Influence of Method of Treatment of Mandibular Condylar Fractures on Range of Articular Path Measured by Cadiax Device
Abstract
1. Introduction
2. Materials and Methods
- A single fracture of the condylar process, regardless of the dislocation and degree of head dislocation in the TMJ, and regardless of the treatment method used.
- No other injuries of the facial skeleton upon admission to the clinic and in the period from the end of treatment to examination with the Cadiax device.
- Permissible simultaneous fracture of the mandibular body treated in a similar way to the fractured condylar process with anatomical effect.
- No further trauma to the TMJ in the period between the completed treatment of the condylar process fracture and the examination of the articular path for the needs of the analysis.
- Adult patients without systemic diseases.
- Patients without TMJ disorders based on the history.
- Presence of teeth in the upper and lower arch for lateral support.
- No malocclusion.
- Consent for testing with the Cadiax device.
- Group I: 20 patients qualified for conservative treatment who underwent condylar fracture treatment with the use of an elastic fixation based on standard dental splints for a period of 3 weeks. The eligibility criteria for conservative treatment in the above-mentioned period were mainly fractures without significant fragment dislocation and without occlusal disorders.
- Group II: 40 patients qualified for surgical treatment of mandibular condylar fractures. The eligibility criteria for surgical treatment in the above-mentioned period were mainly fractures with dislocation of the fragments disrupting the occlusion.
- Twelve patients: after fracture of the condylar process without dislocation of the head in the joint—internal fixation (IF).
- Eight patients: after fracture with displacement and fragmentation of the head of the condylar process possible for fixation—external fixation (EF)
- Thirteen patients: after shattering the head of the mandible that did not qualify for fixation—fragments of the head were removed without cutting branches and without additional procedures [R1—removal without cutting branches]
- Seven patients: after shattering the head of the mandible that was not eligible for fixation, fragments of the head were removed, mandible branch cut, shaped, and the positioned to rebuild height of the branch [R2—removal with cutting and branch modeling]
- Adult patients without systemic diseases.
- Patients without a TMJ injury and without symptoms suggesting TMJ disorders, including arthropathies.
- No malocclusion.
- Full dental arches.
- Consent for testing with the Cadiax device.
3. Results
- Internal Fixation (IF)—typical fixation of fractures with titanium plates after adjusting the condylar process in anatomical positions.
