A Systematic Review and Narrative Synthesis of Cognitive Training in the Treatment of Mental Illness and Substance Use Disorder
Abstract
1. Introduction
2. Aims
2.1. Primary Aims
- To evaluate the impact of CT on cognitive outcomes in people with a psychiatric disorder other than schizophrenia.
2.2. Secondary Aims
- To evaluate the impact of CT on clinical outcomes (e.g., psychosocial function, depression, or substance use) in people with a psychiatric disorder other than schizophrenia.
- To determine the differential impacts of CT across psychiatric diagnoses.
- To identify whether specific CT characteristics or formats provide superior outcomes.
3. Materials and Methods
3.1. Eligibility Criteria
3.1.1. Participants
3.1.2. Interventions
3.1.3. Study Type
3.1.4. Outcomes
3.2. Search Strategy
3.3. Study Selection
3.4. Quality Assessment
3.5. Data Extraction
4. Results
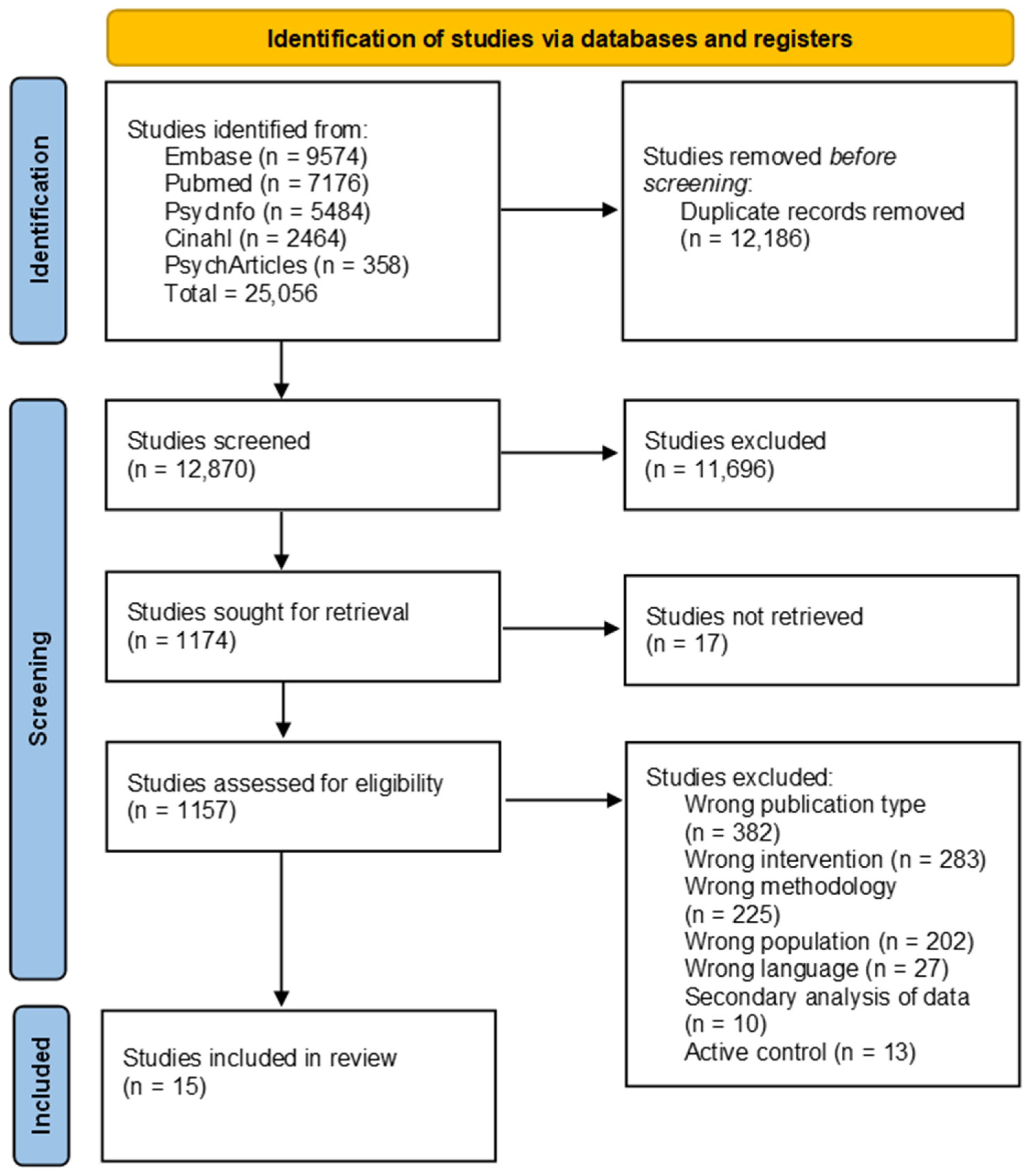
4.1. Study Selection
4.2. Study Characteristics
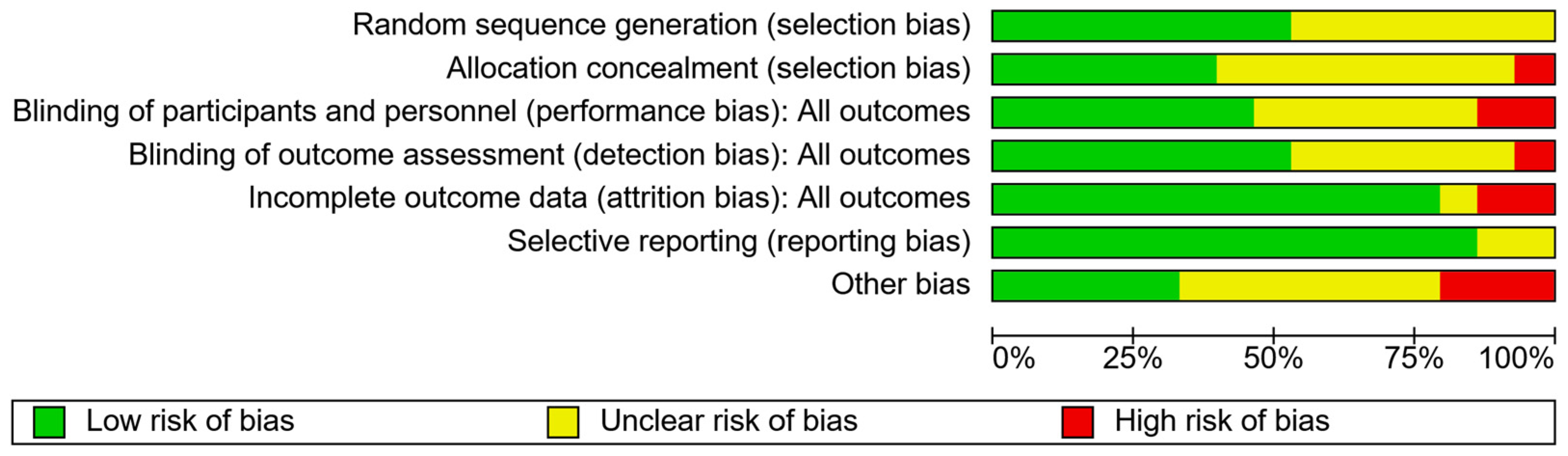
4.3. Risk of Bias
4.4. CT Characteristics
4.5. Cognitive Domains
4.6. Cognitive Outcomes
4.7. Clinical Outcomes
4.8. Duration
5. Discussion
6. Strengths and Limitations
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Girotti, M.; Adler, S.M.; Bulin, S.E.; Fucich, E.A.; Paredes, D.; Morilak, D.A. Prefrontal cortex executive processes affected by stress in health and disease. Prog. Neuropsychopharmacol. Biol. Psychiatry 2018, 85, 161–179. [Google Scholar] [CrossRef] [PubMed]
- Keshavan, M.S.; Vinogradov, S.; Rumsey, J.; Sherrill, J.; Wagner, A. Cognitive training in mental disorders: Update and future directions. Am. J. Psychiatry 2014, 171, 510–522. [Google Scholar] [CrossRef] [PubMed]
- Trapp, W.; Heid, A.; Röder, S.; Wimmer, F.; Hajak, G. Cognitive Remediation in Psychiatric Disorders: State of the Evidence, Future Perspectives, and Some Bold Ideas. Brain Sci. 2022, 12, 683. [Google Scholar] [CrossRef] [PubMed]
- Bowie, C.R.; Bell, M.D.; Fiszdon, J.M.; Johannesen, J.K.; Lindenmayer, J.P.; McGurk, S.R.; Medalia, A.A.; Penadés, R.; Saperstein, A.M.; Twamley, E.W.; et al. Cognitive remediation for schizophrenia: An expert working group white paper on core techniques. Schizophr. Res. 2020, 215, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Segal, A.; Parkes, L.; Aquino, K.; Kia, S.M.; Wolfers, T.; Franke, B.; Hoogman, M.; Beckmann, C.F.; Westlye, L.T.; Andreassen, O.A.; et al. Regional, circuit and network heterogeneity of brain abnormalities in psychiatric disorders. Nat. Neurosci. 2023, 26, 1613–1629. [Google Scholar] [CrossRef]
- Tu, P.C.; Chang, W.C.; Chen, M.H.; Hsu, J.W.; Lin, W.C.; Li, C.T.; Su, T.P.; Bai, Y.M. Identifying common and distinct subcortical volumetric abnormalities in 3 major psychiatric disorders: A single-site analysis of 640 participants. J. Psychiatry Neurosci. 2022, 47, E230–E238. [Google Scholar] [CrossRef] [PubMed]
- Walton, C.C.; Kavanagh, A.; Downey, L.A.; Lomas, J.; Camfield, D.A.; Stough, C. Online cognitive training in healthy older adults: A preliminary study on the effects of single versus multi-domain training. Transl. Neurosci. 2015, 6, 13–19. [Google Scholar] [CrossRef] [PubMed]
- ten Brinke, L.F.; Davis, J.C.; Barha, C.K.; Liu-Ambrose, T. Effects of computerized cognitive training on neuroimaging outcomes in older adults: A systematic review. BMC Geriatr. 2017, 17, 139. [Google Scholar] [CrossRef]
