Impact of the COVID-19 Pandemic on the Surgical Management of Head and Neck Non-Melanoma Skin Cancers in a Maxillofacial Center of Cluj-Napoca
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection and Statistical Analysis
2.2. Analysis of Statistical Data
3. Results
3.1. Demographical and Epidemiological Consideration of the Population
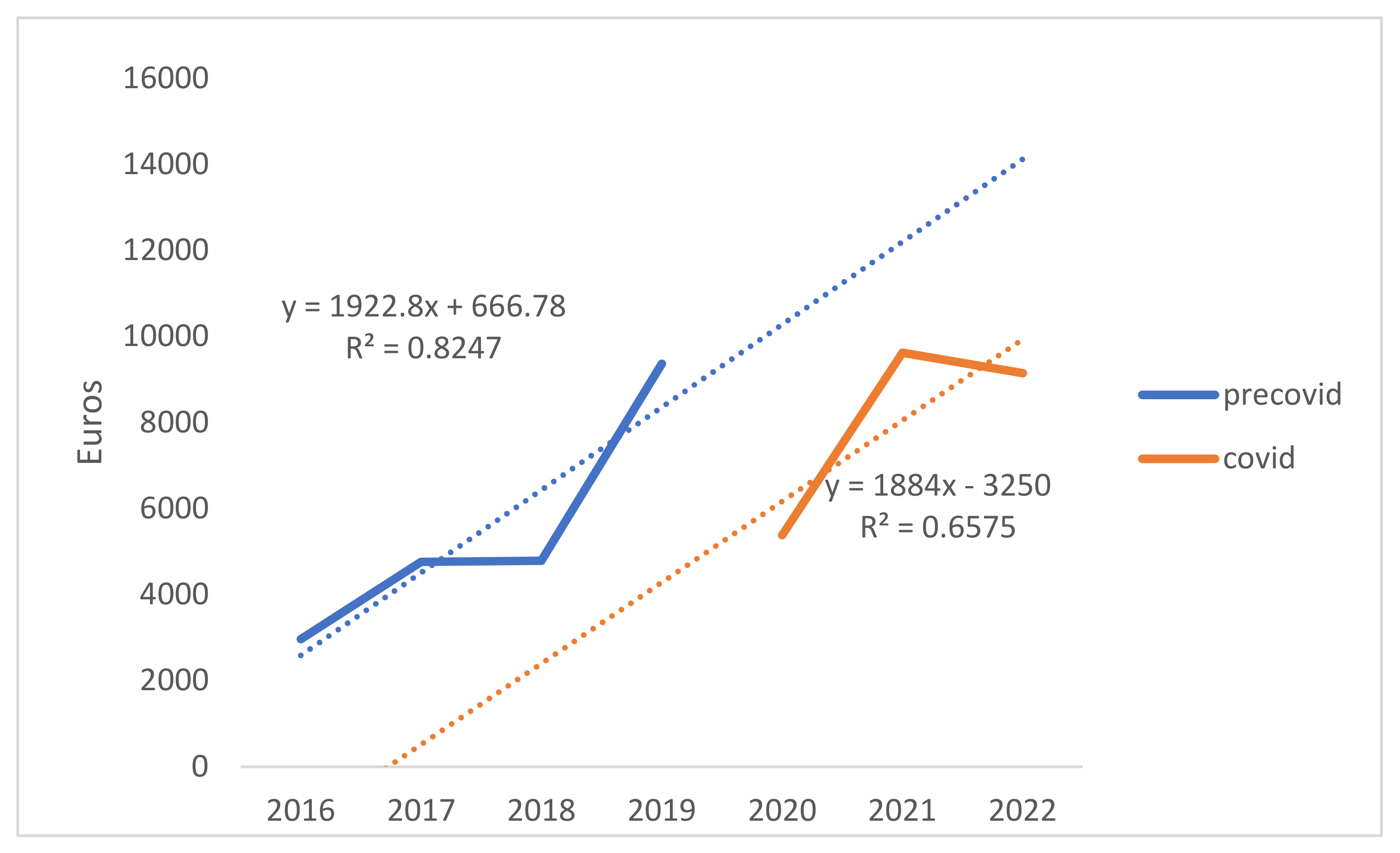
3.2. Treatment Costs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global Cancer Statistics 2022: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef] [PubMed]
- Mudigonda, T.; Pearce, D.J.; Yentzer, B.A.; Williford, P.; Feldman, S.R. The Economic Impact of Non-Melanoma Skin Cancer: A Review. J. Natl. Compr. Cancer Netw. 2010, 8, 888–896. [Google Scholar] [CrossRef] [PubMed]
- The American Cancer Society. Key Statistics for Basal and Squamous Cell Skin Cancers. Available online: https://www.cancer.org/cancer/types/basal-and-squamous-cell-skin-cancer/about/key-statistics.html#:~:text=According%20to%20one%20estimate%2C%20about,cell%20cancers%20occur%20less%20often (accessed on 2 May 2024).