- External Fixation (EF)—vertical cut of mandible branch, removal of fractured head, extracorporeal fixation of its elements with screws, extracorporeal attachment of the head of the convex branch, and fixation to the mandible.
- Removal without cutting branches [R1].
- Removal with cutting and modeling the branch [R2]—after cutting the branch, head fragment removal, modeling, and transposition of the branch.
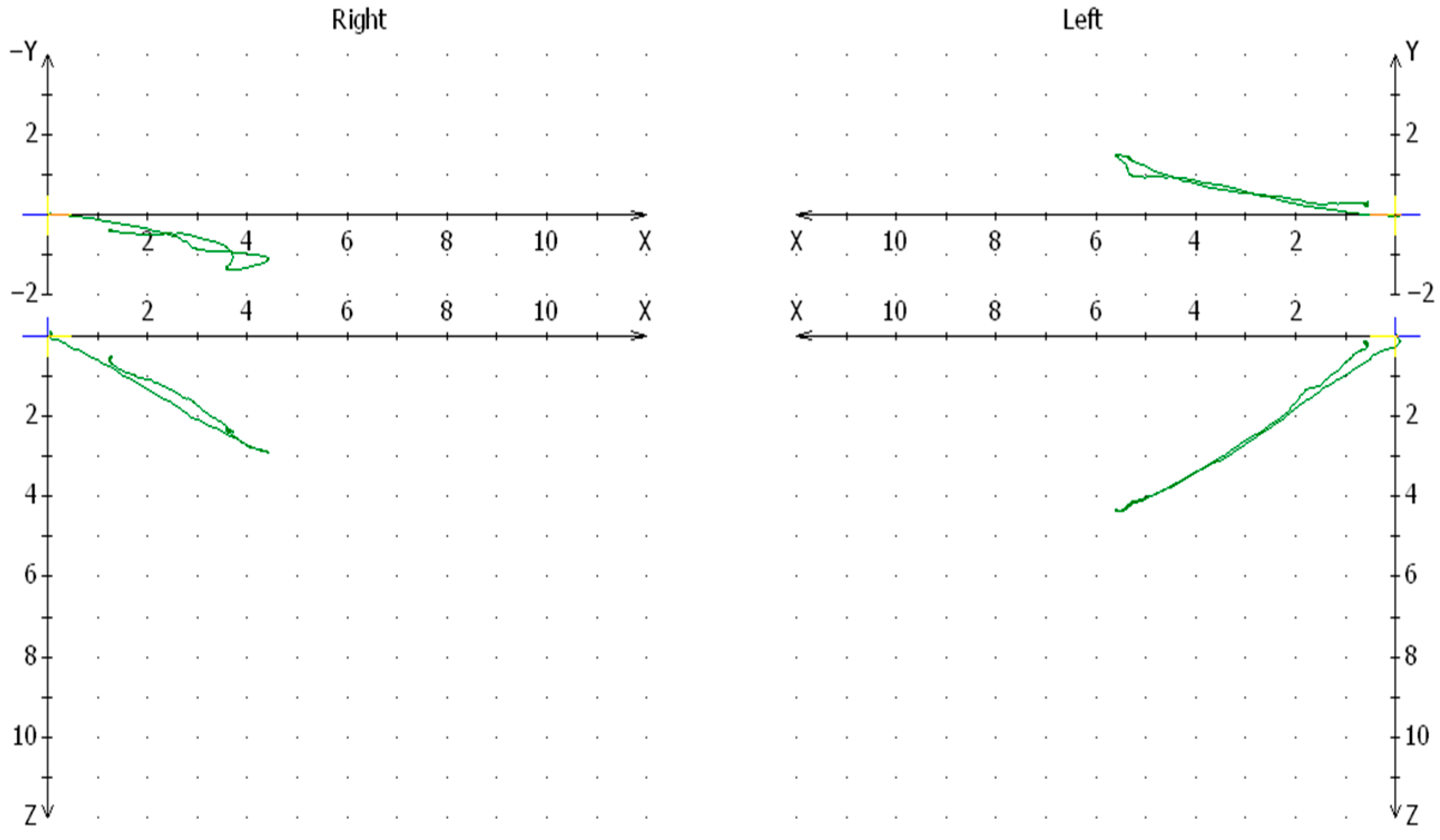
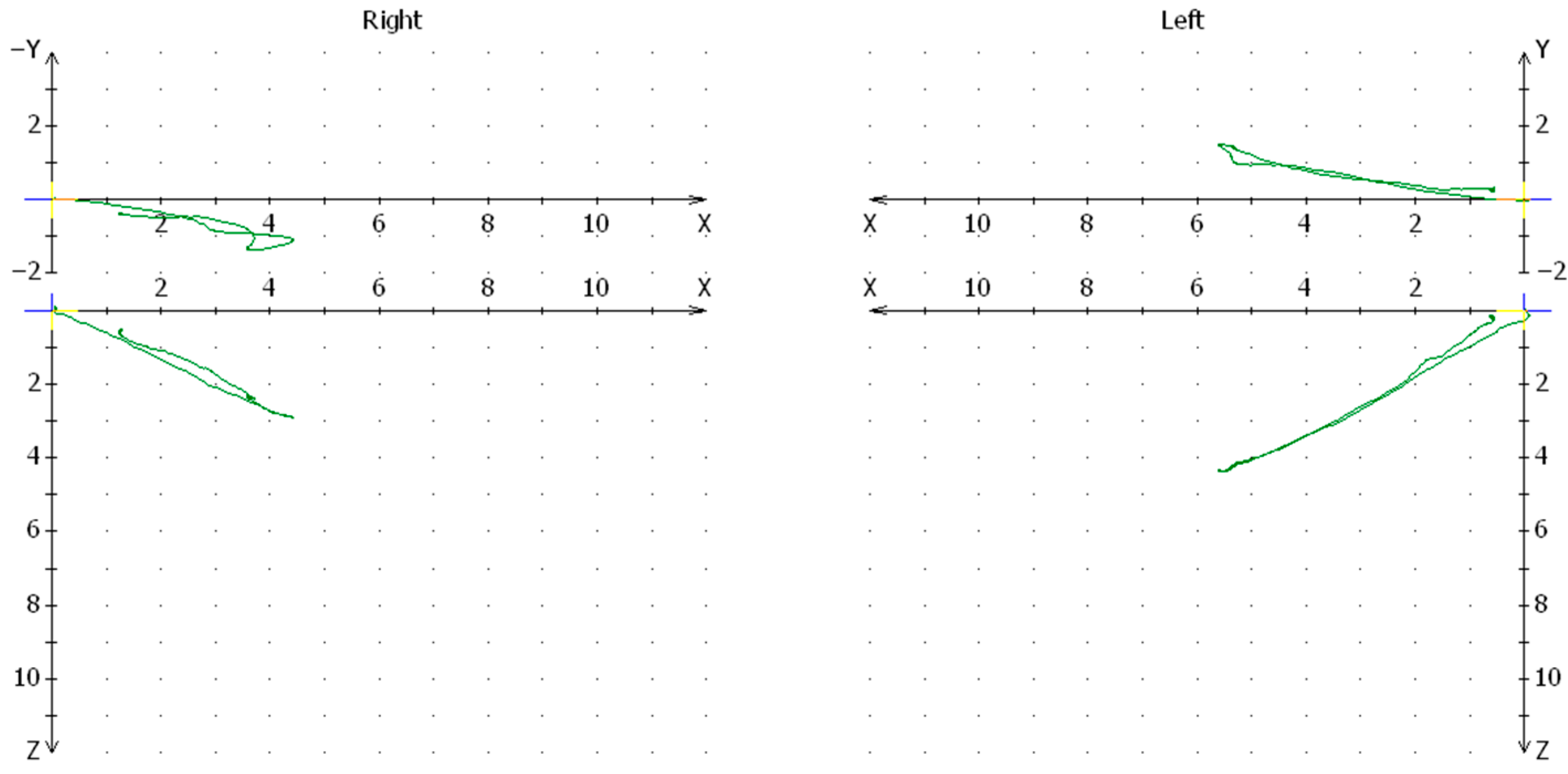
Comparison of Average Values of The Condylar Path in the Group of Patients Treated with Conservative and Surgical Method in Comparison to the Control Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bae, S.S.; Aronovich, S. Trauma to the Pediatric Temporomandibular Joint. Oral Maxillofac. Surg. Clin. North Am. 2018, 30, 47–60. [Google Scholar] [CrossRef] [PubMed]
- Boffano, P.; Kommers, S.C.; Karagozoglu, K.H.; Gallesio, C.; Forouzanfar, T. Mandibular trauma: A two-centre study. Int. J. Oral Maxillofac. Surg. 2015, 44, 998–1004. [Google Scholar] [CrossRef] [PubMed]
- Lindahl, L. Condylar fractures of the mandible: I. Classification and relation to age, occlusion, and concomitant injuries of teeth and teeth-supporting structures, and fractures of the mandibular body. Int. J. Oral Surg. 1977, 6, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Kozakiewicz, M.; Swiniarski, J. “a” Shape Plate for Open Rigid Internal Fixation of Mandible Condyle Neck Fracture. J. Cranio-Maxillofac. Surg. 2014, 42, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.; Kahn, J.L.; Boutemi, P.; Wilk, A. Photoelastic analysis of bone deformation in the region of the mandibular condyle during mastication. J. Cranio-Maxillofac. Surg. 2002, 30, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Haim, D. Biomechanical study of the delta plate and the TriLock Delta condyle trauma plate. J. Oral Maxillofac. Surg. 2011, 69, 2619–2625. [Google Scholar] [CrossRef] [PubMed]
- Aquilina, P.; Chamoli, U.; Parr, W.C.H.; Clausen, P.D.; Wroe, S. Finite element analysis of three patterns of internal fixation of fractures of the mandibular condyle. Br. J. Oral Maxillofac. Surg. 2013, 51, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Vartanian, A.J.; Alvi, A. Bone-screw mandible fixation: An intraoperative alternative to arch bars. Otolaryngol.—Head Neck Surg. 2000, 123, 718–721. [Google Scholar] [CrossRef] [PubMed]
- Nandini, G.D.; Balakrishna, R.; Rao, J. Self Tapping Screws v/s Erich Arch Bar for Inter Maxillary Fixation: A Comparative Clinical Study in the Treatment of Mandibular Fractures. J. Maxillofac. Oral Surg. 2011, 10, 127–131. [Google Scholar] [CrossRef]