- Cao, X.; Yao, Y.; Li, T.; Cheng, Y.; Feng, W.; Shen, Y.; Li, Q.; Jiang, L.; Wu, W.; Wang, J.; et al. The Impact of Cognitive Training on Cerebral White Matter in Community-Dwelling Elderly: One-Year Prospective Longitudinal Diffusion Tensor Imaging Study. Sci. Rep. 2016, 6, 33212. [Google Scholar] [CrossRef][Green Version]
- Li, J.Y.; Wu, H.; Yuan, S.; Wang, C.; Wang, Q.; Zhong, Y.; Zhang, N.; Heffner, K.; Fox, P.T. A meta-analysis on neural changes of cognitive training for mental disorders in executive function tasks: Increase or decrease brain activation? BMC Psychiatry 2022, 22, 155. [Google Scholar] [CrossRef]
- Kriesche, D.; Woll, C.F.J.; Tschentscher, N.; Engel, R.R.; Karch, S. Neurocognitive deficits in depression: A systematic review of cognitive impairment in the acute and remitted state. Eur. Arch. Psychiatry Clin. Neurosci. 2023, 273, 1105–1128. [Google Scholar] [CrossRef] [PubMed]
- Bruning, A.L.; Mallya, M.M.; Lewis-Peacock, J.A. Rumination burdens the updating of working memory. Atten. Percept. Psychophys. 2023, 85, 1452–1460. [Google Scholar] [CrossRef]
- Kovács, L.N.; Takacs, Z.K.; Tóth, Z.; Simon, E.; Schmelowszky, Á.; Kökönyei, G. Rumination in major depressive and bipolar disorder—A meta-analysis. J. Affect. Disord. 2020, 276, 1131–1141. [Google Scholar] [CrossRef]
- Pan, D.N.; Hoid, D.; Gu, R.L.; Li, X. Emotional working memory training reduces rumination and alters the EEG microstate in anxious individuals. Neuroimage Clin. 2020, 28, 102488. [Google Scholar] [CrossRef] [PubMed]
- Onraedt, T.; Koster, E.H. Training working memory to reduce rumination. PLoS ONE 2014, 9, e90632. [Google Scholar] [CrossRef] [PubMed]
- Woolridge, S.M.; Harrison, G.W.; Best, M.W.; Bowie, C.R. Attention bias modification in depression: A randomized trial using a novel, reward-based, eye-tracking approach. J. Behav. Ther. Exp. Psychiatry 2021, 71, 101621. [Google Scholar] [CrossRef]
- Field, M.; Mogg, K.; Mann, B.; Bennett, G.A.; Bradley, B.P. Attentional biases in abstinent alcoholics and their association with craving. Psychol. Addict. Behav. 2013, 27, 71–80. [Google Scholar] [CrossRef]
- Heitmann, J.; Bennik, E.C.; van Hemel-Ruiter, M.E.; de Jong, P.J. The effectiveness of attentional bias modification for substance use disorder symptoms in adults: A systematic review. Syst. Rev. 2018, 7, 160. [Google Scholar] [CrossRef]
- Xia, H.S.; Li, Y.X.; Zhang, Q.Y.; Zhong, D.L.; Liu, X.B.; Gou, X.Y.; Fan, J.; Zhao, J.; Zhang, Y.; Ai, S.C.; et al. Attention bias modification for depression: A systematic review and meta-analysis. Front. Psychiatry 2023, 14, 1098610. [Google Scholar] [CrossRef]
- Rudner, T.; Hume, D.J.; Larmuth, K.; Atterbury, E.; Rauch, H.G.L.; Kroff, J. Substance use disorder and obesogenic eating: Does working memory training strengthen ability to abstain from unwanted behaviors? A systematic review. J. Subst. Abus. Treat. 2022, 137, 108689. [Google Scholar] [CrossRef]
- McCabe, D.P.; Roediger, H.L.; McDaniel, M.A.; Balota, D.A.; Hambrick, D.Z. The relationship between working memory capacity and executive functioning: Evidence for a common executive attention construct. Neuropsychology 2010, 24, 222–243. [Google Scholar] [CrossRef]
- Roberts, M.E.; Tchanturia, K.; Stahl, D.; Southgate, L.; Treasure, J. A systematic review and meta-analysis of set-shifting ability in eating disorders. Psychol. Med. 2007, 37, 1075–1084. [Google Scholar] [CrossRef] [PubMed]
- Stott, N.; Fox, J.R.E.; Williams, M.O. Attentional bias in eating disorders: A meta-review. Int. J. Eat. Disord. 2021, 54, 1377–1399. [Google Scholar] [CrossRef] [PubMed]
