Hyperbaric Oxygen Therapy for Complications in Nipple-Sparing Mastectomy with Breast Reconstruction: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Inclusion Criteria
2.3.1. Population
2.3.2. Intervention
2.3.3. Comparison
2.3.4. Outcome Measures
2.3.5. Study Designs
2.3.6. Publication Date and Language
2.4. Exclusion Criteria
2.4.1. Study Design
2.4.2. Non-English Publications
2.4.3. Unrelated Interventions
2.4.4. Irrelevant Outcomes
2.4.5. Duplicated Articles
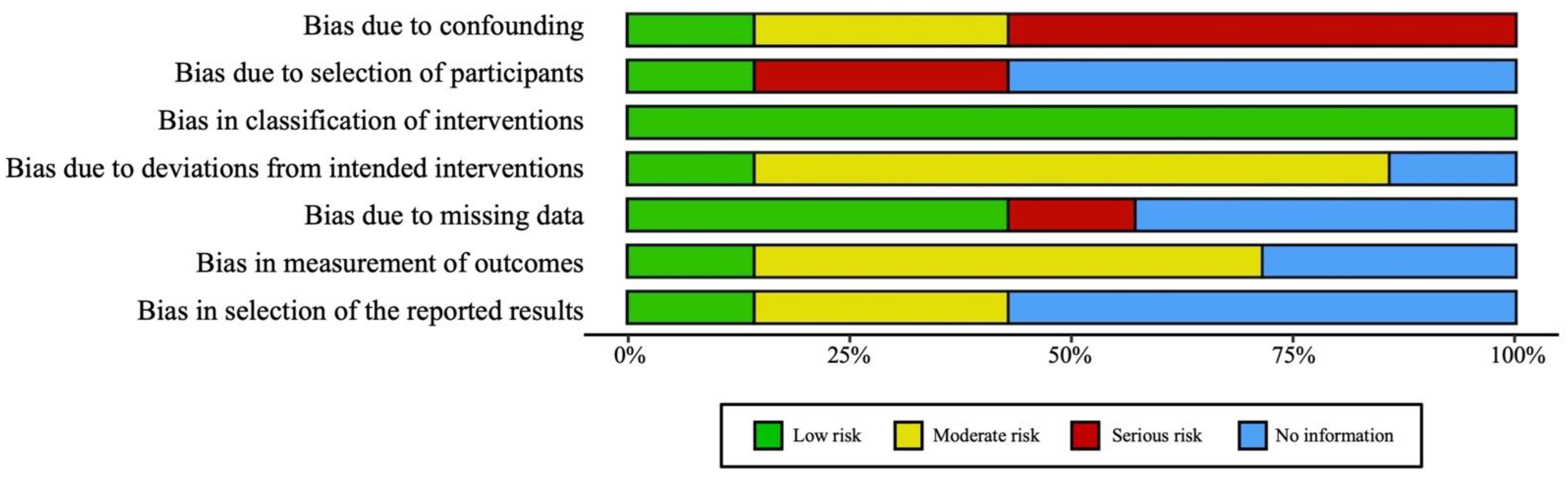
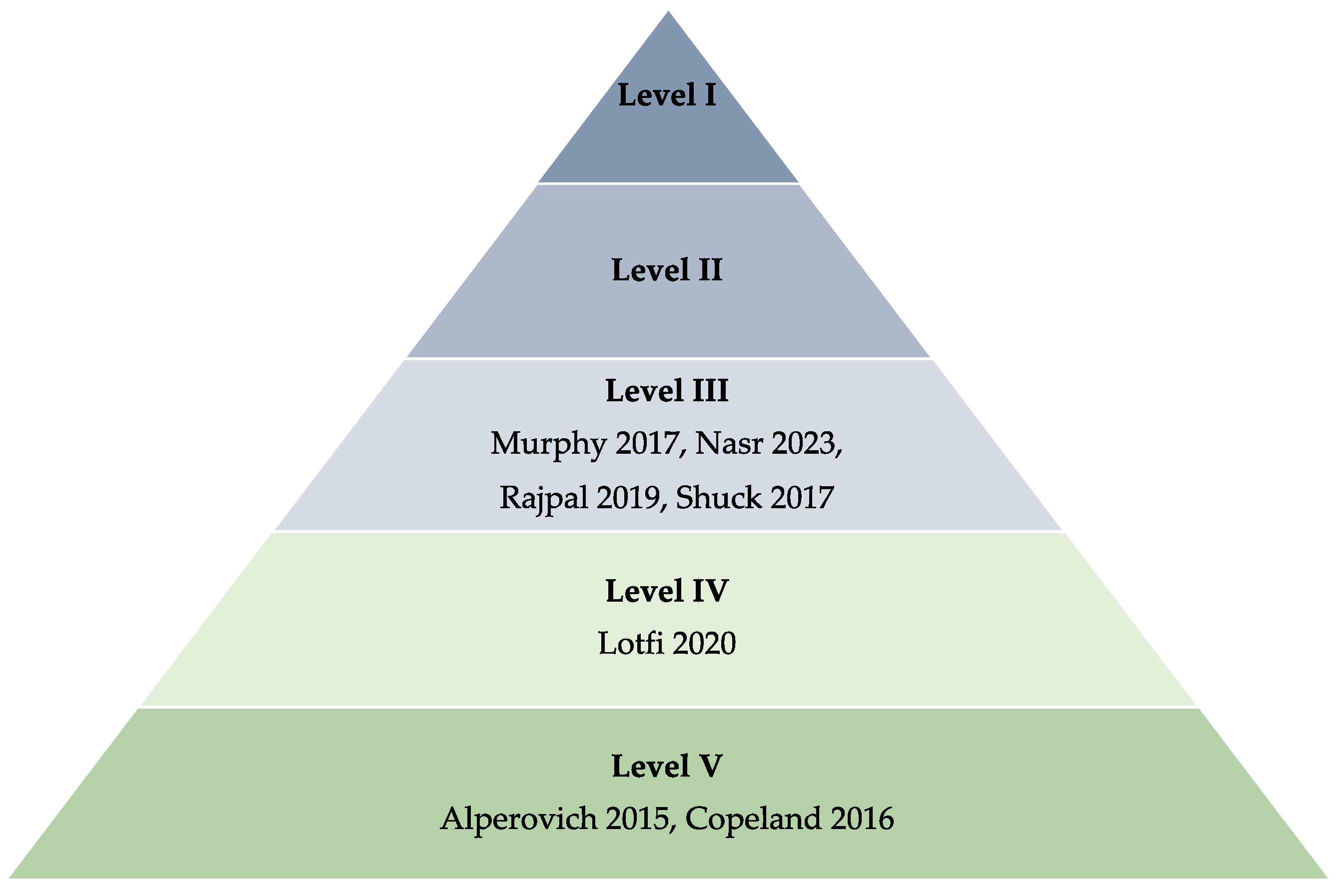
2.5. Quality Assessment and Evidence Level Classification
2.6. Data Extraction
3. Results
3.1. Summary of Selected Studies
3.2. Data Synthesis and Analysis
3.3. Assessment of Comorbidities of the Included Patient Population
3.4. Influence of the Timing of HBOT Intervention on Managing Threatened Skin Flap Necrosis Post-NSM
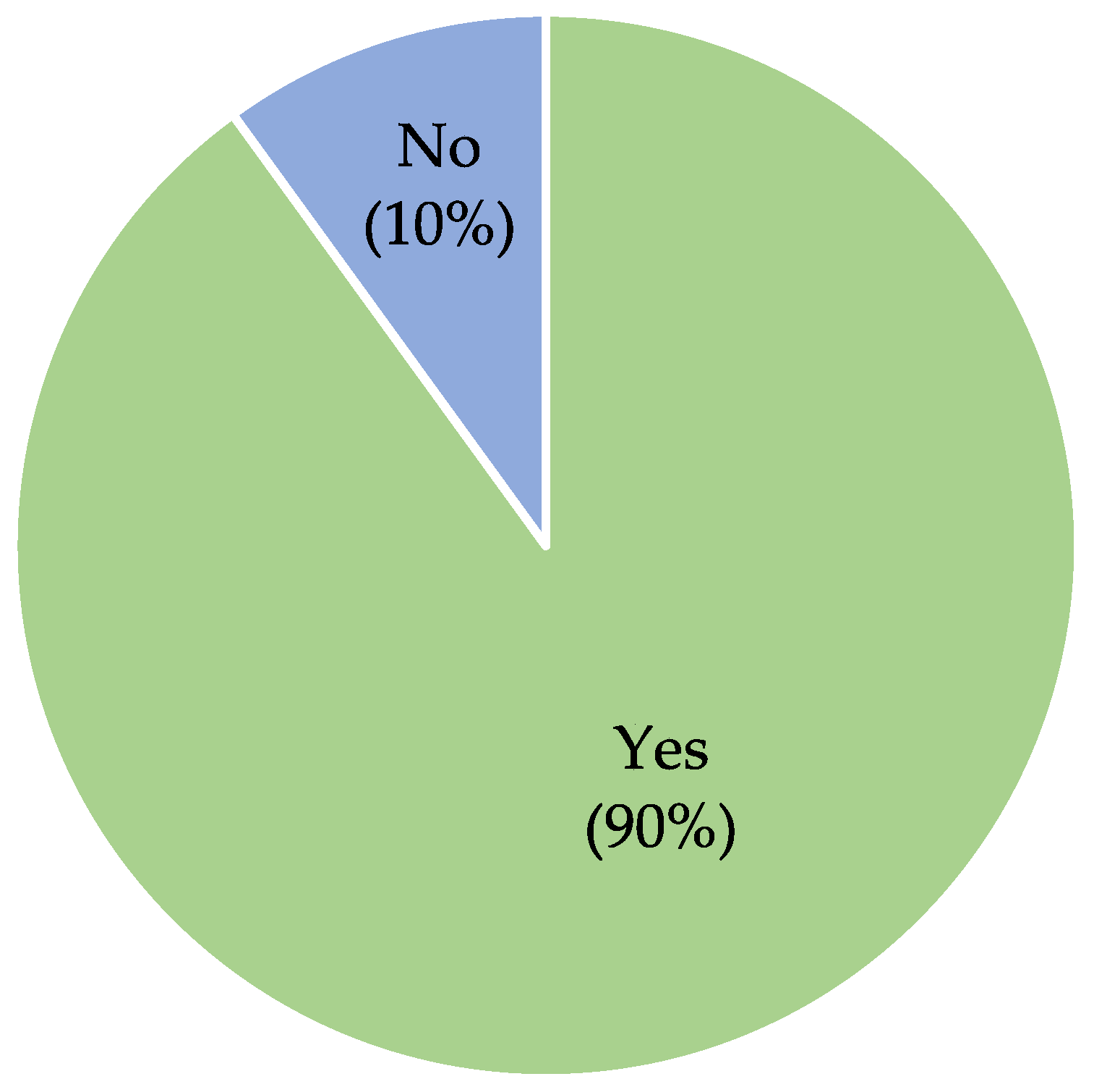
3.5. Qualitative Analysis of HBOT Efficacy in Managing Flap Ischemia and Threatened Skin Flap Necrosis Post-NSM
3.6. Assessment of HBOT Efficacy for Various Surgical Complications following NSM
4. Discussion
4.1. HBOT and Its Role as Post-Operative Treatment
4.2. Mechanism of Action of HBOT and Factors Contributing to Its Efficacy
4.3. Impact of Comorbidities on HBOT Efficacy in Patients Undergoing NSM
4.4. Role of HBOT in Surgical Complications following NSM
4.5. Safety of HBOT
4.6. Limitations and Future Direction
