Abstract
Androgenetic alopecia, the most common cause of hair loss affecting both men and women, is typically treated using pharmaceutical options, such as minoxidil and finasteride. While these medications work for many individuals, they are not suitable options for all. To date, the only non-pharmaceutical option that the United States Food and Drug Administration has cleared as a treatment for androgenetic alopecia is low-level laser therapy (LLLT). Numerous clinical trials utilizing LLLT devices of various types are available. However, a myriad of other physical treatments for this form of hair loss have been reported in the literature. This review evaluated the effectiveness of microneedling, pulsed electromagnetic field (PEMF) therapy, low-level laser therapy (LLLT), fractional laser therapy, and nonablative laser therapy for the treatment of androgenetic alopecia (AGA). It also explores the potential of multimodal treatments combining these physical therapies. The majority of evidence in the literature supports LLLT as a physical therapy for androgenetic alopecia. However, other physical treatments, such as nonablative laser treatments, and multimodal approaches, such as PEMF-LLLT, seem to have the potential to be equally or more promising and merit further exploration.
1. Introduction
Androgenetic alopecia (AGA) is the most common cause of hair loss, potentially affecting over 50% men and women throughout their lives. It is a non-scarring alopecia in which the progressive miniaturization of hair follicles leads to a loss of hair density. Without treatment, AGA may result in extensive areas of complete baldness, resulting in significant emotional repercussions for the patients and impacting their quality of life [1,2].
Currently, the treatment of AGA relies on the use of two fundamental drugs: minoxidil and 5-alpha reductase inhibitors (5ARIs). Minoxidil has been approved for this indication in topical form (2% or 5% concentrations), or is orally administered off-label (from 0.5 to 10 mg per day). 5ARIs include medications such as 1 mg finasteride, which is formally approved for this indication, and dutasteride, which is more effective than finasteride, but, to date, lacks formal approval in the vast majority of countries. These drugs have demonstrated satisfactory results in a significant percentage of patients with AGA [3,4,5,6,7].
However, certain limitations, such as the inability to use 5ARIs for patients with a history of hormone-dependent neoplasms or those desiring pregnancy, as well as the desire to improve therapeutic outcomes without continuously using pharmacological treatments, have led to the exploration of other treatment approaches, especially those based on physical therapies. With increasing evidence of their effectiveness and safety, these therapeutics represent a valid alternative and are positioning themselves as complementary approaches to improve the results achieved with conventional treatments in a significant number of patients [8,9].
2. Methods
This is a narrative review. Clinical pictures of male and female patients with androgenetic alopecia are presented, reporting the course of the disease, differential diagnoses, and common treatment options. This narrative presentation focuses on physical therapeutic options for the treatment of androgenetic alopecia, which can be divided into three categories: microneedling, laser hair therapy, and pulsed electromagnetic field therapy.
The available literature on androgenetic alopecia was analyzed, seeking non-pharmacological, nutraceutical, or regenerative medicine approaches to the treatment of this form of hair loss. A literature search was conducted using MEDLINE via PubMed and Google Scholar databases, covering the period from 1 January 1980 to 1 May 2024. The following keywords were used: androgenetic alopecia, pattern hair loss, microneedling, laser, LLLT, pulsed electromagnetic, pulsed electrostatic, pulsed electrical, and PEMF. Studies on other forms of hair loss were excluded unless they made specific mention of androgenetic alopecia as well. The exclusion criteria were conference abstracts and articles in languages other than English, Spanish, or Portuguese.
3. Results
3.1. Low-Level Laser Therapy (LLLT)
LLLT for AGA is based on the principle of photobiomodulation, a branch of photobiology that studies the effect of low-energy light on dysregulated biological processes. One of the primary underlying principles of photobiomodulation is hormesis, the use of low-level energy to stimulate a specific biological process, whereas the use of the same type of energy at higher doses could have a completely opposite, suppressive effect [10,11,12,13].
The main mechanisms of action attributed to photobiomodulation involve the mobilization of molecules, such as reactive oxygen species (ROS), nitric oxide (NO), and adenosine triphosphate (ATP), as shown in Figure 1. This occurs through interaction with mitochondrial chromophores like cytochrome C oxidase (CCO), leading to mitochondrial respiration and ATP production. These molecules, including ROS, ATP, and NO, activate the redox-related signaling pathways, positively impacting hair growth by stimulating cellular proliferation, migration, and the differentiation of hair bulge stem cells, as shown in Figure 2. Additionally, ATP prompts increased hair growth through the transition from the telogen to anagen phases. Photobiomodulation also mediates skin benefits through pathways, such as VEGF and Wnt/β-catenin signaling, further enhancing its therapeutic effects [14,15,16]. In 2007, the United States Food and Drug Administration (FDA) cleared the first LLLT device, the Hairmax Laser Comb®, for male AGA. The device was cleared for the treatment of female pattern hair loss shortly after in 2011 [17,18,19]. There are, to date, over 80 LLLT devices that have been granted 510(k) clearance by the US FDA. These devices, which are generally designed as comb-type or helmet-type tools, typically have red laser diodes or red light-emitting diodes with wavelengths between 630 and 660 nm. Despite the difference in the number of diodes and the variations in wavelengths, power, and treatment times, these devices are considered to be nearly equivalent in effectiveness, with laser helmets showing slightly more effectiveness than laser combs or brushes [18,20,21].
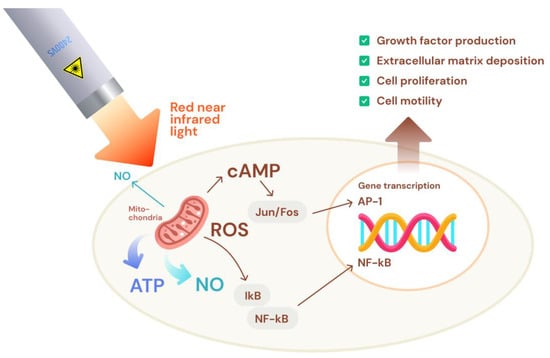
Figure 1.
The effect of photobiomodulation on mitochondria and gene expression.
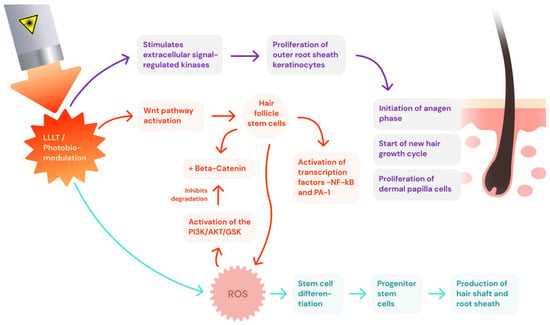
Figure 2.
The pathways photobiomodulation use to influence hair growth.
Since then, several clinical trials have been conducted to demonstrate the efficacy of LLLT in the treatment of AGA, as shown in Table 1. These studies typically utilize short treatment times from around 8 to 30 min in duration, with treatments applied as infrequently as twice a week or as frequently as every day. Interestingly, the shortest treatment time of 8 min a day, three times per week over 26 weeks reported the largest increase: 25.7 hairs per cm2. Conversely, a 24 week treatment applying 30-min-a-day treatments produced an increase of just 6 hairs per cm2 [22,23,24,25].
In most LLLT studies, mild-to-moderate efficacy has been demonstrated showing improved hair density and tensile strength and reduced hair loss. While some studies did not report a clear overall improvement, more than 70% of patients expressed satisfaction with the results obtained, highlighting the absence of serious adverse effects and excellent treatment tolerance [22,23,24,26,27,28,29,30].

Table 1.
Reported improvements in hair growth at 12–36 weeks following the administration of physical therapy.
Table 1.
Reported improvements in hair growth at 12–36 weeks following the administration of physical therapy.