- Gruner, P.; Pittenger, C. Cognitive inflexibility in Obsessive-Compulsive Disorder. Neuroscience 2017, 345, 243–255. [Google Scholar] [CrossRef] [PubMed]
- Hagan, K.E.; Christensen, K.A.; Forbush, K.T. A preliminary systematic review and meta-analysis of randomized-controlled trials of cognitive remediation therapy for anorexia nervosa. Eat. Behav. 2020, 37, 101391. [Google Scholar] [CrossRef] [PubMed]
- Buhlmann, U.; Deckersbach, T.; Engelhard, I.; Cook, L.M.; Rauch, S.L.; Kathmann, N.; Wilhelm, S.; Savage, C.R. Cognitive retraining for organizational impairment in obsessive-compulsive disorder. Psychiatry Res. 2006, 144, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Park, H.S.; Shin, Y.W.; Ha, T.H.; Shin, M.S.; Kim, Y.Y.; Lee, Y.H.; Kwon, J.S. Effect of cognitive training focusing on organizational strategies in patients with obsessive-compulsive disorder. Psychiatry Clin. Neurosci. 2006, 60, 718–726. [Google Scholar] [CrossRef] [PubMed]
- Weng, W.; Liang, J.; Xue, J.; Zhu, T.; Jiang, Y.; Wang, J.; Chen, S. The Transfer Effects of Cognitive Training on Working Memory Among Chinese Older Adults with Mild Cognitive Impairment: A Randomized Controlled Trial. Front. Aging Neurosci. 2019, 11, 212. [Google Scholar] [CrossRef] [PubMed]
- Kelly, M.E.; Loughrey, D.; Lawlor, B.A.; Robertson, I.H.; Walsh, C.; Brennan, S. The impact of cognitive training and mental stimulation on cognitive and everyday functioning of healthy older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2014, 15, 28–43. [Google Scholar] [CrossRef]
- Ripp, I.; Emch, M.; Wu, Q.; Lizarraga, A.; Udale, R.; von Bastian, C.C.; Koch, K.; Yakushev, I. Adaptive working memory training does not produce transfer effects in cognition and neuroimaging. Transl. Psychiatry 2022, 12, 512. [Google Scholar] [CrossRef]
- Grynszpan, O.; Perbal, S.; Pelissolo, A.; Fossati, P.; Jouvent, R.; Dubal, S.; Perez-Diaz, F. Efficacy and specificity of computer-assisted cognitive remediation in schizophrenia: A meta-analytical study. Psychol. Med. 2011, 41, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Wykes, T.; Huddy, V.; Cellard, C.; McGurk, S.R.; Czobor, P. A meta-analysis of cognitive remediation for schizophrenia: Methodology and effect sizes. Am. J. Psychiatry 2011, 168, 472–485. [Google Scholar] [CrossRef] [PubMed]
- Vita, A.; Barlati, S.; Ceraso, A.; Nibbio, G.; Durante, F.; Facchi, M.; Deste, G.; Wykes, T. Durability of Effects of Cognitive Remediation on Cognition and Psychosocial Functioning in Schizophrenia: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Am. J. Psychiatry 2024, 181, 520–531. [Google Scholar] [CrossRef] [PubMed]
- Revell, E.; Neill, J.; Harte, M.; Khan, Z.; Drake, R. A systematic review and meta-analysis of cognitive remediation in early schizophrenia. Schizophr. Res. 2015, 168, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Tsapekos, D.; Seccomandi, B.; Mantingh, T.; Cella, M.; Wykes, T.; Young, A.H. Cognitive enhancement interventions for people with bipolar disorder: A systematic review of methodological quality, treatment approaches, and outcomes. Bipolar Disord. 2020, 22, 216–230. [Google Scholar] [CrossRef]
- Zhang, H.; Huntley, J.; Bhome, R.; Holmes, B.; Cahill, J.; Gould, R.L.; Wang, H.; Yu, X.; Howard, R. Effect of computerised cognitive training on cognitive outcomes in mild cognitive impairment: A systematic review and meta-analysis. BMJ Open 2019, 9, e027062. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef] [PubMed]
