Autologous Fat Grafting (AFG): A Systematic Review to Evaluate Oncological Safety in Breast Cancer Patients
Abstract
1. Introduction
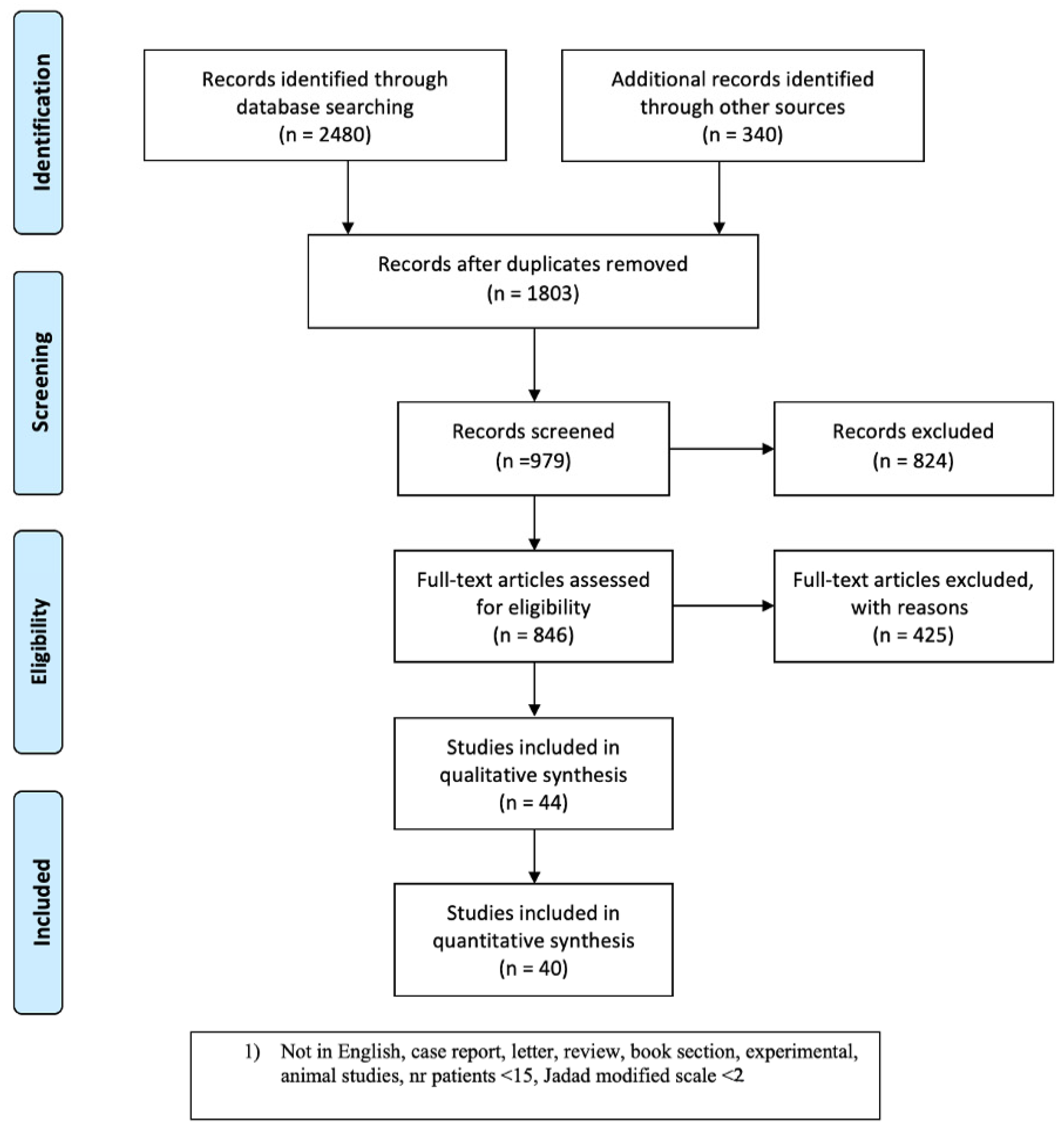
2. Materials and Methods
3. Results
3.1. Study Selection
3.2. Analysis of Selected Studies
3.3. Comparative Analysis
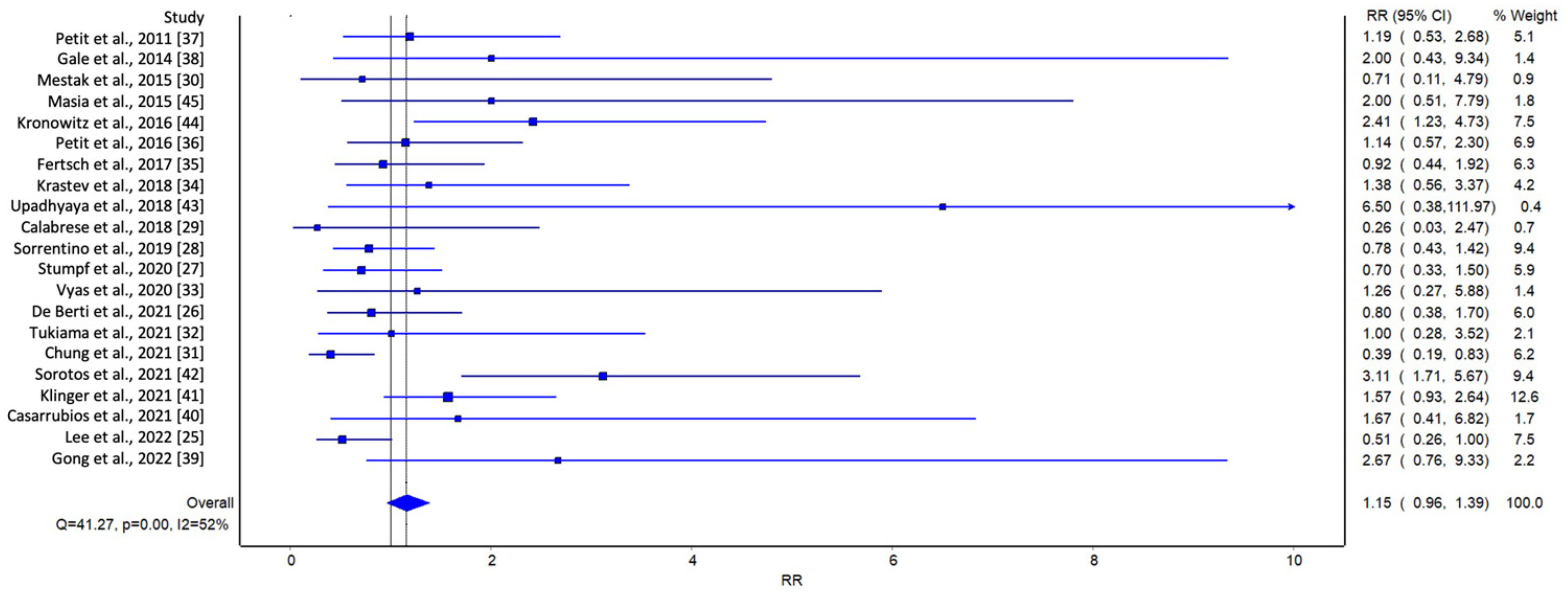
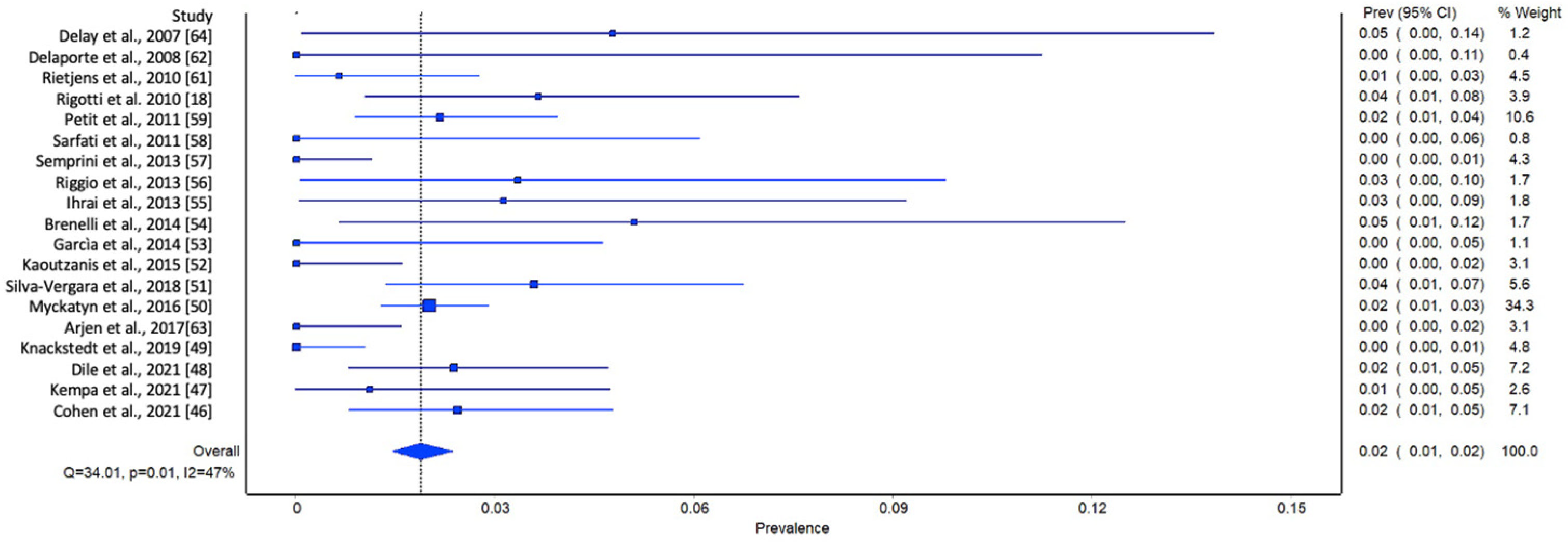
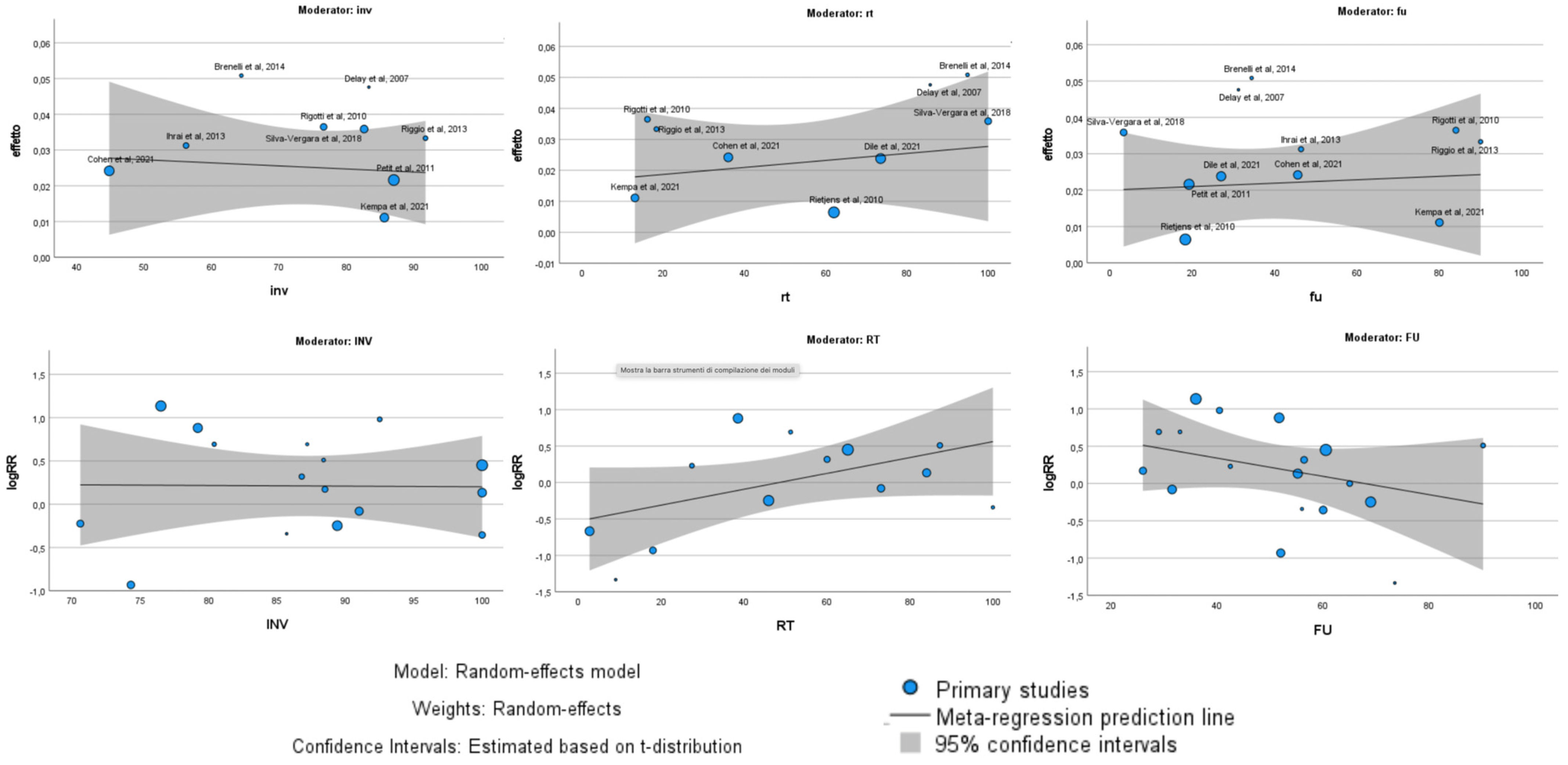
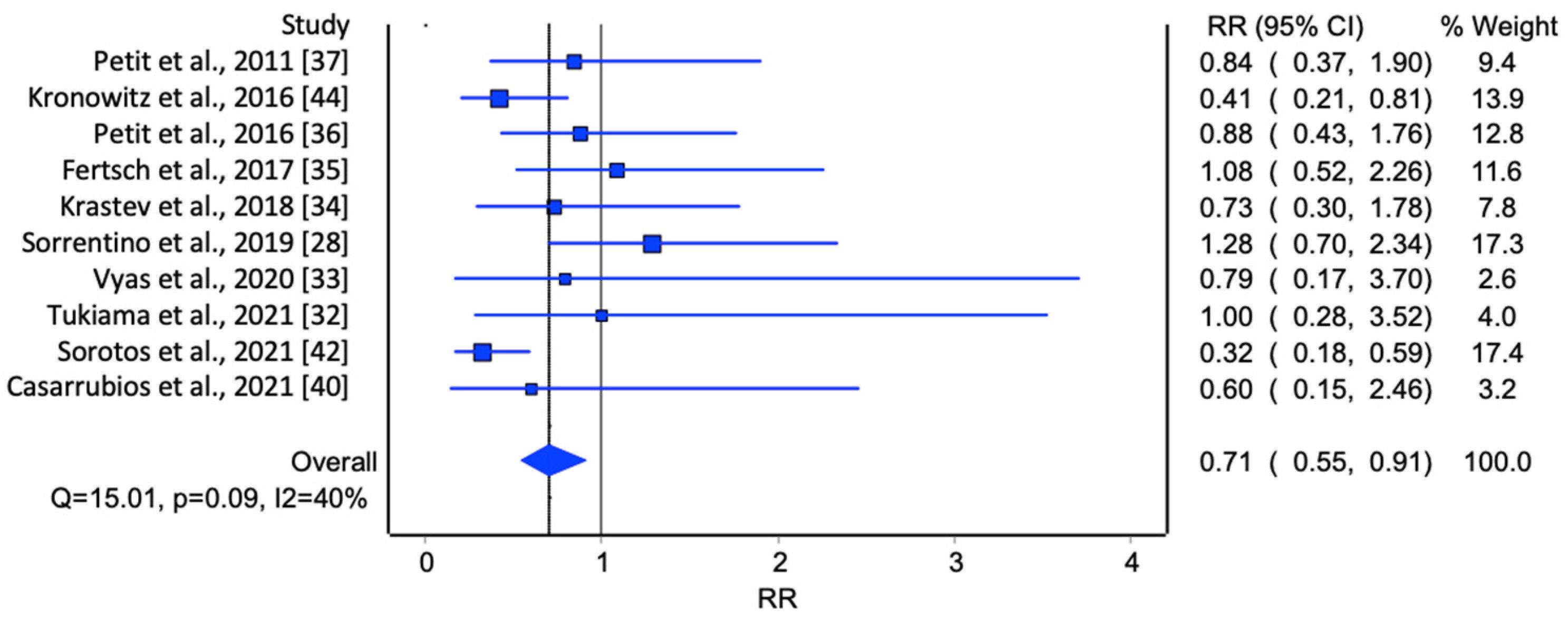
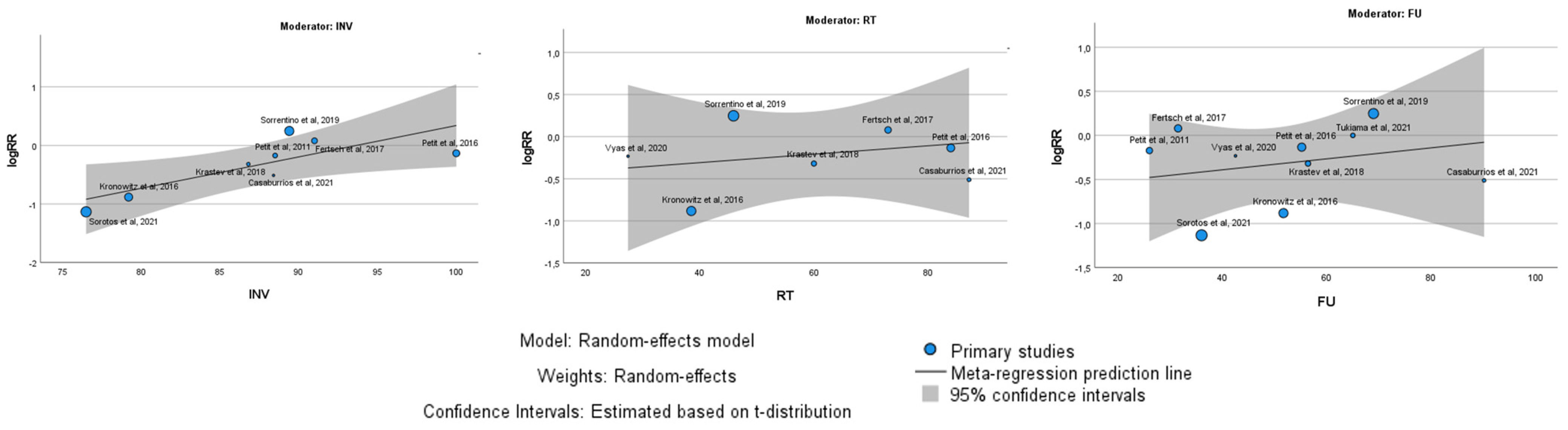
3.4. Meta-Analysis
| Author | Year of Publication | Type of Study | Group | Study Period | Patients (n) | Mean Age (y) | Type of Surgery | Invasive Carcinomas (n) | In Situ Carcinomas (n) | RT before AFG (%) | Mean Surgery-AFG (m) | Mean Follow-up (m) | LRR (%) | LRR (n) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Delay et al. [64] | 2007 | Observational study | BCS + AFG | 2002–2007 | 42 | 51 | BCS + AFG | 35 | 3 | 85.70 | 78 | 31.2 | 4.76 | 2 |
| Delaporte et al. [62] | 2008 | Observational study | MST + AFG | 2002–2007 | 15 | 50 | MST + AFG | 9 | 6 | 78.50 | N/A | 27.6 | 0 | 0 |
| Rietjens et al. [61] | 2010 | Observational study | BCS + MST + AFG | 2005–2008 | 155 | 48 | BCS + MST + IBR + ABR + AFG | N/A | N/A | 62 | 50.5 | 18.3 | 0.70 | 1 |
| Rigotti et al. [18] | 2010 | Retrospective cohort study | MST +AFG | 2000–2005 | 137 | 46.5 | MST +AFG | 105 | 31 | 16.10 | 3.2 | 84 | 3.65 | 5 |
| Petit et al. [37] | 2011 | Multicenter retrospective study | BCS + MST + AFG | 2000–2010 | 370 | 52 | BCS + MST +AFG | 87 | 13 | N/A | N/A | 19.2 | 2.16 | 8 |
| Petit et al. [59] | 2011 | Matched cohort study | MST | 1997–2008 | 642 | 46 | MST | 568 | 74 | N/A | N/A | 26 | 3 | 19 |
| MST + AFG | 321 | 45 | MST + AFG | 284 | 37 | N/A | 26 | 26 | 2.50 | 8 | ||||
| Sarfati et al. [58] | 2011 | Prospective study | MST + AFG | 2007–2009 | 28 | 45 | MST + AFG | N/A | N/A | 100 | N/A | 17 | 0 | 0 |
| Semprini et al. [57] | 2013 | Observational study | BCS + AFG | 2006–2012 | 151 | N/A | BCS + AFG | N/A | N/A | N/A | 24 | 45 | 0 | 0 |
| Riggio et al. [56] | 2013 | Observational study | MST + AFG | 2000–2007 | 60 | 49.7 | MST + AFG | 55 | 5 | 18.30 | 55.2 | 90 | 3.30 | 2 |
| Ihrai et al. [55] | 2013 | Retrospective study | MST + AFG | 2004–2009 | 64 | N/A | MST + AFG | 36 | 10 | N/A | N/A | 46.44 | 3.10 | 2 |
| Brenelli et al. [54] | 2014 | Prospective study | BCS + AFG | 2005–2008 | 59 | 50 | BCS + AFG | 38 | 7 | 94.90 | N/A | 34.4 | 5.10 | 3 |
