The Silent Threat of Hypokalemia after High Voltage Electrical Injuries: A Case Study and Review of the Literature
Abstract
1. Introduction
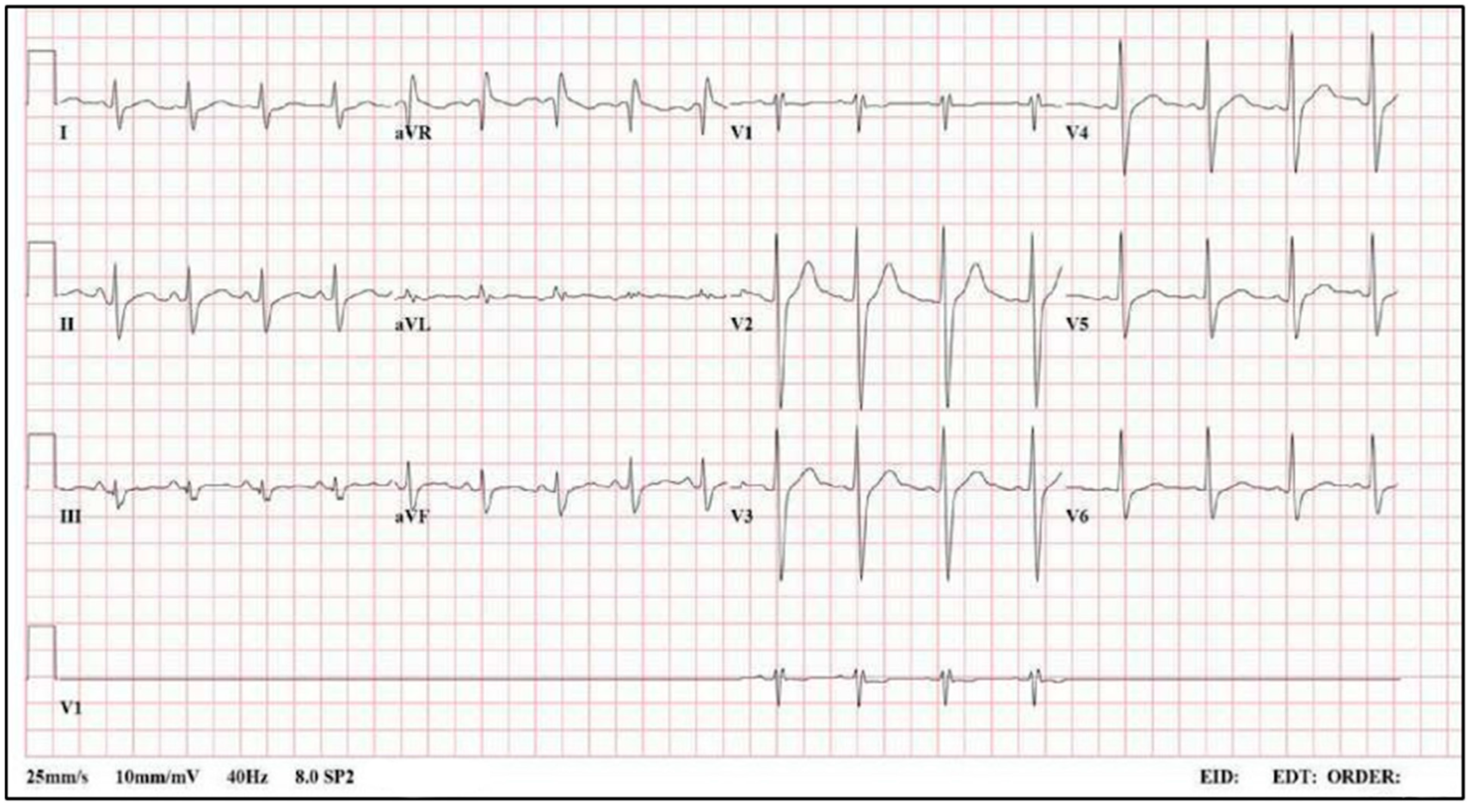
2. Case Report