- Bowie, C.R.; Gupta, M.; Holshausen, K.; Jokic, R.; Best, M.; Milev, R. Cognitive remediation for treatment-resistant depression: Effects on cognition and functioning and the role of online homework. J. Nerv. Ment. Dis. 2013, 201, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Wang, Y.; Feng, T.; Prudic, J. Cognitive training to improve memory in individuals undergoing electroconvulsive therapy: Negative findings. J. Psychiatr. Res. 2017, 92, 8–14. [Google Scholar] [CrossRef]
- Klojčnik, M.; Bakracevic, K. The effectiveness of computerized cognitive remediation therapy (CCRT) for deficits in attention and executive functions in depression: A pilot study. Appl. Neuropsychol. Adult 2023, 30, 306–314. [Google Scholar] [CrossRef]
- Listunova, L.; Kienzle, J.; Bartolovic, M.; Jaehn, A.; Grützner, T.M.; Wolf, R.C.; Aschenbrenner, S.; Weisbrod, M.; Roesch-Ely, D. Cognitive remediation therapy for partially remitted unipolar depression: A single-blind randomized controlled trial. J. Affect Disord. 2020, 276, 316–326. [Google Scholar] [CrossRef] [PubMed]
- Neshat-Doost, H.T.; Dalgleish, T.; Yule, W.; Kalantari, M.; Ahmadi, S.J.; Dyregrov, A.; Jobson, L. Enhancing Autobiographical Memory Specificity Through Cognitive Training: An Intervention for Depression Translated From Basic Science. Clin. Psychol. Sci. 2013, 1, 84–92. [Google Scholar] [CrossRef]
- Trapp, W.; Engel, S.; Hajak, G.; Lautenbacher, S.; Gallhofer, B. Cognitive remediation for depressed inpatients: Results of a pilot randomized controlled trial. Aust. N. Z. J. Psychiatry 2016, 50, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.J.; Wiemerslage, L.; Burch, K.; Maiorana, S.; Cocolas, E.; Schiöth, H.; Kamaloodien, K.; Stein, D. The impact of cognitive training in substance use disorder: The effect of working memory training on impulse control in methamphetamine users. Psychopharmacology 2017, 234, 1911–1921. [Google Scholar] [CrossRef] [PubMed]
- Gamito, P.; Oliveira, J.; Matias, M.; Cunha, E.; Brito, R.; Lopes, P.F.; Deus, A. Virtual Reality Cognitive Training Among Individuals with Alcohol Use Disorder Undergoing Residential Treatment: Pilot Randomized Controlled Trial. J. Med. Internet Res. 2021, 23, e18482. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Jiang, H.; Su, H.; Zhong, N.; Li, R.; Li, X.; Chen, T.; Tan, H.; Du, J.; Xu, D.; et al. A Newly Designed Mobile-Based Computerized Cognitive Addiction Therapy App for the Improvement of Cognition Impairments and Risk Decision Making in Methamphetamine Use Disorder: Randomized Controlled Trial. JMIR Mhealth Uhealth 2018, 6, e10292. [Google Scholar] [CrossRef] [PubMed]
- Demant, K.M.; Vinberg, M.; Kessing, L.V.; Miskowiak, K.W. Effects of Short-Term Cognitive Remediation on Cognitive Dysfunction in Partially or Fully Remitted Individuals with Bipolar Disorder: Results of a Randomised Controlled Trial. PLoS ONE. 2015, 10, e0127955. [Google Scholar] [CrossRef] [PubMed]
- Strawbridge, R.; Tsapekos, D.; Hodsoll, J.; Mantingh, T.; Yalin, N.; McCrone, P.; Boadu, J.; Macritchie, K.; Cella, M.; Reeder, C.; et al. Cognitive remediation therapy for patients with bipolar disorder: A randomised proof-of-concept trial. Bipolar Disord. 2021, 23, 196–208. [Google Scholar] [CrossRef] [PubMed]
- Torrent, C.; Bonnin Cdel, M.; Martínez-Arán, A.; Valle, J.; Amann, B.L.; González-Pinto, A.; Crespo, J.M.; Ibáñez, Á.; Garcia-Portilla, M.P.; Tabarés-Seisdedos, R.; et al. Efficacy of functional remediation in bipolar disorder: A multicenter randomized controlled study. Am. J. Psychiatry 2013, 170, 852–859. [Google Scholar] [CrossRef]