| Study | AGA Diagnosis | Treatment Regimen | Treatment | Subject Demographics | Duration (Weeks) | Improvement in Hair Density (Total Hairs/cm2) |
|---|---|---|---|---|---|---|
| Kumar et al., 2018 [31] | 2× daily treatment | Minoxidil 5% | 34 M 27.53 Y (avg.) | 12 | 1.89 ± 8.94 | |
| NH III-IV | 2× daily treatment, as well as 8 sessions: four 1× per week, then four fortnightly sessions | Minoxidil 5% Microneedling | 34 M 24.56 Y (avg.) | 12 | 12.82 ± 6.82 | |
| Dhurat et al., 2013 [32] | 2× daily treatment | Minoxidil 5% | 44 M 28.6 Y (avg.) | 12 | 22 | |
| NH III-IV | 2× daily treatment, as well as 1× weekly microneedling (with no minoxidil on day of microneedling) | Minoxidil 5% Microneedling | 50 M 28.6 Y (avg.) | 12 | 91.4 | |
| Choi and Park 2022 [33] | NH II+ L I+ | 15 min LLLT and 10 min PEMF 17 treatments: 1× per week for 12 weeks, then 1× every 2 weeks for 8 weeks, then 1× in 4 weeks | PEMF and LLLT | 31 M, 9 F 40.18 ± 6.77 Y | 23 | 24.8 ± 2.65 |
| Sham | 28 M, 12 F 39.55 ± 7.75 Y | 23 | 6.5 ± 1.85 | |||
| Bureau et al., 2003 [34] | NH I-VII L I-II | 30 min 3× per week | PEMF and Nutraceutical | 31 M, 9 F 38.6 ± 8.14 Y | 26 | 34 |
| Sham and placebo nutraceutical | 21 M, 8 F 40.6 ± 9.32 Y | 26 | 9 | |||
| Maddin et al., 1990 [35] | 12 min 20 1× per week 4 2× per week | PEMF using Electrotricho-genesis | 30 M 37.23 ± 5.24 Y | 12 | 3.67 ± 6.72 * | |
| PEMF using Electrotricho-genesis | 30 M 37.23 ± 5.24 Y | 24 | 7.08 ± 8.59 * | |||
| NH III-IV | PEMF using Electrotricho-genesis | 30 M 37.23 ± 5.24 Y | 36 | 11.87 ± 10.61 * | ||
| Sham | 26 M 37.96 ± 6.76 Y | 12 | −1.97 ± 8.79 * | |||
| Sham | 26 M 37.96 ± 6.76 Y | 24 | 1.93 ± 8.3 * | |||
| Sham | 26 M 37.96 ± 6.76 Y | 36 | 5.61 ± 10.25 * | |||
| Maddin et al., 1992 [36] | NH III-IV | 12 min 20 1× per week 4 2× per week | PEMF using Electrotricho-genesis | 14 M 37 ± 2.1 Y | 24 | 11.66 ± 1.38 * |
| 12 min 26 1× per week 4 2× per week | PEMF using Electrotricho-genesis | 14 M 37 ± 2.1 Y | 30 | 17.59 ± 1.98 * | ||
| Leavitt et al., 2009 [22] | NH IIa-V FS I-IV | 15 min 3× per week | LLLT using the HairMax LaserComb | 71 M 47.9 ± 8.7 Y | 26 | 17.3 ± 11.9 * |
| Sham | 39 M 47.9 ± 8.7 Y | 26 | −8.9 ± 11.7 * | |||
| Kim et al., 2013 [23] | NH III-VII L I-III | 18 min daily | LLLT using the Oaze 3R Helmet | 15 M and F 43.9 ± 12.2 Y | 24 | 17.2 ± 12.1 |
| Sham | 14 M and F 44.5 ± 11.4 Y | 24 | −2.1 ± 18.3 | |||
| Mai-Yi Fan et al., 2018 [25] | NH IIa-V LI-4, II-1, II-2 FS I-IV | 30 min 3× per week | LLLT using the Restore ID-520 | 61 M 37.2 ± 8.3 Y 13 F 37.2 ± 8.3 Y 61 M 37.1 ± 8.1 Y | 24 24 | 6 ± 12.5 |
| Sham | 13 F 37.1 ± 8.1 Y | −2 ± 12.6 | ||||
| 11 min 3× per week | LLLT using 9-beam HairMax LaserComb | 42 F 49.3 ± 9.1 Y | 26 | 20.2 ± 11.2 * | ||
| Sham | 21 F 49.8 ± 7.3 Y | 26 | 2.8 ± 16.5 * | |||
| 8 min 3× per week | LLLT using 12-beam HairMax LaserComb | 39 F 48.7 ± 10.2 Y | 26 | 20.6 ± 11.6 * | ||
| Jimenez et al., 2014 [24] | NH IIa-V | Sham | 18 F 49.1 ± 8.3 Y | 26 | 3.0 ± 9.3 * | |
| 15 min 3× per week | LLLT using 7-beam HairMax LaserComb | 24 M 47.8 ± 9.0 Y | 26 | 18.4 ± 13.7 * | ||
| Sham | 14 M 40.9 ± 9.5 Y | 26 | 3.0 ± 9.3 * | |||
| 11 min, 3× per week 8 min, 3× per week | LLLT using 9-beam or HairMax Laser Comb or 12-beam HairMax Laser Comb | 21 M 45.6 ± 9.3 Y 19 M 47.9 ± 9.6 Y | 26 | 20.9 ± 13.5 * 25.7 ± 17.1 * | ||
| Sham | 21 M 45.9 ± 10.4 Y | 26 | 9.4 ± 12.9 * | |||
| Lodi et al., 2021 [37] | NH III-VI | 24 min 2× per week | Blue LLLT | 20 M 38.55 ±11.68 Y | 10 | 11 ± 3 |
| Lee et al., 2011 [38] | L I-II | 10 treatments (every fortnight) | 1550 fractional Er/Glass Laser | 27 F 41.8 ± 1.96 Y | 20 | 57 ± 14 |
Abbreviations: NH = Norwood–Hamilton Scale; FS = Fitzpatrick Scale; L = Ludwig Scale, M = Male; F = Female; Y = Years of age. *: Only ‘terminal hairs per cm/2′ were reported for this study.
Adverse effects from LLLT used as an AGA treatment are usually very limited, including mild adverse events, such as scalp tenderness and itchiness. The side effects are generally self-resolvable within a 2 week period, and no serious side effects requiring the discontinuation of treatment have been reported [20]. However, as an increasing number of copycat devices entered the market, manufacturers attempted to increase the effectiveness of their LLLT devices by changing the number of diodes, the power emitted, and other variables. Manufacturers like LaserCap noted that increasing power correlates with increased effectiveness, but it can also result in increased adverse events [39].
FDA-cleared LLLT devices usually deliver less than 1 J/cm2 of fluence (light energy per area at the surface) at the skin’s surface [39]. But due to losses in the epidermis, around 95% of the incident irradiance does not reach 2 mm depth [40]. When some laser cap manufacturers tried to increase light power, and thus fluence, in order to increase effectiveness, it led to adverse events, such as burns, itchiness, and hair shedding, which resulted in warning letters from the US FDA [39].
As the effects of photobiomodulation are independent of temperature increase, it is neither necessary nor desirable to use excessively high temperatures that could cause epidermal damage. Moreover, the use of excessive energies could result in a suppressive effect due to the hormetic behavior of photobiomodulation. Safely increasing the effectiveness of photobiomodulation treatments is essential in order to improve hair regrowth results.
3.2. Alternative Forms of Laser Hair Therapy
Although LLLT remains the only type of light and laser therapy that has been approved as a treatment for AGA, other light and laser therapies are being assessed in clinical trials and used privately in dermatological clinics. The clinical studies have reported a number of positive improvements on skin and hair, with a handful of case studies reporting unique secondary effects, such as melanogenesis.
3.2.1. Fractional Lasers
Multiple fractional lasers have been used to treat AGA, including 1550 nm fractional erbium–glass lasers, fractional CO2 lasers, Er/YAG fractional lasers, and fractional thulium lasers [41]. When used properly, fractional lasers are ablative, but cause minimal damage. They strike a happy medium between nonablative and ablative lasers, acting only on the stratum corneum, the outermost segment of the skin’s surface, and causing microtrauma. However, fractional lasers can cause thermal damage zones within skin that can kill some hair follicles and damage some of the surrounding tissue [42]. The microscopic injuries induced by fractional lasers can trigger a wound healing environment that stimulates a regenerative wound healing process, activates hair follicle cells, and results in hair growth. Simultaneously, the microtrauma specific to the stratum corneum allows for the enhanced transdermal delivery of drugs and topical nutraceuticals to the scalp’s hair follicles [43].
Fractional lasers are currently used for a number of dermatological purposes, including the treatment of pigmentation-related issues, scars, and wrinkles [44,45,46]. They are also being explored as solutions for the treatment of other types of hair loss, including scarring alopecia [47]. More recently, there has been increased interest in the use of fractional ablative lasers to facilitate the delivery of topical treatments (i.e., laser-assisted drug delivery), such as minoxidil, platelet-rich plasma, and various growth factors, thereby enhancing their penetration and efficacy [43,48,49]. However, fractional lasers have not been yet approved as treatments for any type of alopecia, and it is likely that their role in the treatment of alopecia will evolve as a complement to enhance the administration and efficacy of the standard treatments [42].
3.2.2. Nonablative Lasers
Unlike fractional lasers and ablative lasers, nonablative lasers do not intentionally damage any component of the skin. However, nonablative lasers still deliver heat, unlike FDA-cleared LLLT for the treatment of AGA (that is sometimes referred to as a “cold laser”). A variety of nonablative lasers are used in dermatology, but erbium–glass (Er/G) is the primary nonablative option used in the treatment of AGA. Er/YAG lasers have also shown promise in the treatment of this form of hair loss [41,50].
The nonablative laser uses light that is absorbed in the most superficial layer of the skin, while releasing heat that diffuses into the skin’s deeper layers. The heat penetrates up to 0.5 mm through the skin, triggering paracrine signaling, activating fibroblasts, and prompting a regenerative response. This treatment can be used as an AGA monotherapy for men and women. Recently, ten Er/G treatments on a small group of women with AGA showed an improvement of 57 total hairs/cm2 after 5 months [38]. Nonablative Er/G and Er/YAG treatments have also been used in conjunction with platelet-rich plasma therapy, minoxidil, and oral supplements [41,50].
3.2.3. Blue and Yellow LLLT
Photobiomodulation using blue light and yellow light have also been used in the treatment of AGA. Blue light, which is typically administered at wavelengths between 380 nm and 460 nm, is typically used for the management of cutaneous diseases and wound healing. It has also been reported to have anti-inflammatory and antimicrobial effects when applied to skin [51]. At 453 nm, blue light has been shown to stimulate the cryptochrome (CRY)-1 protein in keratinocyte cells, which helps regulate hair follicle cell proliferation and the maintenance of the anagen phase of the hair growth cycle [52].
Recently, a 10-week study administering blue LED light (at 417 ± 10 nm with a fluence of 120 J/cm2 and power intensity of 60 mW/cm2 ± 20%) reported an increase in 90% of their patients’ hair density and hair shaft diameters. The treatments in this study were performed twice a week, as shown in Table 1. Notably, the study also reported the darkening of 30% of the participants’ hair [37].