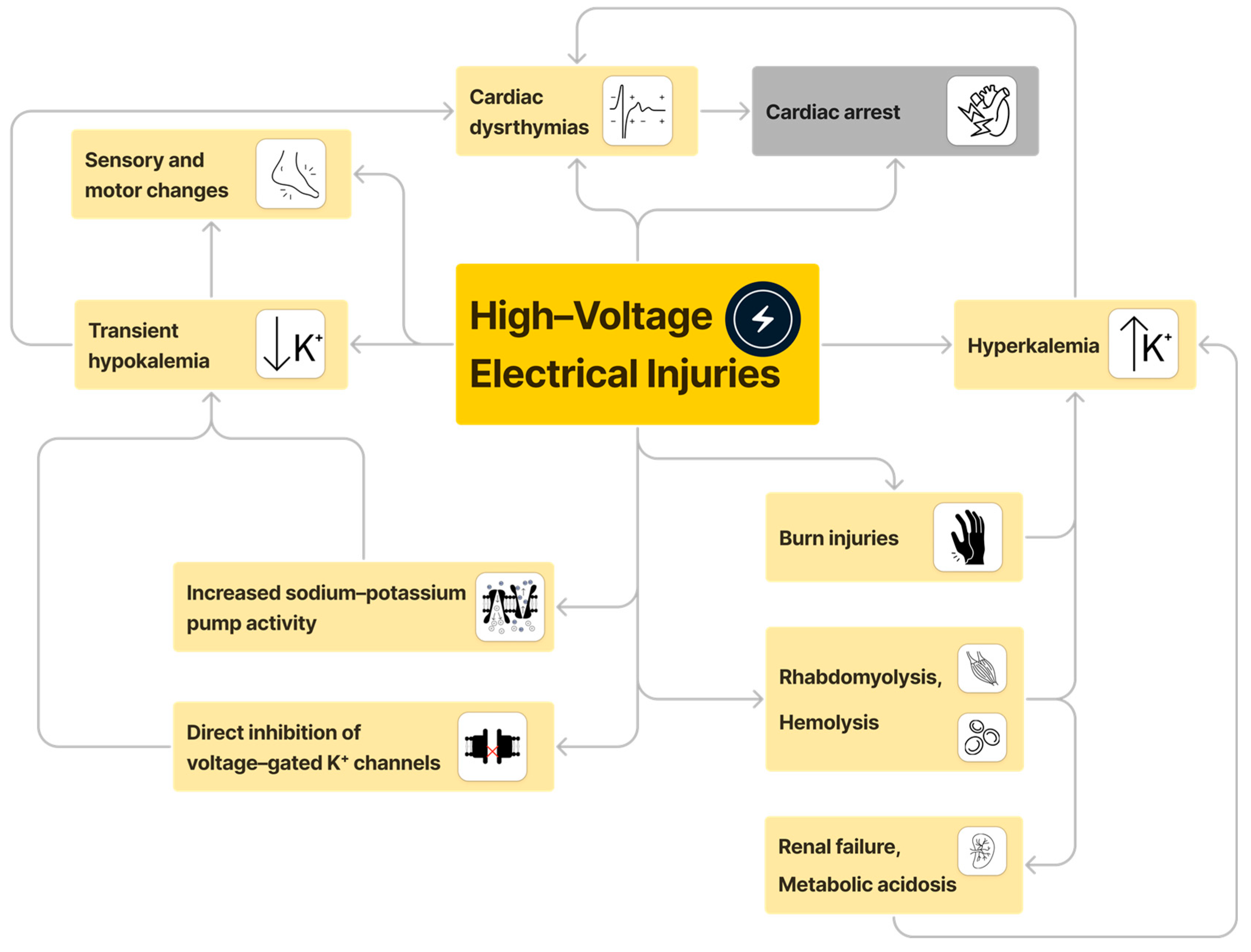
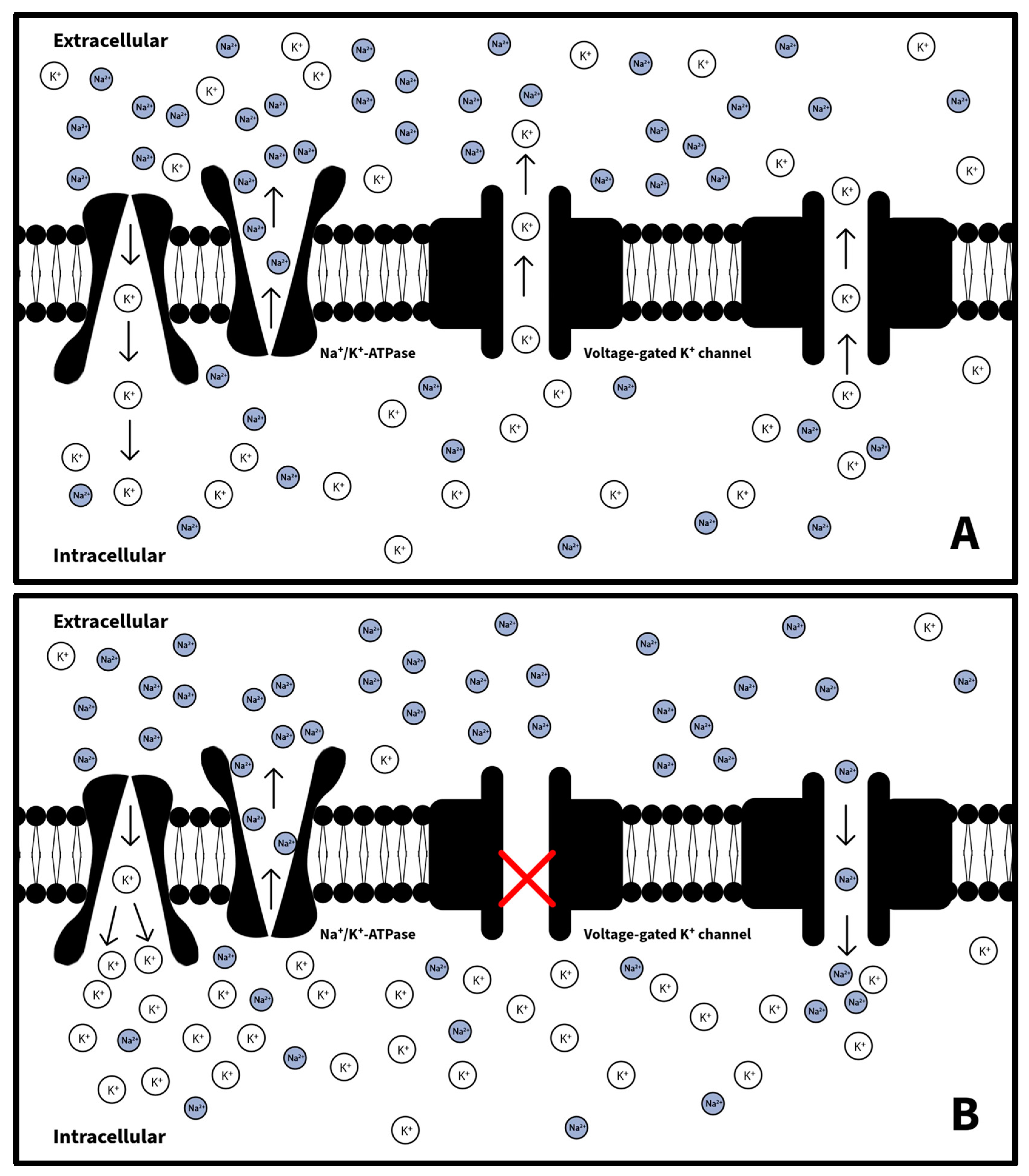
3. Review of the Literature
4. Discussion
5. Limitations and Directions for Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zemaitis, M.R.; Foris, L.A.; Lopez, R.A.; Huecker, M.R. Electrical Injuries. In StatPearls, Treasure Island; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: http://www.ncbi.nlm.nih.gov/books/NBK448087/ (accessed on 29 March 2024).