- Dingemans, A.E.; Danner, U.N.; Donker, J.M.; Aardoom, J.J.; van Meer, F.; Tobias, K.; van Elburg, A.A.; van Furth, E.F. The effectiveness of cognitive remediation therapy in patients with a severe or enduring eating disorder: A randomized controlled trial. Psychother. Psychosom. 2014, 83, 29–36. [Google Scholar] [CrossRef]
- Sproch, L.E.; Anderson, K.P.; Sherman, M.F.; Crawford, S.F.; Brandt, H.A. A randomized controlled trial of group cognitive remediation therapy for anorexia nervosa: Effects on set-shifting tasks for inpatient adults and adolescents. Int. J. Eat Disord. 2019, 52, 1004–1014. [Google Scholar] [CrossRef] [PubMed]
- Naismith, S.L.; Diamond, K.; Carter, P.E.; Norrie, L.M.; Redoblado-Hodge, M.A.; Lewis, S.J.; Hickie, I.B. Enhancing memory in late-life depression: The effects of a combined psychoeducation and cognitive training program. Am. J. Geriatr. Psychiatry 2011, 19, 240–248. [Google Scholar] [CrossRef]
- Naismith, S.L.; Redoblado-Hodge, M.A.; Lewis, S.J.; Scott, E.M.; Hickie, I.B. Cognitive training in affective disorders improves memory: A preliminary study using the NEAR approach. J. Affect. Disord. 2010, 121, 258–262. [Google Scholar] [CrossRef]
- Brockmeyer, T.; Schmidt, H.; Leiteritz-Rausch, A.; Zimmermann, J.; Wünsch-Leiteritz, W.; Leiteritz, A.; Friederich, H.C. Cognitive remediation therapy in anorexia nervosa-A randomized clinical trial. J. Consult Clin. Psychol. 2021, 89, 805–815. [Google Scholar] [CrossRef]
- Tang, H.; Riley, M.R.; Singh, B.; Qi, X.-L.; Blake, D.T.; Constantinidis, C. Prefrontal cortical plasticity during learning of cognitive tasks. Nat. Commun. 2022, 13, 90. [Google Scholar] [CrossRef]
- Kim, J.; Andrews-Hanna, J.R.; Eisenbarth, H.; Lux, B.K.; Kim, H.J.; Lee, E.; Lindquist, M.A.; Losin, E.A.R.; Wager, T.D.; Woo, C.-W. A dorsomedial prefrontal cortex-based dynamic functional connectivity model of rumination. Nat. Commun. 2023, 14, 3540. [Google Scholar] [CrossRef]
- Hu, S.; Li, X.-J.; Law, S.; Shen, C.-Y.; Yao, G.-Q.; Zhang, X.-Q.; Li, J.; Chen, G.-F.; Xu, B.; Liu, X.-M.; et al. Prefrontal cortex alterations in major depressive disorder, generalized anxiety disorder and their comorbidity during a verbal fluency task assessed by multi-channel near-infrared spectroscopy. Psychiatry Res. 2021, 306, 114229. [Google Scholar] [CrossRef]
- Fals-Stewart, W.; Lam, W.K. Computer-assisted cognitive rehabilitation for the treatment of patients with substance use disorders: A randomized clinical trial. Exp Clin Psychopharmacol. 2010, 18, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Rezapour, T.; Hatami, J.; Farhoudian, A.; Sofuoglu, M.; Noroozi, A.; Daneshmand, R.; Samiei, A.; Ekhtiari, H. Cognitive rehabilitation for individuals with opioid use disorder: A randomized controlled trial. Neuropsychol. Rehabil. 2019, 29, 1273–1289. [Google Scholar] [CrossRef] [PubMed]
- Smoski, M.J.; LaBar, K.S.; Steffens, D.C. Relative Effectiveness of Reappraisal and Distraction in Regulating Emotion in Late-Life Depression. Am. J. Geriatr. Psychiatry 2014, 22, 898–907. [Google Scholar] [CrossRef]
- Clausen, A.N.; Thelen, J.; Francisco, A.J.; Bruce, J.; Martin, L.; McDowd, J.; Aupperle, R.L. Computer-Based Executive Function Training for Combat Veterans With PTSD: A Pilot Clinical Trial Assessing Feasibility and Predictors of Dropout. Front. Psychiatry 2019, 10, 62. [Google Scholar] [CrossRef] [PubMed]
