Assessment of Obesity as Risk Factor of Lumbar Disc Surgery: Retrospective Analysis of 598 Cases and Simulated Surgery on 3D-Printed Models
Abstract
:1. Introduction
2. Materials and Methods
2.1. Evaluation of Obesity-Dependent Complications and Surgery Duration
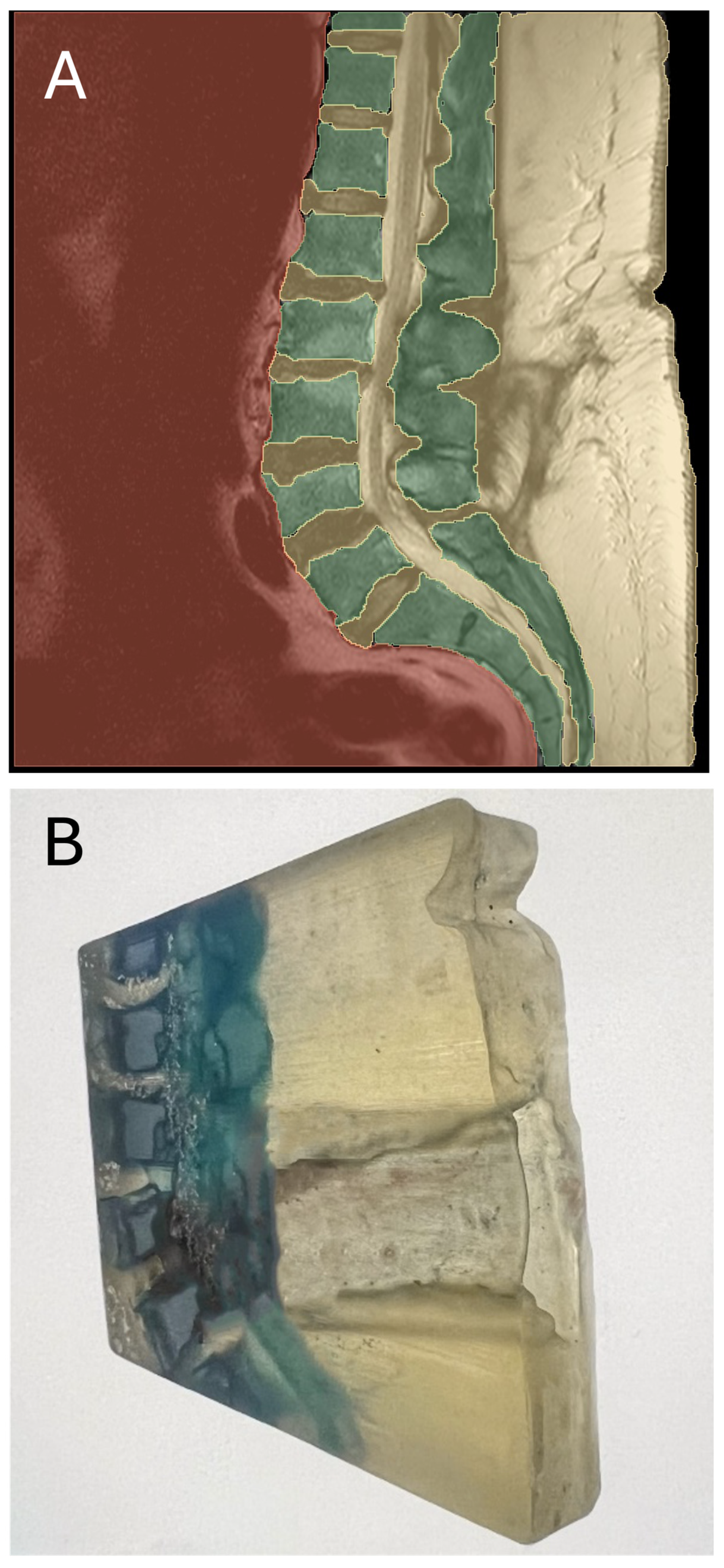
2.2. Creation of 3D-Printed Models
2.3. Simulation of a Herniated Disc Operation
2.4. Questionnaire-Based Assessment of the Simulation Process
2.5. Statistics
3. Results
3.1. Evaluation of Obesity-Dependent Complications and Surgery Duration
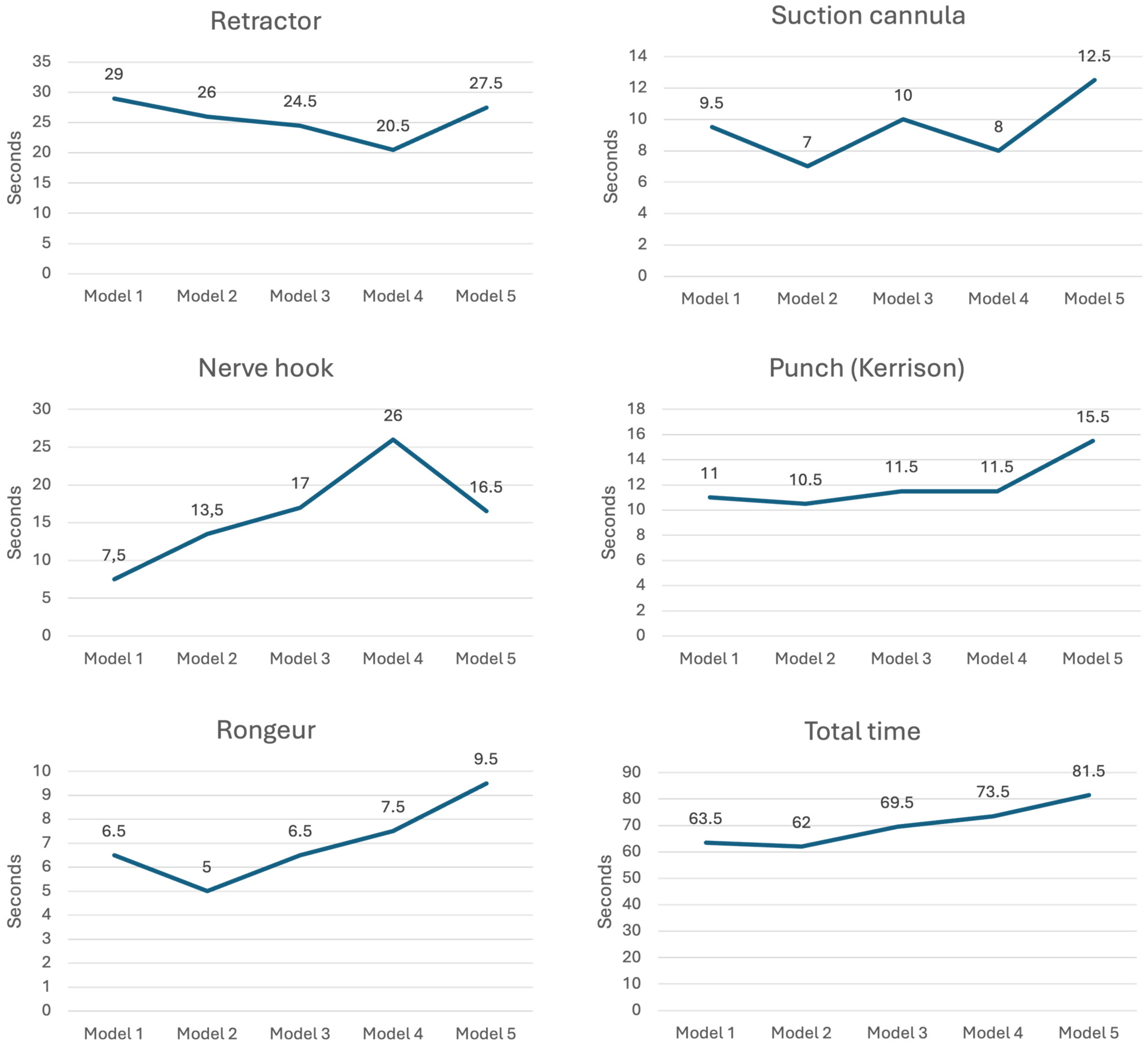
3.2. Simulation of Surgeries using 3D-Printed Models
3.3. Questionnaire-Based Assessment of the Simulation Process
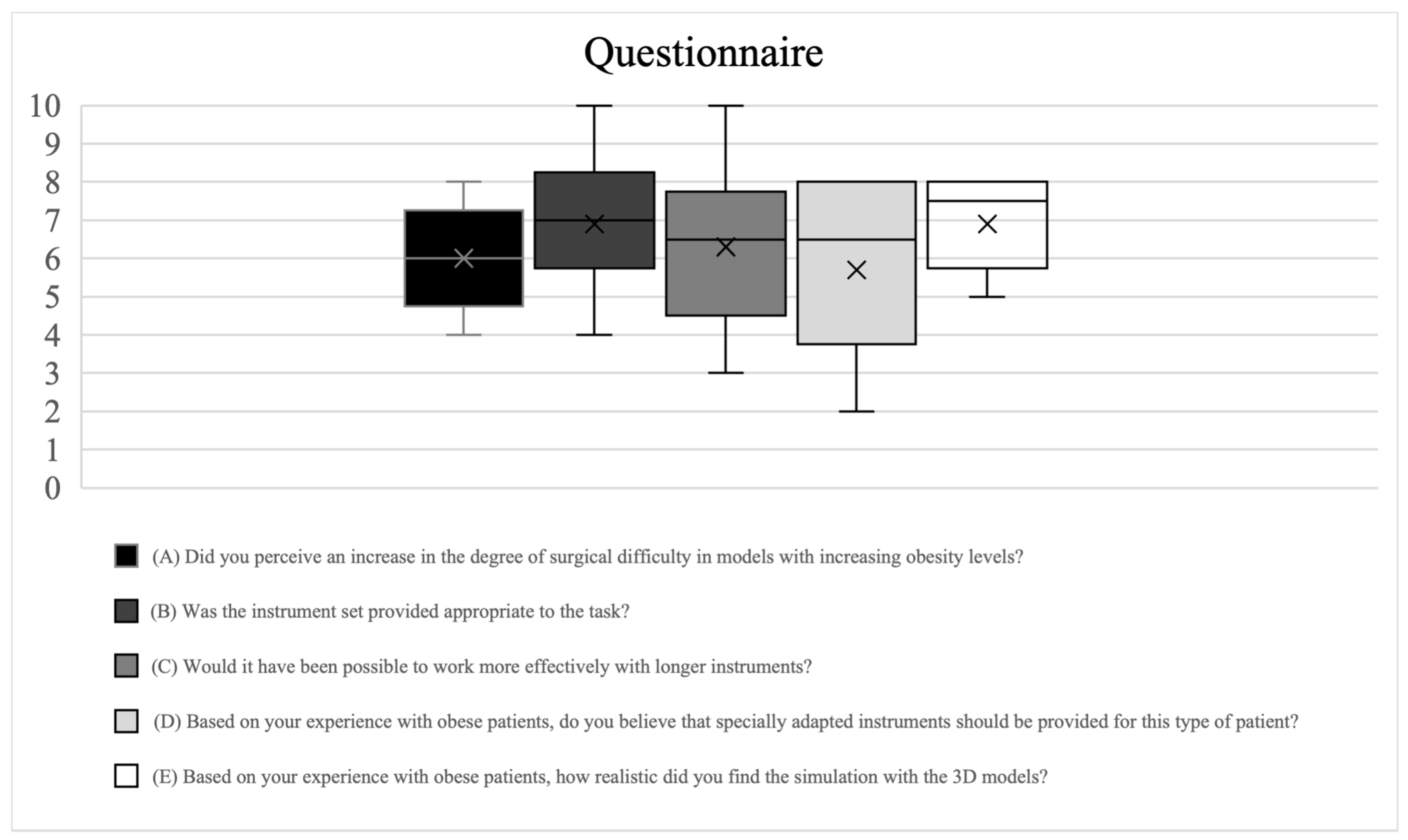
- (A)