- Choi, J.W.; Kim, H.B.; Jeong, W.S.; Kim, S.C.; Koh, K.S. Comparison Between Intermaxillary Fixation with Screws and an Arch Bar for Mandibular Fracture. J. Craniofacial Surg. 2019, 30, 1787–1789. [Google Scholar] [CrossRef]
- Banks, P. A pragmatic approach to the management of condylar fractures. Int. J. Oral Maxillofac. Surg. 1998, 27, 244–246. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.Y.; Yang, J.D.; Chung, H.Y.; Cho, B.C. Current concepts in the mandibular condyle fracture management part I: Overview of condylar fracture. Arch. Plast. Surg. 2012, 39, 291–300. [Google Scholar] [CrossRef]
- Valiati, R. The treatment of condylar fractures: To open or not to open? A critical review of this controversy. Int. J. Med. Sci. 2008, 5, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Haug, R.H.; Assael, L.A. Outcomes of open versus closed treatment of mandibular subcondylar fractures. J. Oral Maxillofac. Surg. 2001, 59, 370–375. [Google Scholar] [CrossRef]
- Tullio, A.; Sesenna, E. Role of surgical reduction of condylar fractures in the management of panfacial fractures. Br. J. Oral Maxillofac. Surg. 2000, 38, 472–476. [Google Scholar] [CrossRef] [PubMed]
- Rastogi, S.; Sharma, S.; Kumar, S.; Reddy, M.P.; Indra, N. Fracture of mandibular condyle—To open or not to open: An attempt to settle the controversy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 119, 608–613. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, D.A. A multicentre audit of unilateral fractures of the mandibular condyle. Br. J. Oral Maxillofac. Surg. 1997, 35, 230–236. [Google Scholar] [CrossRef]
- He, D.; Yang, C.; Chen, M.; Jiang, B.; Wang, B. Intracapsular Condylar Fracture of the Mandible: Our Classification and Open Treatment Experience. J. Oral Maxillofac. Surg. 2009, 67, 1672–1679. [Google Scholar] [CrossRef]
- Kempers, K.G.; Quinn, P.D.; Silverstein, K. Surgical approaches to mandibular condylar fractures: A review. J. Cranio-Maxillofac. Trauma 1999, 5, 25–30. [Google Scholar]
- Bhavsar, D.; Barkdull, G.; Berger, J.; Tenenhaus, M. A novel surgical approach to subcondylar fractures of mandible. J. Craniofacial Surg. 2008, 19, 496–499. [Google Scholar] [CrossRef]
- Meyer, C.; Martin, E.; Kahn, J.L.; Zink, S. Development and biomechanical testing of a new osteosynthesis plate (TCP®) designed to stabilize mandibular condyle fractures. J. Cranio-Maxillofac. Surg. 2007, 35, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Conci, R.A. Does lag screw fixation of condylar fractures result in adequate stability? A finite element analysis. J. Cranio-Maxillofac. Surg. 2018, 46, 1041–1045. [Google Scholar] [CrossRef] [PubMed]
- Leonhardt, H.; Franke, A.; McLeod, N.M.H.; Lauer, G.; Nowak, A. Fixation of fractures of the condylar head of the mandible with a new magnesium-alloy biodegradable cannulated headless bone screw. Br. J. Oral Maxillofac. Surg. 2017, 55, 623–625. [Google Scholar] [CrossRef] [PubMed]