Blue light has also been used in combination with red light as part of a treatment regimen for skin issues like acne and to restore hair growth. When treating acne, the combination of blue and red light has been shown to reduce inflammatory and non-inflammatory acne, decrease the size of the sebaceous gland, and consequently reducing sebum output [53]. When used for hair loss, blue light has also been used in combination with red light, along with microneedling and growth, in non-responders to finasteride. In this study, blue light (423 nm) was specifically thought to reduce scalp sebaceous glands and scalp fat and activate keratin in hair shafts. While this study was successful in improving hair regrowth, it combined too many variables to be able to attribute any specific improvements to the inclusion of blue photobiomodulation [54].
Compared to other colors of light used in photobiomodulation, yellow light is used sparingly. However, one recent study utilized a combination of dissolvable microneedle patches containing exosomes and yellow light irradiation (intended to reduce inflammation) to improve hair regrowth. Although this is the first study to report the use of yellow light photobiomodulation for this purpose, it may indicate that there is the potential for this form of light therapy to be useful in the treatment of alopecia [55].
3.3. Pulsed Electromagnetic Field Therapy (PEMF)
Pulsed electromagnetic field therapy (PEMF) devices are well-established tools for bone healing, wound healing, and pain relief, with the earliest devices dating back to the 1950s. PEMF is also known to have a positive effect on skin and hair cells and has been shown to promote hair regrowth. Electromagnetic fields are known to open calcium channels and facilitate the entrance of calcium ions. This mechanism of action is thought to be the fundamental principle behind all the PEMF devices used in regenerative medicine. The modulation of ion channels in this manner prompts cell differentiation and communication, as has been shown on dermal papilla mesenchymal cells in vitro due to increased MAP2 or Nestin gene expression [56]. PEMF also directly stimulates the drivers of hair restoration, promoting hair shaft growth and increasing hair length. It works by upregulating enzymes and increasing expression of cytokines and proteins, particularly those involved in the Wnt/β-catenin signaling pathway [57].
In vivo, PEMF encourages hair follicle regrowth, accelerates the hair growth rate, and can even promote hair follicle regeneration. Epidermal stem cells and dermal papilla cells were injected into the epidermis of mice, and their skin was then exposed to electromagnetic fields, facilitating the induction of hair follicle regeneration. The combined treatment specifically resulted in a higher density of hair follicles, implying that PEMF would complement hair transplants and other regenerative biological therapeutics for hair loss, such as exosomes, growth factors, stem cell, and platelet-rich plasma treatments [58,59].
However, the mechanism of action of PEMF in relation to AGA is likely quite complex, as it is also known to reduce the stressors, modulate inflammation, and indirectly balance hormone production and the melatonin levels in the neuroendocrine system. All four of these major factors have been implicated in the progression and exacerbation of AGA [31,60,61,62,63,64]. The observed effects of PEMF on such a wide range of body systems is presumably due to the fact that the cell membrane is the main target for PEMF signals. However, even the well-established anti-inflammatory effect of PEMF arises from a mechanism of action that has yet to be fully elucidated, and is currently believed to be partially due to PEMF’s ability to stabilize membranes and restore faulty Ca2+ ATPase and intracellular Ca2+ levels, inhibiting prostaglandin E2 biosynthesis [60].
3.3.1. PEMF Treatments for AGA
The pioneering work that led to the use of electrical fields to treat AGA was inspired by an anecdotal report of hair regrowth following transcutaneous electrical neural stimulation (TENS). The TENS device reduced hair shedding and improved the hair texture and hair growth rate in four men. In the 1980s, another two studies showed that PEMF could also counteract hair loss, with 84% of a group of 25 subjects and 70% of a group of 40 subjects showing improvements in hair regrowth after using an early version of a PEMF device [35].
Maddin et al. pioneered the first two formal studies of PEMF for hair loss in the 1990s. Their success set the stage for the use of PEMF as a treatment for AGA. In his first study, Maddin reported an increase of 7 terminal hairs/cm2 vs. the control group increase of 2 hairs/cm2 after 24 weeks, and an increase of 12 terminal hairs/cm2 after 36 weeks vs. the control group increase of 6 terminal hairs/cm2, as shown in Table 1. This was equivalent to an increase in the terminal hair count of over 66% after 36 weeks of treatment compared to the control group’s increase of 26%. Notably, 83% of the subjects saw an increase in hair growth, while 97% exhibited regrowth or no further hair loss [35].
The longitudinal data for a part of the same study group were reported in a second extension study, which found that terminal hair counts continued to increase to 19 terminal hairs/cm2 at 52 weeks and 38 terminal hairs/cm2 at 70 weeks. This showed that PEMF was able to produce continuous improvement in hair regrowth, even after more than a year of treatment [35,36].
3.3.2. Multimodal PEMF Treatments for AGA
Since the 1990s, AGA in males and females has been treated using PEMF, but only in combination with another treatment. Bureau et al. used PEMF in combination with essential plant oils administered over 26 weeks. A total of 83% of the treatment group exhibited a decrease in hair loss, while 53% of patients had an increase in hair count of 20% or more. The combination of their topical solution with PEMF resulted in an increase of 34 total hairs/cm2 compared to 9 hairs/cm2 in the control group, which used a placebo nutraceutical with anti-inflammatory properties and a sham PEMF device [34].
More recently, Choi and Park combined LLLT and PEMF over a 24-week period to treat androgenetic alopecia in men and women. The use of PEMF with LLLT resulted in an increase of 25 total hairs/cm2 vs. 6.5 total hairs/cm2 in the sham device control. The side effects were limited to minor issues, such as itching, burning, redness, and irritation [33].
Despite overwhelmingly positive results, the data on the use of PEMF as a treatment for AGA are still limited. To date, less than half a dozen papers have been published studying PEMF as a hair loss treatment. An established mechanism of action, defined parameters, recommended treatment regimens, and longitudinal data are lacking.
3.4. Microneedling
Microneedling is a minimally invasive procedure that is often used for cosmetic and aesthetic dermatological indications, such as the removal or minimization of acne scars, wrinkles around the eyes and mouth, skin laxity, scars from burns or trauma, and stretch marks. More recently, it has also been used as both a monotherapy and adjunct hair loss treatment as it can contribute to the induction of new hair growth cycles and the production of new hair strands. The wound healing cascade that it triggers increases blood flow and releases growth factors that help create a conducive environment for hair regeneration. Microneedling for hair loss involves the use of multiple fine needles, usually in the form of a dermaroller or dermapen-type device, to create small punctures on the scalp. These microtraumas, which are usually generated within the upper layers of skin specifically, the epidermis and dermis stimulate the body’s natural wound healing process [32,65,66,67,68,69,70,71].
Microneedling triggers increased blood flow to the affected areas, enabling additional nutrients and oxygen to reach hair follicles and promoting healthy hair growth. The increase in blood flow also stimulates dermal papilla and hair follicle stem cells, encouraging them to produce new hair cells and activating the release of various growth factors involved in the healing process, including platelet-derived, epidermal, and vascular endothelial growth factors. These growth factors are essential for the regeneration of new skin cells, the formation of collagen and other connective tissue components, the formation of blood vessels, the development of new hair follicles, and the production of hair from existing follicles. This, in turn, yields visible improvements in hair quality, density, and thickness [65,66,67,68,69,70,71].
Microneedling is also believed to work by activating cellular regeneration via genetic signaling, including the VEGF and Wnt/β-catenin signaling pathways, leading to angiogenesis, collagen induction, tissue rejuvenation, and follicular vascularization. Hair follicle neogenesis has also been shown to occur via the Wnt signaling pathway following wounding and wound healing. Wnt/β-Catenin signaling is important for hair follicle regeneration, hair shaft growth, and the initiation and maintenance of hair morphogenesis. Microneedling can produce modest improvements in hair growth when used as a monotherapy. However, when used as an adjunct hair loss treatment, it can produce much greater improvements in hair regrowth [32,65,66,67,68,69,70,71].
3.4.1. Microneedling as an Adjunct Treatment
In clinics, microneedling is rarely used as a monotherapy to treat androgenetic alopecia. Instead, it is more often used as an adjuvant therapy and combined with topical medications, like minoxidil or other topical hair loss products. The microchannels created through microneedling are believed to improve the transdermal penetration of these topicals, allowing for higher concentrations to reach the vascularized dermis directly, and therefore increasing their effectiveness, for example, in the case of non-responders to FDA-approved treatments such as minoxidil and finasteride. Between 50 and 75% of non-responders to 5% minoxidil and oral finasteride have achieved improvements in hair regrowth after adding microneedling to their hair loss treatment routines [72].
Most notable example of improved effectiveness has been a comparative study of 100 men with androgenetic alopecia that were split into two groups. The first group received the standard FDA-approved minoxidil treatment, while the second received minoxidil along with microneedling. The addition of microneedling resulted in an increased hair count of 91.4 follicles per cm2 compared to that in the minoxidil monotherapy group, whose hair count increased by just 22.2 follicles per cm2 [32]. While the results involving the addition of microneedling always show an improvement, they are not always as dramatic. A similar study assessing minoxidil and the combination of minoxidil and microneedling showed an increased hair count of 12.82 hairs per cm2 in the minoxidil and microneedling group, compared to an increase of 1.89 ± 8.94 in the group using minoxidil on its own [73].