- Boot, W.; Simons, D.; Stothart, C.; Stutts Berry, C. The Pervasive Problem with Placebos in Psychology Why Active Control Groups Are Not Sufficient to Rule Out Placebo Effects. Perspect. Psychol. Sci. 2013, 8, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Au, J.; Gibson, B.C.; Bunarjo, K.; Buschkuehl, M.; Jaeggi, S.M. Quantifying the Difference between Active and Passive Control Groups in Cognitive Interventions Using two Meta-Analytical Approaches. J. Cogn. Enhanc. 2020, 4, 192–210. [Google Scholar] [CrossRef] [PubMed]
| Author, Year | Study Characteristics | Training/Intervention Characteristics | Study Outcomes | |||||
|---|---|---|---|---|---|---|---|---|
| Country | Sample N; Age (SD); Female | Diagnosis (Criteria) | Intervention | Format | Duration (Minutes) and Frequency | Training Tasks | Main Findings | |
| Bowie, 2013 [38] | Canada | N = 33 outpatients I: n = 17; 49.2 (11.8); F = 11 C: n = 16; 42.2 (13.4); F = 12 | Treatment-resistant MDD | Scientific Brain Training Pro Control—Wait list | Group, computerised | Length: 90 Sessions: 10 Weeks: 10 | Exercises with adaptive difficulty and strategy coaching, targeting processing speed, attention, working memory, delayed memory, and EF. | ↑Attention and processing speed (p = 0.012) ↑Verbal memory (p = 0.023) EF (ns) Social function (ns) |
| Choi, 2017 [39] | USA | N = 59 inpatients I: n = 21; 39.0 (12.7); F = 12. C1: n = 20; 41.7 (14.4); F = 12. C2: n = 18; 48.2 (10.8); F = 8. | MDD (DSM-IV) | Memory training for ECT (Mem-ECT) Control (C1)-TAU | Pen-and-paper, computerised | Length: 60–75 Sessions: 7 Weeks: 3 | Memory strategies and skills. | Cognitive status (ns) Memory (ns) Subjective cognition (ns) Quality of life (ns) Depression (ns) |
| Klojčnik, 2023 [40] | Slovenia | N = 20 outpatients I: n = 10; 43.6 (11.5), F = 6 C: n = 10; 47.0 (9.2); F = 6 | Depression (ICD 10) | Cogniplus Control-TAU | Therapist-led, computerised | Length: 40–50 Sessions: 12 Weeks: 10 | Tasks with adaptive difficulty, training attention, and EF. | ↑EF (p < 0.000 to 0.021) ↑Attentional performance (p < 0.000 to p = 0.007) ↓Depression (p = 0.006) ↑Self-reported cognition subscales of shifting, emotional control, initiate: (p < 0.000) Self-reported cognition subscales of inhibition (ns) working memory (ns) Planning (ns) |
| Listunova, 2020 [41] | Germany | N = 57 community members aged 18–60. I (GT): n = 18; 45.3 (15.1); F = 14 I (IT): n = 20; 45.9 (11.3); F = 15 C: n = 19; 44.9 (10.3); F = 13 | MDD (DSM-IV) | Cogniplus GT (generalised training): trained all cognitive domains IT (individualised training): trained three worst domains Control—no care | Computerised + therapist-led sessions. | Length: 60 Sessions: 12–15 Weeks: 5 | Tasks with adaptive difficulty, training attention, alertness, working memory, inhibition, planning + weekly transfer sessions with psychoeducation on cognition and strategy training. | No difference between GT and IT. ↑Psychosocial function (p = 0.014) ↑Attention (p = 0.014) Information processing (ns) EF (ns) Learning and memory (ns) Depression (ns) |
| Neshat-Doost, 2013 [42] | Iran | N = 23 adolescent students I: n = 12; 15.3 (1.7); F = 6 C: n = 11; 15.5 (2.1); F = 5 | Depression (MFQ) | Memory specificity training (MEST) Control—no care | Group, therapist-led | Length: 80 Sessions: 5 Weeks: 5 | Memory education, training, and practice. | ↑Retrieval of specific autobiographical memories (p < 0.01). ↓Depression at 2-months follow-up (p = 0.04). Autobiographical memory specificity predicted follow-up depression (p < 0.01). |