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Masannat, Y.; Agrawal, A.; Maraqa, L.; Fuller, M.; Down, S.; Tang, S.; Pang, D.; Kontos, M.; Romics, L.; Heys, S. Multifocal and multicentric breast cancer, is it time to think again? Ann. R. Coll. Surg. Engl. 2020, 102, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Carbine, N.E.; Lostumbo, L.; Wallace, J.; Ko, H. Risk-reducing mastectomy for the prevention of primary breast cancer. Cochrane Database Syst. Rev. 2018, 4, CD002748. [Google Scholar] [CrossRef] [PubMed]
- Bland, K.I.; Chang, H.R.; Copeland, E.M., III. Modified radical and simple mastectomies. In The Breast; Elsevier: Amsterdam, The Netherlands, 2018; pp. 443–461. [Google Scholar]
- Galimberti, V.; Vicini, E.; Corso, G.; Morigi, C.; Fontana, S.; Sacchini, V.; Veronesi, P. Nipple-sparing, and skin-sparing mastectomy: Review of aims, oncological safety and contraindications. Breast 2017, 34, S82–S84. [Google Scholar] [CrossRef] [PubMed]
- Parus, A.; Venturi, M.L. A strategic approach to nipple-sparing mastectomy reconstruction with a wide-based inframammary fold flap. Plast. Reconstr. Surg. 2020, 8, e3053. [Google Scholar] [CrossRef]
- Burke, E.E.; Laronga, C.; Sun, W.; DeBiase, S.; Naqvi, S.M.H.; Fridley, B.; Czerniecki, B.J.; Hoover, S.J.; Khakpour, N.; Kiluk, J.V.; et al. Implant-sparing mastectomy: An alternative for women undergoing mastectomy with retropectoral implants. Clin. Breast Cancer 2020, 20, e14–e19. [Google Scholar] [CrossRef] [PubMed]