Microneedling has also been shown to help improve healthy hair growth in other studies. A study involving three treatment groups—minoxidil, minoxidil plus platelet-rich plasma treatments, and minoxidil, platelet-rich plasma treatments and microneedling—found that hair strength was best in the tri-therapy-treated men, followed by those who had received the di-therapy. Nearly twice as many men (87.1%) who received the tri-therapy treatment retained hair following a hair pull test compared to those who received minoxidil monotherapy (48.4%) [67]. To date, no microneedling device has obtained clearance for the treatment of hair loss. While over a dozen microneedling devices have been cleared for use by the FDA, all of them have been cleared for cosmetic dermatological uses, such as wrinkle and scar reduction.
3.4.2. Delivering LLLT via Microneedling
Maintaining the safety profile of an LLLT-based hair loss treatment, while improving effectiveness, would substantially impact the hair loss treatment industry, particularly given the large number of non-responders to current FDA-approved solutions. The primary challenge of this technique is the need to deliver enough energy to the dermis to achieve an effect, often thermal, without causing severe disruption that could lead to burns. Several researchers have demonstrated how the blood vessels taken from animal models could be dilated using delivery of light in the red spectrum (from 630 to 700 nm wavelength). The light fluences shown to be most effective for dilation ranged from 5 to 10 J/cm2 when irradiated directly on the vessel surface [74,75,76].
It is possible to bypass the skin’s barrier in a controlled fashion. One can create a hole or another type of opening through surgery, or create many holes simultaneously in a minimally invasive manner via microneedling. Combining lasers with a technique such as microneedling would allow light to bypass the skin’s barrier in a controlled manner that can be used to deliver stimulation therapies.
Based on prior optical simulations, only 5% of the light applied to the skin’s surface reached a depth of 2 mm, where the majority of blood vessels and capillaries of the hair follicles reside. Approximately 90% of light loss typically occurs in the epidermis due to the skin’s melanin layer, found less than 500 μm deep [40]. However, inserting a light source into the skin by as little as 500 microns can increase light delivery by an order of magnitude or more, specifically, the desired 2 mm depth. This is the premise of a novel device for AGA developed using the concept of precision LLLT, which is currently being tested in clinical trials [77].
Combining microneedling devices and topical minoxidil has shown success [72]. Precision LLLT utilizes a novel approach to photobiomodulation delivery, which is intended to reproduce the success of combining minoxidil with microneedling without the use of pharmaceuticals. This concept applied using the SAGA-001 device combines microneedling and laser light delivery for hair growth. This device uses lasers injected into the skin’s dermis to increase light penetration and the effectiveness of LLLT treatments. Microneedling utilizes mechanical damage to induce a wound healing effect, while LLLT utilizes red to near-infared light to stimulate vascular dilation, cell proliferation, and regeneration [78,79]. The SAGA device pierces through the epidermis using novel optical microneedles that bypass the melanin layer in order to safely and efficiently deliver more energy to the hair follicle, as shown in Figure 3. Red, pulsed lasers are used to deliver the maximum amount of stimulatory energy without causing photothermal damage, remaining a safer, purely photostimulatory regime [77].
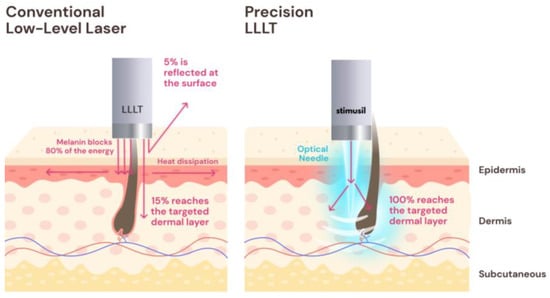
Figure 3.
Skin penetrance using a conventional LLLT device versus precision LLLT.
In mid-2023, StimuSIL initiated a pivotal human study testing two versions of the SAGA-001 device on men with androgenetic alopecia. The participants are males aged from 22 to 55 years old with Hamilton–Norwood stage IIa-V hair loss and Fitzpatrick Skin Types I-IV. The study aims to confirm the safety and effectiveness of two versions of the SAGA-001 device in treating male pattern hair loss. Unlike most hair loss treatments that require the users to apply or take medications daily, or use devices multiple times a week, SAGA-001 treatments are only required every two weeks. This means that participants in this 24-week clinical trial receive a total of 12 treatments. The study will quantify results by assessing changes in terminal hair density and hair thickness at 16 and 24 weeks through use of global and macro photography [77].
4. Discussion
Physical therapies seem to be promising treatments for AGA, with various options available for individuals to use at home as well as in clinical settings, as summarized in Figure 4. These treatments all work directly on the hair follicle, producing improvements with a low risk of side effects. In fact, these physical therapies act across the same pathways, simply taking effect at different stages, as shown in Figure 5.
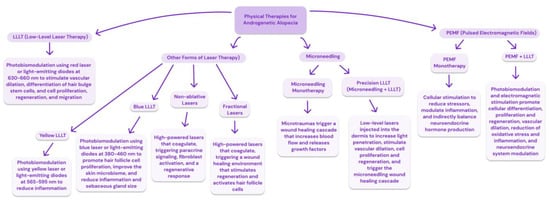
Figure 4.
A summary of physical therapies available for the treatment of androgenetic alopecia.
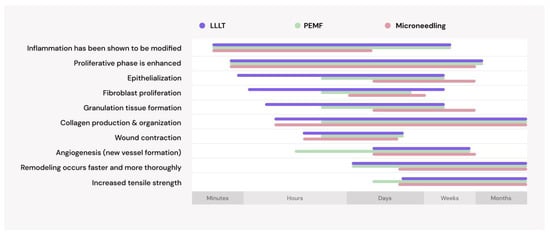
Figure 5.
Similar pathways are activated after administering LLLT [80,81,82,83,84,85,86,87,88,89,90,91], PEMF [92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114], and microneedling [31,32,48,49,115,116,117].
Photobiomodulation, especially LLLT, has been widely studied for its beneficial effects on wound healing and its ability to increase the production of ATP, ROS, and NO, which are essential for cellular energy, signaling, and vascular functions, respectively. LLLT helps modulate the inflammatory response, reducing the duration and intensity of inflammation, thus creating a more conducive environment for healing. LLLT also supports a number of proliferative activities, stimulating fibroblast proliferation, granulation tissue formation, collagen production, epithelialization, and remodeling, which significantly accelerate the healing process. These beneficial effects are not necessarily limited to the wound itself, as LLLT may produce effects distant from the immediately treated area [80,81,82,83,84,85,86,87,88,89,90,91].
While it is less well studied, Figure 5 shows that PEMF has very similar mechanisms of action and works along the same pathways as LLLT. Like LLLT, PEMF has been shown to modulate inflammatory responses, promote proliferative activities, enhance cellular metabolism, improve blood flow, and encourage the release of growth factors and cytokines necessary for wound healing [92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114]. Microneedling induces controlled microtrauma, directly implicating it in the wound itself. However, by initiating an intentional inflammatory response, it sets the stage for subsequent healing that ultimately use the same mechanisms of action as LLLT and PEMF [31,32,48,49,115,116,117].
As the only physical therapy cleared for the treatment of AGA by the US FDA, the vast majority of the literature on physical treatments for this type of hair loss focuses on red low-level light therapy. However, there is a notable and substantial amount of variability reported in LLLT study parameters, which range from 8-min treatments three times per week to 18-min treatments once a day. Notably, the 8-min treatments using the HairMax Laser Comb showed an increase of 26 terminal hairs/cm2 after 26 weeks compared to an increase of 6 total hairs/cm2 after 24 weeks using the Restore ID-520 for 30 min, three times per week [24,25]. This dose-dependent response is indicative of hormesis and may be relevant to consider for all the physical therapies, given that they involve similar regenerative pathways, as shown in Figure 5.
To date, the only available options for home-use physical treatments are LLLT devices, which are available as comb/brush or cap/helmet type devices [21]. These products have been proven as safe and effective tools for the treatment of hair loss. There are currently no FDA-approved blue or yellow LLLT devices, and all the other forms of laser hair therapy must be administered in a clinical setting. The studies on these alternative forms of laser hair therapy remain very limited. However, of note is the Er/G laser, which reported an increase of 57 total hairs/cm2 after 20 weeks of treatment (10 treatment sessions) [38]. This study applied significantly fewer treatments and attained approximately 3–4 times as much hair growth compared to what has been reported by some LLLT studies. It will be of great interest to see if further studies exploring the use of nonablative lasers for hair loss will be able to produce comparable results.
A wide variety of microneedling devices are sold over the counter and can be used by individuals at home. However, microneedling treatments for hair loss are generally the most successful and have a much lower risk when performed in a sterile clinical setting. Furthermore, this physical therapy is best used as an adjunct treatment. It is still unknown how effective combining microneedling with most other physical therapies would be. The first study of this kind, combining microneedling with LLLT, is still in clinical trials [77].
Thus far, the studies exploring PEMF as a treatment for AGA have been minimal. However, the limited research on this subject shown in Table 1 indicates that PEMF may very well produce results that are comparable with LLLT. In fact, PEMF may very well have the potential to be a superior hair loss treatment as, when used as a monotherapy, the reported increases in terminal hair growth are comparable to the improvements in total hair growth reported in some LLLT studies [35,36]. Multimodal approaches reporting improvements in total hair growth indicate that the addition of PEMF produces enhanced outcomes [33,34], implying that there may be a synergistic effect or a novel mechanism of action on the hair follicle. Notably, the administered treatments listed in Table 1 utilize devices that are only appropriate for use in clinical settings. However, given the array of other indications safely utilizing PEMF, it will be interesting to see if future research utilizes devices for AGA that can be implemented in home-use settings.