| Trapp, 2016 [43] | Germany | N = 46 inpatients I: n = 23; 34.26 (11.60); F = 14 C: n = 23; 36.87 (12.14); F = 17 | Depression (DSM-IV and ICD-10) | X-Cog Control-TAU | Group, therapist-led, computerised training. | Length: 60 Sessions: 12 Weeks: 4 | Game-like tasks with increasing difficulty and strategy development, targeting visuomotor, memory, EF, attention. | ↑Working memory (p = 0.030) ↑Memory (p = 0.006) ↑Cognitive flexibility (p = 0.019) Depression (ns) |
| Brooks, 2017 [44] | South Africa | N = 35 inpatients I: n = 20; 29.83 (7.32) Control: n = 15; 28.11 (6.01) | Methamphetamine use disorder | Curb Your Addiction Control—TAU | Group, therapist-led, computerised. | Length: 30 Sessions: 20 Weeks: 4 | N-back task, training working memory with adaptive difficulty. | Mood (ns) Craving (ns) Self-control (ns) Impulsivity (ns) Self-regulation (ns) Anxiety (ns) Depression (ns) Executive function (ns) |
| Gamito, 2021 [45] | Portugal | N = 36 adult residential patients, F = 6. I: n = 19; 40.0, (9.2) C: n = 17 51.0 (12.3) | Alcohol use disorder | Systemic Lisbon Battery (SLB) Control—TAU | Individual, therapist-led sessions. | Length: 30–40 Sessions: 10 Weeks: 5 | Virtual reality (VR)-based cognitive intervention targeting memory, attention, and EF in real-life scenarios | ↑Attention (p = 0.03 to p = 0.02). ↑Cognitive flexibility (p = 0.001) Visual perception (ns) Memory (ns) |
| Zhu, 2018 [46] | China | N = 40 Male inpatients I: n = 20; 32.7 (5.3) C: n = 20; 35.1 (8.0) | Methamphetamine use disorder (DSM-V) | Mobile-based computerised cognitive addiction therapy App Control—TAU | Independent, computerised training. | Length: 60 Sessions: 20 Weeks: 4 | Working memory and attentional bias training plus relaxation. | ↑Verbal learning and memory (p < 0.001) ↑Spatial working memory (p < 0.001) ↑Decision making (p < 0.001) ↑Risk taking (p < 0.001) Problem-solving (ns) Attentional bias (ns) |
| Demant, 2015 [47] | Demark | N = 40 outpatients aged 18–50. I: n = 18; 33.9 (6.8); F = 12 C: n = 22; 34.0(7.9); F = 13 | Partially of fully remitted Bipolar (ICD-10) | RehaCom Control—TAU | Group, therapist education and computerised training | Length: 120 Sessions: 12 Weeks: 12 | Computer tasks plus psychoeducation strategy training targeting memory, attention, and EF. | ↑Verbal fluency (p = 0.005) and quality of life (p = 0.048) at 12 weeks follow-up. Verbal memory (ns) Attention (ns) EF (ns) Psychosocial function (ns) Psychomotor speed (ns) |
| Strawbridge, 2020 [48] | England | N = 60 community members aged 18–65. I: n = 29; median (IQR) = 43 (34, 52.5); F = 21 Control: n = 31; median (IQR) 42.5 (31.8, 52.2); F = 20 | Bipolar | CIRCuiTS Control—TAU | Therapist-led, computerised training. | Sessions: ~36 Weeks: 12 Minimum 20 h of training | Drill and practice tasks plus strategy-based approaches targeting attention, memory, and executive function. | Week 13: ↑Working memory (p = 0.024) ↑IQ (p = 0.015) ↑Executive function (p = 0.027) ↑Functional capacity (p = 0.015) ↑Psychosocial functioning (p = 0.004) ↑Goal attainment (p < 0.001) Week 25: ↑Processing speed and attention (p < 0.05) ↑Working memory (p = 0.001) ↑Verbal memory (p = 0.007) ↑IQ (p = 0.001) ↑Verbal fluency (p = 0.004) ↑Executive function (p = 0.003) ↑Global cognition (p = 0.001) ↑Psychosocial functioning (p = 0.002) ↑Goal attainment (p = 0.001) |
| Torrent, 2013 [49] | Spain | N = 239 outpatients aged 18–55. I1: n = 77; 40.6 (9.1) I2: n = 82; mean age = 39.3 (8.9) C: n = 80, 40.5 (8.7) | Bipolar in remission (DSM-IV) | Functional remediation Control—TAU I1: Functional remediation I2: Psychoeducation | Group, pen-and-paper | Length: 90 Sessions: 21 Weeks: 21 | Training and strategy coaching targeting attention, memory, problem-solving, multitasking, and organisation. | ↑Functioning compared to TAU (p = 0.002) but not compared to psychoeducation (p = 0.056). Improvements were seen in ‘interpersonal’ and ‘occupational’ domains of function. Executive function (ns) Set shifting (ns) Planning (ns) Inhibition (ns) Verbal fluency (ns) Memory (ns) Attention (ns) |