- Roland, N.; Memon, A. Non-Melanoma Skin Cancer of the Head and Neck. Br. J. Hosp. Med. 2023, 84, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Peris, K.; Fargnoli, M.C.; Kaufmann, R.; Arenberger, P.; Bastholt, L.; Seguin, N.B.; Bataille, V.; Brochez, L.; del Marmol, V.; Dummer, R.; et al. European Consensus-Based Interdisciplinary Guideline for Diagnosis and Treatment of Basal Cell Carcinoma—Update 2023. Eur. J. Cancer 2023, 192, 113254. [Google Scholar] [CrossRef] [PubMed]
- Verkouteren, J.A.C.; Ramdas, K.H.R.; Wakkee, M.; Nijsten, T. Epidemiology of Basal Cell Carcinoma: Scholarly Review. Br. J. Dermatol. 2017, 177, 359–372. [Google Scholar] [CrossRef] [PubMed]
- Flohil, S.C.; van der Leest, R.J.T.; Arends, L.R.; de Vries, E.; Nijsten, T. Risk of Subsequent Cutaneous Malignancy in Patients with Prior Keratinocyte Carcinoma: A Systematic Review and Meta-Analysis. Eur. J. Cancer 2013, 49, 2365–2375. [Google Scholar] [CrossRef] [PubMed]
- The American Cancer Society. What Are Basal and Squamous Cell Skin Cancers? Available online: https://www.cancer.org/cancer/types/basal-and-squamous-cell-skin-cancer/about/what-is-basal-and-squamous-cell.html (accessed on 2 May 2024).
- Quazi, S.J.; Aslam, N.; Saleem, H.; Rahman, J.; Khan, S. Surgical Margin of Excision in Basal Cell Carcinoma: A Systematic Review of Literature. Cureus 2020, 12, e9211. [Google Scholar] [CrossRef]
- Bichakjian, C.K.; Olencki, T.; Aasi, S.Z.; Alam, M.; Andersen, J.S.; Berg, D.; Bowen, G.M.; Cheney, R.T.; Daniels, G.A.; Glass, L.F.; et al. Basal Cell Skin Cancer, Version 1.2016, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2016, 14, 574–597. [Google Scholar] [CrossRef] [PubMed]
- Barker, C.A.; Arron, S.; Ho, A.; Algazi, A.; Dunn, L.; Humphries, A.; Hultman, C.; Lian, M.; Knott, P.D.; Yom, S.S. A Phase II Single Arm Trial of Induction and Concurrent Vismodegib with Curative Intent Radiation Therapy for Locally Advanced, Unresectable Basal Cell Carcinoma of the Head and Neck. Int. J. Radiat. Oncol. Biol. Phys. 2024, 118, e7. [Google Scholar] [CrossRef]
- Wong, C.S.M.; Strange, R.C.; Lear, J.T. Basal Cell Carcinoma. BMJ 2003, 327, 794–798. [Google Scholar] [CrossRef]
- Samir, S.; Puneet, K.; Deepthi, B.; Laurence, P.-D.; Delphine, K.; Thierry, P. A Comprehensive Analysis of Global Skin Cancer Incidence and Mortality with a Focus on Dermatologist Density and Population Risk Factors. 2023. Available online: https://s3.eu-central-1.amazonaws.com/m-anage.com.storage.eadv/abstracts_congress2023/37072.pdf (accessed on 5 May 2024).