- A certain, but not too pronounced, increase in difficulty was reported toward the models representing a higher obesity level.
- (B)
- The instruments were rated by the operators as ‘rather appropriate’, and, in some cases, ‘appropriate’ for carrying out the simulation tasks, even on the models representing a higher obesity level.
- (C)
- Although all operators stated an increased effectiveness of longer instruments in carrying out the simulation tasks, the expected degree of increased effectiveness varied considerably.
- (D)
- Although the need for longer instruments for surgery on obese patients was recognized, it was rated as rather moderate.
- (E)
- The model was recognized as having a certain degree of realism, and the operators were relatively consistent in this assessment.
- (F)
- All surgeons agreed that the nerve hook was the least suitable option, and three out of seven surgeons also mentioned the punch.
4. Discussion
4.1. Evaluation of Obesity-Dependent Complications and Surgery Duration
4.2. Simulation using 3D-Printed Models
4.3. Significance of 3D-Printed Models
4.4. Addressing the Dilemma of Surgery for Herniated Discs
4.5. Limitations
4.6. Future Research Directions
4.7. Tissue Modeling Challenges
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Statistisches Bundesamt. Die 20 Häufigsten Operationen Insgesamt (OPS5). Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Krankenhaeuser/Tabellen/drg-operationen-insgesamt.html (accessed on 3 August 2023).
