Traumatic Brain Injury as an Independent Predictor of Futility in the Early Resuscitation of Patients in Hemorrhagic Shock
Abstract
1. Introduction: The Importance of Defining Futility in the Current Blood Product Shortage
2. The Attempt to Define Parameters which Predict Futility in Patients with Polytrauma and TBI: Refining the STOP Algorithm
“The authors feel that this is the population in which we can expeditiously apply our findings to and provide an opportunity for resource stewardship. Locally, these patients have been described by several of our faculty as ones we are able to rescue on the macro level (with ROSC and often making it the OR), but fail to capture them on the micro level (with endothelial, coagulation, and electrophysiological uncoupling).”[7]
3. Historical Definitions of Severe TBI in Relation to Transfusion Cut Points and Early Declaration of Futility
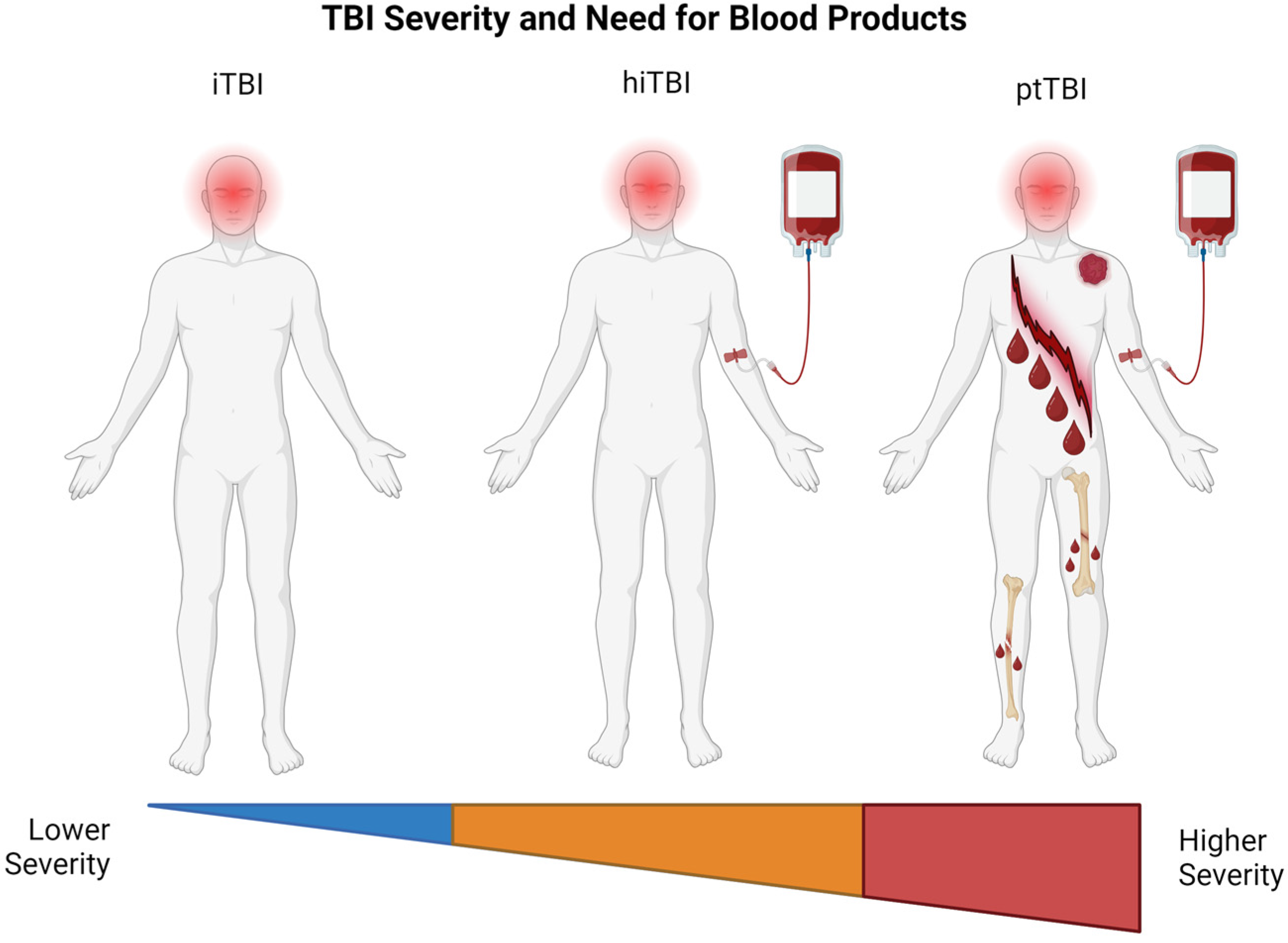
4. Defining iTBI, hiTBI, and ptTBI in Relation to Early Declaration of Futility
5. General Definition of Futility in TBI
5.1. Defining Futility in iTBI
5.2. Defining Futility in hiTBI
5.3. Timing of Prediction of Futility in iTBI and hiTBI: Prehospital, ER, OR, and ICU
5.4. Defining Futility in ptTBI
5.5. Timing of Prediction of Futility in ptTBI: Prehospital, ER, OR, and ICU
6. The Evolution of Bedside Futility Markers for Hemorrhaging Patients with TBI and Trauma
6.1. From Clinical Gestalt to Metric-Assisted Gestalt: Addressing Equitable Distribution of Scarce Blood Products during MT
6.2. Non-Bedside Predictors of Late Mortality for TBI Patients
6.3. Prehospital and Early Bedside Predictors of Early Mortality in Patients with TBI
7. Proposal to Combine STOP Criteria with the Most Recently Accepted Guidelines for Early WOC of TBI: Adding Palliative Timeout to FTO/TTO
- Limit early and potentially premature neuroprognostication prior to hemodynamic stabilization;
- Optimize individual patient outcomes;
- Engage in a reasonable allocation of scarce resources;
- Incorporate patient-respecting, end-of-life practices including organ donation as part of the continuum of compassionate care to patient and family
8. Ethical Implications of Defining Early TBI in the Presence of Shock
9. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ACP | American College of Physicians |
| AIS | Abbreviated Injury Scale |
| APACHE | Acute Physiology and Chronic Health Evaluation |
| BCT | Blood component therapy |
| BIG | Brain injury guideline |
| CCT | Common coagulation testing |
| ciTBI | Clinically important traumatic brain injury |
| CPP | Cerebral perfusion pressure |
| CRASH | Corticosteroid Randomization after Significant Head Injury |
| CT | Computerized axial tomography |
| CTBI | Coagulopathy of traumatic brain injury |
| DAI | Diffuse axonal injury |
| DBI | Devastating brain injury |
| DDD-TEG | Double diamond of death thromboelastography |
| DIC | Disseminated intravascular coagulation |
| EMAT | Elderly Mortality After Trauma |
| ETCO2 | End-tidal CO2 |
| FFP | Fresh frozen plasma |
| FR | Futile resuscitation |
| FTO | Futility timeout |
| GCS | Glasgow Coma Scale |
| GTOS | Geriatric Trauma Outcome Score |
| HIC | Higher-income country |
| hiTBI | Hemorrhagic isolated traumatic brain injury |
| ICP | Intracranial pressure |
| IMPACT | International Mission for Prognosis and Clinical Trials in Traumatic Brain Injury |
| ISS | Injury Severity Score |
| iTBI | Isolated traumatic brain injury |
| LMIC | Low to middle-income country |
| LY30 | Lysis at 30 min |
| MAP | Mean arterial pressure |
| MT | Massive transfusion |
| PAIP | Portable automated infrared pupillometry |
| PLT | Platelets |
| PPV | Positive predictive value |
| PRBC | Packed red blood cells |
| PTO | Palliative timeout |
| ptTBI | Polytraumatic traumatic brain injury |
| ROSC | Return of spontaneous circulation |
| SAH | Subarachnoid hemorrhage |
| SFP | Self-fulfilling prophecy |
| SOFA | Sequential Organ Failure Assessment |
| STOP | Suspension of Transfusions and Other Procedures |
| TBI | Traumatic brain injury |
| TEG | Thromboelastography |
| TF | Tissue factor |
| TIC | Trauma-induced coagulopathy |
| TRACULA | Tracts Constrained by Underlying Anatomy |
| VET | Viscoelastic testing |
| WOC | Withdrawal of care |
References
- Clements, T.W.; Van Gent, J.M.; Lubkin, D.E.; Wandling, M.W.; Meyer, D.E.; Moore, L.J.; Cotton, B.A. The Reports of my Death are Greatly Exaggerated: An Evaluation of Futility Cut-Points in Massive Transfusion. J. Trauma Acute Care Surg. 2023, 95, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Doughty, H.; Green, L.; Callum, J.; Murphy, M.F. Triage tool for the rationing of blood for massively bleeding patients during a severe national blood shortage: Guidance from the National Blood Transfusion Committee. Br. J. Haematol. 2020, 191, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Casem, C.F.; Baral, E.; Inaba, K.; Kuza, C.M. Narrative Review: Is There a Transfusion Cutoff Value After Which Nonsurvivability Is Inevitable in Trauma Patients Receiving Ultramassive Transfusion? Anesth. Analg. 2023, 137, 354–364. [Google Scholar] [CrossRef] [PubMed]
- Loudon, A.M.; Rushing, A.P.; Hue, J.J.; Ziemak, A.; Sarode, A.L.; Moorman, M.L. When is enough enough? Odds of survival by unit transfused. J. Trauma Acute Care Surg. 2023, 94, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Mladinov, D.; Frank, S.M. Massive transfusion and severe blood shortages: Establishing and implementing predictors of futility. Br. J. Anaesth. 2022, 128, e71–e74. [Google Scholar] [CrossRef] [PubMed]
- Saillant, N.N.; Kornblith, L.Z.; Moore, H.; Barrett, C.; Schreiber, M.A.; Cotton, B.A.; Neal, M.D.; Makar, R.; Cap, A.P. The National Blood Shortage-An Impetus for Change. Ann. Surg. 2022, 275, 641–643. [Google Scholar] [CrossRef] [PubMed]