- Dimitroulis, G. Condylar injuries in growing patients. Aust. Dent. J. 1997, 42, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.L.; Misch, K.; Wang, H.L. Dental imaging in implant treatment planning. Implant Dent. 2010, 19, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Visser, H.; Rödig, T.; Hermann, K.P. Dose Reduction by Direct-Digital Cephalometric Radiography. Angle Orthod. 2001, 71, 159–163. [Google Scholar] [PubMed]
- Wilson, I.; Lokeh, A.B.C. Prospective comparison of panoramic tomography (zonography) and helical computed tomography in the diagnosis and operative management of mandibular fractures. Plast. Reconstr. Surg. 2001, 107, 1369–1375. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.P. Modification of the measurement of the major variables in mandibular condylar fractures: Angulation of sidewards displacement and shortening of the height of the ramus. Br. J. Oral Maxillofac. Surg. 2018, 56, 113–119. [Google Scholar] [CrossRef]
- Kaeppler, G.; Cornelius, C.P.; Ehrenfeld, M.; Mast, G. Diagnostic efficacy of cone-beam computed tomography for mandibular fractures. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, 98–104. [Google Scholar] [CrossRef]
- Emshoff, R. Magnetic resonance imaging findings of internal derangement in temporomandibular joints without a clinical diagnosis of temporomandibular disorder. J. Oral Rehabil. 2002, 29, 516–522. [Google Scholar] [CrossRef]
- Zheng, J. Assessment of magnetic resonance images of displacement of the disc of the temporomandibular joint in different types of condylar fracture. Br. J. Oral Maxillofac. Surg. 2016, 54, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, R.E.; Plambeck, K.; Bartel-Friedrich, S.; Giese, M.; Schmelzle, R. Limitations of B-scan ultrasound for diagnosing fractures of the mandibular condyle and ramus. Clin. Oral Investig. 2001, 5, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Guarda-Nardini, L. Ultrasonography of the temporomandibular joint: A literature review. Int. J. Oral Maxillofac. Surg. 2009, 38, 1229–1236. [Google Scholar] [CrossRef] [PubMed]
- Adeyemo, W.L.; Akadiri, O.A. A systematic review of the diagnostic role of ultrasonography in maxillofacial fractures. Int. J. Oral Maxillofac. Surg. 2011, 40, 655–661. [Google Scholar] [CrossRef] [PubMed]
- Ambrose, J. Computerized transverse axial scanning (tomography): II. Clinical application. Br. J. Radiol. 1973, 46, 1023–1047. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, I.; Abrahami, E.; Mintz, S.S. Demonstration of condylar fractures of the mandible by computed tomography. Oral Surg. Oral Med. Oral Pathol. 1982, 54, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Schubert, W. Radiographic diagnosis of mandibular fractures: Mode and implications. Oper. Tech. Otolaryngol.—Head Neck Surg. 2002, 13, 246–253. [Google Scholar] [CrossRef]