- Weber, W.P.; Haug, M.; Kurzeder, C.; Bjelic-Radisic, V.; Koller, R.; Reitsamer, R.; Fitzal, F.; Biazus, J.; Brenelli, F.; Urban, C.; et al. Oncoplastic breast consortium consensus conference on nipple-sparing mastectomy. Breast Cancer Res. Treat. 2018, 172, 523–537. [Google Scholar] [CrossRef] [PubMed]
- Lanitis, S.; Kontos, M.; Chortis, P.; Gkanis, V.; Peristeraki, S.; Lainas, S.; Hadjiminas, D.J.M. De-epithelialized skin flaps to minimize complications in large breast reconstruction. Ann. Plast. Surg. 2021, 87, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Kracoff-Sella, S.L.; Allweis, T.M.; Bokov, I.; Kadar-Sfarad, H.; Shifer, Y.; Golzman, E.; Egozi, D. Tumor-to-Nipple Distance in Selecting Patients for Nipple-sparing Mastectomy. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2963. [Google Scholar] [CrossRef] [PubMed]
- Dent, B.L.; Miller, J.A.; Eden, D.J.; Swistel, A.; Talmor, M. Tumor-to-Nipple Distance as a Predictor of Nipple Involvement: Expanding the Inclusion Criteria for Nipple-Sparing Mastectomy. Plast. Reconstr. Surg. 2017, 140, 1e–8e. [Google Scholar] [CrossRef]
- Ashitate, Y.; Lee, B.T.M.; Ngo, L.H.; Laurence, R.G.B.; Hutteman, M.M.; Oketokoun, R.; Lunsford, E.B.; Choi, H.S.; Frangioni, J.V. Quantitative assessment of nipple perfusion with near-infrared fluorescence imaging. Ann. Plast. Surg. 2013, 70, 149–153. [Google Scholar] [CrossRef]
- Cheville, A.L.; Tchou, J.; Barriers, L.S. Exercise and rehabilitation for women with breast cancer: A review of the literature. Breast Cancer Res. Treat. 2016, 159, 1–12. [Google Scholar]