- Van Gent, J.M.; Clements, T.W.; Lubkin, D.T.; Wade, C.E.; Cardenas, J.C.; Kao, L.S.; Cotton, B.A. Predicting Futility in Severely Injured Patients: Using Arrival Lab Values and Physiology to Support Evidence-Based Resource Stewardship. J. Am. Coll. Surg. 2023, 236, 874–880. [Google Scholar] [CrossRef] [PubMed]
- Quintana, M.T.; Zebley, J.A.; Vincent, A.; Chang, P.; Estroff, J.; Sarani, B.; Forssten, M.P.; Cao, Y.; Chen, M.; Corrado, C.; et al. Cresting mortality: Defining a plateau in ongoing massive transfusion. J. Trauma Acute Care Surg. 2022, 93, 43–51. [Google Scholar] [CrossRef]
- Kockelmann, F.; Maegele, M. Acute Haemostatic Depletion and Failure in Patients with Traumatic Brain Injury (TBI): Pathophysiological and Clinical Considerations. J. Clin. Med. 2023, 12, 2809. [Google Scholar] [CrossRef]
- Maegele, M.; Aversa, J.; Marsee, M.K.; McCauley, R.; Chitta, S.H.; Vyakaranam, S.; Walsh, M. Changes in Coagulation following Brain Injury. Semin. Thromb. Hemost. 2020, 46, 155–166. [Google Scholar] [CrossRef]
- Maegele, M.; Schöchl, H.; Menovsky, T.; Maréchal, H.; Marklund, N.; Buki, A.; Stanworth, S. Coagulopathy and haemorrhagic progression in traumatic brain injury: Advances in mechanisms, diagnosis, and management. Lancet Neurol. 2017, 16, 630–647. [Google Scholar] [CrossRef]
- Moore, E.E.; Moore, H.B.; Kornblith, L.Z.; Neal, M.D.; Hoffman, M.; Mutch, N.J.; Schochl, H.; Hunt, B.J.; Sauaia, A. Trauma-induced coagulopathy. Nat. Rev. Dis. Primers 2021, 7, 30. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, J.; Walsh, M.; Grisoli, A.; Thomas, A.V.; Shariff, F.; McCauley, R.; Vande Lune, S.; Zackariya, N.; Patel, S.; Farrell, M.S.; et al. Diagnosis and Treatment of Trauma-Induced Coagulopathy by Viscoelastography. Semin. Thromb. Hemost. 2020, 46, 134–146. [Google Scholar] [CrossRef] [PubMed]
- Miranda, S.P.; Morris, R.S.; Rabas, M.; Creutzfeldt, C.J.; Cooper, Z. Early Shared Decision-Making for Older Adults with Traumatic Brain Injury: Using Time-Limited Trials and Understanding Their Limitations. Neurocrit Care 2023, 39, 284–293. [Google Scholar] [CrossRef] [PubMed]
- Souter, M.J.; Blissitt, P.A.; Blosser, S.; Bonomo, J.; Greer, D.; Jichici, D.; Mahanes, D.; Marcolini, E.G.; Miller, C.; Sangha, K.; et al. Recommendations for the Critical Care Management of Devastating Brain Injury: Prognostication, Psychosocial, and Ethical Management: A Position Statement for Healthcare Professionals from the Neurocritical Care Society. Neurocrit Care 2015, 23, 4–13. [Google Scholar] [CrossRef] [PubMed]
- American College of Surgeons Trauma Quality Improvement Program. Best practices in the management of traumatic brain injury. ACS Comm. Trauma 2015, 3–23. [Google Scholar]
- Tran, A.; Saigle, V.; Manhas, N.; McIntyre, L.; Turgeon, A.F.; Lauzier, F.; Chassé, M.; Golka, C.; Millington, S.J.; Kyeremanteng, K.; et al. Association of age with death and withdrawal of life-sustaining therapy after severe traumatic brain injury. Can. J. Surg. 2023, 66, e348–e355. [Google Scholar] [CrossRef]
- Williamson, T.; Ryser, M.D.; Ubel, P.A.; Abdelgadir, J.; Spears, C.A.; Liu, B.; Komisarow, J.; Lemmon, M.E.; Elsamadicy, A.; Lad, S.P. Withdrawal of Life-supporting Treatment in Severe Traumatic Brain Injury. JAMA Surg. 2020, 155, 723–731. [Google Scholar] [CrossRef] [PubMed]
- Turgeon, A.F.; Lauzier, F.; Simard, J.F.; Scales, D.C.; Burns, K.E.; Moore, L.; Zygun, D.A.; Bernard, F.; Meade, M.O.; Dung, T.C.; et al. Mortality associated with withdrawal of life-sustaining therapy for patients with severe traumatic brain injury: A Canadian multicentre cohort study. Cmaj 2011, 183, 1581–1588. [Google Scholar] [CrossRef]
- Livingston, D.H.; Mosenthal, A.C. Withdrawing life-sustaining therapy for patients with severe traumatic brain injury. Cmaj 2011, 183, 1570–1571. [Google Scholar] [CrossRef]
- Raj, R.; Wennervirta, J.M.; Tjerkaski, J.; Luoto, T.M.; Posti, J.P.; Nelson, D.W.; Takala, R.; Bendel, S.; Thelin, E.P.; Luostarinen, T.; et al. Dynamic prediction of mortality after traumatic brain injury using a machine learning algorithm. NPJ Digit. Med. 2022, 5, 96. [Google Scholar] [CrossRef] [PubMed]
- Kheirbek, T.; Martin, T.J.; Cao, J.; Hall, B.M.; Lueckel, S.; Adams, C.A. Prehospital shock index outperforms hypotension alone in predicting significant injury in trauma patients. Trauma Surg. Acute Care Open 2021, 6, e000712. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Chen, H.; Zhou, H.; Sun, X.; Ren, J.; Sun, H.; Chen, C.; Chen, G. Comparison of noninvasive continuous arterial blood pressure measured by NICAP with arterial line in elderly patients. BMC Geriatr. 2022, 22, 108. [Google Scholar]
- Hansen, L.H.; Ettrup-Christensen, A.; Bülow, K. Feasibility of continuous noninvasive arterial pressure monitoring in a prehospital setting, measurements during emergency transfer. Eur. J. Emerg. Med. 2019, 26, 334–339. [Google Scholar] [CrossRef] [PubMed]
- Anand, T.; Nelson, A.C.; Obaid, O.; Ditillo, M.F.; El-Qawaqzeh, K.W.M.; Stewart, C.; Reina Limon, R.F.A.; Hosseinpour, H.; Nguyen, L.; Joseph, B. Futility of Resuscitation among Geriatric Trauma Patients: Do We Need to Define When to Withdraw Care? J. Am. Coll. Surg. 2022, 235, S92–S93. [Google Scholar] [CrossRef]
- Cosgriff, N.; Moore, E.E.; Sauaia, A.; Kenny-Moynihan, M.; Burch, J.M.; Galloway, B. Predicting life-threatening coagulopathy in the massively transfused trauma patient: Hypothermia and acidoses revisited. J. Trauma 1997, 42, 857–861; discussion 852–861. [Google Scholar] [CrossRef] [PubMed]
- Criddle, L.M.; Eldredge, D.H.; Walker, J. Variables predicting trauma patient survival following massive transfusion. J. Emerg. Nurs. 2005, 31, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Hakala, P.; Hiippala, S.; Syrjala, M.; Randell, T. Massive blood transfusion exceeding 50 units of plasma poor red cells or whole blood: The survival rate and the occurrence of leukopenia and acidosis. Injury 1999, 30, 619–622. [Google Scholar] [CrossRef] [PubMed]
