8 ± 1.8 | −0.90 | 0.370 | [−1.14, 0.43] | −0.18 |
| FEV1 % | 102.9 ± 15.3 | 106.8 ± 13.3 | −1.54 | 0.126 | [−8.89, 1.12] | −0.27 |
| FEF25–75% (L/s) | 4.2 ± 1.0 | 4.5 ± 1.2 | −1.38 | 0.171 | [−0.72, 0.13] | −0.27 |
| MVV (L/min) | 180 ± 20 | 175 ± 25 | 1.23 | 0.220 | [−3.02, 13.02] | 0.22 |
| COVID-19 Group (n = 60) | Control Group (n = 60) | t-Value | p-Value | 95% CI | Cohen’s d | |
|---|---|---|---|---|---|---|
| Heart rate (bpm) | 79.3 ± 9.5 | 81.5 ± 12.7 | −1.01 | 0.316 | [−6.51, 2.11] | −0.20 |
| HF (%) | 32.7 ± 7.1 | 31.4 ± 7.4 | 0.94 | 0.349 | [−1.39, 3.79] | 0.18 |
| LF (%) | 35.7 ± 9.1 | 35.1 ± 11.8 | 0.29 | 0.770 | [−3.40, 4.60] | 0.06 |
| LF/HF | 1.2 ± 0.5 | 1.2 ± 0.6 | 0.00 | 1.000 | [−0.21, 0.21] | 0.00 |
| SDNN (ms) | 51.9 ± 10.5 | 53.5 ± 16.1 | −0.56 | 0.576 | [−6.97, 3.77] | −0.11 |
| COVID-19 Group (n = 60) | Control Group (n = 60) | t | p | 95% CI | Cohen’s d | |
|---|---|---|---|---|---|---|
| TI (unitless) | 128.0 ± 56.2 | 128.9 ± 80.6 | −0.07 | 0.945 | [−29.66, 27.86] | −0.01 |
| SI (unitless) | 6.4 ± 0.7 | 6.1 ± 0.9 | 1.86 | 0.065 | [−0.02, 0.62] | 0.35 |
| RI (%) | 25.8 ± 2.7 | 27.2 ± 4.3 | −2.10 | 0.038 | [−2.73, −0.08] | −0.40 |
| AI (unitless) | 1.0 ± 0.1 | 1.0 ± 0.1 | 0.00 | 1.000 | [−0.03, 0.03] | 0.00 |
| b/a (unitless) | −1.1 ± 0.2 | −1.1 ± 0.2 | 0.00 | 1.000 | [−0.08, 0.08] | 0.00 |
| c/a (unitless) | −0.1 ± 0.1 | −0.1 ± 0.1 | 0.00 | 1.000 | [−0.03, 0.03] | 0.00 |
| d/a (unitless) | −0.3 ± 0.0 | −0.3 ± 0.0 | 0.00 | 1.000 | [−0.01, 0.01] | 0.00 |
| e/a (uniform) | 0.3 ± 0.1 | 0.3 ± 0.2 | 0.00 | 1.000 | [−0.06, 0.06] | 0.00 |
| COVID-19 Group (n = 60) | Control Group (n = 60) | t | p | 95% CI | Cohen’s d | |
|---|---|---|---|---|---|---|
| MBP (mmHg) | 89.8 ± 8.7 | 89.4 ± 7.7 | 0.27 | 0.785 | [−1.99, 2.59] | 0.04 |
| SBP (mmHg) | 125.0 ± 12.0 | 124.3 ± 11.9 | 0.29 | 0.772 | [−3.54, 4.94] | 0.06 |
| DBP (mmHg) | 72.1 ± 8.7 | 71.9 ± 7.9 | 0.14 | 0.886 | [−2.37, 2.77] | 0.02 |
| PVR (dyn·s/cm2) | 1085.4 ± 123.7 | 1142.5 ± 166.2 | −2.00 | 0.048 | [−113.50, −0.50] | −0.37 |
| CO (L/min) | 6.7 ± 0.7 | 6.4 ± 0.9 | 1.89 | 0.061 | [−0.01, 0.61] | 0.34 |
| SVI (mL/m2/beat) | 3.3 ± 0.3 | 3.3 ± 0.4 | 0.00 | 1.000 | [−0.10, 0.10] | 0.00 |
| SpO2 (%) | 94.4 ± 1.6 | 94.5 ± 1.8 | −0.31 | 0.756 | [−0.85, 0.65] | −0.06 |
| ACI (mlO2/min/m2) | 71 ± 5 | 73 ± 7 | −1.80 | 0.074 | [−4.20, 0.2] | −0.33 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ammar, M.M.; Ben Said, N.M.; Ben Said, Y.N.; Abdelsalam, A.M.; Levushkin, S.P.; Laptev, A.; Inoubli, M.; Chlif, M. Comparative Analysis of Heart Rate Variability and Arterial Stiffness in Elite Male Athletes after COVID-19. J. Clin. Med. 2024, 13, 5990. https://doi.org/10.3390/jcm13195990
Ammar MM, Ben Said NM, Ben Said YN, Abdelsalam AM, Levushkin SP, Laptev A, Inoubli M, Chlif M. Comparative Analysis of Heart Rate Variability and Arterial Stiffness in Elite Male Athletes after COVID-19. Journal of Clinical Medicine. 2024; 13(19):5990. https://doi.org/10.3390/jcm13195990
Chicago/Turabian StyleAmmar, Mohamed M., Noureddine M. Ben Said, Younes N. Ben Said, Ahmed M. Abdelsalam, Sergey P. Levushkin, Aleksey Laptev, Mokhtar Inoubli, and Mehdi Chlif. 2024. "Comparative Analysis of Heart Rate Variability and Arterial Stiffness in Elite Male Athletes after COVID-19" Journal of Clinical Medicine 13, no. 19: 5990. https://doi.org/10.3390/jcm13195990
APA StyleAmmar, M. M., Ben Said, N. M., Ben Said, Y. N., Abdelsalam, A. M., Levushkin, S. P., Laptev, A., Inoubli, M., & Chlif, M. (2024). Comparative Analysis of Heart Rate Variability and Arterial Stiffness in Elite Male Athletes after COVID-19. Journal of Clinical Medicine, 13(19), 5990. https://doi.org/10.3390/jcm13195990