5. Conclusions
Several physical treatments show promise for the management of AGA. In particular, low-level laser therapy demonstrates significant potential due to the photobiomodulation effects on mitochondria, which can enhance cellular energy production and potentially stimulate hair growth. The other light sources, including fractional and nonablative lasers, as well as blue and yellow light therapies, offer a range of options that are becoming increasingly popular treatment options for AGA, particularly as adjunct treatments for individuals who are non-responsive to FDA-approved solutions.
Pulsed electromagnetic field therapy is another modality that has been explored for AGA, with the studies indicating its efficacy not only as a standalone treatment, but also in combination with other therapies. Multimodal approaches that include PEMF have shown enhanced outcomes, implying a synergistic effect or a novel mechanism of action affecting the hair follicle, which should be explored further in future research.
Microneedling is primarily recognized for its adjunctive role in the treatment of AGA. By creating micro-injuries to the skin, microneedling facilitates the deeper penetration of other hair loss therapies, potentially increasing their effectiveness. The integration of LLLT delivery via microneedling devices is a novel approach that combines the mechanical and photonic stimulation of hair follicle stem cells, which could revolutionize the treatment protocols.
The benefits and efficacy of multimodal physical treatments for AGA is of great interest as the side effects of these devices are minimal, making their combined potential both highly effective and low-risk. Future research should focus on optimizing treatment parameters, exploring the synergistic effects of multimodal approaches, and establishing long-term efficacy and safety profiles for these physical therapies. It is crucial for the upcoming studies to continue to explore these combinations in clinical settings, with a focus on identifying treatment parameters that maximize patient outcomes. Once the protocols using these minimally invasive, non-pharmacological treatments are optimized, they will provide substantial relief to those suffering from AGA, enhancing both hair growth and quality of life for affected individuals.
Author Contributions
All authors made substantial contributions to the conception, acquisition, analysis, and/or interpretation of data. They all participated in drafting the article or revising it critically for important intellectual content. Furthermore, all authors consented to submit to the current journal, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by StimuSIL., Inc.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
The data generated and analyzed during this study are included in this published article.
Conflicts of Interest
Dr. Siddhi Bianca Camila Lama and Dr. Mehmet Kosoglu are collaborators of StimuSIL, Inc. Dr. Robert Dennis, licenses technology to StimuSIL, Inc. The remaining authors declare no conflicts of interest. The funders commissioned this study and supported the publication of the results.
References
- Ho, C.H.; Sood, T.; Zito, P.M. Androgenetic Alopecia. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Nestor, M.S.; Ablon, G.; Gade, A.; Han, H.; Fischer, D.L. Treatment options for androgenetic alopecia: Efficacy, side effects, compliance, financial considerations, and ethics. J. Cosmet. Dermatol. 2021, 20, 3759–3781. [Google Scholar] [CrossRef] [PubMed]
- Badri, T.; Nessel, T.A.; Kumar, D.D. Minoxidil. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Choi, M.C.; Cheung, K.K.; Li, X.; Cheing, G.L.Y. Pulsed electromagnetic field (PEMF) promotes collagen fibre deposition associated with increased myofibroblast population in the early healing phase of diabetic wound. Arch. Dermatol. Res. 2016, 308, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Andy, G.; John, M.C.; Mirna, S.; Rachita, D.; Michael, K.; Maja, K.; Aseem, S.; Zeljana, B. Controversies in the treatment of androgenetic alopecia: The history of finasteride. Dermatol. Ther. 2019, 32, e12647. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.; Cantisani, C.; Melis, L.; Iorio, A.; Scali, E.; Calvieri, S. Minoxidil Use in Dermatology, Side Effects and Recent Patents. Recent Pat. Inflamm. Allergy Drug Discov. 2012, 6, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Suchonwanit, P.; Thammarucha, S.; Leerunyakul, K. Minoxidil and its use in hair disorders: A review. Drug Des. Dev. Ther. 2019, 13, 2777–2786. [Google Scholar] [CrossRef] [PubMed]
- Birch, M.P.; Messenger, J.F.; Messenger, A.G. Hair density, hair diameter and the prevalence of female pattern hair loss. Br. J. Dermatol. 2001, 144, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Olsen, E.A.; Messenger, A.G.; Shapiro, J.; Bergfeld, W.F.; Hordinsky, M.K.; Roberts, J.L.; Stough, D.; Washenik, K.; Whiting, D.A. Evaluation and treatment of male and female pattern hair loss. J. Am. Acad. Dermatol. 2005, 52, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Austin, E.; Geisler, A.N.; Nguyen, J.; Kohli, I.; Hamzavi, I.; Lim, H.W.; Jagdeo, J. Visible light. Part I: Properties and cutaneous effects of visible light. J. Am. Acad. Dermatol. 2021, 84, 1219–1231. [Google Scholar] [CrossRef] [PubMed]
- Avci, P.; Gupta, A.; Sadasivam, M.; Vecchio, D.; Pam, Z.; Pam, N.; Hamblin, M.R. Low-level laser (light) therapy (LLLT) in skin: Stimulating, healing, restoring. Semin. Cutan. Med. Surg. 2013, 32, 41–52. [Google Scholar]
- Glass, G.E. Photobiomodulation: A review of the molecular evidence for low level light therapy. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 1050–1060. [Google Scholar] [CrossRef]
- Glass, G.E. Photobiomodulation: The Clinical Applications of Low-Level Light Therapy. Aesthet. Surg. J. 2021, 41, 723–738. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Qu, Q.; Chen, J.; Miao, Y.; Hu, Z. Proposed mechanisms of low-level light therapy in the treatment of androgenetic alopecia. Lasers Med. Sci. 2021, 36, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Hamblin, M.R. Photobiomodulation for the management of alopecia: Mechanisms of action, patient selection and perspectives. Clin. Cosmet. Investig. Dermatol. 2019, 12, 669–678. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.-H.; Liu, D.; Chen, Y.-T.; Chin, S.-Y. Comparative effectiveness of low-level laser therapy for adult androgenic alopecia: A system review and meta-analysis of randomized controlled trials. Lasers Med. Sci. 2019, 34, 1063–1069. [Google Scholar] [CrossRef] [PubMed]
- Dompe, C.; Moncrieff, L.; Matys, J.; Grzech-Leśniak, K.; Kocherova, I.; Bryja, A.; Bruska, M.; Dominiak, M.; Mozdziak, P.; Skiba, T.H.I.; et al. Photobiomodulation—Underlying Mechanism and Clinical Applications. J. Clin. Med. 2020, 9, 1724. [Google Scholar] [CrossRef] [PubMed]
- Gentile, P.; Garcovich, S. The Effectiveness of Low-Level Light/Laser Therapy on Hair Loss. Facial Plast. Surg. Aesthet. Med. 2021, 26, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Munck, A.; Gavazzoni, M.F.; Trüeb, R.M. Use of low-level laser therapy as monotherapy or concomitant therapy for male and female androgenetic alopecia. Int. J. Trichol. 2014, 6, 45–49. [Google Scholar] [PubMed]
- Egger, A.; Resnik, S.R.; Aickara, D.; Maranda, E.; Kaiser, M.; Wikramanayake, T.C.; Jimenez, J.J. Examining the safety and efficacy of low-level laser therapy for male and female pattern hair loss: A review of the literature. Ski. Appendage Disord. 2020, 6, 259–267. [Google Scholar] [CrossRef]
- Galadari, H.; Shivakumar, S.; Lotti, T.; Wollina, U.; Goren, A.; Rokni, G.R.; Grabbe, S.; Goldust, M. Low-level laser therapy and narrative review of other treatment modalities in androgenetic alopecia. Lasers Med. Sci. 2020, 35, 1239–1244. [Google Scholar] [CrossRef]
- Leavitt, M.; Charles, G.; Heyman, E.; Michaels, D. HairMaxLaserComb laser phototherapy device in the treatment of male androgenetic alopecia: A randomized, double-blind, sham device-controlled, multicentre trial. Clin. Drug Investig. 2009, 29, 283–292. [Google Scholar] [CrossRef]