- Tait, R.C.; Zoberi, K.; Ferguson, M.; Levenhagen, K.; Luebbert, R.A.; Rowland, K.; Salsich, G.B.; Herndon, C. Persistent postmastectomy pain: Risk factors and current approaches to treatment. J. Pain 2018, 19, 1367–1383. [Google Scholar] [CrossRef] [PubMed]
- Wilke, L.G.; McCall, L.M.; Posther, K.E.; Whitworth, P.W.; Reintgen, D.S.; Leitch, A.M.; Gabram, S.G.A.; Lucci, A.; Cox, C.E.; Hunt, K.K.; et al. Surgical complications associated with sentinel lymph node biopsy: Results from a prospective international cooperative group trial. Ann. Surg. Oncol. 2006, 13, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Ortega, M.A.; Fraile-Martinez, O.; García-Montero, C.; Callejón-Peláez, E.; Sáez, M.A.; Álvarez-Mon, M.A.; García-Honduvilla, N.; Monserrat, J.; Álvarez-Mon, M.; Bujan, J.; et al. General overview on hyperbaric oxygen therapy: Applications, mechanisms, and translational opportunities. Medicina 2021, 57, 864. [Google Scholar] [CrossRef] [PubMed]
- Glik, J.; Cholewka, A.; Stanek, A.; Sieroń, K.; Mikuś-Zagórska, K.; Knefel, G.; Nowak, M.; Kawecki, M. Thermal imaging and planimetry evaluation of the results of chronic wounds treatment with hyperbaric oxygen therapy. Adv. Clin. Exp. Med. 2019, 28, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Carl, U.M.; Feldmeier, J.J.; Schmitt, G.; Hartmann, K.A. Hyperbaric oxygen therapy for late sequelae in women receiving radiation after breast-conserving surgery. Int. J. Radiat. Oncol. Biol. Phys. 2001, 49, 1029–1031. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Covidence Systematic Review Software. Available online: www.covidence.org (accessed on 2 October 2023).