- Kivioja, A.; Myllynen, P.; Rokkanen, P. Survival after massive transfusions exceeding four blood volumes in patients with blunt injuries. Am. Surg. 1991, 57, 398–401. [Google Scholar]
- Liu, S.; Fujii, Q.; Serio, F.; McCague, A. Massive Blood Transfusions and Outcomes in Trauma Patients; An Intention to Treat Analysis. Bull. Emerg. Trauma 2018, 6, 217–220. [Google Scholar] [CrossRef]
- Lo, B.D.; Merkel, K.R.; Dougherty, J.L.; Kajstura, T.J.; Cruz, N.C.; Sikorski, R.A.; Frank, S.M. Assessing predictors of futility in patients receiving massive transfusions. Transfusion 2021, 61, 2082–2089. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.C.; Niziolek, G.M.; Baker, J.E.; Huebner, B.R.; Hanseman, D.; Makley, A.T.; Pritts, T.A.; Goodman, M.D. Death by Decade: Establishing a Transfusion Ceiling for Futility in Massive Transfusion. J. Surg. Res. 2020, 252, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Muldowney, M.; Liu, Z.; Stansbury, L.G.; Vavilala, M.S.; Hess, J.R. Ultramassive Transfusion for Trauma in the Age of Hemostatic Resuscitation: A Retrospective Single-Center Cohort From a Large US Level-1 Trauma Center, 2011–2021. Anesth. Analg. 2023, 136, 927–933. [Google Scholar] [CrossRef] [PubMed]
- Phillips, T.F.; Soulier, G.; Wilson, R.F. Outcome of massive transfusion exceeding two blood volumes in trauma and emergency surgery. J. Trauma 1987, 27, 903–910. [Google Scholar] [CrossRef] [PubMed]
- Rangarajan, K.; Subramanian, A.; Pandey, R.M. Determinants of mortality in trauma patients following massive blood transfusion. J. Emerg. Trauma Shock 2011, 4, 58–63. [Google Scholar]
- Schneider, A.B.; Adams, U.; Gallaher, J.; Purcell, L.N.; Raff, L.; Eckert, M.; Charles, A. Blood Utilization and Thresholds for Mortality Following Major Trauma. J. Surg. Res. 2023, 281, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Siegel, J.H.; Rivkind, A.I.; Dalal, S.; Goodarzi, S. Early physiologic predictors of injury severity and death in blunt multiple trauma. Arch. Surg. 1990, 125, 498–508. [Google Scholar] [CrossRef] [PubMed]
- Vaslef, S.N.; Knudsen, N.W.; Neligan, P.J.; Sebastian, M.W. Massive transfusion exceeding 50 units of blood products in trauma patients. J. Trauma 2002, 53, 291–295; discussion 295–296. [Google Scholar] [CrossRef]
- Velmahos, G.C.; Chan, L.; Chan, M.; Tatevossian, R.; Cornwell III, E.E.; Asensio, J.A.; Berne, T.V.; Demetriades, D. Is there a limit to massive blood transfusion after severe trauma? Arch. Surg. 1998, 133, 947–952. [Google Scholar] [CrossRef]
- Wilson, R.F.; Dulchavsky, S.A.; Soullier, G.; Beckman, B. Problems with 20 or more blood transfusions in 24 hours. Am. Surg. 1987, 53, 410–417. [Google Scholar]
- Yu, A.J.; Inaba, K.; Biswas, S.; de Leon, L.A.; Wong, M.; Benjamin, E.; Lam, L.; Demetriades, D. Supermassive Transfusion: A 15-Year Single Center Experience and Outcomes. Am. Surg. 2018, 84, 1617–1621. [Google Scholar] [CrossRef] [PubMed]
- Dorken Gallastegi, A.; Secor, J.D.; Maurer, L.R.; Dzik, W.S.; Saillant, N.N.; Hwabejire, J.O.; Fawley, J.; Parks, J.; Kaafarani, H.M.; Velmahos, G.C. Role of Transfusion Volume and Transfusion Rate as Markers of Futility During Ultramassive Blood Transfusion in Trauma. J. Am. Coll. Surg. 2022, 235, 468–480. [Google Scholar] [CrossRef] [PubMed]
- Holcomb, J.B.; Tilley, B.C.; Baraniuk, S.; Fox, E.E.; Wade, C.E.; Podbielski, J.M.; del Junco, D.J.; Brasel, K.J.; Bulger, E.M.; Callcut, R.A.; et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: The PROPPR randomized clinical trial. JAMA 2015, 313, 471–482. [Google Scholar] [CrossRef] [PubMed]
- Dzik, W. Misunderstanding the PROPPR trial. Transfusion 2017, 57, 2056. [Google Scholar] [CrossRef] [PubMed]
- Holcomb, J.B.; Hess, J.R.; Group, P.S. Response to: “Misunderstanding the PROPPR trial”. Transfusion 2017, 57, 2057–2058. [Google Scholar] [CrossRef]
- Eagle, S.R.; Nwachuku, E.; Elmer, J.; Deng, H.; Okonkwo, D.O.; Pease, M. Performance of CRASH and IMPACT Prognostic Models for Traumatic Brain Injury at 12 and 24 Months Post-Injury. Neurotrauma Rep. 2023, 4, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Kotwica, Z.; Jakubowski, J.K. Head-injured adult patients with GCS of 3 on admission--who have a chance to survive? Acta Neurochir (Wien) 1995, 133, 56–59. [Google Scholar] [CrossRef] [PubMed]
- Majdan, M.; Steyerberg, E.W.; Nieboer, D.; Mauritz, W.; Rusnak, M.; Lingsma, H.F. Glasgow coma scale motor score and pupillary reaction to predict six-month mortality in patients with traumatic brain injury: Comparison of field and admission assessment. J. Neurotrauma 2015, 32, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Siegel, J.H. The effect of associated injuries, blood loss, and oxygen debt on death and disability in blunt traumatic brain injury: The need for early physiologic predictors of severity. J. Neurotrauma 1995, 12, 579–590. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Mushkudiani, N.; Perel, P.; Butcher, I.; Lu, J.; McHugh, G.S.; Murray, G.D.; Marmarou, A.; Roberts, I.; Habbema, J.D.; et al. Predicting outcome after traumatic brain injury: Development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008, 5, e165; discussion e165. [Google Scholar] [CrossRef]
- Tenovuo, O.; Diaz-Arrastia, R.; Goldstein, L.E.; Sharp, D.J.; van der Naalt, J.; Zasler, N.D. Assessing the Severity of Traumatic Brain Injury-Time for a Change? J. Clin. Med. 2021, 10, 148. [Google Scholar] [CrossRef]
- Tien, H.C.; Cunha, J.R.; Wu, S.N.; Chughtai, T.; Tremblay, L.N.; Brenneman, F.D.; Rizoli, S.B. Do trauma patients with a Glasgow Coma Scale score of 3 and bilateral fixed and dilated pupils have any chance of survival? J. Trauma 2006, 60, 274–278. [Google Scholar] [CrossRef]