- Kim, H.; Choi, J.W.; Kim, J.Y.; Shin, J.W.; Lee, S.J.; Huh, C.H. Low-level light therapy for androgenetic alopecia: A 24-week, randomized double-blind, sham device-controlled multicenter trial. Dermatol. Surg. 2013, 39, 1177–1183. [Google Scholar] [CrossRef]
- Jimenez, J.J.; Wikramanayake, T.C.; Bergfeld, W.; Hordinsky, M.; Hickman, J.G.; Hamblin, M.R.; Schachner, L.A. Efficacy and safety of a low-level laser device in the treatment of male and female pattern hair loss: A multicenter, randomized, sham device-controlled, double-blind study. Am. J. Clin. Dermatol. 2014, 15, 115–127. [Google Scholar] [CrossRef] [PubMed]
- Fan, S.M.Y.; Cheng, Y.-P.; Lee, M.-Y.; Lin, S.-J.; Chiu, H.-Y. Efficacy and safety of a low-level light therapy for androgenetic alopecia: A 24-week, randomized, double-blind, self-comparison, sham device-controlled trial. Dermatol. Surg. 2018, 44, 1411–1420. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.S.; Park, M.W.; Lee, C.J. Phototherapy of Androgenetic Alopecia with Low Level Narrow Band 655-nm Red Light and 780-nm Infrared Light. J. Am. Acad. Dermatol. 2007, 56, AB112. [Google Scholar]
- Satino, J.L.; Markou, M. Hair regrowth and increased hair tensile strength using the HairMaxLaserComb for low-level laser therapy. Int. J. Cos. Surg. Aest. Dermatol. 2003, 5, 113–117. [Google Scholar] [CrossRef]
- Lanzafame, R.J.; Blanche, R.R.; Bodian, A.B.; Chiacchierini, R.P.; Fernandez-Obregon, A.; Kazmirek, E.R. The growth of human scalp hair mediated by visible red light laser and LED sources in males. Lasers Surg. Med. 2013, 45, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Avram, M.R.; Rogers, N.E. The use of low-level light for hair growth: Part I. J. Cosmet. Laser Ther. 2009, 11, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Esmat, S.M.; Hegazy, R.A.; Gawdat, H.I.; Hay, R.M.A.; Allam, R.S.; El Naggar, R.; Moneib, H. Low level light-minoxidil 5% combination versus either therapeutic modality alone in management of female patterned hair loss: A randomized controlled study. Lasers Surg. Med. 2017, 49, 835–843. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.K.; Inamadar, A.C.; Palit, A. A randomized controlled, single-observer blinded study to determine the efficacy of topical minoxidil plus microneedling versus topical minoxidil alone in the treatment of androgenetic alopecia. J. Cutan. Aesthet. Surg. 2018, 11, 211–216. [Google Scholar] [PubMed]
- Dhurat, R.; Sukesh, M.; Avhad, G.; Dandale, A.; Pal, A.; Pund, P. A randomized evaluator blinded study of effect of microneedling in androgenetic alopecia: A pilot study. Int. J. Trichol. 2013, 5, 6–11. [Google Scholar] [CrossRef]
- Choi, M.S.; Park, B.C. The efficacy and safety of the combination of photobiomodulation therapy and pulsed electromagnetic field therapy on androgenetic alopecia. J. Cosmet. Dermatol. 2023, 22, 831–836. [Google Scholar] [CrossRef] [PubMed]
- Bureau, J.P.; Guilbaud, J.; Roux, F.M.E. Essential Oils and Low-Intensity Electromagnetic Pulses in the Treatment of Andro-gen-Dependent Alopecia. Adv. Ther. 2003, 20, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Maddin, W.S.; Bell, P.W.; James, J.H.M. The Biological Effects of a Pulsed Electrostatic Field with Specific Reference to Hair Electrotrichogenesis. Int. J. Dermatol. 1990, 29, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Maddin, W.S.; Amara, I.; Sollecito, W.A. Electrotrichogenesis: Further evidence of efficacy and safety on extended use. Int. J. Dermatol. 1992, 31, 878–880. [Google Scholar] [CrossRef] [PubMed]
- Lodi, G.; Sannino, M.; Cannarozzo, G.; Giudice, A.; Del Duca, E.; Tamburi, F.; Bennardo, L.; Nisticò, S.P. Blue light-emitting diodes in hair regrowth: The first prospective study. Lasers Med. Sci. 2021, 36, 1719–1723. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.Y.; Lee, S.J.; Kim, W.S. The effect of a 1550 nm fractional erbium–glass laser in female pattern hair loss. J. Eur. Acad. Dermatol. Venereol. 2011, 25, 1450–1454. [Google Scholar] [CrossRef] [PubMed]
- U.S. Food and Drug Administration. Warning Letter to Transdermal Cap Inc. 2015. Available online: https://web.archive.org/web/20190424174411/https://www.fda.gov/ICECI/EnforcementActions/WarningLetters/2015/ucm458008.htm (accessed on 12 April 2024).
- Ash, C.; Dubec, M.; Donne, K.; Bashford, T. Effect of wavelength and beam width on penetration in light-tissue interaction using computational methods. Lasers Med. Sci. 2017, 32, 1909–1918. [Google Scholar] [CrossRef] [PubMed]
- Jedlowski, P.M.; Anthony, M. Use of fractionated laser therapy for the treatment of androgenetic alopecia: A systematic review and meta-analysis. Lasers Med. Sci. 2023, 39, 4. [Google Scholar] [CrossRef] [PubMed]
- Dabek, R.J.; Austen, W.G.; Bojovic, B. Laser-assisted Hair Regrowth: Fractional Laser Modalities for the Treatment of Androgenic Alopecia. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2157. [Google Scholar] [CrossRef]
- Balazic, E.; Muskat, A.; Kost, Y.; Cohen, J.L.; Kobets, K. The role of laser and energy-assisted drug delivery in the treatment of alopecia. Lasers Med. Sci. 2024, 39, 73. [Google Scholar] [CrossRef]
- Bernabe, R.M.; Choe, D.; Calero, T.; Lin, J.; Pham, C.; Dang, J.; Madrigal, P.; Yenikomshian, H.A.; Gillenwater, T.J. Laser-Assisted Drug Delivery in the Treatment of Hypertrophic Scars and Keloids: A Systematic Review. J. Burn Care Res. 2024, 45, 590–600. [Google Scholar] [CrossRef] [PubMed]
- Modena, D.A.; Miranda, A.C.; Grecco, C.; Liebano, R.E.; Cordeiro, R.C.; Guidi, R.M. Efficacy, safety, and guidelines of application of the fractional ablative laser erbium YAG 2940 nm and non-ablative laser erbium glass in rejuvenation, skin spots, and acne in different skin phototypes: A systematic review. Lasers Med. Sci. 2020, 35, 1877–1888. [Google Scholar] [CrossRef] [PubMed]
- Nobari, N.N.; Tabavar, A.; Sadeghi, S.; Dehghani, A.; Kalantari, Y.; Ghassemi, M.; Atefi, N.; Goodarzi, A. A systematic review of the comparison between needling (RF-needling, meso-needling, and micro-needling) and ablative fractional lasers (CO2, erbium YAG) in the treatment of atrophic and hypertrophic scars. Lasers Med. Sci. 2023, 38, 67. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Choi, M.J.; Zheng, Z.; Goo, B.; Kim, D.Y.; Cho, S.B. Clinical effects of non-ablative and ablative fractional lasers on various hair disorders: A case series of 17 patients. J. Cosmet. Laser Ther. 2013, 15, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Abd ElKawy, F.A.E.W.; Aly, S.H.M.; Ibrahim, S.M.A. Fractional CO2 laser versus microneedling as a transepidermal drug delivery system for the treatment of alopecia areata: A clinical dermoscopic evaluation. Dermatol. Ther. 2022, 35, e15553. [Google Scholar] [CrossRef] [PubMed]
- Omar, M.M.; Obaid, Z.M.; Sayedahmed, O.M.E. Comparative study between topical application of triamcinolone acetonide after fractional carbon dioxide laser versus microneedling in the treatment of resistant alopecia areata. Dermatol. Ther. 2022, 35, e15913. [Google Scholar] [CrossRef] [PubMed]
- Day, D.; McCarthy, M.; Talaber, I. Non-ablative Er: YAG laser is an effective tool in the treatment arsenal of androgenetic alopecia. J. Cosmet. Dermatol. 2022, 21, 2056–2063. [Google Scholar] [CrossRef] [PubMed]
- Bayat, M.; Azari, A.; Golmohammadi, M.G. Effects of 780-nm low-level laser therapy with a pulsed gallium aluminum arsenide laser on the healing of a surgically induced open skin wound of rat. Photomed. Laser Surg. 2010, 28, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Buscone, S.; Mardaryev, A.N.; Westgate, G.E.; Uzunbajakava, N.E.; Botchkareva, N.V. Cryptochrome 1 is modulated by blue light in human keratinocytes and exerts positive impact on human hair growth. Exp. Dermatol. 2021, 30, 271–277. [Google Scholar] [CrossRef]
- Kwon, H.H.; Lee, J.B.; Yoon, J.Y.; Park, S.Y.; Ryu, H.H.; Park, B.M.; Kim, Y.J.; Suh, D.H. The clinical and histological effect of home-use, combination blue–red LED phototherapy for mild-to-moderate acne vulgaris in Korean patients: A double-blind, randomized controlled trial. Br. J. Dermatol. 2013, 168, 1088–1094. [Google Scholar] [CrossRef]
- Gentile, P.; Ki, M.-S. Hair Growth Booster Effects of Micro-Needling with Low-Level Led Therapy and Growth Factors on Subjects Treated with Finasteride®. Appl. Sci. 2022, 12, 9164. [Google Scholar] [CrossRef]
