Perception of Young European Otolaryngologists toward Transoral Robotic Surgery in Head and Neck Oncology and Surgery
Abstract
1. Introduction
2. Methods
2.1. Survey Distribution
2.2. Data Collection
3. Results
3.1. Robot Access
3.2. Benefit, Barrier, and Overall Perception
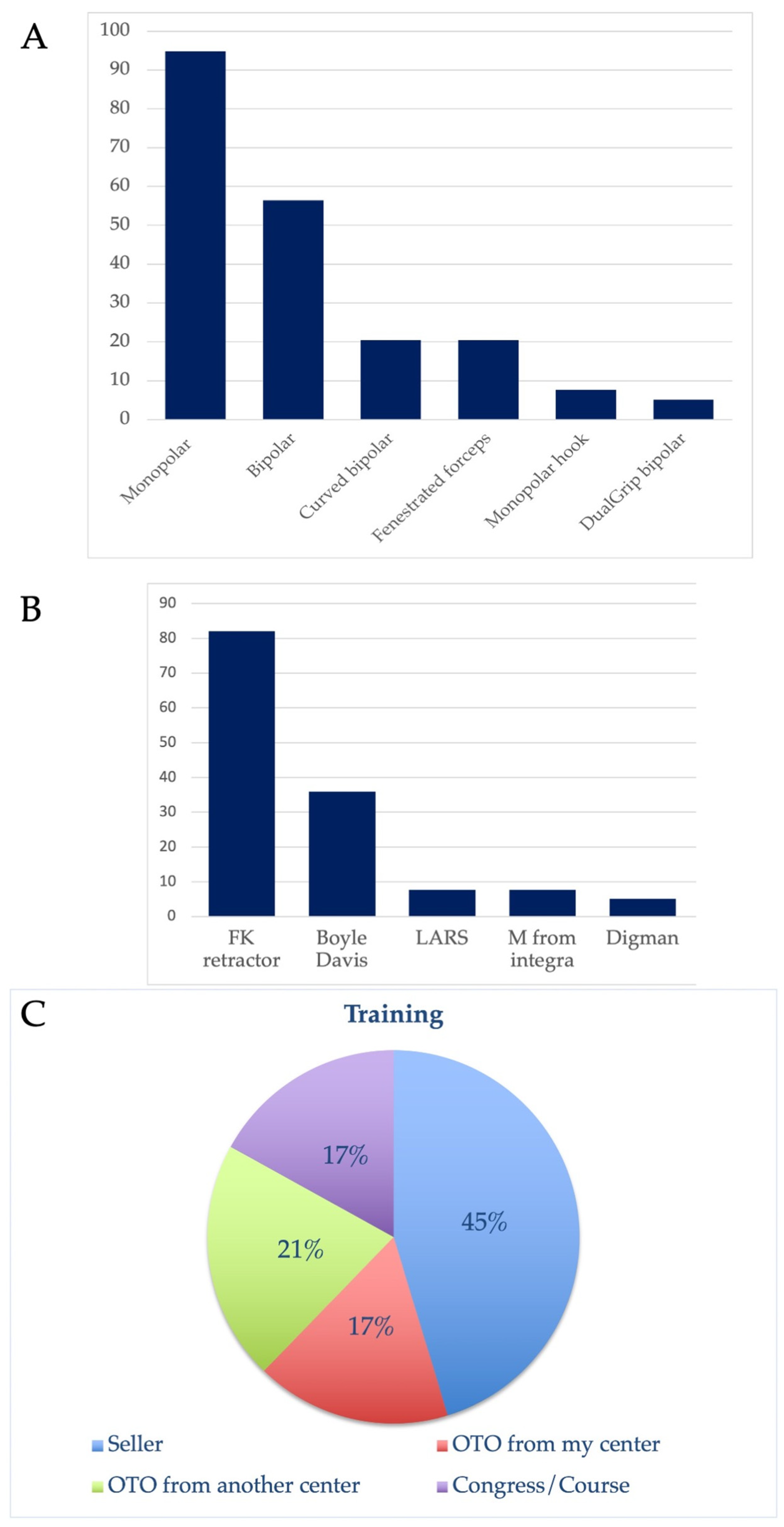
3.3. Training, Instruments, and Setting
3.4. Indications of Robotic Surgery
3.5. Improvements and Perspectives
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Survey
- Country of practice:………………..