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomized studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- The American Society of Plastic Surgeons. ASPS Evidence Rating Scales. Available online: https://www.plasticsurgery.org/documents/medical-professionals/health-policy/ASPS_PathwaystoPreventionGuide.pdf (accessed on 20 May 2024).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, T.P. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing the risk of bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Alperovich, M.; Harmaty, M.; Chiu, E.S. Treatment of nipple-sparing mastectomy necrosis with hyperbaric oxygen therapy. Plast. Reconstr. Surg. 2015, 135, 1071e–1072e. [Google Scholar] [CrossRef] [PubMed]
- Lotfi, P.; Dayan, J.; Chiu, E.S.; Mehrara, B.; Nelson, J.A. Hyperbaric oxygen therapy and mastectomy flap ischemia following nipple-sparing mastectomy and immediate breast reconstruction. Plast. Reconstr. Surg. 2020, 145, 1114e–1115e. [Google Scholar] [CrossRef] [PubMed]
- Murphy, B.L.; Boughey, J.C.; Hieken, T.J. Nipple-sparing mastectomy for the management of recurrent breast cancer. Clin. Breast Cancer 2017, 17, e209–e213. [Google Scholar] [CrossRef] [PubMed]
- Nasr, H.Y.; Rifkin, W.J.; Muller, J.N.; Chiu, E.S. Hyperbaric oxygen therapy for threatened nipple-sparing mastectomy flaps: An adjunct for flap salvage. Ann. Plast. Surg. 2023, 90, S125–S129. [Google Scholar] [CrossRef]
- Rajpal, N.; Walters, E.T.; Elmarsafi, T.; Pittman, T.A.; Johnson-Arbor, K.K. Use of hyperbaric oxygen therapy for tissue ischemia after breast reconstruction. Undersea Hyperb. Med. 2019, 46, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Shuck, J.; O’Kelly, N.; Endara, M.; Nahabedian, M.Y. A critical look at the effect of hyperbaric oxygen on the ischemic nipple following nipple-sparing mastectomy and implant-based reconstruction: A case series. Gland. Surg. 2017, 6, 659–665. [Google Scholar] [CrossRef]
- Copeland-Halperin, L.R.; Bruce, S.B.; Mesbahi, A.N. Hyperbaric oxygen therapy following bilateral skin-sparing mastectomies: A case report. Plast. Reconstr. Surg. Glob. Open 2016, 4, e680. [Google Scholar] [CrossRef]
- Fredman, R.; Wiser, I.; Friedman, T.; Heller, L.; Karni, T. Skin-sparing mastectomy flap ischemia salvage using urgent hyperbaric chamber oxygen therapy: A case report. Case Rep. 2014, 41, 145–147. [Google Scholar]
- Hammond, J.B.; Han, G.-R.; Cronin, P.A.; Kosiorek, H.E.; Rebecca, A.M.; Casey, W.J.; Kruger, E.A.; Teven, C.M.; Pockaj, B.A. Exploring the effect of postmastectomy complications on 5-year survival. Am. J. Surg. 2020, 220, 1422–1427. [Google Scholar] [CrossRef]
- Jagsi, R.; Jiang, J.; Momoh, A.O.; Alderman, A.; Giordano, S.H.; Buchholz, T.A.; Pierce, L.J.; Kronowitz, S.J.; Smith, B.D. Complications after mastectomy and immediate breast reconstruction for breast cancer: A claims-based analysis. Ann. Surg. 2016, 263, 219–227. [Google Scholar] [CrossRef]