- Hong, C.; Zhang, G.; Zhang, W.; Liu, J.; Zhang, J.; Chen, Y.; Peng, H.; Cheng, Y.; Ding, X.; Xin, H.; et al. Hair grows hair: Dual-effective hair regrowth through a hair enhanced dissolvable microneedle patch cooperated with the pure yellow light irradiation. Appl. Mater. Today 2021, 25, 101188. [Google Scholar] [CrossRef]
- Moraveji, M.; Haghighipour, N.; Keshvari, H.; Abbariki, T.N.; Shokrgozar, M.A.; Amanzadeh, A. Effect of Extremely Low-Frequency Electromagnetic Field on MAP2 and Nestin Gene Expression of Hair Follicle Dermal Papilla Cells. Int. J. Artif. Organs 2016, 39, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.H.; Kim, Y.M.; Park, H.J.; Nam, M.H.; Seo, Y.K. Extremely Low-Frequency Electromagnetic Fields Increase Cytokines in Human Hair Follicles through Wnt/β-Catenin Signaling. Biomedicines 2022, 10, 924. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, X.; Bai, L.; Zhao, P.; Zhang, M. Exposure to 50 Hz electromagnetic fields enhances hair follicle regrowth in C57BL/6 mice. Exp. Biol. Med. 2019, 244, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Pan, Q.; Zhang, N.; Wang, B.; Yang, Z.; Ryaby, J.T.; Waldorff, E.I.; Lee, W.Y.W.; Li, G. A Novel Pulsed Electromagnetic Field Promotes Distraction Osteogenesis Via Enhancing Osteogenesis and Angiogenesis in a Rat Model. J. Orthop. Transl. 2020, 25, 87–95. [Google Scholar] [CrossRef]
- Selvam, R.; Ganesan, K.; Raju, K.N.; Gangadharan, A.C.; Manohar, B.M.; Puvanakrishnan, R. Low frequency and low intensity pulsed electromagnetic field exerts its antiinflammatory effect through restoration of plasma membrane calcium ATPase activity. Life Sci. 2007, 80, 2403–2410. [Google Scholar] [CrossRef] [PubMed]
- Hadshiew, I.M.; Foitzik, K.; Arck, P.C.; Paus, R. Burden of hair loss: Stress and the underestimated psychosocial impact of telogen effluvium and androgenetic alopecia. J. Investig. Dermatol. 2004, 123, 455–457. [Google Scholar] [CrossRef] [PubMed]
- Prie, B.E.; Iosif, L.; Tivig, I.; Stoian, I.; Giurcaneanu, C. Oxidative stress in androgenetic alopecia. J. Med. Life 2016, 9, 79–83. [Google Scholar]
- Lolli, F.; Pallotti, F.; Rossi, A.; Fortuna, M.C.; Caro, G.; Lenzi, A.; Sansone, A.; Lombardo, F. Androgenetic alopecia: A review. Endocrine 2017, 57, 9–17. [Google Scholar] [CrossRef]
- Heilmann-Heimbach, S.; Hochfeld, L.M.; Henne, S.K.; Nöthen, M.M. Hormonal regulation in male androgenetic alopecia—Sex hormones and beyond: Evidence from recent genetic studies. Exp. Dermatol. 2020, 29, 814–827. [Google Scholar] [CrossRef] [PubMed]
- Han, X.; Chang, L.; Qiu, Z.; Lin, M.; Wang, Y.; Liu, D.; Diao, Q.; Zhong, J.L.; Xu, W. Micro-Injury Induces Hair Regeneration and Vitiligo Repigmentation through Wnt/β-Catenin Pathway. Stem Cells Dev. 2022, 31, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Huang, P.; Yan, R.; Zhang, X.; Wang, L.; Ke, X.; Qu, Y. Activating Wnt/β-catenin signaling pathway for disease therapy: Challenges and opportunities. Pharmacol. Ther. 2019, 196, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Jha, A.K.; Vinay, K.; Zeeshan, M.; Roy, P.K.; Chaudhary, R.K.P.; Priya, A. Platelet-rich plasma and microneedling improves hair growth in patients of androgenetic alopecia when used as an adjuvant to minoxidil. J. Cosmet. Dermatol. 2019, 18, 1330–1335. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Tang, Y.; Huang, Y.; Wang, J.; Yang, K.; Zhang, Y.; Pu, W.; Liu, J.; Shi, X.; Ma, Y.; et al. Insights into male androgenetic alopecia using comparative transcriptome profiling: Hypoxia-inducible factor-1 and Wnt/β-catenin signalling pathways. Br. J. Dermatol. 2022, 187, 936–947. [Google Scholar] [CrossRef] [PubMed]
- Premanand, A.; Reena Rajkumari, B. Androgen modulation of Wnt/β-catenin signaling in androgenetic alopecia. Arch. Dermatol. Res. 2018, 310, 391–399. [Google Scholar] [CrossRef]
- Lu, G.Q.; Wu, Z.B.; Chu, X.Y.; Bi, Z.G.; Fan, W.X. An investigation of crosstalk between Wnt/β-catenin and transforming growth factor-β signaling in androgenetic alopecia. Medicine 2016, 95, e4297. [Google Scholar] [CrossRef]
- Tosti, A.; Zaiac, M.N.; Canazza, A.; Sanchis-Gomar, F.; Pareja-Galeano, H.; Alis, R.; Lucia, A.; Emanuele, E. Topical application of the Wnt/β-catenin activator methyl vanillate increases hair count and hair mass index in women with androgenetic alopecia. J. Cosmet. Dermatol. 2016, 15, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Bao, L.; Gong, L.; Guo, M.; Liu, T.; Shi, A.; Zong, H.; Xu, X.; Chen, H.; Gao, X.; Li, Y. Randomized trial of electrodynamic microneedle combined with 5% minoxidil topical solution for the treatment of Chinese male Androgenetic alopecia. J. Cosmet. Laser Ther. 2020, 22, 1–7. [Google Scholar] [CrossRef]
- Kumar, S.; Kesari, K.K.; Behari, J. The therapeutic effect of a pulsed electromagnetic field on the reproductive patterns of male Wistar rats exposed to a 2.45-GHz microwave field. Clinics 2011, 66, 1237–1245. [Google Scholar] [CrossRef]
- Keszler, A.; Lindemer, B.; Weihrauch, D.; Jones, D.; Hogg, N.; Lohr, N.L. Red/near infrared light stimulates release of an endothelium-dependent vasodilator and rescues vascular dysfunction in a diabetes model. Free Radic. Biol. Med. 2017, 113, 157–164, Erratum in Free Radic. Biol. Med. 2019, 131, 443. [Google Scholar] [CrossRef]
- Keszler, A.; Lindemer, B.; Broeckel, G.; Weihrauch, D.; Gao, Y.; Lohr, N.L. In Vivo Characterization of a Red Light-Activated Vasodilation: A Photobiomodulation Study. Front. Physiol. 2022, 13, 880158. [Google Scholar] [CrossRef] [PubMed]
- Weihrauch, D.; Keszler, A.; Broeckel, G.; Aranda, E.; Lindemer, B.; Lohr, N.L. Red light mediates the exocytosis of vasodilatory vesicles from cultured endothelial cells: A cellular, and ex vivo murine model. Photochem. Photobiol. Sci. 2024, 23, 355–364. [Google Scholar] [CrossRef] [PubMed]
- Assessing the Safety and Efficacy of a Novel Microneedling and Laser Device for Male Pattern Hair Loss (CS-SAGA-001). Available online: https://classic.clinicaltrials.gov/ct2/show/NCT05970809 (accessed on 1 April 2024).
- Weihrauch, D.; Keszler, A.; Lindemer, B.; Krolikowski, J.; Lohr, N.L. Red light stimulates vasodilation through extracellular vesicle trafficking. J. Photochem. Photobiol. B Biol. 2021, 220, 112212. [Google Scholar] [CrossRef]
- Wunsch, A.; Matuschka, K. A controlled trial to determine the efficacy of red and near-infrared light treatment in patient satisfaction, reduction of fine lines, wrinkles, skin roughness, and intradermal collagen density increase. Photomed. Laser Surg. 2014, 32, 93–100. [Google Scholar] [CrossRef]
- Jahangiri Noudeh, Y.; Shabani, M.; Vatankhah, N.; Hashemian, S.J.; Akbari, K. A combination of 670 and 810 nm diode lasers for wound healing acceleration in diabetic rats. Photomed. Laser Surg. 2010, 28, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Meirelles, G.C.; Santos, J.N.; Chagas, P.O.; Moura, A.P.; Pinheiro, A.L. A comparative study of the effects of laser photobiomodulation on the healing of third-degree burns: A histological study in rats. Photomed. Laser Surg. 2008, 26, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Pessoa, E.S.; Melhado, R.M.; Theodoro, L.H.; Garcia, V.G. A histologic assessment of the influence of low-intensity laser therapy on wound healing in steroid-treated animals. Photomed. Laser Surg. 2004, 22, 199–204. [Google Scholar] [CrossRef]
- Rodrigo, S.M.; Cunha, A.; Pozza, D.H.; Blaya, D.S.; Moraes, J.F.; Weber, J.B.; de Oliveira, M.G. Analysis of the systemic effect of red and infrared laser therapy on wound repair. Photomed. Laser Surg. 2009, 27, 929–935. [Google Scholar] [CrossRef]
- Treichel, J.L.; Henry, M.M.; Skumatz, C.M.; Eells, J.T.; Burke, J.M. Formate, the toxic metabolite of methanol, in cultured ocular cells. Neurotoxicology 2003, 24, 825–834. [Google Scholar] [CrossRef]
- Byrnes, K.R.; Barna, L.; Chenault, V.M.; Waynant, R.W.; Ilev, I.K.; Longo, L.; Miracco, C.; Johnson, B.; Anders, J.J. Photobiomodulation improves cutaneous wound healing in an animal model of type II diabetes. Photomed. Laser Surg. 2004, 22, 281–290. [Google Scholar] [CrossRef]