- Center of practice:
- Gender: ………………..
- Place of practice: Academic–Private (selection of one or both)
| Laryngology | Head and Neck |
| Pediatric Otolaryngology | Rhinology |
| Otology | Residency |
- 5.
- Do you have any experience with TORS? yes–no (never)
- 6.
- Number of years of practice after the end of the residency.
- 7.
- Number of procedures performed yearly.
- -
- … cases
- 8.
- About my opinion/awareness about TORS:
- -
- I never used TORS but I am interested to use it.
- -
- There are many benefits to TORS.
- -
- There are more disadvantages to TORS than advantages.
- -
- I trust TORS for the future.
- -
- I advocate TORS to my colleagues.
- -
- I encourage my colleagues to adopt TORS.
- -
- TORS has affected me positively since adoption.
- -
- TORS has affected me negatively since adoption.
- -
- The adoption of TORS by my colleagues has affected me positively.
- -
- The lack of adoption of TORS by my colleagues has affected me negatively.
- -
- I believe that TORS is the future of minimal invasive surgeries in otolaryngology—head neck surgery.
- 9.
- About the barriers to use TORS:
- -
- Robot availability and cost
- -
- Cost related to TORS in my healthcare system
- -
- Time restraint
- -
- Low volumes of procedures performed at my center
- -
- Low theoretical volumes of procedures performed with TORS
- -
- Lack of personal training
- -
- Lack of interest
- -
- Long setting/docking time
- -
- Difficulty of surgical field exposure
- 10.
- What are the presumed benefits of TORS according to you?
- -
- Esthetic benefit (scar)
- -
- Avoid tracheotomy in some selected cases
- -
- Shorter hospital stay
- -
- Better patient postoperative quality of life
- -
- Better view of the operative field
- -
- Better movements of the robot arm in the operative field
- -
- Others:
- 11.
- According to your opinion, in which condition TORS may be adequate? Score between 0 (not indicated) to 5 (perfect indication).
- -
- Oropharyngeal cancer cT1-T2
- -
- Oropharyngeal cancer cT3
- -
- Oropharyngeal cancer cT4a
- -
- Base of tongue resection (sleep apnea syndrome)
- -
- Tongue base mucosectomy (unknown primary tumor)
- -
- Supraglottic laryngeal cancer cT1-T2
- -
- Supraglottic laryngeal cancer cT3
- -
- Supraglottic laryngeal cancer cT4a
- -
- Total laryngectomy
- -
- Vocal cord cancer cT1-T2
- -
- Hypopharyngeal cancer cT1-T2
- -
- Hypopharyngeal cancer cT3
- -
- Hypopharyngeal cancer cT4a
- -
- Nasopharyngeal cancer (cT1-T2-T3)
- -
- Neck dissection
- -
- Hemi-thyroid surgery (limited lesion)
- -
- Total thyroidectomy (limited lesion)
- -
- Branchial cyst
- -
- Pharyngeal flap
- 12.
- About my access to TORS:
- -
- I have no access to TORS, and I am not interested to TORS.
- -
- I have no access to TORS, but I would like to have access.
- -
- I have adequate access to TORS, but I did not use it.
- -
- I have adequate access to TORS, and I use it.
- -
- TORS cases are cost-prohibitive.
- 13.
- Are you ready to refer your patient to a center with a robot for indications where TORS may be performed? (if you have a robot in your center and if you use it, SKIP this question)
- -
- Yes
- -
- No opinion
- -
- No, I prefer to perform the surgery myself (open or endoscopic surgery).
- -
- No
- 14.
- FOR A SURGEON WHO USES TORS, about the training:
- -
- I received adequate training for TORS.
- -
- I received good support from my management.
- -
- My organization (hospital) encourages me to perform TORS.
- -
- My organization does not encourage me to perform TORS.
- 15.
- FOR A SURGEON WHO USES TORS, my training was organized by:
- -
- Training program by seller
- -
- Senior otolaryngologists from my department
- -
- Senior otolaryngologists from another department
- -
- University course/congress
- 16.
- FOR A SURGEON WHO USES TORS, what are the instruments that you use? (skip if you do not use robotic surgery)
- -
- Monopolar spatula
- -
- Maryland bipolar forceps
- -
- Monopolar hook
- -
- Curved bipolar (dissector)
- -
- Fenestrated bipolar forceps
- -
- Bipolar with dual grip
- -
- Other: ….