| Gale et al. [38] | 2014 | Clinical study | BCS + MST | 2007–2013 | 422 | 48.2 | BCS + MST | 368 | 54 | N/A | 54 | 34 | 1.90 | 8 |
| BCS + MST + AFG | 211 | 47 | BCS + MST + AFG | 184 | 27 | 108 | 54 | 32 | 0.95 | 2 | ||||
| Garcìa et al. [53] | 2014 | Observational study | BCS + AFG | N/A | 37 | 55 | BCS + AFG | 0 | 37 | N/A | 0 | 1 | 0 | 0 |
| Kaoutzanis et al. [52] | 2015 | Retrospective study | MST + AFG | 2008–2013 | 108 | 48 | MST + AFG | 68 | 40 | 23.30 | 10.8 | 20.2 | 0 | 0 |
| Mestak et al. [30] | 2015 | Prospective study | BCS | 2011–2014 | 45 | 64 | BCS | 41 | 3 | N/A | N/A | 56 | 4.88 | 2 |
| BCS + AFG | 32 | 53 | BCS + AFG | 25 | 4 | 100 | 77 | 56 | 6.25 | 2 | ||||
| Silva-Vergara et al. [51] | 2015 | Retrospective study | BCS + MST + AFG | 2007–2015 | 195 | 52 | BCS + MST + AFG | 161 | 44 | 100 | 4 | 3.3 | 3.58 | 7 |
| Masia et al. [45] | 2015 | Retrospective study case-control | MST + ABR | 1989–2017 | 107 | 49 | MST + ABR | 87 | 16 | N/A | N/A | 29 | 5.60 | 6 |
| MST + ABR + AFG | 107 | 49.19 | MST + ABR + AFG | 85 | 14 | N/A | N/A | 29 | 2.80 | 3 | ||||
| Kronowitz et al. [44] | 2016 | Retrospective cohort study | MST | 2001–2014 | 670 | 46.5 | MST | 548 | 61 | N/A | N/A | 43.8 | 4.10 | 27 |
| BCS + MST + AFG | 719 | 47.1 | BCS + MST + AFG | 552 | 108 | 38.50 | 2.63 | 59.6 | 1.60 | 12 | ||||
| Myckatyn et al. [50] | 2016 | Multicenter case cohort study | MST + AFG | 2006–2011 | 1197 | 47 | MST + IBR + ABR | N/A | N/A | N/A | N/A | N/A | 11.00% | 24 |
| Petit et al. [36] | 2016 | Matched case-control study | MST | 2006–2013 | 322 | N/A | MST + BCS | 322 | 0 | 86 | N/A | 52.8 | 5 | 16 |
| MST + AFG | 322 | N/A | MST + BCS + AFG | 322 | 0 | 84 | N/A | 57.6 | 4.30 | 14 | ||||
| Arjen et al. [63] | 2017 | Retrospective cohort study | BCS + AFG | 2008–2016 | 109 | 55 | BCS + AFG | N/A | N/A | 100 | 18 | 26.4 | 0 | 0 |
| Fertsch et al. [35] | 2017 | Matched retrospective cohort study | MST + DIEP | 2009–2013 | 100 | 50.7 | MST + ABR | 91 | 9 | N/A | N/A | 31 | 12 | 12 |
| MST + DIEP + AFG | 100 | 49.6 | MST + ABR + AFG | 91 | 9 | 73 | 40.5 | 32 | 13 | 13 | ||||
| Krastev et al. [34] | 2018 | Matched cohort study | MST + BCS | 2006–2014 | 300 | 49.4 | MST + BCS | 260 | 40 | N/A | N/A | 52.8 | 3.60 | 11 |
| MST + BCS + AFG | 300 | 48.1 | MST + BCS + AFG | 261 | 39 | 60 | N/A | 60 | 2.60 | 8 | ||||
| Upadhyaya et al. [43] | 2018 | Retrospective chart review study | MST | 2011–2016 | 449 | N/A | MST + IBR + ABR | N/A | N/A | N/A | N/A | 26 | 1.70 | 8 |