- WHO. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 3 August 2023).
- Liuke, M.; Solovieva, S.; Lamminen, A.; Luoma, K.; Leino-Arjas, P.; Luukkonen, R.; Riihimäki, H. Disc Degeneration of the Lumbar Spine in Relation to Overweight. Int. J. Obes. 2005, 29, 903–908. [Google Scholar] [CrossRef]
- Gandhi, R.; Woo, K.M.; Zywiel, M.G.; Rampersaud, Y.R. Metabolic Syndrome Increases the Prevalence of Spine Osteoarthritis. Orthop. Surg. 2014, 6, 23–27. [Google Scholar] [CrossRef]
- Tjeertes, E.E.; Hoeks, S.S.; Beks, S.S.; Valentijn, T.T.; Hoofwijk, A.A.; Stolker, R.J.R. Obesity—A Risk Factor for Postoperative Complications in General Surgery? BMC Anesthesiol. 2015, 15, 112. [Google Scholar] [CrossRef]
- Goyal, A.; Elminawy, M.; Kerezoudis, P.; Lu, V.M.; Yolcu, Y.; Alvi, M.A.; Bydon, M. Impact of Obesity on Outcomes Following Lumbar Spine Surgery: A Systematic Review and Meta-Analysis. Clin. Neurol. Neurosurg. 2019, 177, 27–36. [Google Scholar] [CrossRef]
- McGuire, K.J.; Khaleel, M.A.; Rihn, J.A.; Lurie, J.D.; Zhao, W.; Weinstein, J.N. The Effect of High Obesity on Outcomes of Treatment for Lumbar Spinal Conditions: Subgroup Analysis of the Spine Patient Outcomes Research Trial. Spine 2014, 39, 1975–1980. [Google Scholar] [CrossRef]
- Rihn, J.A.; Kurd, M.; Hilibrand, A.S.; Lurie, J.; Zhao, W.; Albert, T.; Weinstein, J. The Influence of Obesity on the Outcome of Treatment of Lumbar Disc Herniation: Analysis of the Spine Patient Outcomes Research Trial (Sport). J. Bone Jt. Surg. 2013, 95, 1–8. [Google Scholar] [CrossRef]
- Brennan, P.M.; Loan, J.J.; Watson, N.; Bhatt, P.M.; Bodkin, P.A. Pre-Operative Obesity Does Not Predict Poorer Symptom Control and Quality of Life after Lumbar Disc Surgery. Br. J. Neurosurg. 2017, 31, 682–687. [Google Scholar] [CrossRef]
- Gugliotta, M.; da Costa, B.R.; Dabis, E.; Theiler, R.; Jüni, P.; Reichenbach, S.; Landolt, H.; Hasler, P. Surgical versus Conservative Treatment for Lumbar Disc Herniation: A Prospective Cohort Study. BMJ Open 2016, 6, e012938. [Google Scholar] [CrossRef]
- Wegner, M.; Dusse, F.; Beeser, F.; Leister, N.; Lefarth, M.; Finke, S.R.; Böttiger, B.W.; Dorweiler, B.; Stoll, S.E. Comparing Simulation Training of Bronchoscopy-Guided Percutaneous Dilatational Tracheostomy Using Conventional versus 3D Printed Simulators (Trac-Sim Study). J. Intensive Care Med. 2024, 8850666241232918. [Google Scholar] [CrossRef]
- Jain, S.; Sayed, M.E.; Shetty, M.; Alqahtani, S.M.; Al Wadei, M.H.D.; Gupta, S.G.; Othman, A.A.A.; Alshehri, A.H.; Alqarni, H.; Mobarki, A.H.; et al. Physical and Mechanical Properties of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to Cad/Cam Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Polymers 2022, 14, 2691. [Google Scholar] [CrossRef]
- Tejo-Otero, A.; Buj-Corral, I.; Fenollosa-Artés, F. 3D Printing in Medicine for Preoperative Surgical Planning: A Review. Ann. Biomed. Eng. 2020, 48, 536–555. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Szary, J.; Luis, M.S.; Mikulski, S.; Patel, A.; Schulz, F.; Tretiakow, D.; Fercho, J.; Jaguszewska, K.; Frankiewicz, M.; Pawłowska, E.; et al. The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals-Cross-Sectional Multispecialty Review. Int. J. Environ. Res. Public Health 2022, 19, 3331. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, F. Recent Trends in Bioprinting. Procedia Manuf. 2019, 32, 95–101. [Google Scholar] [CrossRef]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an Image Computing Platform for the Quantitative Imaging Network. Magn. Reson. Imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef] [PubMed]