- 17.
- FOR A SURGEON WHO USES TORS, what are the retraction materials that you use to open the mouth?
- -
- FK retractor
- -
- Boyle Davis retractor
- -
- LARS
- -
- Digman
- -
- Other: ….
- 18.
- What are the improvements that seem important for the future model of the robots?
- -
- Better access to oropharynx
- -
- Better access to supraglottis larynx
- -
- Better access to glottis
- -
- Better access to hypopharynx
- -
- Better access to nasal fossea
- -
- Better access to nasopharynx
- -
- Integration of GPS based on MRI imaging
- -
- Integration of CO2 or another laser
- -
- Integration of narrow-banded imaging system
- -
- Better back strength
- -
- Flexible instruments
- -
- Other: …………………..
Appendix B. Perceptions, Barriers, and Benefits of TORS among TORS and Non-TORS Head and Neck Surgeons
| Overall Opinion | TORS (39) | Non-TORS (28) | p-Value |
| TORS is associated with many surgical and hospital stay benefits | 29 (74) | 18 (64) | NS |
| There are more disadvantages to TORS than advantages | 1 (3) | 4 (14) | NS |
| I trust TORS for the future | 23 (59) | 12 (43) | NS |
| I advocate TORS to my colleagues | 13 (33) | 2 (7) | 0.011 |
| I encourage colleagues to use TORS in the future | 19 (49) | 5 (18) | 0.009 |
| TORS is important for the future of minimal invasive surgeries | 27 (69) | 9 (32) | 0.003 |
| Main barriers of TORS | |||
| Robot availability | 29 (74) | 17 (61) | NS |
| Cost related to TORS in my healthcare system | 22 (56) | 20 (71) | NS |
| Time restraint | 6 (15) | 7 (25) | NS |
| Low volumes of procedures performed at my center | 9 (23) | 7 (25) | NS |
| Low theoretical volumes of procedures performed with TORS | 17 (44) | 10 (36) | NS |
| Lack of personal training | 7 (18) | 12 (43) | 0.026 |
| Lack of interest | 1 (3) | 3 (11) | NS |
| Docking time (setting the robot) | 2 (5) | 6 (21) | 0.042 |
| Difficulty of exposure of the surgical field | 13 (33) | 6 (21) | NS |
| Main benefits | |||
| 1. Esthetic benefit (scar) | 18 (46) | 13 (46) | NS |
| 2. Avoid tracheotomy in some selected cases | 26 (67) | 14 (50) | NS |
| 3. Shorter hospital stay | 27 (69) | 15 (54) | NS |
| 4. Better patient postoperative quality of life | 27 (69) | 16 (57) | NS |
| 5. Better view of the operative field | 29 (74) | 23 (82) | NS |
| 6. Better movements of the robot arm in the operative field | 24 (62) | 17 (61) | NS |
| The results are reported as the number of responders (%). Abbreviations: NS = non-significant; TORS = transoral robotic surgery. | |||
References
- Lörincz, B.B.; Jowett, N.; Knecht, R. Decision management in transoral robotic surgery: Indications, individual patient selection, and role in the multidisciplinary treatment for head and neck cancer from a European perspective. Head Neck 2016, 38 (Suppl. S1), E2190–E2196. [Google Scholar] [CrossRef] [PubMed]
- Sejima, T.; Morizane, S.; Fujiwara, K.; Ashida, K.; Saito, H.; Taniguchi, Y.; Nakamura, H.; Takenaka, A. The First Pilot Comprehensive Evaluation of the Outcomes of Different Types of Robotic Surgeries in the Different Surgical Departments: The Penta, Tetra and Trifecta Achievements in Robotic Surgeries. Yonago Acta Med. 2016, 59, 135–142. [Google Scholar] [PubMed]