| MST + AFG | 171 | 50.51 | MST + IBR + ABR + AFG | N/A | N/A | N/A | N/A | 26 | 0 | 0 | ||||
| Calabrese et al. [29] | 2018 | Prospective multi arm single center cohort study | MST | 2008–2011 | 72 | 47.7 | MST | N/A | N/A | N/A | N/A | 72 | 1.60 | 1 |
| MST + AFG | 57 | 50.3 | MST + AFG | N/A | N/A | 9 | 9 | 75 | 4.70 | 3 | ||||
| MST + EAFG | 54 | 48.8 | MST +EAFG | N/A | N/A | 17 | 10 | 84 | 2.40 | 1 | ||||
| Sorrentino et al. [28] | 2019 | Retrospective exact matching study | MST + BCS | 2007–2017 | 597 | 50.7 | MST + BCS | 535 | 62 | N/A | N/A | 63.8 | 5.00% | 30 |
| MST + BCS + AFG | 233 | 49.4 | MST + BCS + AFG | 207 | 26 | 45.90 | 22.9 | 74.1 | 6.40 | 15 | ||||
| Knackstedt et al. [49] | 2019 | Retrospective cohort study | MST + IBR + AFG | 2006–2015 | 166 | 52 | MST + IBR + AFG | 106 | 52 | 20 | N/A | 28 | 0 | 0 |
| Stumpf et al. [27] | 2020 | Matched retrospective cohort study | BCS | 2004–2016 | 255 | 54 | BCS | 255 | 0 | N/A | N/A | 60 | 8.60 | 22 |
| BCS + AFG | 65 | 53 | BCS + AFG | 65 | 0 | N/A | N/A | 60 | 12.30 | 8 | ||||
| Vyas et al. [33] | 2020 | Matched case-control study | MST | 2000–2017 | 69 | N/A | MST | N/A | N/A | N/A | N/A | 42.5 | 8.50 | 6 |
| MST +AFG | 29 | 48.6 | MST + AFG | N/A | N/A | 27.4 | N/A | 42.5 | 8.20 | 2 | ||||
| Dile et al. [48] | 2021 | Retrospective study | MST + BCS + AFG | 2013–2016 | 252 | 50 | MST + BCS + ABR + IBR + AFG | N/A | N/A | 73.50 | 35 | 27 | 2.40 | 6 |
| Kempa et al. [47] | 2021 | Monocentric cohort study | MST + BCS + AFG | 2008–2020 | 90 | 46.1 | MST + BCS + AFG | 77 | 13 | 13 | 57 | 80 | 0.90 | 1 |
| De Berti et al. [26] | 2021 | Retrospective monocentric case-control study | MST | 2007–2017 | 303 | 52 | MST + BCS + ABR + IBR | 202 | 87 | N/A | N/A | N/A | 6.60 | 20 |
| MST + AFG | 109 | 50 | MST + BCS + ABR +IBR + AFG | 89 | 16 | N/A | N/A | N/A | 8.30 | 9 | ||||
| Tukiama et al. [32] | 2021 | Retrospective matched cohort study | MST | 2007–2016 | 126 | N/A | MST + BCS | N/A | N/A | N/A | N/A | 65 | 7.10 | 9 |
| MST + AFG | 42 | N/A | MST + BCS + AFG | N/A | N/A | N/A | N/A | 65 | 6.30% | 3 | ||||
| Chung et al. [31] | 2021 | Retrospective cohort study | MST | 2009–2019 | 272 | 50.4 | MST + BCS + ABR + IBR | 200 | 66 | N/A | N/A | 52 | 6 | 16 |
| MST + AFG | 67 | 50.4 | MST + BCS + ABR + IBR + AFG | 52 | 15 | 18 | N/A | 52 | 15 | 10 | ||||
| Sorotos et al. [42] | 2021 | Retrospective matched case control study | MST | 2005–2017 | 494 | 45 -49 | MST + IBR + ABR | 379 | 115 | N/A | N/A | 36 | 9.60 | 47 |