- Dorweiler, B.; Baqué, P.E.; Chaban, R.; Ghazy, A.; Salem, O. Quality Control in 3D Printing: Accuracy Analysis of 3D-Printed Models of Patient-Specific Anatomy. Materials 2021, 14, 1021. [Google Scholar] [CrossRef] [PubMed]
- Wixted, C.M.; Peterson, J.R.; Kadakia, R.J.; Adams, S.B. Three-Dimensional Printing in Orthopaedic Surgery: Current Applications and Future Developments. JAAOS Glob. Res. Rev. 2021, 5, e20.00230-11. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Lee, S.-Y. A Systematic Review of 3-D Printing in Cardiovascular and Cerebrovascular Diseases. Anatol. J. Cardiol. 2017, 17, 423–435. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Liu, D. A Systematic Review of Clinical Value of Three-Dimensional Printing in Renal Disease. Quant. Imaging Med. Surg. 2018, 8, 311–325. [Google Scholar] [CrossRef] [PubMed]
- Belykh, E.; Giovani, A.; Abramov, I.; Ngo, B.; Bardonova, L.; Zhao, X.; Loymak, T.; Mooney, M.A.; Sheehy, J.P.; McBryan, S.; et al. Novel System of Simulation Models for Aneurysm Clipping Training: Description of Models and Assessment of Face, Content, and Construct Validity. Oper. Neurosurg. 2021, 21, 558–569. [Google Scholar] [CrossRef]
- Pearce, P.; Novak, J.; Wijesekera, A.; Loch-Wilkinson, T.; Redmond, M.; Winter, C.; Alexander, H.; Maclachlan, L. Properties and Implementation of 3-Dimensionally Printed Models in Spine Surgery: A Mixed-Methods Review with Meta-Analysis. World Neurosurg. 2023, 169, 57–72. [Google Scholar] [CrossRef]
- Bernhard, B.; Illi, J.; Gloeckler, M.; Pilgrim, T.; Praz, F.; Windecker, S.; Haeberlin, A.; Gräni, C. Imaging-Based, Patient-Specific Three-Dimensional Printing to Plan, Train, and Guide Cardiovascular Interventions: A Systematic Review and Meta-Analysis. Heart Lung Circ. 2022, 31, 1203–1218. [Google Scholar] [CrossRef] [PubMed]
- Rajzer, I.; Kurowska, A.; Frankova, J.; Sklenářová, R.; Nikodem, A.; Dziadek, M.; Jabłoński, A.; Janusz, J.; Szczygieł, P.; Ziąbka, M. 3D-Printed Polycaprolactone Implants Modified with Bioglass and Zn-Doped Bioglass. Materials 2023, 16, 1061. [Google Scholar] [CrossRef] [PubMed]
- Qu, L.; Wang, Y.; Wang, F.; Zhang, S. Surgical Outcomes of Percutaneous Endoscopic Lumbar Discectomy in Obese Adolescents with Lumbar Disc Herniation. BMC Musculoskelet. Disord. 2023, 24, 710. [Google Scholar] [CrossRef] [PubMed]
- Vinas-Rios, J.M.; Sanchez-Aguilar, M.; Medina Govea, F.A.; Von Beeg-Moreno, V.; Meyer, F. Incidence of Early Postoperative Complications Requiring Surgical Revision for Recurrent Lumbar Disc Herniation after Spinal Surgery: A Retrospective Observational Study of 9,310 Patients from the German Spine Register. Patient Saf. Surg. 2018, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Atesok, K.; Satava, R.M.; Marsh, J.L.; Hurwitz, S.R. Measuring Surgical Skills in Simulation-Based Training. J. Am. Acad. Orthop. Surg. 2017, 25, 665–672. [Google Scholar] [CrossRef]