- Perel, P.; Al-Shahi Salman, R.; Kawahara, T.; Morris, Z.; Prieto-Merino, D.; Roberts, I.; Sandercock, P.; Shakur, H.; Wardlaw, J. CRASH-2 (Clinical Randomisation of an Antifibrinolytic in Significant Haemorrhage) intracranial bleeding study: The effect of tranexamic acid in traumatic brain injury--a nested randomised, placebo-controlled trial. Health Technol. Assess. 2012, 16, iii-54. [Google Scholar] [CrossRef] [PubMed]
- National Association of EMS Physicians and American College of Surgeons Committee on Trauma. Withholding of resuscitation for adult traumatic cardiopulmonary arrest. Prehosp Emerg. Care 2013, 17, 291. [Google Scholar] [CrossRef] [PubMed]
- Millin, M.G.; Galvagno, S.M.; Khandker, S.R.; Malki, A.; Bulger, E.M. Withholding and termination of resuscitation of adult cardiopulmonary arrest secondary to trauma: Resource document to the joint NAEMSP-ACSCOT position statements. J. Trauma Acute Care Surg. 2013, 75, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, D. The self-fulfilling prophecy in intensive care. Theor. Med. Bioeth. 2009, 30, 401–410. [Google Scholar] [CrossRef]
- Roberts, G.; Lloyd, M.; Parker, M.; Martin, R.; Philp, B.; Shelley, O.; Dziewulski, P. The Baux score is dead. Long live the Baux score: A 27-year retrospective cohort study of mortality at a regional burns service. J. Trauma Acute Care Surg. 2012, 72, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.; Kryzanski, J. Prognosis and futility in neurosurgical emergencies: A review. Clin. Neurol. Neurosurg. 2020, 195, 105851. [Google Scholar] [CrossRef]
- Mohammadifard, M.; Ghaemi, K.; Hanif, H.; Sharifzadeh, G.; Haghparast, M. Marshall and Rotterdam Computed Tomography scores in predicting early deaths after brain trauma. Eur. J. Transl. Myol. 2018, 28, 7542. [Google Scholar] [CrossRef]
- Plum, F.; Posner, J.B. Prognosis in Coma and Related Disorders of Consciousness, Mechanisms Underlying Outcomes, and Ethical Considerations. In The Diagnosis of Stupor and Coma; Oxford Academic: Oxford, UK, 2007; Volume 67, pp. 344–345. [Google Scholar]
- Zakrison, T.L.; Essig, R.; Polcari, A.; McKinley, W.; Arnold, D.; Beyene, R.; Wilson, K.; Rogers, S., Jr.; Matthews, J.B.; Millis, J.M.; et al. Review Paper on Penetrating Brain Injury: Ethical Quandaries in the Trauma Bay and Beyond. Ann. Surg. 2023, 277, 66–72. [Google Scholar] [CrossRef]
- Plum, F.; Posner, J.B. Structural Cases of Stupor and Coma. In The Diagnosis of Stupor and Coma; Oxford Academic: Oxford, UK, 2007; Volume 67, pp. 88–118. [Google Scholar]
- Pease, M.; Nwachuku, E.; Goldschmidt, E.; Elmer, J.; Okonkwo, D.O. Complications from Multimodal Monitoring Do not Affect Long-Term Outcomes in Severe Traumatic Brain Injury. World Neurosurg. 2022, 161, e109–e117. [Google Scholar] [CrossRef]
- Stocker, R.A. Intensive Care in Traumatic Brain Injury Including Multi-Modal Monitoring and Neuroprotection. Med. Sci. 2019, 7, 37. [Google Scholar] [CrossRef]
- Barker, M.D.; Whyte, J.; Pretz, C.R.; Sherer, M.; Temkin, N.; Hammond, F.M.; Saad, Z.; Novack, T. Application and clinical utility of the Glasgow Coma Scale over time: A study employing the NIDRR traumatic brain injury model systems database. J. Head Trauma Rehabil. 2014, 29, 400–406. [Google Scholar] [CrossRef]
- Perrin, P.B.; Niemeier, J.P.; Mougeot, J.L.; Vannoy, C.H.; Hirsch, M.A.; Watts, J.A.; Rossman, W.; Grafton, L.M.; Guerrier, T.D.; Pershad, R.; et al. Measures of injury severity and prediction of acute traumatic brain injury outcomes. J. Head Trauma Rehabil. 2015, 30, 136–142. [Google Scholar] [CrossRef]
- Lulla, A.; Lumba-Brown, A.; Totten, A.M.; Maher, P.J.; Badjatia, N.; Bell, R.; Donayri, C.T.J.; Fallat, M.E.; Hawryluk, G.W.J.; Goldberg, S.A.; et al. Prehospital Guidelines for the Management of Traumatic Brain Injury—3rd Edition. Prehosp. Emerg. Care 2023, 27, 507–538. [Google Scholar] [CrossRef]
- Roozenbeek, B.; Lingsma, H.F.; Lecky, F.E.; Lu, J.; Weir, J.; Butcher, I.; McHugh, G.S.; Murray, G.D.; Perel, P.; Maas, A.I.; et al. Prediction of outcome after moderate and severe traumatic brain injury: External validation of the International Mission on Prognosis and Analysis of Clinical Trials (IMPACT) and Corticoid Randomisation after Significant Head injury (CRASH) prognostic models. Crit. Care Med. 2012, 40, 1609–1617. [Google Scholar]
- Muehlschlegel, S.; Rajajee, V.; Wartenberg, K.E.; Alexander, S.A.; Busl, K.M.; Creutzfeldt, C.J.; Fontaine, G.V.; Hocker, S.E.; Hwang, D.Y.; Kim, K.S.; et al. Guidelines for Neuroprognostication in Critically Ill Adults with Moderate-Severe Traumatic Brain Injury. Neurocrit. Care 2024, 40, 448–476. [Google Scholar] [CrossRef]
- Ahmadi, S.; Sarveazad, A.; Babahajian, A.; Ahmadzadeh, K.; Yousefifard, M. Comparison of Glasgow Coma Scale and Full Outline of UnResponsiveness score for prediction of in-hospital mortality in traumatic brain injury patients: A systematic review and meta-analysis. Eur. J. Trauma Emerg. Surg. 2023, 49, 1693–1706. [Google Scholar] [CrossRef]
- Cook, A.C.; Joseph, B.; Inaba, K.; Nakonezny, P.A.; Bruns, B.R.; Kerby, J.D.; Brasel, K.J.; Wolf, S.E.; Cuschieri, J.; Paulk, M.E.; et al. Multicenter external validation of the Geriatric Trauma Outcome Score: A study by the Prognostic Assessment of Life and Limitations After Trauma in the Elderly (PALLIATE) consortium. J. Trauma Acute Care Surg. 2016, 80, 204–209. [Google Scholar] [CrossRef]
- Egglestone, R.; Sparkes, D.; Dushianthan, A. Prediction of mortality in critically-ill elderly trauma patients: A single centre retrospective observational study and comparison of the performance of trauma scores. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 95. [Google Scholar] [CrossRef]