| MST + AFG | 425 | 45–49 | MST + IBR + ABR + AFG | 324 | 101 | N/A | N/A | 36 | 3 | 13 | ||||
| Klinger et al. [41] | 2021 | Retrospective multicenter study case- control | MST + BCS | 2000–2018 | 923 | 52.9 | MST + BCS | 923 | N/A | N/A | N/A | 58 | 6.10 | 56 |
| MST +BCS + AFG | 466 | 51.4 | MST + BCS + AFG | 466 | N/A | 65 | N/A | 63 | 3.90 | 18 | ||||
| Casarrubios et al. [40] | 2021 | Matched cohort study | MST | 2011–2019 | 125 | 47.2 | MST + BCS | 115 | 10 | N/A | N/A | 85 | 4 | 5 |
| MST + AFG | 125 | 45.6 | MST + BCS + AFG | 106 | 19 | 87.20 | 48.1 | 95.3 | 2.40 | 3 | ||||
| Cohen et al. [46] | 2021 | Retrospective cohort study | MST + AFG | 2010–2015 | 248 | 47.95 | MST + AFG | 111 | 51 | 36 | 13.2 | 45.6 | 2.40 | 6 |
| Lee et al. [25] | 2022 | Retrospective cohort study | MST | 2011–2016 | 126 | 43.9 | MST + IBR | N/A | N/A | N/A | N/A | N/A | 9 | 11 |
| MST + AFG | 141 | 43.9 | MST + IBR + AFG | N/A | N/A | 2.70 | 12 | N/A | 17 | 24 | ||||
| Gong et al. [39] | 2022 | Retrospective cohort study | BCS | 2018 | 40 | 50.8 | BCS | 36 | 4 | N/A | N/A | 40.28 | 10 | 8 |
| BCS + AFG | 40 | 50.2 | BCS + AFG | 38 | 2 | N/A | N/A | 40.58 | 7.50 | 3 |
4. Discussion
5. Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- DeSantis, C.E.; Ma, J.; Gaudet, M.M.; Newman, L.A.; Miller, K.D.; Goding Sauer, A.; Jemal, A.; Siegel, R.L. Breast cancer statistics, 2019. Cancer J. Clin. 2019, 69, 438–451. [Google Scholar] [CrossRef]
- Buyse, M.; Saad, E.D.; Burzykowski, T.; Regan, M.M.; Sweeney, C.S. Surrogacy beyond prognosis: The importance of “trial-level” surrogacy. Oncologist 2022, 27, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Black, D.M.; Mittendorf, E.A. Landmark trials affecting the surgical management of invasive breast cancer. Surg. Clin. N. Am. 2013, 93, 501–518. [Google Scholar] [CrossRef]
- Calabrese, C.; Casella, D.; Di Taranto, G.; Marcasciano, M.; Kothari, A.; Sordi, S.; Barellini, L.; Torto, F.L.; Tarallo, M.; Perra, A.; et al. Oncoplastic conservative surgery for breast cancer: Long-term outcomes of our first ten years experience. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 7333–7342. [Google Scholar] [CrossRef]
- Hanson, S.E.; Lei, X.; Roubaud, M.S.; DeSnyder, S.M.; Caudle, A.S.; Shaitelman, S.F.; Hoffman, K.E.; Smith, G.L.; Jagsi, R.; Peterson, S.K.; et al. Long-term Quality of Life in Patients with Breast Cancer after Breast Conservation vs. Mastectomy and Reconstruction. JAMA Surg. 2022, 157, e220631. [Google Scholar] [CrossRef]