- Flohil, S.C.; Seubring, I.; van Rossum, M.M.; Coebergh, J.-W.W.; de Vries, E.; Nijsten, T. Trends in Basal Cell Carcinoma Incidence Rates: A 37-Year Dutch Observational Study. J. Investig. Dermatol. 2013, 133, 913–918. [Google Scholar] [CrossRef] [PubMed]
- Stratigos, A.J.; Garbe, C.; Dessinioti, C.; Lebbe, C.; van Akkooi, A.; Bataille, V.; Bastholt, L.; Dreno, B.; Dummer, R.; Fargnoli, M.C.; et al. European Consensus-Based Interdisciplinary Guideline for Invasive Cutaneous Squamous Cell Carcinoma. Part 1: Diagnostics and Prevention—Update 2023. Eur. J. Cancer 2023, 193, 113251. [Google Scholar] [CrossRef]
- De Boer, M.F.; McCormick, L.K.; Pruyn, J.F.A.; Ryckman, R.M.; van den Borne, B.W. Physical and Psychosocial Correlates of Head and Neck Cancer: A Review of the Literature. Otolaryngol. Head Neck Surg. 1999, 120, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Pillai, S.; Siddika, N.; Hoque Apu, E.; Kabir, R. COVID-19: Situation of European Countries so Far. Arch. Med. Res. 2020, 51, 723–725. [Google Scholar] [CrossRef]
- Enciu, B.G.; Tănase, A.A.; Drăgănescu, A.C.; Aramă, V.; Pițigoi, D.; Crăciun, M.-D. The COVID-19 Pandemic in Romania: A Comparative Description with Its Border Countries. Healthcare 2022, 10, 1223. [Google Scholar] [CrossRef]
- Rashid, S.; Tsao, H. Effect of the COVID-19 Pandemic on Delayed Skin Cancer Services. Dermatol. Clin. 2021, 39, 627–637. [Google Scholar] [CrossRef] [PubMed]
- Kourtidis, S.; Münst, J.; Hofmann, V.M. Effects of the COVID-19 Pandemic on Head and Neck Cancer Stage and Treatment Duration. Cureus 2022, 14, e26744. [Google Scholar] [CrossRef] [PubMed]
- Flores, C.E.R.; de Almeida, D.O.; Freitas, L.V.D.; Martins, I.S.; Martins, N.M.B.; Danesi, C.C.; Ferrazzo, K.L. Diagnosis of head and neck squamous cell carcinoma during the COVID-19 pandemic: A retrospective case-control study. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2023, 136, e51. [Google Scholar] [CrossRef]
- Crossley, J.R.; Nelson, L.L.; VanDolah, H.; Davidson, B.J.; Maxwell, J.H. The Impact of COVID-19 on Presentation and Diagnosis of Head and Neck Squamous Cell Carcinoma. Laryngoscope Investig. Otolaryngol. 2022, 7, 1436–1440. [Google Scholar] [CrossRef]
- Lucidi, D.; Valerini, S.; Federici, G.; Miglio, M.; Cantaffa, C.; Alicandri-Ciufelli, M. Head and Neck Cancer During COVID-19 Pandemic: Was There a Diagnostic Delay? Indian J. Otolaryngol. Head Neck Surg. 2022, 74, 3245–3251. [Google Scholar] [CrossRef]
- Antohi, V.M.; Ionescu, R.V.; Zlati, M.L.; Mirica, C. Approaches Related to the Effects of COVID-19 Pandemics on Financing of the Healthcare System in Romania. Front. Public Health 2022, 10, 94002. [Google Scholar] [CrossRef]
- Eurostat. Main Cause of Death. 2020. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/w/DDN-20230307-3 (accessed on 5 May 2024).
- Worldometers. Coronavirus Cases. Available online: https://www.worldometers.info/coronavirus/ (accessed on 5 May 2024).