- Park, J.; Lee, Y. Predicting Mortality of Korean Geriatric Trauma Patients: A Comparison between Geriatric Trauma Outcome Score and Trauma and Injury Severity Score. Yonsei Med. J. 2022, 63, 88–94. [Google Scholar] [CrossRef]
- Ravindranath, S.; Ho, K.M.; Rao, S.; Nasim, S.; Burrell, M. Validation of the geriatric trauma outcome scores in predicting outcomes of elderly trauma patients. Injury 2021, 52, 154–159. [Google Scholar] [CrossRef]
- Scherer, J.; Kalbas, Y.; Ziegenhain, F.; Neuhaus, V.; Lefering, R.; Teuben, M.; Sprengel, K.; Pape, H.C.; Jensen, K.O. The GERtality Score: The Development of a Simple Tool to Help Predict in-Hospital Mortality in Geriatric Trauma Patients. J. Clin. Med. 2021, 10, 1362. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, Y.; Feng, Q.; Tang, H.; Wang, Y.; Li, Z.; Bai, X. Predictive value of the geriatric trauma outcome score in older patients after trauma: A retrospective cohort study. Int. J. Gen. Med. 2022, 15, 4379–4390. [Google Scholar] [CrossRef] [PubMed]
- El-Qawaqzeh, K.; Anand, T.; Alizai, Q.; Colosimo, C.; Hosseinpour, H.; Spencer, A.; Ditillo, M.; Magnotti, L.J.; Stewart, C.; Joseph, B. Trauma in the Geriatric and the Super-Geriatric: Should They Be Treated the Same? J. Surg. Res. 2024, 293, 316–326. [Google Scholar] [CrossRef]
- El-Qawaqzeh, K.; Magnotti, L.J.; Hosseinpour, H.; Nelson, A.; Spencer, A.L.; Anand, T.; Bhogadi, S.K.; Alizai, Q.; Ditillo, M.; Joseph, B. Geriatric trauma, frailty, and ACS trauma center verification level: Are there any correlations with outcomes? Injury 2024, 55, 110972. [Google Scholar] [CrossRef]
- Joseph, B.; Obaid, O.; Dultz, L.; Black, G.; Campbell, M.; Berndtson, A.E.; Costantini, T.; Kerwin, A.; Skarupa, D.; Burruss, S.; et al. Validating the Brain Injury Guidelines: Results of an American Association for the Surgery of Trauma prospective multi-institutional trial. J. Trauma Acute Care Surg. 2022, 93, 157–165. [Google Scholar] [CrossRef]
- Joseph, B.; Pandit, V.; Zangbar, B.; Kulvatunyou, N.; Tang, A.; O‘Keeffe, T.; Green, D.J.; Vercruysse, G.; Fain, M.J.; Friese, R.S.; et al. Validating Trauma-Specific Frailty Index for Geriatric Trauma Patients: A Prospective Analysis. J. Am. Coll. Surg. 2014, 219, 10–17e11. [Google Scholar] [CrossRef]
- Zhao, F.Z.; Wolf, S.E.; Nakonezny, P.A.; Minhajuddin, A.; Rhodes, R.L.; Paulk, M.E.; Phelan, H.A. Estimating Geriatric Mortality after Injury Using Age, Injury Severity, and Performance of a Transfusion: The Geriatric Trauma Outcome Score. J. Palliat. Med. 2015, 18, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Alizai, Q.; Joseph, B. Systematic Review—From Challenge to Success: Transforming Care Through Brain Injury Guidelines. Kos. J Surg. 2024, 8, 46–54. Available online: https://koscs.org/en/systematic-review-from-challenge-to-success-transforming-care-through-brain-injury-guidelines/ (accessed on 25 June 2024).
- Benhamed, A.; Emond, M.; Mercier, E.; Heidet, M.; Gauss, T.; Saint-Supery, P.; Yadav, K.; David, J.-S.; Claustre, C.; Tazarourte, K. Accuracy of a prehospital triage protocol in predicting in-hospital mortality and severe trauma cases among older adults. Int. J. Environ. Res. Public. Health 2023, 20, 1975. [Google Scholar] [CrossRef]
- Chow, J.; Kuza, C.M. Predicting mortality in elderly trauma patients: A review of the current literature. Curr. Opin. Anesthesiol. 2022, 35, 160–165. [Google Scholar] [CrossRef]
- Hosseinpour, H.; Anand, T.; Bhogadi, S.K.; Colosimo, C.; El-Qawaqzeh, K.; Spencer, A.L.; Castanon, L.; Ditillo, M.; Magnotti, L.J.; Joseph, B. Emergency Department Shock Index Outperforms Prehospital and Delta Shock Indices in Predicting Outcomes of Trauma Patients. J. Surg. Res. 2023, 291, 204–212. [Google Scholar] [CrossRef]
- Kıhtır, H.S.; Ongun, E.A. BIG score is a strong predictor of mortality and morbidity for high-energy traumas in pediatric intensive care unit. Turk. J. Trauma Emerg. Surg. 2022, 28, 1292. [Google Scholar] [CrossRef]
- Nishimura, S.; Kumamaru, H.; Shoji, S.; Nakatani, E.; Yamamoto, H.; Ichihara, N.; Miyachi, Y.; Sandhu, A.T.; Heidenreich, P.A.; Yamauchi, K.; et al. Assessment of coding-based frailty algorithms for long-term outcome prediction among older people in community settings: A cohort study from the Shizuoka Kokuho Database. Age Ageing 2022, 51, afac009. [Google Scholar] [CrossRef]
- Bai, X.; Wang, R.; Zhang, C.; Wen, D.; Ma, L.; He, M. The prognostic value of an age-adjusted BIG score in adult patients with traumatic brain injury. Front. Neurol. 2023, 14, 1272994. [Google Scholar] [CrossRef]
- Fulkerson, D.H.; White, I.K.; Rees, J.M.; Baumanis, M.M.; Smith, J.L.; Ackerman, L.L.; Boaz, J.C.; Luerssen, T.G. Analysis of long-term (median 10.5 years) outcomes in children presenting with traumatic brain injury and an initial Glasgow Coma Scale score of 3 or 4. J. Neurosurg. Pediatr. 2015, 16, 410–419. [Google Scholar] [CrossRef]
- Hemphill, J.C., 3rd; White, D.B. Clinical nihilism in neuroemergencies. Emerg. Med. Clin. N. Am. 2009, 27, 27–37. [Google Scholar] [CrossRef]
- Stein, N.R.; McArthur, D.L.; Etchepare, M.; Vespa, P.M. Early cerebral metabolic crisis after TBI influences outcome despite adequate hemodynamic resuscitation. Neurocrit. Care 2012, 17, 49–57. [Google Scholar] [CrossRef]
- Castellino, F.J.; Chapman, M.P.; Donahue, D.L.; Thomas, S.; Moore, E.E.; Wohlauer, M.V.; Fritz, B.; Yount, R.; Ploplis, V.; Davis, P.; et al. Traumatic brain injury causes platelet adenosine diphosphate and arachidonic acid receptor inhibition independent of hemorrhagic shock in humans and rats. J. Trauma Acute Care Surg. 2014, 76, 1169–1176. [Google Scholar] [CrossRef]