- Gal, P.; Vidinsky, B.; Toporcer, T.; Mokry, M.; Mozes, S.; Longauer, F.; Sabo, J. Histological assessment of the effect of laser irradiation on skin wound healing in rats. Photomed. Laser Surg. 2006, 24, 480–488. [Google Scholar] [CrossRef]
- Iordanou, P.; Lykoudis, E.G.; Athanasiou, A.; Koniaris, E.; Papaevangelou, M.; Fatsea, T.; Bellou, P. Effect of visible and infrared polarized light on the healing process of full-thickness skin wounds: An experimental study. Photomed. Laser Surg. 2009, 27, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, P.C.; Pinheiro, A.L.; Reis Junior, J.A.; de Castro, I.C.; Gurgel, C.; Noia, M.P.; Meireles, G.C.; Cangussu, M.C.; Ramalho, L.M. Polarized light (lambda 400–2000 nm) on third-degree burns in diabetic rats: Immunohistochemical study. Photomed. Laser Surg. 2010, 28, 613–619. [Google Scholar] [CrossRef]
- Ribeiro, M.S.; Silva, D.F.; Maldonado, E.P.; de Rossi, W.; Zezell, D.M. Effects of 1047-nm neodymium laser radiation on skin wound healing. J. Clin. Laser Med. Surg. 2002, 20, 37–40. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, A.L.; Pozza, D.H.; Oliveira, M.G.; Weissmann, R.; Ramalho, L.M. Polarized light (400–2000 nm) and non-ablative laser (685 nm): A description of the wound healing process using immunohistochemical analysis. Photomed. Laser Surg. 2005, 23, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Vasilenko, T.; Slezak, M.; Kovac, I.; Bottkova, Z.; Jakubco, J.; Kostelnikova, M.; Tomori, Z.; Gal, P. The effect of equal daily dose achieved by different power densities of low-level laser therapy at 635 and 670 nm on wound tensile strength in rats: A short report. Photomed. Laser Surg. 2010, 28, 281–283. [Google Scholar] [CrossRef]
- Keskin, Y.; Taştekin, N.; Kanter, M.; Top, H.; Özdemir, F.; Erboğa, M.; Taşpınar, Ö.; Süt, N. The effect of magnetic field therapy and electric stimulation on experimental burn healing. Turk. J. Phys. Med. Rehabil. 2019, 65, 352–360. [Google Scholar] [CrossRef]
- Athanasiou, A.; Karkambounas, S.; Batistatou, A.; Lykoudis, E.; Katsaraki, A.; Kartsiouni, T.; Papalois, A.; Evangelou, A. The effect of pulsed electromagnetic fields on secondary skin wound healing: An experimental study. Bioelectromagnetics 2007, 28, 362–368. [Google Scholar] [CrossRef]
- Ganesan, K.; Gengadharan, A.C.; Balachandran, C.; Manohar, B.M.; Puvanakrishnan, R. Low frequency pulsed electromagnetic field—A viable alternative therapy for arthritis. Indian J. Exp. Biol. 2009, 47, 939–948. [Google Scholar]
- Tenuta, M.; Tarsitano, M.G.; Mazzotta, P.; Lucchini, L.; Sesti, F.; Fattorini, G.; Pozza, C.; Olivieri, V.; Naro, F.; Gianfrilli, D.; et al. Therapeutic use of pulsed electromagnetic field therapy reduces prostate volume and lower urinary tract symptoms in benign prostatic hyperplasia. Andrology 2020, 8, 1076–1085. [Google Scholar] [CrossRef] [PubMed]
- Cossarizza, A.; Monti, D.; Bersani, F.; Cantini, M.; Cadossi, R.; Sacchi, A.; Franceschi, C. Extremely low frequency pulsed electromagnetic fields increase cell proliferation in lymphocytes from young and aged subjects. Biochem. Biophys. Res. Commun. 1989, 160, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.M.; Kwon, U.H.; Kim, H.; Kim, H.J.; Kim, B.; Park, J.O.; Moon, E.S.; Moon, S.H. Pulsed electromagnetic field stimulates cellular proliferation in human intervertebral disc cells. Yonsei Med. J. 2010, 51, 954–959. [Google Scholar] [CrossRef] [PubMed]
- Pezzetti, F.; De Mattei, M.; Caruso, A.; Cadossi, R.; Zucchini, P.; Carinci, F.; Traina, G.C.; Sollazzo, V. Effects of pulsed electromagnetic fields on human chondrocytes: An in vitro study. Calcif. Tissue Int. 1999, 65, 396–401. [Google Scholar] [CrossRef] [PubMed]
- Kwan, L.C.R. A Comprehensive Assessment and Management Program for Diabetic Ulcer. Ph.D. Dissertation, Hong Kong Polytechnic University, Hong Kong, China, 2012. [Google Scholar]
- Duran, V.; Zamurović, A.; Stojanović, S.; Poljacki, M.; Jovanović, M.; Durisić, S. Therapy of venous ulcers using pulsating electromagnetic fields—Personal results. Med. Pregl. 1991, 44, 485–488. [Google Scholar] [PubMed]
- Lee, E.W.C.; Maffulli, N.; Li, C.K.; Chan, K.M. Pulsed magnetic and electromagnetic fields in experimental achilles tendonitis in the rat: A prospective randomized study. Arch. Phys. Med. Rehabil. 1997, 78, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Girgin, S.; Gedik, E.; Ozturk, H.; Akbulut, V.; Kale, E.; Buyukbayram, H.; Celik, S. Effects of combined pulse electromagnetic field stimulation plus glutamine on the healing of colonic anastomosis in rats. Dig. Dis. Sci. 2009, 54, 745–750. [Google Scholar] [CrossRef] [PubMed]
- Hussain, M.S.E.D.; Anwar, H.W.; Elnakib, M.M.; Mosaad, A.E. Assessment of the effect of pulsed electromagnetic field therapy in the treatment of chronic wounds. Microbes Infect. Dis. 2023, 4, 928–942. [Google Scholar]
- Amareswari, V.H. Evaluation of Effect of Pulsed Electromagnetic Field Therapy in Chronic Non-Healing Diabetic Foot Ulcers. Ph.D. Dissertation, Madras Medical College, Chennai, India, 2016. [Google Scholar]
- Ahmadian, S.; Zarchi, S.R.; Bolouri, B. Effects of Extremely-Low-Frequency Pulsed Electromagnetic Fields on Collagen Synthesis in Rat Skin. Biotechnol. Appl. Biochem. 2006, 43, 71–75. [Google Scholar] [CrossRef]
- El Rasheed, N.A.A.; Mahmoud, N.F.; Hamada, H.A.; El Khatib, A. Pulsed Electromagnetic Fields Versus Laser Therapy on Enhancing Recovery of Diabetic Foot Ulcer: A Single Blind Randomized Controlled Trial. Biomed. Res. 2017, 28, 8509–8514. [Google Scholar]
- Cheing, G.L.Y.; Li, X.; Huang, L.; Kwan, R.L.C.; Cheung, K.K. Pulsed Electromagnetic Fields (PEMF) Promote Early Wound Healing and Myofibroblast Proliferation in Diabetic Rats. Bioelectromagnetics 2014, 35, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.L.; Wong-Gibbons, D.; Maultsby, J. Microcirculatory Effects of Pulsed Electromagnetic Fields. J. Orthop. Res. 2004, 22, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Fu, C.; Wang, L.; Zhang, Q.; Liang, Z.; He, C.; Wei, Q. The Effect of Pulsed Electromagnetic Fields on Angiogenesis. Bioelectromagnetics 2021, 42, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Fu, C.; Liang, Z.; Zhang, Q.; Xiong, F.; Chen, L.; He, C.; Wei, Q. Pulsed Electromagnetic Fields Increase Angiogenesis and Improve Cardiac Function after Myocardial Ischemia in Mice. Circ. J. 2020, 84, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Umiatin, U.; Hadisoebroto Dilogo, I.; Sari, P.; Kusuma Wijaya, S. Histological Analysis of Bone Callus in Delayed Union Model Fracture Healing Stimulated with Pulsed Electromagnetic Fields (PEMF). Scientifica 2021, 2021, 4791172. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Chen, X.; He, F.; Li, S.; He, R.; Liu, Q.; Dong, Q.; Zhou, S.; Miao, H.; Lu, Q.; et al. Low Frequency Pulsed Electromagnetic Fields Exposure Alleviate the Abnormal Subchondral Bone Remodeling at the Early Stage of Temporomandibular Joint Osteoarthritis. BMC Musculoskelet. Disord. 2022, 23, 987. [Google Scholar] [CrossRef] [PubMed]
- Jing, D.; Zhai, M.; Tong, S.; Xu, F.; Cai, J.; Shen, G.; Wu, Y.; Li, X.; Xie, K.; Liu, J.; et al. Pulsed Electromagnetic Fields Promote Osteogenesis and Osseointegration of Porous Titanium Implants in Bone Defect Repair through a Wnt/β-Catenin Signaling-Associated Mechanism. Sci. Rep. 2016, 6, 32045. [Google Scholar] [CrossRef] [PubMed]
- Jansen, J.H.; van der Jagt, O.P.; Punt, B.J.; Verhaar, J.A.; van Leeuwen, J.P.; Weinans, H.; Jahr, H. Stimulation of Osteogenic Differentiation in Human Osteoprogenitor Cells by Pulsed Electromagnetic Fields: An In Vitro Study. BMC Musculoskelet. Disord. 2010, 11, 188. [Google Scholar] [CrossRef]
- El-Domyati, M.; Barakat, M.; Awad, S.; Medhat, W.; El-Fakahany, H.; Farag, H. Multiple Microneedling Sessions for Minimally Invasive Facial Rejuvenation: An Objective Assessment. Int. J. Dermatol. 2015, 54, 1361–1369. [Google Scholar] [CrossRef]
- Mehta-Ambalal, S.R. Neocollagenesis and Neoelastinogenesis: From the Laboratory to the Clinic. J. Cutan. Aesthet. Surg. 2016, 9, 145–151. [Google Scholar] [CrossRef]
- Zduńska, K.; Kołodziejczak, A.; Rotsztejn, H. Is Skin Microneedling a Good Alternative Method of Various Skin Defects Removal. Dermatol. Ther. 2018, 31, e12714. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).