- Zanoni, D.K.; Patel, S.G.; Shah, J.P. Changes in the 8th Edition of the American Joint Committee on Cancer (AJCC) Staging of Head and Neck Cancer: Rationale and Implications. Curr. Oncol. Rep. 2019, 21, 52. [Google Scholar] [CrossRef]
- AJCC. AJCC Cancer Staging Manual, 8th ed.; Amin, M.B., Edge, S.B., Greene, F.L., Byrd, D.R., Brookland, R.K., Washington, M.K., Gershenwald, J.E., Compton, C.C., Hess, K.R., Sullivan, D.C., et al., Eds.; Springer: Cham, Switzerland, 2016. [Google Scholar]
- Faur, C.I.; Moldovan, M.A.; Văleanu, M.; Rotar, H.; Filip, L.; Roman, R.C. The Prevalence and Treatment Costs of Non-Melanoma Skin Cancer in Cluj-Napoca Maxillofacial Center. Medicina 2023, 59, 220. [Google Scholar] [CrossRef]
- Raghupathi, V.; Raghupathi, W. The Influence of Education on Health: An Empirical Assessment of OECD Countries for the Period 1995–2015. Arch. Public Health 2020, 78, 20. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Xiang, W. Income Gradient in Health-Related Quality of Life—The Role of Social Networking Time. Int. J. Equity Health 2019, 18, 44. [Google Scholar] [CrossRef] [PubMed]
- Benedetti, S.; Frosolini, A.; Catarzi, L.; Marsiglio, A.; Gennaro, P.; Gabriele, G. Impact of the COVID-19 Pandemic on the Diagnosis and Management of Non-Melanoma Skin Cancer in the Head and Neck Region: A Retrospective Cohort Study. Healthcare 2024, 12, 501. [Google Scholar] [CrossRef] [PubMed]
- Lembo, F.; Cecchino, L.; Parisi, D.; Portincasa, A. Nonmelanoma Skin Cancer in COVID-19 Era: The Foggia Experience. J. Cutan. Aesthet. Surg. 2022, 15, 436. [Google Scholar] [CrossRef] [PubMed]
- Silvia, C.; Denis, C.; Mario, C.; Luigi, V.; Federico, T.; Marcello, C. Impact of COVID-19 Pandemic on Non-Melanoma Skin Cancer’s Tumor Burden and Care: A Multi-Center Study Based in Northern Italy. J. Plast. Reconstr. Aesthet. Surg. 2022, 75, 3616–3621. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, D.L.; Howe, J.R.; Chang, G.; Crago, A.; Hogg, M.; Karakousis, G.; Levine, E.; Maker, A.; Mamounas, E.; McGuire, K.; et al. Management of Cancer Surgery Cases During the COVID-19 Pandemic: Considerations. Ann. Surg. Oncol. 2020, 27, 1717–1720. [Google Scholar] [CrossRef]
- Søreide, K.; Hallet, J.; Matthews, J.B.; Schnitzbauer, A.A.; Line, P.D.; Lai, P.B.S.; Otero, J.; Callegaro, D.; Warner, S.G.; Baxter, N.N.; et al. Immediate and Long-Term Impact of the COVID-19 Pandemic on Delivery of Surgical Services. Br. J. Surg. 2020, 107, 1250–1261. [Google Scholar] [CrossRef] [PubMed]
- Souza, A.F.; de Arruda, J.A.A.; Costa, F.P.D.; Bemquerer, L.M.; Castro, W.H.; Campos, F.E.B.; Kakehasi, F.M.; Travassos, D.V.; Silva, T.A. Safety Protocols for Dental Care during the COVID-19 Pandemic: The Experience of a Brazilian Hospital Service. Braz. Oral. Res. 2021, 35. [Google Scholar] [CrossRef] [PubMed]