- Meier, E.L.; Hummelink, S.; Lansdorp, N.; Boonstra, O.; Ulrich, D.J. Perioperative hyperbaric oxygen treatment and postoperative complications following secondary breast reconstruction after radiotherapy: A case-control study of 45 patients. Diving Hyperb. Med. 2021, 51, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Barton, M.B.; West, C.N.; Liu, I.L.A.; Harris, E.L.; Rolnick, S.J.; Elmore, J.G.; Herrinton, L.J.; Greene, S.M.; Nekhlyudov, L.; Fletcher, S.W.; et al. Complications following with bilateral prophylactic mastectomy. J. Natl. Cancer Inst. Monogr. 2005, 2005, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.-S.; Chiu, W.-T.; Hsu, P.-L.; Lin, S.-C.; Peng, I.-C.; Wang, C.-Y.; Tsai, S.-J. Pathophysiological implications of hypoxia in human diseases. J. Biomed. Sci. 2020, 27, 63. [Google Scholar] [CrossRef] [PubMed]
- Leveque, C.; Mrakic Sposta, S.; Theunissen, S.; Germonpré, P.; Lambrechts, K.; Vezzoli, A.; Bosco, G.; Lévénez, M.; Lafère, P.; Guerrero, F.; et al. Oxidative stress response kinetics after 60 min at different (1.4 ATA and 2.5 ATA) hyperbaric hyperoxia exposures. Int. J. Mol. Sci. 2023, 24, 12361. [Google Scholar] [CrossRef] [PubMed]
- Tao, L.; Yuan, X. Efficacy and Safety of hyperbaric oxygen therapy in the management of diabetic foot ulcers: A systematic review and meta-analysis. Int. Wound J. 2023, 21, e14507. [Google Scholar] [CrossRef] [PubMed]
- Buckley, C.J.; Cooper, J.S. Hyperbaric oxygen affects angiogenesis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482485/ (accessed on 9 December 2023).
- Sedlacek, M.; Harlan, N.P.; Buckey, J.C. Renal effects of hyperbaric oxygen therapy in patients with diabetes mellitus: A retrospective study. Int. J. Nephrol. 2021, 2021, 9992352. [Google Scholar] [CrossRef] [PubMed]
- Teguh, D.N.; Raap, R.B.; Struikmans, H.; Verhoef, C.; Koppert, L.B.; Koole, A.; Huang, Y.; van Hulst, R.A. Hyperbaric oxygen therapy for late radiation-induced tissue toxicity: Prospective patient-reported outcome measures in patients with breast cancer. Radiat. Oncol. 2016, 11, 130. [Google Scholar] [CrossRef] [PubMed]
- Plafki, C.; Peters, P.; Almeling, M.; Welslau, W.; Busch, R. Complications and side effects of hyperbaric oxygen therapy. Aviat. Space Environ. Med. 2000, 71, 119–124. [Google Scholar]
- Mermans, J.F.; Tuinder, S.; von Meyenfeldt, M.F.; van der Hulst, R.R.W.J. Hyperbaric oxygen therapy for skin flap necrosis after mastectomy: A case study. Undersea Hyperb. Med. 2012, 39, 719–723. [Google Scholar]
- Spruijt, N.E.; van den Berg, R. Effect of hyperbaric oxygen treatment on late radiation tissue injury after breast cancer: A case series of 67 patients. Diving Hyperb. Med. 2020, 50, 206–213. [Google Scholar] [CrossRef]
- Enomoto, M.; Yagishita, K.; Okuma, K.; Oyaizu, T.; Kojima, Y.; Okubo, A.; Maeda, T.; Miyamoto, S.; Okawa, A. Hyperbaric oxygen therapy for a refractory skin ulcer after radical mastectomy and radiation therapy: A case report. J. Med. Case Rep. 2017, 11, 5. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhang, S.; Yang, Z.; Cheng, Y.; Guo, X.; Liu, C.; Wang, S.; Zhang, L. BRAF L485-P490 deletion mutant metastatic melanoma sensitive to BRAF and MEK inhibition: A case report and literature review. Front. Pharmacol. 2023, 13, 1019217. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Gu, L.; Qin, Z.; Wang, Q.; Ma, J. Efficacy and safety of topical nitroglycerin in the prevention of mastectomy flap necrosis: A systematic review and meta-analysis. Sci. Rep. 2020, 10, 6753. [Google Scholar] [CrossRef] [PubMed]
- DeVito, R.G.; Stranix, J.T. Is nitropaste effective in stressed flaps? Ann. Plast. Surg. 2020, 90, S356–S358. [Google Scholar] [CrossRef] [PubMed]