- Biazus, J.V.; Falcão, C.C.; Parizotto, A.C.; Stumpf, C.C.; Cavalheiro, J.A.C.; Schuh, F.; Cericatto, R.; Zucatto, E.; Melo, M.P. Immediate Reconstruction with Autologous fat Transfer Following Breast-Conserving Surgery. Breast J. 2015, 21, 268–275. [Google Scholar] [CrossRef]
- Torto, F.L.; Marcasciano, M.; Kaciulyte, J.; Redi, U.; Barellini, L.; De Luca, A.; Perra, A.; Frattaroli, J.M.; Cavalieri, E.; Di Taranto, G.; et al. Prepectoral breast reconstruction with TiLoop® Bra Pocket: A single center prospective study. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 991–999. [Google Scholar] [CrossRef]
- Vaia, N.; Torto, F.L.; Marcasciano, M.; Casella, D.; Cacace, C.; De Masi, C.; Ricci, F.; Ribuffo, D. From the “Fat Capsule” to the “Fat Belt”: Limiting Protective Lipofilling on Irradiated Expanders for Breast Reconstruction to Selective Key Areas. Aesthetic Plast. Surg. 2018, 42, 986–994. [Google Scholar] [CrossRef] [PubMed]
- Ribuffo, D.; Atzeni, M.; Guerra, M.; Bucher, S.; Politi, C.; Deidda, M.; Atzori, F.; Dessi, M.; Madeddu, C.; Lay, G. Treatment of irradiated expanders: Protective lipofilling allows immediate prosthetic breast reconstruction in the setting of postoperative radiotherapy. Aesthetic Plast. Surg. 2013, 37, 1146–1152. [Google Scholar] [CrossRef] [PubMed]
- Lo Torto, F.; Parisi, P.; Casella, D.; Di Taranto, G.; Cigna, E.; Ribuffo, D. Impact of Evolving Radiation Therapy Techniques on Implant-Based Breast Reconstruction. Plast. Reconstr. Surg. 2018, 141, 182e–183e. [Google Scholar] [CrossRef]
- Zhang, X.; Cai, L.; Yin, B.; Han, X.; Li, F. Total breast reconstruction using large-volume condensed and viable fat grafting after mastectomy. J. Plast. Reconstr. Aesthetic Surg. 2021, 74, 966–973. [Google Scholar] [CrossRef] [PubMed]
- Doren, E.L.; Parikh, R.P.; Laronga, C.; Hiro, M.E.; Sun, W.; Lee, M.C.; Smith, P.D.; Fulp, W.J. Sequelae of fat grafting postmastectomy: An algorithm for management of fat necrosis. Eplasty 2012, 12, e53. [Google Scholar] [PubMed]
- Choi, J.; Cha, Y.J.; Koo, J.S. Adipocyte biology in breast cancer: From silent bystander to active facilitator. Prog. Lipid Res. 2018, 69, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Buache, E.; Chenard, M.P.; Dali-Youcef, N.; Rio, M.C. Adipocyte is a non-trivial, dynamic partner of breast cancer cells. Int. J. Dev. Biol. 2011, 55, 851–859. [Google Scholar] [CrossRef] [PubMed]
- Report on autologous fat transplantation. ASPRS Ad-Hoc committee on new procedures, September 30, 1987. Plast. Aesthetic Nurs. 1987, 7, 140–141.