- Caporale, C.D.; Chiari, F.; D’Alessio, P.; Barbara, F.; Guarino, P. Transoral robotic surgery for supraglottic cancer. A review of oncological and functional outcomes compared to open surgery. Acta Otorhinolaryngol. Ital. 2024, 44 (Suppl. S1), S20–S27. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Haddad, L.; Holsinger, F.C.; Mendelsohn, A.H.; Hans, S. Awareness, Perception and Adoption of Otolaryngologist-Head Neck Surgeons toward Transoral Robotic Surgery: An International Survey. Oral Oncol. 2023, 8, 95–102. [Google Scholar]
- Chillakuru, Y.; Benito, D.A.; Strum, D.; Mehta, V.; Saini, P.; Shim, T.; Darwish, C.; Joshi, A.S.; Thakkar, P.; Goodman, J.F. Transoral robotic surgery versus nonrobotic resection of oropharyngealsquamous cell carcinoma. Head Neck 2021, 43, 2259–2273. [Google Scholar] [CrossRef] [PubMed]
- Orosco, R.K.; Tam, K.; Nakayama, M.; Holsinger, F.C.; Spriano, G. Transoral supraglottic laryngectomy using a next-generation single-port robotic surgical system. Head Neck 2019, 41, 2143–2147. [Google Scholar] [CrossRef]
- Tae, K.; Song, C.M.; Ji, Y.B.; Sung, E.S.; Jeong, J.H.; Kim, D.S. Oncologic outcomes of robotic thyroidectomy: 5-year experience with propensity score matching. Surg. Endosc. 2016, 30, 4785–4792. [Google Scholar] [CrossRef] [PubMed]
- O’Malley, B.W., Jr.; Weinstein, G.S.; Snyder, W.; Hockstein, N.G. Transoral robotic surgery (TORS) for base of tongue neoplasms. Laryngoscope 2006, 116, 1465–1472. [Google Scholar] [CrossRef] [PubMed]
- Mandapathil, M.; Meyer, J.E. Acceptance and adoption of transoral robotic surgery in Germany. Eur. Arch. Otorhinolaryngol. 2021, 278, 4021–4026. [Google Scholar] [CrossRef]
- Arshad, H.; Durmus, K.; Ozer, E. Transoral robotic resection of selected parapharyngeal space tumors. Eur. Arch. Otorhinolaryngol. 2013, 270, 1737–1740. [Google Scholar] [CrossRef]
- Chauvet, D.; Missistrano, A.; Hivelin, M.; Carpentier, A.; Cornu, P.; Hans, S. Transoral robotic-assisted skull base surgery to approach the sella turcica: Cadaveric study. Neurosurg. Rev. 2014, 37, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.Y.K.; Holsinger, F.C.; Liu, S.; Sorger, J.M.; Azizian, M.; Tsang, R.K.Y. Augmented reality for image guidance in transoral robotic surgery. J. Robot. Surg. 2020, 14, 579–583. [Google Scholar] [CrossRef] [PubMed]
- Virós Porcuna, D.; Pardo Muñoz, L.; Viña Soria, C.; Nicastro, V.; Palau Viarnès, M.; Pollán Guisasola, C. A retrospective analysis of surgery in prestyloid parapharyngeal tumors: Lateral approaches vs transoral robotic surgery. Laryngoscope Investig. Otolaryngol. 2021, 6, 1062–1067. [Google Scholar] [CrossRef]
- Hammoudi, K.; Pinlong, E.; Kim, S.; Bakhos, D.; Morinière, S. Transoral robotic surgery versus conventional surgery in treatment for squamous cell carcinoma of the upper aerodigestive tract. Head Neck 2015, 37, 1304–1309. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, G.; Mintz, J.; Foreman, A.; Hodge, J.C.; Krishnan, S. The acceptance and adoption of transoral robotic surgery in Australia and New Zealand. J. Robot. Surg. 2019, 13, 301–307. [Google Scholar] [CrossRef]
- Mirza, F.A.; Johnson, C.Z.; Byrd, J.K.; Albergotti, W.G., 3rd. Treatment trends for advanced oropharyngeal squamous cell carcinoma in the era of human papillomavirus. Head Neck 2021, 43, 3476–3492. [Google Scholar] [CrossRef]