| Dingemans, 2014 [50] | Netherlands | N = 82 female inpatients aged 17–53. I: n = 41; 26 (22) C: n = 41; 23 (21) | Anorexia Nervosa (DSM-IV) | Manualised cognitive remediation therapy for AN Control—TAU | Therapist-led, individual, pen-and-paper sessions. | Length: 45 Sessions: 10 Weeks: 6 | Exercises, pychoeducation, strategy coaching, and reflection target cognitive flexibility and information processing. | ↓EDQoL at 6 weeks (p < 0.05) ↓EDEQ at 6 months (p < 0.05) BMI (ns) Quality of life (ns) Depression (ns) Anxiety (ns) Self-esteem (ns) Perfectionism (ns) Motivation to change (ns) Neuropsychological functioning (ns) |
| Sproch, 2019 [51] | USA | N = 275 inpatients I: n = 135; 23.9 (12.8); F = 121 C: n = 140; 22.2 (12.8); F = 129 | Anorexia Nervosa (DSM-IV) | Manualised cognitive remediation therapy for AN Control—TAU | Therapist-led, group, pen-and-paper sessions. | Length: 60 Sessions: 5 Weeks: 3 | Exercises, pychoeducation, strategy coaching, and reflection targeting cognitive flexibility. | Executive function (ns) Cognitive flexibility (ns) Age by group analysis provided evidence that adults may benefit more than children from CRT on cognitive flexibility. |
| Park, 2006 [27] | N = 30 outpatients I: n = 15; 30.5 (10.4); F = 5 C: n = 15; 28.1 (6.8); F = 4 | OCD (DSM-IV) | Revised block design subtest of K-WAIS. | Therapist-led | Length: 60 Session: 9 Weeks: 5 | Training of organisational strategies. | ↑Visuospatial construction ability (p < 0.05) ↑Visuospatial memory (p < 0.01 to p < 0.05) Verbal learning and memory (ns) Better performance for control condition on trial B recall. ↓Obsessions (F = 13.7, p < 0.01) ↓Compulsions (F = 6.8, p < 0.05) ↓OCD symptom severity (F = 19.8, p < 0.001) Depression (ns) Anxiety (ns) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gillespie, K.M.; Dymond, A.H.; Li, X.; Schweitzer, D.; Branjerdporn, G.; Khan, S.; Hii, Q.; Keller, S.; Bartlett, S.E. A Systematic Review and Narrative Synthesis of Cognitive Training in the Treatment of Mental Illness and Substance Use Disorder. J. Clin. Med. 2024, 13, 4348. https://doi.org/10.3390/jcm13154348
Gillespie KM, Dymond AH, Li X, Schweitzer D, Branjerdporn G, Khan S, Hii Q, Keller S, Bartlett SE. A Systematic Review and Narrative Synthesis of Cognitive Training in the Treatment of Mental Illness and Substance Use Disorder. Journal of Clinical Medicine. 2024; 13(15):4348. https://doi.org/10.3390/jcm13154348
Chicago/Turabian StyleGillespie, Kerri M., Alexander H. Dymond, Xin Li, Daniel Schweitzer, Grace Branjerdporn, Saleha Khan, Quang Hii, Suzie Keller, and Selena E. Bartlett. 2024. "A Systematic Review and Narrative Synthesis of Cognitive Training in the Treatment of Mental Illness and Substance Use Disorder" Journal of Clinical Medicine 13, no. 15: 4348. https://doi.org/10.3390/jcm13154348
APA StyleGillespie, K. M., Dymond, A. H., Li, X., Schweitzer, D., Branjerdporn, G., Khan, S., Hii, Q., Keller, S., & Bartlett, S. E. (2024). A Systematic Review and Narrative Synthesis of Cognitive Training in the Treatment of Mental Illness and Substance Use Disorder. Journal of Clinical Medicine, 13(15), 4348. https://doi.org/10.3390/jcm13154348