- Stroop, R.; Nakamura, M.; Schoukens, J.; Oliva Uribe, D. Tactile Sensor-Based Real-Time Clustering for Tissue Differentiation. Int. J. Comput. Assist. Radiol. Surg. 2019, 14, 129–137. [Google Scholar] [CrossRef]

| Model | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Segment | LVB 4/5 | LVB 4/5 | LVB 4/5 | LVB 4/5 | LVB 5/SVB 1 |
| Surgical Situs Depth (mm) | 106 | 127 | 155 | 169 | 172 |
| BMI (kg/m2) | 32.1 | 32.7 | 52.6 | 44.2 | 44.2 |
| ICC | 0.973 | 0.940 | 0.912 | 0.931 | 0.879 |
| All Patients (n = 598) | BMI < 30 kg/m2 (n = 438) | BMI > 30 kg/m2 (n = 160) | p-Value | |
|---|---|---|---|---|
| Age in years | 50 (40–61) | 51 (40–62) | 48 (39–60) | 0.143 |
| Female gender | 263 (44.0) | 190 (43.4) | 73 (45.6) | 0.624 |
| BMI (kg/m2) | 26.9 (23.9–30.2) | 25.0 (23.0–27.4) | 32.8 (31.1–35.6) | <0.001 |
| BMI < 30 | BMI ≥ 30 | ||||
|---|---|---|---|---|---|
| All patients | All | all | 0.039 (p = 0.001; n = 438) | 0.059 (p = 0.002; n = 160) | |
| Age | <60 | 0.046 (p = 0.001; n = 302) | 0.104 (p = 0.001; n = 117) | ||
| ≥60 | 0.027 (p = 0.035; n = 136) | 0.008 (p = 0.057; n = 43) | |||
| Gender | Male | Age | <60 | 0.054 (p = 0.001; n = 176) | 0.156 (p = 0.001; n = 66) |
| ≥60 | 0.087 (p = 0.005; n = 72) | 0.11 (p = 0.141; n = 21) | |||
| Female | Age | <60 | 0.041 (p = 0.08; n =126) | 0.055 (p = 0.102; n = 51) | |
| ≥60 | 0.01 (p = 0.792; n = 64) | 0.02 (p = 0.846; n = 22) | |||
| Orientation | Medial/mediolateral | 0.042 (p = 0.001; n = 363) | 0.05 (p = 0.01; n = 135) | ||
| Intraforaminal | 0.014 (p = 0.421; n = 38) | 0.261 (p = 0.242; n = 7) | |||
| Extraforaminal | 0.058 (p = 0.307; n = 13) | 0.12 (p = 0.447; n = 7) | |||
| Segment | LVB 2/3 | 0.01 (p = 0.962; n = 20) | 0.57 (p = 0.19; n = 9) | ||
| LVB 3/4 | 0.045 (p = 0.147; n = 51) | 0.062 (p = 0.29; n = 21) | |||
| LVB 4/5 | 0.012 (p = 0.151; n = 179) | 0.082 (p = 0.027; n = 70) | |||
| LVB 5/SVB 1 | 0.02 (p = 0.576; n = 178) | 0.043 (p = 0.127; n = 60) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stroop, R.; Carballar, F.; Zawy Alsofy, S.; Sarkis, H.; Nakamura, M.; Greiner, C.; Dorweiler, B.; Wegner, M. Assessment of Obesity as Risk Factor of Lumbar Disc Surgery: Retrospective Analysis of 598 Cases and Simulated Surgery on 3D-Printed Models. J. Clin. Med. 2024, 13, 4193. https://doi.org/10.3390/jcm13144193
Stroop R, Carballar F, Zawy Alsofy S, Sarkis H, Nakamura M, Greiner C, Dorweiler B, Wegner M. Assessment of Obesity as Risk Factor of Lumbar Disc Surgery: Retrospective Analysis of 598 Cases and Simulated Surgery on 3D-Printed Models. Journal of Clinical Medicine. 2024; 13(14):4193. https://doi.org/10.3390/jcm13144193
Chicago/Turabian StyleStroop, Ralf, Fernando Carballar, Samer Zawy Alsofy, Hraq Sarkis, Makoto Nakamura, Christoph Greiner, Bernhard Dorweiler, and Moritz Wegner. 2024. "Assessment of Obesity as Risk Factor of Lumbar Disc Surgery: Retrospective Analysis of 598 Cases and Simulated Surgery on 3D-Printed Models" Journal of Clinical Medicine 13, no. 14: 4193. https://doi.org/10.3390/jcm13144193
APA StyleStroop, R., Carballar, F., Zawy Alsofy, S., Sarkis, H., Nakamura, M., Greiner, C., Dorweiler, B., & Wegner, M. (2024). Assessment of Obesity as Risk Factor of Lumbar Disc Surgery: Retrospective Analysis of 598 Cases and Simulated Surgery on 3D-Printed Models. Journal of Clinical Medicine, 13(14), 4193. https://doi.org/10.3390/jcm13144193