- Loukota, R.A.; Eckelt, U.; de Bont, L.; Rasse, M. Subclassification of fractures of the condylar process of the mandible. Br. J. Oral Maxillofac. Surg. 2005, 43, 72–73. [Google Scholar] [CrossRef]
- Powers, D.B. Classification of Mandibular Condylar Fractures. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2017, 25, 1–10. [Google Scholar] [CrossRef]
- Kozakiewicz, M. Classification proposal for fractures of the processus condylaris mandibulae. Clin. Oral Investig. 2019, 23, 485–491. [Google Scholar] [CrossRef]
- Neff, A.; Cornelius, C.P.; Rasse, M.; Torre, D.D.; Audigé, L. The comprehensive AOCMF classification system: Condylar process fractures—Level 3 tutorial. Craniomaxillofacial Trauma Reconstr. 2014, 7, S44–S58. [Google Scholar] [CrossRef] [PubMed]
- Kozakiewicz, M. Złamania Wyrostka Kłykciowego Żuchwy; PZWL: Warsaw, Poland, 2019. [Google Scholar]
- Starcke, E.N. The history of articulators: Pursuing the evolution of the incisal-pin and guide, part II. J. Prosthodont. 2001, 10, 113–121. [Google Scholar] [CrossRef]
- Isaacson, D. A clinical study of the Bennett movement. J. Prosthet. Dent. 1958, 8, 641–649. [Google Scholar] [CrossRef]
- Goulet, J.; Clark, G.; Flack, V.; Liu, C. The reproducibility of muscle and joint tenderness detection methods and maximum mandibular movement measurment for temporomandibular system. J. Orofac. Pain 1998, 12, 17–26. [Google Scholar] [PubMed]
- Torabi, K.; Pour, S.; Ahangari, A.; Ghodsi, S. A Clinical Comparative Study of Cadiax Compact II and Intraoral Records Using Wax and Addition Silicone. Int. J. Prosthodont. 2014, 27, 541–543. [Google Scholar] [CrossRef]
- Brandt, M.T.; Haug, R.H. Open Versus Closed Reduction of Adult Mandibular Condyle Fractures: A Review of the Literature Regarding the Evolution of Current Thoughts on Management. J. Oral Maxillofac. Surg. 2003, 61, 1324–1332. [Google Scholar] [CrossRef]
- Umstadt, H.E.; Ellers, M.; Müller, H.H.; Austermann, K.H. Functional reconstruction of the TM joint in cases of severely displaced fractures and fracture dislocation. J. Cranio-Maxillofac. Surg. 2000, 28, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Shiju, M. Fractures of the mandibular condyle—Open versus closed—A treatment dilemma. J. Cranio-Maxillofac. Surg. 2015, 43, 448–451. [Google Scholar] [CrossRef]
- Handschel, J. Comparison of various approaches for the treatment of fractures of the mandibular condylar process. J. Cranio-Maxillofac. Surg. 2012, 40, e397–e401. [Google Scholar] [CrossRef] [PubMed]
- Berner, T. Closed versus open treatment of mandibular condylar process fractures: A meta-analysis of retrospective and prospective studies. J. Cranio-Maxillofac. Surg. 2015, 43, 1404–1408. [Google Scholar] [CrossRef]