- Givi, B.; Schiff, B.A.; Chinn, S.B.; Clayburgh, D.; Iyer, N.G.; Jalisi, S.; Moore, M.G.; Nathan, C.-A.; Orloff, L.A.; O’Neill, J.P.; et al. Safety Recommendations for Evaluation and Surgery of the Head and Neck During the COVID-19 Pandemic. JAMA Otolaryngol. Head Neck Surg. 2020, 146, 579. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.; Gamage, B.; Bryce, E.; Copes, R.; Yassi, A. Protecting Health Care Workers from SARS and Other Respiratory Pathogens: Organizational and Individual Factors That Affect Adherence to Infection Control Guidelines. Am. J. Infect. Control 2005, 33, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Chambers, L.C. Long-Term Health Care Costs Following COVID-19: Implications for Pandemic Preparedness. Am. J. Manag. Care 2023, 29, 566–572. [Google Scholar] [CrossRef]
- Dancer, S.J. Reducing the Risk of COVID-19 Transmission in Hospitals: Focus on Additional Infection Control Strategies. Surgery 2021, 39, 752–758. [Google Scholar] [CrossRef]
| 2016–2022 | Pre-Pandemic (2016–2019) | Pandemic (2020–2022) | Statistical Analysis Pre- vs. during Pandemic | |
|---|---|---|---|---|
| Sex | ||||
| Male | 101 (57.38%) | 68 (58.11%) | 36 (57.14%) | 0.787 |
| Female | 75 (42.61%) | 49 (41.88%) | 27 (42.85%) | |
| Living place | ||||
| Urban | 111 (63.06%) | 69 (58.97%) | 45 (41.02%) | 0.028 |
| Rural | 65 (36.93%) | 48 (41.02%) | 18 (28.57%) | |
| Education | ||||
| Primary school | 10 (13.33%) | 5 (10%) | 5 (20%) | 0.003 |
| Middle school | 26 (34.66%) | 20 (40%) | 6 (24%) | |
| High school | 19 (25.33%) | 14 (28%) | 5 (20%) | |
| University | 20 (26.66%) | 11 (22%) | 9 (36%) | |
| Income | ||||
| Low | 49 (52.68%) | 38 (63.33%) | 11 (33.33%) | 0.037 |
| Medium | 42 (45.16%) | 21 (35%) | 21 (63.63%) | |
| High | 2 (2.15%) | 1 (1.66%) | 1 (3.03%) | |
| ASA risk | ||||
| I | 71 (39.01%) | 43 (35.83%) | 29 (45.31%) | 0.099 |
| II | 60 (32.96%) | 41 (34.16%) | 19 (29.68%) | |
| III | 50 (27.47%) | 36 (30%) | 15 (23.43%) | |
| IV | 1 (0.54%) | 0 (0%) | 1 (1.56%) | |
| Localization | ||||
| Nasal | 58 (27.48%) | 42 (30.88%) | 16 (21.33%) | - |
| Cheek | 47 (22.2%) | 27 (19.85%) | 20 (26.67%) | |
| Temporal | 18 (8.53%) | 14 (10.29%) | 4 (5.33%) | |
| Frontal | 28 (13.27%) | 16 (11.76%) | 12 (16.00%) | |
| Auricular | 17 (8.05%) | 9 (6.62%) | 8 (10.67%) | |
| Cervical | 4 (1.89%) | 2 (1.47%) | 2 (2.67%) | |
| Labial | 5 (2.36%) | 4 (2.94%) | 1 (1.33%) | |
| Mental | 5 (2.36%) | 3 (2.21%) | 2 (2.67%) | |
| Orbital | 22 (10.42%) | 12 (8.82%) | 10 (13.33%) | |
| Infraorbital | 7 (3.31%) | 7 (5.15%) | 0 (0%) | |
| Type of tumor and histopathological grade | ||||
| BCC | 166 (78.64%) | 109 (80.14%) | 57 (76%) | - |
| Nodular | 108 (65.06%) | 70 (64.22%) | 38 (66.66%) | |
| Infiltrative | 34 (20.48%) | 25 (22.93%) | 9 (15.78%) | |
| Other types | 24 (14.45%) | 14 (12.84%) | 10 (17.54%) | |
| SCC | 45 (21.32%) | 27 (19.85%) | 18 (24%) | |
| G1 | 19 (42.22%) | 8 (29.62%) | 11 (61.11%) | |