- Lechien, J.R.; Chiesa-Estomba, C.M.; Fakhry, N.; Saussez, S.; Badr, I.; Ayad, T.; Chekkoury-Idrissi, Y.; Melkane, A.E.; Bahgat, A.; Crevier-Buchman, L.; et al. Surgical, clinical, and functional outcomes of transoral robotic surgery used in sleep surgery for obstructive sleep apnea syndrome: A systematic review and meta-analysis. Head Neck 2021, 43, 2216–2239. [Google Scholar] [CrossRef]
- Alzahrani, F.; Sahovaler, A.; Mundi, N.; Rammal, A.; Fnais, N.; MacNeil, S.D.; Mendez, A.; Yoo, J.; Fung, K.; Laxague, F.; et al. Transoral robotic surgery for the identification of unknown primary head and neck squamous cell carcinomas: Its effect on the wait and the weight. Head Neck 2022, 44, 1206–1212. [Google Scholar] [CrossRef]
- Hans, S.; Chekkoury-Idrissi, Y.; Circiu, M.P.; Distinguin, L.; Crevier-Buchman, L.; Lechien, J.R. Surgical, Oncological, and Functional Outcomes of Transoral RoboticSupraglottic Laryngectomy. Laryngoscope 2021, 131, 1060–1065. [Google Scholar] [CrossRef]
- Patel, K.B.; Lin, C.; Kramer, S.; Fada, C.; Ozer, E. Transoral robotic excision of laryngocele: Surgical considerations. Head Neck 2019, 41, 1140–1143. [Google Scholar] [CrossRef] [PubMed]
- Tsang, R.K.; Chan, W.C.P.; Holsinger, F.C.; Chung, J.C.K.; Chow, V.L.Y.; Chan, J.Y.W.; Ho, W.K.; Wei, W.I. Long-term results of robotic-assisted nasopharyngectomy for recurrent nasopharyngeal carcinoma. Head Neck 2022, 44, 1940–1947. [Google Scholar] [CrossRef] [PubMed]
- Simon, C.; Beharry, A.; Paleri, V.; Dübi, P.; Lambercy, K.; Holsinger, F.C.; Todic, J. The robotic-assisted extended “Sistrunk” approach for tumors of the upper aerodigestive tract with limited transoral access: First description of oncological and functional outcomes. Head Neck 2022, 44, 2335–2341. [Google Scholar] [CrossRef] [PubMed]
- Lira, R.B.; De Cicco, R.; Rangel, L.G.; Bertelli, A.A.; Duque Silva, G.; de Medeiros Vanderlei, J.P.; Kowalski, L.P. Transoral endoscopic thyroidectomy vestibular approach: Experience from a multicenter national group with 412 patients. Head Neck 2021, 43, 3468–3475. [Google Scholar] [CrossRef] [PubMed]
- Park, D.; Kim, H.Y.; Kim, H.K.; You, J.Y.; Dionigi, G.; Russell, J.O.; Tufano, R.P. Institutional experience of 200 consecutive papillary thyroid carcinoma patients in transoral robotic thyroidectomy surgeries. Head Neck 2020, 42, 2106–2114. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.M.; Roman, S.A.; Kraus, D.H.; Sosa, J.A.; Judson, B.L. Transoral robotic surgery: A population-level analysis. Otolaryngol. Head Neck Surg 2014, 150, 968–975. [Google Scholar] [CrossRef]
- Sobel, R.H.; Blanco, R.; Ha, P.K.; Califano, J.A.; Kumar, R.; Richmon, J.D. Implementation of a comprehensive competency-based transoral roboticsurgery training curriculum with ex vivo dissection models. Head Neck 2016, 38, 1553–1563. [Google Scholar] [CrossRef]
| Participants | Head and Neck Surgeons | Non-Head and Neck Surgeons | ||
|---|---|---|---|---|
| Outcomes | N = 120 | N = 67 | N = 53 | p-Value |
| Gender (F/M) | 40/80 | 13/54 | 27/26 | 0.001 |
| Years of experience (years) | 11.6 ± 11.5 | 14.0 ± 13.4 | 8.5 ± 7.9 | 0.018 |
| Main subspecialties | ||||