- Wada, T.; Shiraishi, A.; Gando, S.; Yamakawa, K.; Fujishima, S.; Saitoh, D.; Kushimoto, S.; Ogura, H.; Abe, T.; Mayumi, T.; et al. Pathophysiology of Coagulopathy Induced by Traumatic Brain Injury Is Identical to That of Disseminated Intravascular Coagulation With Hyperfibrinolysis. Front. Med. 2021, 8, 767637. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, R.R.; Rowell, S.E.; Diggs, B.S.; Schreiber, M.A.; Group, T.O. Profoundly abnormal initial physiologic and biochemical data cannot be used to determine futility in massively transfused trauma patients. J. Trauma Acute Care Surg. 2011, 71, S364–S369. [Google Scholar] [CrossRef] [PubMed]
- Neal, C.J.; Bell, R.S.; Carmichael, J.J.; DuBose, J.J.; Grabo, D.J.; Oh, J.S.; Remick, K.N.; Bailey, J.A.; Stockinger, Z.T. Catastrophic Non-Survivable Brain Injury Care-Role 2/3. Mil. Med. 2018, 183, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Lanken, P.N.; Ahlheit, B.D.; Crawford, S.; Hansen-Flaschen, J.H.; Lefrak, S.S.; Luce, J.M.; Matthay, M.A.; Osborne, M.L.; Raffin, T.A.; Robotham, J.L.; et al. Withholding and withdrawing life-sustaining therapy. This Official Statement of the American Thoracic Society was adopted by the ATS Board of Directors, March 1991. Am. Rev. Respir. Dis. 1991, 144, 726–731. [Google Scholar] [CrossRef]
- Kon, A.A.; Shepard, E.K.; Sederstrom, N.O.; Swoboda, S.M.; Marshall, M.F.; Birriel, B.; Rincon, F. Defining Futile and Potentially Inappropriate Interventions: A Policy Statement From the Society of Critical Care Medicine Ethics Committee. Crit. Care Med. 2016, 44, 1769–1774. [Google Scholar] [CrossRef]
- Malaiyandi, D.P.; Henderson, G.V.; Rubin, M.A. Transfusion of Blood Products in the Neurocritical Care Unit: An Exploration of Rationing and Futility. Neurocrit. Care 2018, 28, 296–301. [Google Scholar] [CrossRef]
- Joseph, B.; Saljuqi, A.T.; Amos, J.D.; Teichman, A.; Whitmill, M.L.; Anand, T.; Hosseinpour, H.; Burruss, S.K.; Dunn, J.A.; Najafi, K.; et al. Prospective validation and application of the Trauma-Specific Frailty Index: Results of an American Association for the Surgery of Trauma multi-institutional observational trial. J. Trauma Acute Care Surg. 2023, 94, 36–44. [Google Scholar] [CrossRef]
- Fischer, D.; Edlow, B.L.; Giacino, J.T.; Greer, D.M. Neuroprognostication: A conceptual framework. Nat. Rev. Neurol. 2022, 18, 419–427. [Google Scholar] [CrossRef]
- Li, Y.; Wang, L.; Liu, Y.; Zhao, Y.; Fan, Y.; Yang, M.; Yuan, R.; Zhou, F.; Zhang, Z.; Kang, H. Development and Validation of a Simplified Prehospital Triage Model Using Neural Network to Predict Mortality in Trauma Patients: The Ability to Follow Commands, Age, Pulse Rate, Systolic Blood Pressure and Peripheral Oxygen Saturation (CAPSO) Model. Front. Med. 2021, 8, 810195. [Google Scholar] [CrossRef]
- Stopenski, S.; Grigorian, A.; Inaba, K.; Lekawa, M.; Matsushima, K.; Schellenberg, M.; Kim, D.; de Virgilio, C.; Nahmias, J. Prehospital Variables Alone Can Predict Mortality After Blunt Trauma: A Novel Scoring Tool. Am. Surg. 2021, 87, 1638–1643. [Google Scholar] [CrossRef]
- Vorbeck, J.; Bachmann, M.; Düsing, H.; Hartensuer, R. Mortality Risk Factors of Severely Injured Polytrauma Patients (Prehospital Mortality Prediction Score). J. Clin. Med. 2023, 12, 4724. [Google Scholar] [CrossRef]
- Eichinger, M.; Robb, H.D.P.; Scurr, C.; Tucker, H.; Heschl, S.; Peck, G. Challenges in the PREHOSPITAL emergency management of geriatric trauma patients—A scoping review. Scand. J. Trauma Resusc. Emerg. Med. 2021, 29, 100. [Google Scholar] [CrossRef]
- Li, Z.; Feng, Y.; Wang, P.; Han, S.; Zhang, K.; Zhang, C.; Lu, S.; Lv, C.; Zhu, F.; Bie, L. Evaluation of the prognosis of acute subdural hematoma according to the density differences between gray and white matter. Front. Neurol. 2022, 13, 1024018. [Google Scholar] [CrossRef]
- Choi, Y.; Park, J.H.; Hong, K.J.; Ro, Y.S.; Song, K.J.; Shin, S.D. Development and validation of a prehospital-stage prediction tool for traumatic brain injury: A multicentre retrospective cohort study in Korea. BMJ Open 2022, 12, e055918. [Google Scholar] [CrossRef]
- van Veen, E.; van der Jagt, M.; Citerio, G.; Stocchetti, N.; Gommers, D.; Burdorf, A.; Menon, D.K.; Maas, A.I.R.; Kompanje, E.J.O.; Lingsma, H.F. Occurrence and timing of withdrawal of life-sustaining measures in traumatic brain injury patients: A CENTER-TBI study. Intensive Care Med. 2021, 47, 1115–1129. [Google Scholar] [CrossRef]
- Anestis, D.M.; Marinos, K.; Tsitsopoulos, P.P. Comparison of the prognostic validity of three simplified consciousness assessment scales with the Glasgow Coma Scale. Eur. J. Trauma Emerg. Surg. 2023, 49, 2193–2202. [Google Scholar] [CrossRef]
- van Veen, E.; van der Jagt, M.; Citerio, G.; Stocchetti, N.; Epker, J.L.; Gommers, D.; Burdorf, L.; Menon, D.K.; Maas, A.I.R.; Lingsma, H.F.; et al. End-of-life practices in traumatic brain injury patients: Report of a questionnaire from the CENTER-TBI study. J. Crit. Care 2020, 58, 78–88. [Google Scholar] [CrossRef]
- Cook, C. Is clinical gestalt good enough? J. Man. Manip. Ther. 2009, 17, 6–7. [Google Scholar] [CrossRef]
- Kabrhel, C.; Camargo, C.A., Jr.; Goldhaber, S.Z. Clinical gestalt and the diagnosis of pulmonary embolism: Does experience matter? Chest 2005, 127, 1627–1630. [Google Scholar] [CrossRef]
- Kempainen, R.R.; Migeon, M.B.; Wolf, F.M. Understanding our mistakes: A primer on errors in clinical reasoning. Med. Teach. 2003, 25, 177–181. [Google Scholar] [CrossRef]
- Baik, D.; Yeom, S.R.; Park, S.W.; Cho, Y.; Yang, W.T.; Kwon, H.; Lee, J.I.; Ko, J.K.; Choi, H.J.; Huh, U.; et al. The Addition of ROTEM Parameter Did Not Significantly Improve the Massive Transfusion Prediction in Severe Trauma Patients. Emerg. Med. Int. 2022, 2022, 7219812. [Google Scholar] [CrossRef] [PubMed]