| G2 | 20 (44.44%) | 14 (51.85%) | 6 (33.33%) | |
| G3 | 4 (8.88%) | 3 (11.11%) | 1 (5.55%) | |
| G4 | 2 (4.44%) | 2 (7.40%) | 0 (0%) | |
| Patients with both BCC and SCC | 5 (2.84%) | 5 (4.27%) | 1 (1.58%) | |
| Stage | ||||
| I | 136 (64.45%) | 85 (62.5%) | 51 (68%) | 0.677 |
| II | 44 (20.86%) | 28 (20.58%) | 16 (21.33%) | |
| III | 27 (12.79%) | 20 (14.70%) | 7 (9.33%) | |
| IV | 4 (1.89%) | 3 (2.20%) | 1 (1.33%) | |
| Waiting time for surgery (weeks) | ||||
| 1.71 ± 3.36 | 1.31 ± 2.94 | 2.44 ± 3.92 | 0.004 | |
| Type of surgery | ||||
| Excision | 202 (95.73%) | 132 (97.05%) | 70 (93.33%) | 0.354 |
| Re-excision | 9 (4.26%) | 4 (2.94%) | 5 (6.66%) | |
| Type of reconstruction | ||||
| Primary suture | 74 (35.07%) | 47 (34.55%) | 27 (36%) | 0.354 |
| Local flap | 129 (61.13%) | 87 (63.97%) | 42 (56%) | |
| Skin graft | 8 (3.79%) | 2 (1.47%) | 6 (8%) | |
| Time for surgery (hours) | ||||
| 1.15 ± 0.84 | 1.02 ± 0.87 | 1.39 ± 0.73 | <0.001 | |
| Hospitalization (days) | ||||
| 2.3 ± 1.92 | 2.3 ± 1.77 | 2.31 ± 2.19 | 0.749 | |
| 2016–2022 | Pre-Pandemic (2016–2019) | Pandemic (2020–2022) | Statistical Analysis Pre- vs. during Pandemic | |
|---|---|---|---|---|
| Total cost of treatment | 378.85 ± 409.92 | 333.96 ± 311.5 | 475.57 ± 533.3 | <0.001 |
| Examination costs | 45.48 ± 43.54 | 35.00 ± 34.93 | 65.75 ± 49.95 | <0.001 |
| Costs of medication | 16.97 ± 44.87 | 17.23 ± 53.46 | 17.43 ± 29.77 | 0.002 |
| Costs of materials | 22.23 ± 29.90 | 14.67 ± 17.05 | 36.29 ± 40.44 | <0.001 |
| Accomodation and professional assistance | 294.17 ± 328.74 | 267.06 ± 234.76 | 356.10 ± 445.47 | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roman, R.C.; Faur, C.I.; Gordan, E.; Văleanu, M.; Moldovan, M.A. Impact of the COVID-19 Pandemic on the Surgical Management of Head and Neck Non-Melanoma Skin Cancers in a Maxillofacial Center of Cluj-Napoca. J. Clin. Med. 2024, 13, 3934. https://doi.org/10.3390/jcm13133934
Roman RC, Faur CI, Gordan E, Văleanu M, Moldovan MA. Impact of the COVID-19 Pandemic on the Surgical Management of Head and Neck Non-Melanoma Skin Cancers in a Maxillofacial Center of Cluj-Napoca. Journal of Clinical Medicine. 2024; 13(13):3934. https://doi.org/10.3390/jcm13133934
Chicago/Turabian StyleRoman, Rareș Călin, Cosmin Ioan Faur, Edina Gordan, Mădălina Văleanu, and Mădălina Anca Moldovan. 2024. "Impact of the COVID-19 Pandemic on the Surgical Management of Head and Neck Non-Melanoma Skin Cancers in a Maxillofacial Center of Cluj-Napoca" Journal of Clinical Medicine 13, no. 13: 3934. https://doi.org/10.3390/jcm13133934
APA StyleRoman, R. C., Faur, C. I., Gordan, E., Văleanu, M., & Moldovan, M. A. (2024). Impact of the COVID-19 Pandemic on the Surgical Management of Head and Neck Non-Melanoma Skin Cancers in a Maxillofacial Center of Cluj-Napoca. Journal of Clinical Medicine, 13(13), 3934. https://doi.org/10.3390/jcm13133934