| General otolaryngology | 13 (11) | - | 13 (24) | - |
| Head and neck | 67 (56) | 67 | - | |
| Laryngology | 2 (2) | - | 2 (4) | |
| Rhinology | 6 (5) | - | 6 (11) | |
| Otology | 8 (7) | - | 8 (15) | |
| Pediatrics | 10 (8) | - | 10 (19) | |
| Residency | 14 (11) | - | 14 (26) | |
| Places of practice | ||||
| Academic/university | 89 (74) | 50 (75) | 39 (74) | NS |
| Private | 8 (7) | 3 (4) | 5 (9) | |
| Academic and private | 23 (19) | 14 (21) | 9 (17) |
| Non-Head and Neck Surgeons (N = 53) | Head and Neck Surgeons (N = 67) | |||
|---|---|---|---|---|
| Access Outcomes | TORS (N = 39) | Non-TORS (N = 28) | p-Value | |
| No/limited access and not interested | 9 (17) | 0 (0) | 2 (7) | 0.001 |
| No/limited access but interested | 33 (62) | 7 (18) | 17 (61) | 0.001 |
| Adequate access but I do not use TORS | 11 (21) | 0 (0) | 8 (29) | 0.001 |
| Adequate access but cost-prohibitive | 0 (0) | 2 (5) | 1 (3) | 0.001 |
| Adequate access and I use it | 0 (0) | 30 (77) | 0 (0) | 0.001 |
| Overall Opinion | Non-Head and Neck Surgeons (53) | Head and Neck Surgeons (67) | p-Value |
|---|---|---|---|
| TORS is associated with many surgical and hospital stay benefits | 28 (43) | 47 (70) | 0.040 |
| There are more disadvantages to TORS than advantages | 2 (4) | 5 (8) | NS |
| I trust in TORS for the future | 23 (43) | 35 (52) | NS |
| I advocate TORS to my colleagues | 5 (9) | 15 (22) | 0.048 |
| I encourage colleagues to use TORS in the future | 9 (17) | 24 (36) | 0.022 |
| TORS has affected me positively since adoption | 3 (6) | 19 (28) | 0.001 |
| TORS is important for the future of minimal invasive surgeries | 23 (43) | 36 (54) | NS |
| Main barriers of TORS | |||
| Robot availability | 41 (77) | 46 (69) | NS |
| Cost related to TORS in my healthcare system | 41 (77) | 42 (63) | NS |
| Time restraint | 14 (26) | 13 (19) | NS |
| Low volumes of procedures performed at my center | 16 (30) | 16 (24) | NS |
| Low theoretical volumes of procedures performed with TORS | 14 (26) | 27 (40) | NS |
| Lack of personal training | 25 (47) | 19 (28) | 0.034 |
| Lack of interest | 8 (15) | 4 (6) | NS |
| Docking time (setting the robot) | 9 (17) | 8 (12) | NS |
| Difficulty of exposure of the surgical field | 9 (17) | 19 (28) | NS |
| Main benefits | |||
| 1. Esthetic benefit (scar) | 25 (47) | 31 (46) | NS |
| 2. Avoid tracheotomy in some selected cases | 28 (53) | 40 (60) | NS |
| 3. Shorter hospital stay | 32 (60) | 42 (63) | NS |
| 4. Better patient postoperative quality of life than in the conventional approach | 30 (57) | 43 (64) | NS |
| 5. Better view of the operative field than in the conventional approach | 25 (47) | 52 (78) | 0.001 |
| 6. Better movements of the robot arm in the operative field than in the conventional approach | 25 (47) | 41 (61) | NS |
| TORS Surgeons | Non-TORS Surgeons | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Indications | 0 | 1 | 2 | 3 | 4 | 0 | 1 | 2 | 3 | 4 | p-Value |
| Oropharynx | |||||||||||
| cT1-T2 oropharyngeal cancer | 0 | 0 | 0 | 23.1 | 76.9 | 3.6 | 3.6 | 3.6 | 50.0 | 39.2 | 0.022 |
| cT3 oropharyngeal cancer | 0 | 17.9 | 38.5 | 35.9 | 7.7 | 3.8 | 26.9 | 30.8 | 30.8 | 7.7 | NS |
| cT4a oropharyngeal cancer | 42.1 | 39.5 | 5.3 | 13.2 | 0 | 48.1 | 25.9 | 22.2 | 3.7 | 0 | NS |