- Juhl, A.A.; Redsted, S.; Engberg Damsgaard, T. Autologous fat grafting after breast conserving surgery: Breast imaging changes and patient-reported outcome. J. Plast. Reconstr. Aesthetic Surg. 2018, 71, 1570–1576. [Google Scholar] [CrossRef] [PubMed]
- Lohsiriwat, V.; Curigliano, G.; Rietjens, M.; Goldhirsch, A.; Petit, J.Y. Autologous fat transplantation in patients with breast cancer: “silencing” or “fueling” cancer recurrence? Breast 2011, 20, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Rigotti, G.; Marchi, A.; Galiè, M.; Baroni, G.; Benati, D.; Krampera, M.; Pasini, A.; Sbarbati, A. Clinical treatment of radiotherapy tissue damage by lipoaspirate transplant: A healing process mediated by adipose-derived adult stem cells. Plast. Reconstr. Surg. 2007, 119, 1409–1422. [Google Scholar] [CrossRef]
- Iyengar, P.; Combs, T.P.; Shah, S.J.; Gouon-Evans, V.; Pollard, J.W.; Albanese, C.; Flanagan, L.; Tenniswood, M.P.; Guha, C.; Lisanti, M.P.; et al. Adipocyte-secreted factors synergistically promote mammary tumorigenesis through induction of anti-apoptotic transcriptional programs and proto-oncogene stabilization. Oncogene 2003, 22, 6408–6423. [Google Scholar] [CrossRef]
- Manabe, Y.; Toda, S.; Miyazaki, K.; Sugihara, H. Mature adipocytes, but not preadipocytes, promote the growth of breast carcinoma cells in collagen gel matrix culture through cancer-stromal cell interactions. J. Pathol. 2003, 201, 221–228. [Google Scholar] [CrossRef]
- Salgado, A.J.; Reis, R.L.; Sousa, N.J.; Gimble, J.M. Adipose tissue derived stem cells secretome: Soluble factors and their roles in regenerative medicine. Curr. Stem Cell Res. Ther. 2010, 5, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Daquinag, A.; Traktuev, D.O.; Amaya-Manzanares, F.; Simmons, P.J.; March, K.L.; Pasqualini, R.; Arap, W.; Kolonin, M.G. White adipose tissue cells are recruited by experimental tumors and promote cancer progression in mouse models. Cancer Res. 2009, 69, 5259–5266. [Google Scholar] [CrossRef]
- Howick, J.; Chalmers, I.; Glasziou, P.; Greenhalgh, T.; Heneghan, C.; Liberati, A.; Moschetti, I.; Phillips, B.; Thornton, H. OCEBM Levels of Evidence—Centre for Evidence-Based Medicine (CEBM). University of Oxford. 2011. Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence (accessed on 26 May 2024).
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds DJ, M.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Lee, K.-T.; Kim, J.H.; Jeon, B.-J.; Pyon, J.K.; Mun, G.-H.; Lee, S.K.; Yu, J.; Kim, S.W.; Lee, J.E.; Ryu, J.M.; et al. Association of Fat Graft with Breast Cancer Recurrence in Implant-Based Reconstruction: Does the Timing Matter? Ann. Surg. Oncol. 2023, 30, 1087–1097. [Google Scholar] [CrossRef] [PubMed]
- De Berti, M.; Goupille, C.; Doucet, M.; Arbion, F.; Vilde, A.; Body, G.; Ouldamer, L. Oncological Safety of Autologous Fat Grafting in Breast Reconstruction after Mastectomy for cancer: A case-control study. J. Gynecol. Obstet. Hum. Reprod. 2022, 51, 102257. [Google Scholar] [CrossRef] [PubMed]
- Stumpf, C.C.; Zucatto, E.; Cavalheiro, J.A.C.; de Melo, M.P.; Cericato, R.; Damin, A.P.S.; Biazús, J.V. Oncologic safety of immediate autologous fat grafting for reconstruction in breast-conserving surgery. Breast Cancer Res. Treat. 2020, 180, 301–309. [Google Scholar] [CrossRef] [PubMed]
- Sorrentino, L.; Regolo, L.; Scoccia, E.; Petrolo, G.; Bossi, D.; Albasini, S.; Caruso, A.; Vanna, R.; Morasso, C.; Mazzucchelli, S.; et al. Autologous fat transfer after breast cancer surgery: An exact-matching study on the long-term oncological safety. Eur. J. Surg. Oncol. 2019, 45, 1827–1834. [Google Scholar] [CrossRef]
- Calabrese, C.; Kothari, A.; Badylak, S.; Di Taranto, G.; Marcasciano, M.; Sordi, S.; Barellini, L.; Torto, F.L.; Tarallo, M.; Gaggelli, I.; et al. Oncological safety of stromal vascular fraction enriched fat grafting in two-stage breast reconstruction after nipple sparing mastectomy: Long-term results of a prospective study. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 4768–4777. [Google Scholar] [CrossRef]
- Mestak, O.; Hromadkova, V.; Fajfrova, M.; Molitor, M.; Mestak, J. Evaluation of Oncological Safety of Fat Grafting After Breast-Conserving Therapy: A Prospective Study. Ann. Surg. Oncol. 2016, 23, 776–781. [Google Scholar] [CrossRef]
- Chung, J.H.; Kim, K.J.; Jung, S.P.; Park, S.H.; Yoon, E.S. Analysis of oncological safety of autologous fat grafting after immediate breast reconstruction. Gland. Surg. 2021, 10, 584–594. [Google Scholar] [CrossRef]
- Tukiama, R.; Vieira, R.A.C.; Facina, G.; da Cunha Leal, P.; Zucca-Matthes, G. Oncologic Safety of Autologous Fat Grafting after Breast Cancer Surgical Treatment: A Matched Cohort Study. Plast. Reconstr. Surg. 2021, 148, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Vyas, K.S.M.; DeCoster, R.C.; Burns, J.C.; Rodgers, L.T.B.; Shrout, M.A.; Mercer, J.P.B.; Coquillard, C.; Dugan, A.J.; Baratta, M.D.; Rinker, B.D.M.; et al. Autologous Fat Grafting Does Not Increase Risk of Oncologic Recurrence in the Reconstructed Breast. Ann. Plast. Surg. 2020, 84 (Suppl. S6), S405–S410. [Google Scholar] [CrossRef] [PubMed]
- Krastev, T.; van Turnhout, A.; Vriens, E.; Smits, L.; van der Hulst, R. Long-term Follow-up of Autologous Fat Transfer vs Conventional Breast Reconstruction and Association with Cancer Relapse in Patients with Breast Cancer. JAMA Surg. 2019, 154, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Fertsch, S.; Hagouan, M.; Munder, B.; Schulz, T.; Abu-Ghazaleh, A.; Schaberick, J.; Stambera, P.; Aldeeri, M.; Andree, C.; Thamm, O.C. Increased risk of recurrence associated with certain risk factors in breast cancer patients after DIEP-flap reconstruction and lipofilling-a matched cohort study with 200 patients. Gland Surg. 2017, 6, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Petit, J.Y.; Maisonneuve, P.; Rotmensz, N.; Bertolini, F.; Rietjens, M. Fat Grafting after Invasive Breast Cancer: A Matched Case-Control Study. Plast. Reconstr. Surg. 2017, 139, 1292–1296. [Google Scholar] [CrossRef] [PubMed]