- Nunez, T.C.; Voskresensky, I.V.; Dossett, L.A.; Shinall, R.; Dutton, W.D.; Cotton, B.A. Early prediction of massive transfusion in trauma: Simple as ABC (assessment of blood consumption)? J. Trauma 2009, 66, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Pommerening, M.J.; Goodman, M.D.; Holcomb, J.B.; Wade, C.E.; Fox, E.E.; Del Junco, D.J.; Brasel, K.J.; Bulger, E.M.; Cohen, M.J.; Alarcon, L.H.; et al. Clinical gestalt and the prediction of massive transfusion after trauma. Injury 2015, 46, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Yücel, N.; Lefering, R.; Maegele, M.; Vorweg, M.; Tjardes, T.; Ruchholtz, S.; Neugebauer, E.A.; Wappler, F.; Bouillon, B.; Rixen, D. Trauma Associated Severe Hemorrhage (TASH)-Score: Probability of mass transfusion as surrogate for life threatening hemorrhage after multiple trauma. J. Trauma 2006, 60, 1228–1236; discussion 1227–1236. [Google Scholar] [CrossRef] [PubMed]
- Chapman, M.P.; Moore, E.E.; Moore, H.B.; Gonzalez, E.; Morton, A.P.; Chandler, J.; Fleming, C.D.; Ghasabyan, A.; Silliman, C.C.; Banerjee, A.; et al. The “Death Diamond”: Rapid thrombelastography identifies lethal hyperfibrinolysis. J. Trauma Acute Care Surg. 2015, 79, 925–929. [Google Scholar] [CrossRef] [PubMed]
- Farrell, M.S.; Moore, E.E.; Thomas, A.V.; Coleman, J.R.; Thomas, S.; Vande Lune, S.; Marconi, T., Jr.; Cohen, M.J.; Chapman, M.P.; Moore, H.B.; et al. “Death Diamond” Tracing on Thromboelastography as a Marker of Poor Survival After Trauma. Am. Surg. 2022, 88, 1689–1693. [Google Scholar] [CrossRef]
- Moore, E.E.; Moore, H.B.; Thomas, S.G.; Farrell, M.S.; Sixta, S.; Coleman, J.R.; Miller, J.B.; Bunch, C.M.; Waxman, D.; Walsh, M.M. Serial “Death Diamond” TEGs are a bedside indicator of futile resuscitation during massive transfusion. J. Trauma Acute Care Surg. 2023, 95, e19–e21. [Google Scholar] [CrossRef] [PubMed]
- Ranola, P.A.; Merchant, R.M.; Perman, S.M.; Khan, A.M.; Gaieski, D.; Caplan, A.L.; Kirkpatrick, J.N. How long is long enough, and have we done everything we should?--Ethics of calling codes. J. Med. Ethics 2015, 41, 663–666. [Google Scholar] [CrossRef]
- Anazodo, A.N.; Murthi, S.B.; Frank, M.K.; Hu, P.F.; Hartsky, L.; Imle, P.C.; Stephens, C.T.; Menaker, J.; Miller, C.; Dinardo, T.; et al. Assessing trauma care provider judgement in the prediction of need for life-saving interventions. Injury 2015, 46, 791–797. [Google Scholar] [CrossRef]
- Shiber, J.; Fontane, E.; Patel, J.; Akinleye, A.; Kerwin, A.; Chiu, W.; Scalea, T. Gestalt clinical severity score (GCSS) as a predictor of patient severity of illness or injury. Am. J. Emerg. Med. 2023, 66, 11–15. [Google Scholar] [CrossRef]
- Bhogadi, S.K.; Magnotti, L.J.; Hosseinpour, H.; Anand, T.; El-Qawaqzeh, K.; Nelson, A.; Colosimo, C.; Spencer, A.L.; Friese, R.; Joseph, B. The final decision among the injured elderly, to stop or to continue? Predictors of withdrawal of life supporting treatment. J. Trauma Acute Care Surg. 2023, 94, 778–783. [Google Scholar] [CrossRef] [PubMed]
- Eckstein, M. Termination of resuscitative efforts: Medical futility for the trauma patient. Curr. Opin. Crit. Care 2001, 7, 450–454. [Google Scholar] [CrossRef] [PubMed]
- Maas, A.I.; Lingsma, H.F.; Roozenbeek, B. Predicting outcome after traumatic brain injury. Handb. Clin. Neurol. 2015, 128, 455–474. [Google Scholar] [PubMed]
- Gang, M.C.; Hong, K.J.; Shin, S.D.; Song, K.J.; Ro, Y.S.; Kim, T.H.; Park, J.H.; Jeong, J. New prehospital scoring system for traumatic brain injury to predict mortality and severe disability using motor Glasgow Coma Scale, hypotension, and hypoxia: A nationwide observational study. Clin. Exp. Emerg. Med. 2019, 6, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Spaite, D.W.; Hu, C.; Bobrow, B.J.; Chikani, V.; Barnhart, B.; Gaither, J.B.; Denninghoff, K.R.; Adelson, P.D.; Keim, S.M.; Viscusi, C.; et al. The Effect of Combined Out-of-Hospital Hypotension and Hypoxia on Mortality in Major Traumatic Brain Injury. Ann. Emerg. Med. 2017, 69, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Martín-Rodríguez, F.; López-Izquierdo, R.; Mohedano-Moriano, A.; Polonio-López, B.; Maestre Miquel, C.; Viñuela, A.; Fernández, C.D.; Correas, J.G.; Marques, G.; Martín-Conty, J.L. Identification of Serious Adverse Events in Patients with Traumatic Brain Injuries, from Prehospital Care to Intensive-Care Unit, Using Early Warning Scores. Int. J. Environ. Res. Public Health 2020, 17, 1504. [Google Scholar] [CrossRef] [PubMed]
- Vrettou, C.S.; Fragkou, P.C.; Mallios, I.; Barba, C.; Giannopoulos, C.; Gavrielatou, E.; Dimopoulou, I. The Role of Automated Infrared Pupillometry in Traumatic Brain Injury: A Narrative Review. J. Clin. Med. 2024, 13, 614. [Google Scholar] [CrossRef] [PubMed]
- van Rein, E.A.J.; van der Sluijs, R.; Voskens, F.J.; Lansink, K.W.W.; Houwert, R.M.; Lichtveld, R.A.; de Jongh, M.A.; Dijkgraaf, M.G.W.; Champion, H.R.; Beeres, F.J.P.; et al. Development and Validation of a Prediction Model for Prehospital Triage of Trauma Patients. JAMA Surg. 2019, 154, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Åkerlund, C.A.I.; Holst, A.; Bhattacharyay, S.; Stocchetti, N.; Steyerberg, E.; Smielewski, P.; Menon, D.K.; Ercole, A.; Nelson, D.W. Clinical descriptors of disease trajectories in patients with traumatic brain injury in the intensive care unit (CENTER-TBI): A multicentre observational cohort study. Lancet Neurol. 2024, 23, 71–80. [Google Scholar] [CrossRef]
- Nelson, L.; Magnus, B.; Yue, J.; Balsis, S.; Patrick, C.; Temkin, N.; Diaz-Arrastia, R.; Manley, G. Data-driven characterization of traumatic brain injury severity from clinical, neuroimaging, and blood-based indicators. Res. Sq. 2024, preprint. [Google Scholar] [CrossRef]
- Walsh, M.; Thomas, S.; Kwaan, H.; Aversa, J.; Anderson, S.; Sundararajan, R.; Zimmer, D.; Bunch, C.; Stillson, J.; Draxler, D.; et al. Modern methods for monitoring hemorrhagic resuscitation in the United States: Why the delay? J. Trauma Acute Care Surg. 2020, 89, 1018–1022. [Google Scholar] [CrossRef] [PubMed]