| Base of tongue | |||||||||||
| Sleep apnea syndrome | 0 | 17.9 | 30.8 | 51.3 | 0 | 0 | 7.4 | 33.3 | 59.3 | 0 | NS |
| Unknown primary cancer | 2.6 | 7.7 | 20.5 | 30.8 | 38.5 | 0 | 3.6 | 10.7 | 35.7 | 50 | NS |
| Larynx | |||||||||||
| cT1-T2 supraglottic cancer | 0 | 2.6 | 5.1 | 28.2 | 64.1 | 0 | 10.7 | 7.1 | 50.0 | 32.1 | NS |
| cT3 supraglottic cancer | 5.1 | 33.3 | 30.8 | 30.8 | 0 | 11.1 | 37.0 | 18.5 | 22.2 | 11.1 | NS |
| cT4a supraglottic cancer | 51.3 | 38.5 | 10.3 | 0 | 0 | 42.3 | 30.8 | 19.2 | 7.7 | 0 | NS |
| Total laryngectomy | 25.6 | 30.8 | 30.8 | 10.3 | 2.6 | 55.6 | 22.2 | 14.8 | 7.4 | 0 | NS |
| cT1-T2 vocal fold cancer | 0 | 2.6 | 20.5 | 43.6 | 33.3 | 3.6 | 3.6 | 25.0 | 57.1 | 10.7 | NS |
| Hypopharynx | |||||||||||
| cT1-T2 hypopharyngeal cancer | 10.3 | 61.5 | 23.1 | 5.1 | 0 | 22.2 | 51.9 | 11.1 | 11.1 | 3.7 | NS |
| cT3 hypopharyngeal cancer | 60.5 | 36.8 | 2.6 | 0 | 0 | 55.6 | 25.9 | 18.5 | 0 | 0 | NS |
| cT4a hypopharyngeal cancer | 28.2 | 35.9 | 28.2 | 7.7 | 0 | 37.0 | 29.6 | 22.2 | 7.4 | 3.7 | NS |
| Others | |||||||||||
| Nasopharyngeal cancer | 20.5 | 30.8 | 30.8 | 15.4 | 2.6 | 19.2 | 19.2 | 46.2 | 11.5 | 3.8 | NS |
| Neck dissection | 10.3 | 43.6 | 30.8 | 15.4 | 0 | 14.8 | 55.6 | 18.5 | 11.1 | 0 | NS |
| Partial thyroidectomy (lobectomy) | 12.8 | 12.8 | 41.0 | 23.1 | 10.3 | 11.1 | 40.7 | 14.8 | 29.6 | 3.7 | 0.41 |
| Total thyroidectomy | 15.4 | 17.9 | 35.9 | 28.2 | 2.6 | 19.2 | 38.5 | 11.5 | 26.9 | 3.8 | NS |
| Branchial cyst | 10.3 | 30.8 | 41.0 | 15.4 | 2.6 | 22.2 | 40.7 | 18.5 | 14.8 | 3.7 | NS |
| Pharyngeal flap | 5.1 | 15.4 | 41.0 | 30.8 | 7.7 | 11.1 | 22.2 | 40.7 | 25.9 | 0 | NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lechien, J.R.; Hamdan, A.-L.; Fakhry, N.; Vaira, L.A.; Iannella, G.; Gengler, I.M.; Michel, J.; Radulesco, T.; Remacle, M.; Hans, S.; et al. Perception of Young European Otolaryngologists toward Transoral Robotic Surgery in Head and Neck Oncology and Surgery. J. Clin. Med. 2024, 13, 3055. https://doi.org/10.3390/jcm13113055
Lechien JR, Hamdan A-L, Fakhry N, Vaira LA, Iannella G, Gengler IM, Michel J, Radulesco T, Remacle M, Hans S, et al. Perception of Young European Otolaryngologists toward Transoral Robotic Surgery in Head and Neck Oncology and Surgery. Journal of Clinical Medicine. 2024; 13(11):3055. https://doi.org/10.3390/jcm13113055
Chicago/Turabian StyleLechien, Jerome R., Abdul-Latif Hamdan, Nicolas Fakhry, Luigi A. Vaira, Giannicola Iannella, Isabelle M. Gengler, Justin Michel, Thomas Radulesco, Marc Remacle, Stephane Hans, and et al. 2024. "Perception of Young European Otolaryngologists toward Transoral Robotic Surgery in Head and Neck Oncology and Surgery" Journal of Clinical Medicine 13, no. 11: 3055. https://doi.org/10.3390/jcm13113055
APA StyleLechien, J. R., Hamdan, A.-L., Fakhry, N., Vaira, L. A., Iannella, G., Gengler, I. M., Michel, J., Radulesco, T., Remacle, M., Hans, S., Cammaroto, G., Saibene, A. M., Mayo-Yanez, M., & Maniaci, A. (2024). Perception of Young European Otolaryngologists toward Transoral Robotic Surgery in Head and Neck Oncology and Surgery. Journal of Clinical Medicine, 13(11), 3055. https://doi.org/10.3390/jcm13113055