- Petit, J.Y.; Botteri, E.; Lohsiriwat, V.; Rietjens, M.; De Lorenzi, F.; Garusi, C.; Rossetto, F.; Martella, S.; Manconi, A.; Bertolini, F.; et al. Locoregional recurrence risk after lipofilling in breast cancer patients. Ann. Oncol. 2012, 23, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Gale, K.L.; Rakha, E.A.; Ball, G.; Tan, V.K.; McCulley, S.J.; Macmillan, R.D. A case-controlled study of the oncologic safety of fat grafting. Plast. Reconstr. Surg. 2015, 135, 1263–1275. [Google Scholar] [CrossRef]
- Gong, F.-X.; Zhou, X.; Niu, Z.-H.; Mao, Y.; Wang, Y.-M.; Lv, M.; Gao, X.-Q.; Liu, W.-J.; Wang, H.-B. Effects of Breast-Conserving Surgery Combined with Immediate Autologous Fat Grafting on Oncologic Safety, Satisfaction and Psychology in Patients with Breast Cancer: A Retrospective Cohort Study. Cancer Manag. Res. 2022, 14, 1113–1124. [Google Scholar] [CrossRef] [PubMed]
- Casarrubios, J.M.; Francés, M.; Fuertes, V.; Singer, M.; Navarro, C.; Duque, O.G.; Fernández-Palacios, J. Oncological outcomes of lipofilling in breast reconstruction: A matched cohort study with 250 patients. Gland Surg. 2021, 10, 914–923. [Google Scholar] [CrossRef]
- Klinger, M.; Losurdo, A.; Lisa, A.V.E.; Morenghi, E.; Vinci, V.; Corsi, F.; Albasini, S.; Leonardi, M.C.; Jereczek-Fossa, B.A.; Veronesi, P.; et al. Safety of autologous fat grafting in breast cancer: A multicenter Italian study among 17 senonetwork breast units autologous fat grafting safety: A multicenter Italian retrospective study. Breast Cancer Res. Treat. 2022, 191, 355–363. [Google Scholar] [CrossRef]
- Sorotos, M.; Paolini, G.; D’orsi, G.; Firmani, G.; Timmermans, F.W.; di Pompeo, F.S. Oncologic Outcome of 1000 Postmastectomy Breast Reconstructions with Fat Transfer: A Single-Center, Matched Case-Control Study. Plast. Reconstr. Surg. 2022, 150, 4S–12S. [Google Scholar] [CrossRef]
- Upadhyaya, S.N.; Bernard, S.L.; Grobmyer, S.R.; Yanda, C.; Tu, C.; Valente, S.A. Outcomes of Autologous Fat Grafting in Mastectomy Patients Following Breast Reconstruction. Ann. Surg. Oncol. 2018, 25, 3052–3056. [Google Scholar] [CrossRef] [PubMed]
- Kronowitz, S.J.; Mandujano, C.C.; Liu, J.; Kuerer, H.M.; Smith, B.; Garvey, P.; Jagsi, R.; Hsu, L.; Hanson, S.; Valero, V. Lipofilling of the Breast Does Not Increase the Risk of Recurrence of Breast Cancer: A Matched Controlled Study. Plast. Reconstr. Surg. 2016, 137, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Masia, J.; Bordoni, D.; Pons, G.; Liuzza, C.; Castagnetti, F.; Falco, G. Oncological safety of breast cancer patients undergoing free-flap reconstruction and lipofilling. Eur. J. Surg. Oncol. 2015, 41, 612–616. [Google Scholar] [CrossRef] [PubMed]
- Cohen, O.; Lam, G.; Karp, N.; Choi, M. Determining the Oncologic Safety of Autologous Fat Grafting as a Reconstructive Modality: An Institutional Review of Breast Cancer Recurrence Rates and Surgical Outcomes. Plast. Reconstr. Surg. 2017, 140, 382e–392e. [Google Scholar] [CrossRef]
- Kempa, S.; Brix, E.; Heine, N.; Hösl, V.; Strauss, C.; Eigenberger, A.; Brébant, V.; Seitz, S.; Prantl, L. Autologous fat grafting for breast reconstruction after breast cancer: A 12-year experience. Arch. Gynecol. Obstet. 2022, 305, 921–927. [Google Scholar] [CrossRef]
- Dile, P.; Hannebicque, K.; Renaudeau, C.; Bogart, É.; Ceugnart, L.; Regis, C.; Boulanger, L.; Chauvet, M.-P. Palpable Nodules After Autologous Fat Grafting in Breast Cancer Patients: Incidence and Impact on Follow-up. Aesthetic Plast. Surg. 2023, 47, 503–511. [Google Scholar] [CrossRef]
- Knackstedt, R.W.; Gatherwright, J.; Ataya, D.; Duraes, E.F.R.; Schwarz, G.S. Fat Grafting and the Palpable Breast Mass in Implant-Based Breast Reconstruction: Incidence and Implications. Plast. Reconstr. Surg. 2019, 144, 265–275. [Google Scholar] [CrossRef]
- Myckatyn, T.M.; Wagner, I.J.; Mehrara, B.J.; Crosby, M.A.; Park, J.E.; Qaqish, B.F.M.; Moore, D.T.; Busch, E.L.; Silva, A.K.; Kaur, S.; et al. Cancer Risk after Fat Transfer: A Multicenter Case-Cohort Study. Plast. Reconstr. Surg. 2017, 139, 11–18. [Google Scholar] [CrossRef]
- Silva-Vergara, C.; Fontdevila, J.; Descarrega, J.; Burdio, F.; Yoon, T.S.; Grande, L. Oncological outcomes of lipofilling breast reconstruction: 195 consecutive cases and literature review. J. Plast. Reconstr. Aesthetic Surg. 2016, 69, 475–481. [Google Scholar] [CrossRef]
- Kaoutzanis, C.; Xin, M.; Ballard, T.N.; Welch, K.B.; Momoh, A.O.; Kozlow, J.H.; Brown, D.L.; Cederna, P.S.; Wilkins, E.G. Autologous Fat Grafting After Breast Reconstruction in Postmastectomy Patients: Complications, Biopsy Rates, and Locoregional Cancer Recurrence Rates. Ann. Plast. Surg. 2016, 76, 270–275. [Google Scholar] [CrossRef]
- Moltó García, R.; González Alonso, V.; Villaverde Doménech, M.E. Fat grafting in immediate breast reconstruction. Avoiding breast sequelae. Breast Cancer 2016, 23, 134–140. [Google Scholar] [CrossRef]
- Brenelli, F.; Rietjens, M.; De Lorenzi, F.; Pinto-Neto, A.; Rossetto, F.; Martella, S.; Rodrigues, J.R.; Barbalho, D. Oncological safety of autologous fat grafting after breast conservative treatment: A prospective evaluation. Breast J. 2014, 20, 159–165. [Google Scholar] [CrossRef]