| Groups | Mean Value of Condylar Path | Sex | Age | Time Injury-Treatment (Days) | ||||
|---|---|---|---|---|---|---|---|---|
| Healthy Side | Injured Side | Women | Men | |||||
| Group I—conservative treatment | 20 | 11.01 | 10.07 | 12 | 8 | 31.70 ± 11.46 | 3.900 ± 2.424 | |
| Group 2—surgical treatment | Internal Fixation (IF) | 12 | 11.54 | 9.19 | 1 | 11 | 32.92 ± 10.92 | 3.400 ± 2.793 |
| External Fixation (EF) | 8 | 9.16 | 4.53 | 4 | 4 | 30.00 ± 14.99 | 5.800 ± 2.949 | |
| Removal (R1) | 13 | 10.94 | 4.71 | 2 | 11 | 33.54 ± 14.08 | 7.000 ± 6.066 | |
| Removal with modeling (R2) | 7 | 8.64 | 5.45 | 4 | 3 | 42.86 ± 11.16 | 5.000 ± 2.828 | |
| Control group | 20 | Healthy | 12 | 8 | 26.95 ± 5.605 | No treatment | ||
| 12.73 | 12.69 | |||||||
| Conservative Treatment | |||||
|---|---|---|---|---|---|
| Cases | Mean Condylar Path Value Healthy Side | Deviation | Mean Condylar Path ValueInjured Side | Deviation | |
| Conservative | 20 | 10.07 | 2.56 | 11.01 | 2.47 |
| Healthy Right Side | Healthy Left Side | ||||
| Control | 20 | 12.73 | 2.93 | 12.69 | 2.66 |
| Student’s t-test p < 0.001 | |||||
| Surgical Treatment | |||||
|---|---|---|---|---|---|
| Cases | Mean Condylar Path Value Healthy Side | Deviation | Mean Condylar Path Value Injured Side | Deviation | |
| Surgical | 40 | 10.362 | 2804 | 6.152 | 3250 |
| Healthy Right Side | Healthy Left SidE | ||||
| Control | 20 | 12.73 | 2.93 | 12.69 | 2.66 |
| Student’s t-test p < 0.001 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niedzielski, D.; Niedzielska, I.; Wziątek-Kuczmik, D.; Kamiński, M.; Baron, S.; Grzegorczyn, S. Influence of Method of Treatment of Mandibular Condylar Fractures on Range of Articular Path Measured by Cadiax Device. J. Clin. Med. 2024, 13, 3706. https://doi.org/10.3390/jcm13133706
Niedzielski D, Niedzielska I, Wziątek-Kuczmik D, Kamiński M, Baron S, Grzegorczyn S. Influence of Method of Treatment of Mandibular Condylar Fractures on Range of Articular Path Measured by Cadiax Device. Journal of Clinical Medicine. 2024; 13(13):3706. https://doi.org/10.3390/jcm13133706
Chicago/Turabian StyleNiedzielski, Damian, Iwona Niedzielska, Daria Wziątek-Kuczmik, Maciej Kamiński, Stefan Baron, and Sławomir Grzegorczyn. 2024. "Influence of Method of Treatment of Mandibular Condylar Fractures on Range of Articular Path Measured by Cadiax Device" Journal of Clinical Medicine 13, no. 13: 3706. https://doi.org/10.3390/jcm13133706
APA StyleNiedzielski, D., Niedzielska, I., Wziątek-Kuczmik, D., Kamiński, M., Baron, S., & Grzegorczyn, S. (2024). Influence of Method of Treatment of Mandibular Condylar Fractures on Range of Articular Path Measured by Cadiax Device. Journal of Clinical Medicine, 13(13), 3706. https://doi.org/10.3390/jcm13133706