- Yao, A.; Greige, N.; Ricci, J.A.; Draper, L.B.; Weichman, K.E. Topical nitroglycerin ointment reduces mastectomy flap necrosis in immediate autologous breast reconstruction. Plast. Reconst. Surg. 2023, 152, 728–735. [Google Scholar] [CrossRef]
- Cro, S.; Mehta, S.; Farhadi, J.; Coomber, B.; Cornelius, V. Measuring skin necrosis in a randomised controlled feasibility trial of heat preconditioning on wound healing after reconstructive breast surgery: Study protocol and statistical analysis plan for the preheat trial. Pilot. Feasibility Stud. 2023, 4, 34–39. [Google Scholar] [CrossRef]

| Study ID | Study Design | Sample Size | BMI | Comorbidities (Number of Cases) | Number of Sessions | Days between Surgery and HBOT |
|---|---|---|---|---|---|---|
| Alperovich 2015 [24] | Case report | T = 1 Pre-HBOT (C) = 1 Post-HBOT (E) = 1 | N/A | Healthy, nonsmoking, nondiabetic | 30 | 2 |
| Lotfi 2020 [25] | Observational case series | T = 7 Pre-HBOT (C) = 7 Post-HBOT (E) = 7 | N/A | Not stated | Not stated | Not stated |
| Murphy 2017 [26] | Cohort study | T = 16 No HBOT (C) = 12 HBOT: Pre-Op (E) = 2 HBOT: Post-Op (E) = 2 | N/A | Nonsmoking | Not stated | Not stated |
| Nasr 2023 [27] | Retrospective study | T = 17 Pre-HBOT (C) = 17 Post-HBOT (E) = 17 | N/A | Smoker (1), nonsmoking (16) | 19.4 ± 10.7 | 9.47 ± 12.7 |
| Rajpal 2019 [28] | Retrospective study | T = 8 Pre-HBOT (C) = 8 Post-HBOT (E) = 8 | 25.6 ± 9.7 | Hypertension (2), hyperlipidemia (3), smoker (1), seizures (1) | 10 | 1 |
| Shuck 2017 [29] | Cohort study | T = 13 Non-HBOT (C) = 5 HBOT (E) = 8 | 24.8 | Smokers (2) | Not stated | Not stated |
| Copeland-Halperin 2016 [30] | Case report | T = 1 Pre-HBOT (C) = 1 Post-HBOT (E) = 1 | N/A | Hypothyroidism | 15 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Idris, O.A.; Ahmedfiqi, Y.O.; Shebrain, A.; Al-Assil, T.; Pacione, S.C.; Haj, D.; Motan, A.D.; Momani, F.; Bzizi, H.; Jahromi, B.S.; et al. Hyperbaric Oxygen Therapy for Complications in Nipple-Sparing Mastectomy with Breast Reconstruction: A Systematic Review. J. Clin. Med. 2024, 13, 3535. https://doi.org/10.3390/jcm13123535
Idris OA, Ahmedfiqi YO, Shebrain A, Al-Assil T, Pacione SC, Haj D, Motan AD, Momani F, Bzizi H, Jahromi BS, et al. Hyperbaric Oxygen Therapy for Complications in Nipple-Sparing Mastectomy with Breast Reconstruction: A Systematic Review. Journal of Clinical Medicine. 2024; 13(12):3535. https://doi.org/10.3390/jcm13123535
Chicago/Turabian StyleIdris, Omer A., Yaqub O. Ahmedfiqi, Abdulaziz Shebrain, Talal Al-Assil, Sabrina C. Pacione, Delour Haj, Abdelrahman D. Motan, Faroog Momani, Hanin Bzizi, Bahar Saadaie Jahromi, and et al. 2024. "Hyperbaric Oxygen Therapy for Complications in Nipple-Sparing Mastectomy with Breast Reconstruction: A Systematic Review" Journal of Clinical Medicine 13, no. 12: 3535. https://doi.org/10.3390/jcm13123535
APA StyleIdris, O. A., Ahmedfiqi, Y. O., Shebrain, A., Al-Assil, T., Pacione, S. C., Haj, D., Motan, A. D., Momani, F., Bzizi, H., Jahromi, B. S., Lewis, R. M., & Steeg, K. V., II. (2024). Hyperbaric Oxygen Therapy for Complications in Nipple-Sparing Mastectomy with Breast Reconstruction: A Systematic Review. Journal of Clinical Medicine, 13(12), 3535. https://doi.org/10.3390/jcm13123535