- Ihrai, T.; Georgiou, C.; Machiavello, J.-C.; Chignon-Sicard, B.; Figl, A.; Raoust, I.; Bourgeon, Y.; Fouche, Y.; Flipo, B. Autologous fat grafting and breast cancer recurrences: Retrospective analysis of a series of 100 procedures in 64 patients. J. Plast. Surg. Hand Surg. 2013, 47, 273–275. [Google Scholar] [CrossRef]
- Riggio, E.; Bordoni, D.; Nava, M.B. Oncologic surveillance of breast cancer patients after lipofilling. Aesthetic Plast. Surg. 2013, 37, 728–735. [Google Scholar] [CrossRef]
- Semprini, G.; Cattin, F.; Vaienti, L.; Brizzolari, M.; Cedolini, C.; Parodi, P.C. Oncoplastic surgery and cancer relapses: Cosmetic and oncological results in 489 patients. Breast 2013, 22, 946–951. [Google Scholar] [CrossRef]
- Sarfati, I.; Ihrai, T.; Kaufman, G.; Nos, C.; Clough, K.B. Adipose-tissue grafting to the post-mastectomy irradiated chest wall: Preparing the ground for implant reconstruction. J. Plast. Reconstr. Aesthetic Surg. 2011, 64, 1161–1166. [Google Scholar] [CrossRef]
- Petit, J.Y.; Lohsiriwat, V.; Clough, K.B.; Sarfati, I.; Ihrai, T.; Rietjens, M.; Veronesi, P.; Rossetto, F.; Scevola, A.; Delay, E. The oncologic outcome and immediate surgical complications of lipofilling in breast cancer patients: A multicenter study-Milan-Paris-Lyon experience of 646 lipofilling procedures. Plast. Reconstr. Surg. 2011, 128, 341–346, Erratum in Plast. Reconstr. Surg. 2011, 128, 1317. [Google Scholar] [CrossRef]
- Rigotti, G.; Marchi, A.; Stringhini, P.; Baroni, G.; Galiè, M.; Molino, A.M.; Mercanti, A.; Micciolo, R.; Sbarbati, A. Determining the oncological risk of autologous lipoaspirate grafting for post-mastectomy breast reconstruction. Aesthetic Plast. Surg. 2010, 34, 475–480. [Google Scholar] [CrossRef]
- Rietjens, M.; De Lorenzi, F.; Rossetto, F.; Brenelli, F.; Manconi, A.; Martella, S.; Intra, M.; Venturino, M.; Lohsiriwat, V.; Ahmed, Y.; et al. Safety of fat grafting in secondary breast reconstruction after cancer. J. Plast. Reconstr. Aesthetic Surg. 2011, 64, 477–483. [Google Scholar] [CrossRef]
- Delaporte, T.; Delay, E.; Toussoun, G.; Delbaere, M.; Sinna, R. Reconstruction mammaire par transfert graisseux exclusif: À propos de 15 cas consécutifs [Breast volume reconstruction by lipomodeling technique: About 15 consecutive cases]. Ann. Chir. Plast. Esthét. 2009, 54, 303–316. [Google Scholar] [CrossRef] [PubMed]
- van Turnhout, A.A.; Fuchs, S.; Lisabeth-Broné, K.; Vriens-Nieuwenhuis, E.J.C.; van der Sluis, W.B. Surgical Outcome and Cosmetic Results of Autologous Fat Grafting After Breast Conserving Surgery and Radiotherapy for Breast Cancer: A Retrospective Cohort Study of 222 Fat Grafting Sessions in 109 Patients. Aesthetic Plast. Surg. 2017, 41, 1334–1341. [Google Scholar] [CrossRef] [PubMed]
- Delay, E.; Gosset, J.; Toussoun, G.; Delaporte, T.; Delbaere, M. Efficacité du lipomodelage pour la correction des séquelles du traitement conservateur du cancer du sein [Efficacy of lipomodelling for the management of sequelae of breast cancer conservative treatment]. Ann. Chir. Plast. Esthét. 2008, 53, 153–168. [Google Scholar] [CrossRef]
- Pearl, R.A.; Leedham, S.J.; Pacifico, M.D. The safety of autologous fat transfer in breast cancer: Lessons from stem cell biology. J. Plast. Reconstr. Aesthetic Surg. 2012, 65, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Perrot, P.; Rousseau, J.; Bouffaut, A.-L.; Rédini, F.; Cassagnau, E.; Deschaseaux, F.; Heymann, M.-F.; Heymann, D.; Duteille, F.; Trichet, V.; et al. Safety concern between autologous fat graft, mesenchymal stem cell and osteosarcoma recurrence. PLoS ONE 2010, 5, e10999. [Google Scholar] [CrossRef] [PubMed]
- Karnoub, A.E.; Weinberg, R.A. Chemokine networks and breast cancer metastasis. Breast Dis. 2006, 26, 75–85. [Google Scholar] [CrossRef]
- Yu, J.L.; Rak, J.W. Host microenvironment in breast cancer development: Inflammatory and immune cells in tumour angiogenesis and arteriogenesis. Breast Cancer Res. 2003, 5, 83–88. [Google Scholar] [CrossRef]
- Müller, A.; Homey, B.; Soto, H.; Ge, N.; Catron, D.; Buchanan, M.E.; McClanahan, T.; Murphy, E.; Yuan, W.; Wagner, S.N.; et al. Involvement of chemokine receptors in breast cancer metastasis. Nature 2001, 410, 50–56. [Google Scholar] [CrossRef]
- Dvorak, H.F. Tumors: Wounds that do not heal. Similarities between tumor stroma generation and wound healing. N. Engl. J. Med. 1986, 315, 1650.e9. [Google Scholar] [CrossRef]
- Fat Transfer/Fat Graft and Fat Injection ASPS Guiding Principles. Available online: www.plasticsurgery.org (accessed on 26 May 2024).

| Patients (No.) | LRR (No) | LRR (%) | |
|---|---|---|---|
| MST/BCS + AFG | 7619 | 240 | 3.15% |
| MST/BCS | 6459 | 342 | 5.30% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lo Torto, F.; Patanè, L.; Abbaticchio, D.; Pagnotta, A.; Ribuffo, D. Autologous Fat Grafting (AFG): A Systematic Review to Evaluate Oncological Safety in Breast Cancer Patients. J. Clin. Med. 2024, 13, 4369. https://doi.org/10.3390/jcm13154369
Lo Torto F, Patanè L, Abbaticchio D, Pagnotta A, Ribuffo D. Autologous Fat Grafting (AFG): A Systematic Review to Evaluate Oncological Safety in Breast Cancer Patients. Journal of Clinical Medicine. 2024; 13(15):4369. https://doi.org/10.3390/jcm13154369
Chicago/Turabian StyleLo Torto, Federico, Luca Patanè, Donato Abbaticchio, Alessia Pagnotta, and Diego Ribuffo. 2024. "Autologous Fat Grafting (AFG): A Systematic Review to Evaluate Oncological Safety in Breast Cancer Patients" Journal of Clinical Medicine 13, no. 15: 4369. https://doi.org/10.3390/jcm13154369
APA StyleLo Torto, F., Patanè, L., Abbaticchio, D., Pagnotta, A., & Ribuffo, D. (2024). Autologous Fat Grafting (AFG): A Systematic Review to Evaluate Oncological Safety in Breast Cancer Patients. Journal of Clinical Medicine, 13(15), 4369. https://doi.org/10.3390/jcm13154369