- Gambhir, S.; Grigorian, A.; Ramakrishnan, D.; Kuza, C.M.; Sheehan, B.; Maithel, S.; Nahmias, J. Risk Factors for Withdrawal of Life-Sustaining Treatment in Severe Traumatic Brain Injury. Am. Surg. 2020, 86, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, A.K.; Shakil, H.; Smith, C.W.; Sader, N.; Ladha, K.; Wijeysundera, D.N.; Singhal, A.; Kulkarni, A.V.; Wilson, J.R.; Witiw, C.D.; et al. Withdrawal of Life-Sustaining Treatment for Pediatric Patients With Severe Traumatic Brain Injury. JAMA Surg. 2024, 159, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Amare, A.T.; Tesfaye, T.D.; Ali, A.S.; Woelile, T.A.; Birlie, T.A.; Kebede, W.M.; Tassew, S.F.; Chanie, E.S.; Fleke, D.G. Survival status and predictors of mortality among traumatic brain injury patients in an Ethiopian hospital: A retrospective cohort study. Afr. J. Emerg. Med. 2021, 11, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Barki, M.T.; Filza, F.; Khattak, A.F.; Khalid, O.B.; Qazi, M.; Gilani, H.; Ayub, S.; Farooq, M. A Survey of Traumatic Brain Injuries from Road Traffic Collisions in a Lower Middle-Income Country. Cureus 2023, 15, e36892. [Google Scholar] [CrossRef] [PubMed]
- McKeown, R.E. The Epidemiologic Transition: Changing Patterns of Mortality and Population Dynamics. Am. J. Lifestyle Med. 2009, 3, 19s–26s. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.; Barber, R.M.; Foreman, K.J.; Abbasoglu Ozgoren, A.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Abraham, J.P.; Abubakar, I.; Abu-Raddad, L.J.; et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: Quantifying the epidemiological transition. Lancet 2015, 386, 2145–2191. [Google Scholar] [CrossRef] [PubMed]
- Reddy, C.L.; Peters, A.W.; Jumbam, D.T.; Caddell, L.; Alkire, B.C.; Meara, J.G.; Atun, R. Innovative financing to fund surgical systems and expand surgical care in low-income and middle-income countries. BMJ Glob. Health 2020, 5, e002375. [Google Scholar] [CrossRef] [PubMed]
- Frechette, R.; Colas, N.; Augustin, M.; Edema, N.; Pyram, G.; Louis, S.; Crevecoeur, C.E.; Mathurin, C.; Louigne, R.; Patel, B.; et al. Sustainable surgical resource initiative for Haiti: The SSRI-Haiti project. Glob. Health Action. 2023, 16, 2180867. [Google Scholar] [CrossRef]
- Milton, M.; Engelbrecht, A.; Geyser, M. Predicting mortality in trauma patients—A retrospective comparison of the performance of six scoring systems applied to polytrauma patients from the emergency centre of a South African central hospital. Afr. J. Emerg. Med. 2021, 11, 453–458. [Google Scholar] [CrossRef]
- Vukoja, M.; Riviello, E.D.; Schultz, M.J. Critical care outcomes in resource-limited settings. Curr. Opin. Crit. Care 2018, 24, 421–427. [Google Scholar] [CrossRef]
- Bosslet, G.T.; Pope, T.M.; Rubenfeld, G.D.; Lo, B.; Truog, R.D.; Rushton, C.H.; Curtis, J.R.; Ford, D.W.; Osborne, M.; Misak, C.; et al. An Official ATS/AACN/ACCP/ESICM/SCCM Policy Statement: Responding to Requests for Potentially Inappropriate Treatments in Intensive Care Units. Am. J. Respir. Crit. Care Med. 2015, 191, 1318–1330. [Google Scholar] [CrossRef]
- De-Arteaga, M.; Elmer, J. Self-fulfilling prophecies and machine learning in resuscitation science. Resuscitation 2023, 183, 109622. [Google Scholar] [CrossRef] [PubMed]
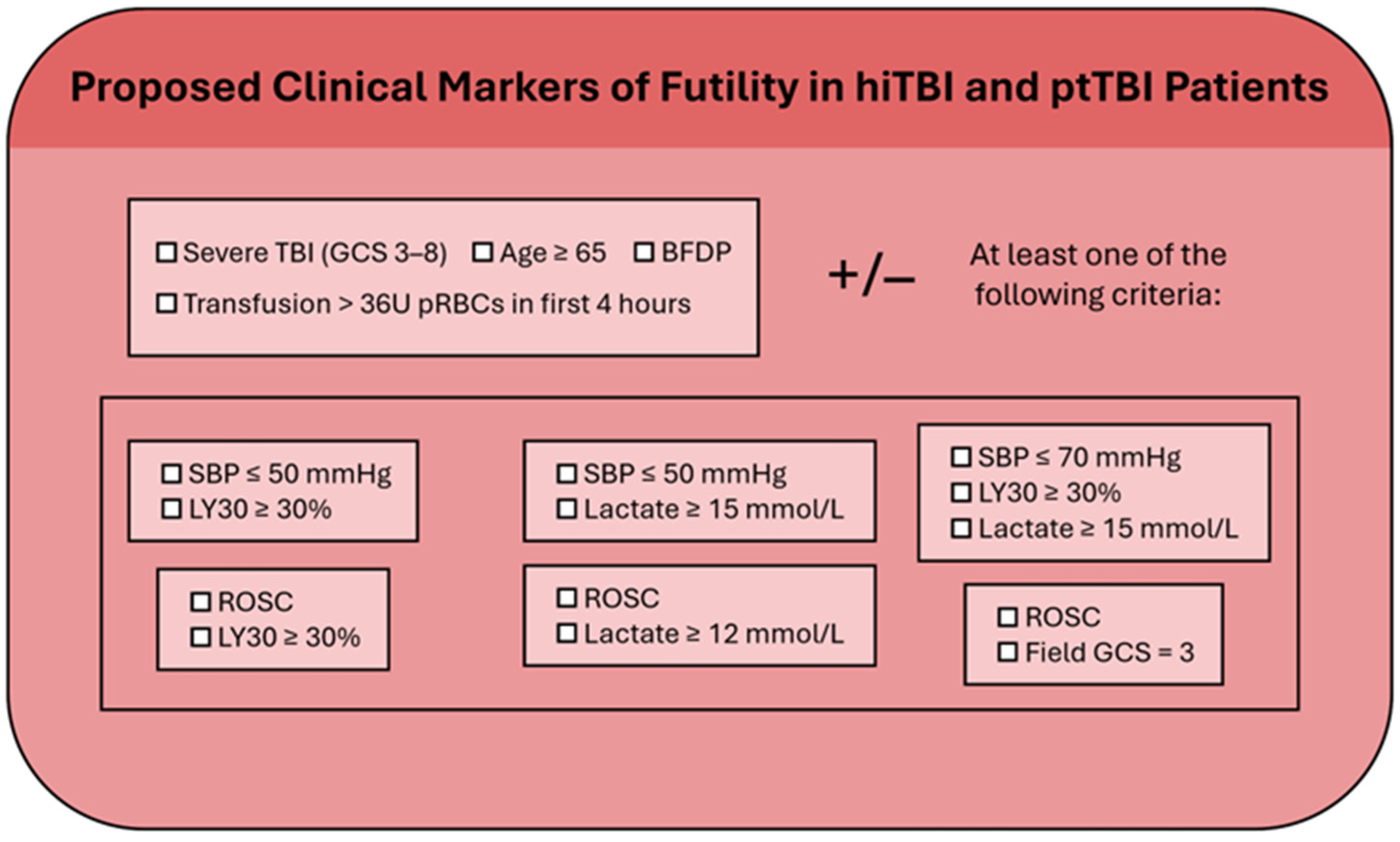
| Variable | PPV, % | NPV, % | Sn, % | Sp, % |
|---|---|---|---|---|
| Arrival SBP ≤ 50 and LY30 ≥ 30% | 100 | 78 | 33 | 100 |
| Arrival SBP ≤ 50 and lactate ≥ 15 | 100 | 77 | 31 | 100 |
| Arrival SBP ≤ 70, LY30 ≥ 30%, and lactate ≥ 15 | 100 | 77 | 30 | 100 |
| ROSC and LY30 ≥ 30% | 100 | 78 | 33 | 100 |
| ROSC and lactate ≥ 12 | 100 | 76 | 29 | 100 |
| ROSC and field GCS 3 | 100 | 77 | 27 | 100 |
| TBI Type | Hemorrhage and Coagulopathy | Abbreviated Head Injury Score | Abbreviated Extracranial Injury Score | Common Futility Wait Time Recommendations | Common Futility Wait Times in Clinical Practice |
|---|---|---|---|---|---|
| iTBI | No | ≥3 | <3 | 72 h | 72 h |
| hiTBI | Yes | ≥3 | <3 | Variable | <72 h * |
| ptTBI | Yes | ≥3 | >3 | Variable | 2–6 h ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Fadhl, M.D.; Karam, M.N.; Chen, J.; Zackariya, S.K.; Lain, M.C.; Bales, J.R.; Higgins, A.B.; Laing, J.T.; Wang, H.S.; Andrews, M.G.; et al. Traumatic Brain Injury as an Independent Predictor of Futility in the Early Resuscitation of Patients in Hemorrhagic Shock. J. Clin. Med. 2024, 13, 3915. https://doi.org/10.3390/jcm13133915
Al-Fadhl MD, Karam MN, Chen J, Zackariya SK, Lain MC, Bales JR, Higgins AB, Laing JT, Wang HS, Andrews MG, et al. Traumatic Brain Injury as an Independent Predictor of Futility in the Early Resuscitation of Patients in Hemorrhagic Shock. Journal of Clinical Medicine. 2024; 13(13):3915. https://doi.org/10.3390/jcm13133915
Chicago/Turabian StyleAl-Fadhl, Mahmoud D., Marie Nour Karam, Jenny Chen, Sufyan K. Zackariya, Morgan C. Lain, John R. Bales, Alexis B. Higgins, Jordan T. Laing, Hannah S. Wang, Madeline G. Andrews, and et al. 2024. "Traumatic Brain Injury as an Independent Predictor of Futility in the Early Resuscitation of Patients in Hemorrhagic Shock" Journal of Clinical Medicine 13, no. 13: 3915. https://doi.org/10.3390/jcm13133915
APA StyleAl-Fadhl, M. D., Karam, M. N., Chen, J., Zackariya, S. K., Lain, M. C., Bales, J. R., Higgins, A. B., Laing, J. T., Wang, H. S., Andrews, M. G., Thomas, A. V., Smith, L., Fox, M. D., Zackariya, S. K., Thomas, S. J., Tincher, A. M., Al-Fadhl, H. D., Weston, M., Marsh, P. L., ... Walsh, M. M., on behalf of the Futile Indicators for Stopping Transfusion in Trauma (FISTT) Collaborative Group. (2024). Traumatic Brain Injury as an Independent Predictor of Futility in the Early Resuscitation of Patients in Hemorrhagic Shock. Journal of Clinical Medicine, 13(13), 3915. https://doi.org/10.3390/jcm13133915