- Rotariu, E.L.; Manole, M.D. Cardiac Arrest Secondary to Lightning Strike: Case Report and Review of the Literature. Pediatr. Emerg. Care 2017, 36, e18–e20. [Google Scholar] [CrossRef] [PubMed]
- Ritenour, A.E.; Morton, M.J.; McManus, J.G.; Barillo, D.J.; Cancio, L.C. Lightning injury: A review. Burns J. Int. Soc. Burn Inj. 2008, 34, 585–594. [Google Scholar] [CrossRef]
- van Ruler, R.; Eikendal, T.; Kooij, F.O.; Tan, E.C. A shocking injury: A clinical review of lightning injuries high-lighting pitfalls and a treatment protocol. Injury 2022, 53, 3070–3077. [Google Scholar] [CrossRef]
- Lightning. Available online: https://www.public.asu.edu/~gbadams/lightning/lightning.html (accessed on 16 November 2023).
- Hyperkalemia in Electrical Burns: A Retrospective Study in Colombia-PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/29395406/ (accessed on 29 March 2024).
- Iqbal, S.B.; Rao, S.J.; Pyrgos, G.J.; Haas, C.J.; Padmanabhan, S. Acute inferior ST-elevation myocardial infarction mimicked by direct lightning strike: A case report. Eur. Heart J. Case Rep. 2023, 7, ytad578. [Google Scholar] [CrossRef]
- Palmer, B.F.; Clegg, D.J. Diagnosis and treatment of hyperkalemia. Clevel. Clin. J. Med. 2017, 84, 934–942. [Google Scholar] [CrossRef]
- Giudicessi, J.R.; Noseworthy, P.A.; Ackerman, M.J. The QT Interval. Circulation 2019, 139, 2711–2713. [Google Scholar] [CrossRef] [PubMed]
- Bird, R.; Naji, S.; Vowles, B.; Shaw, A.; Martin, N. Hypokalaemia with flaccid paralysis following high-voltage electrical injury in an adolescent patient. Trauma 2019, 21, 317–320. [Google Scholar] [CrossRef]
- Dasgupta, R.; Schulz, J.; Lee, R.; Ryan, C. Severe hypokalemia as a cause of acute transient paraplegia following electrical shock. Burns J. Int. Soc. Burn Inj. 2002, 28, 609–611. [Google Scholar] [CrossRef]
- Phuyal, P.; Nagalli, S. Hypokalemic Periodic Paralysis. In StatPearls, Treasure Island; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK559178/ (accessed on 17 November 2023).
- Grosson, C.L.; Esteban, J.; McKenna-Yasek, D.; Gusella, J.F.; Brown, R.H. Hypokalemic periodic paralysis mutations: Confirmation of mutation and analysis of founder effect. Disord 1996, 6, 27–31. [Google Scholar] [CrossRef]
- Blum, H.; Nioka, S.; Johnson, R.G. Activation of the Na+, K(+)-ATPase in Narcine brasiliensis. Proc. Natl. Acad. Sci. USA 1990, 87, 1247–1251. [Google Scholar] [CrossRef]
- Brumback, R.A.; Feeback, D.L.; Leech, R.W. Rhabdomyolysis following electrical injury. Semin. Neurol. 1995, 15, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Arnoldo, B.D.; Purdue, G.F.; Kowalske, K.; Helm, P.A.; Burris, A.; Hunt, J.L. Electrical injuries: A 20-year review. J. Burn. Care Rehabil. 2004, 25, 479–484. [Google Scholar] [CrossRef]
- Halperin, M.L.; Kamel, K.S. Potassium. Lancet 1998, 352, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Sardar, Z.; Waheed, K.A.F.; Javed, M.A.; Akhtar, F.; Bokhari, S.R.A. Clinical and Etiological Spectrum of Hypokalemic Periodic Paralysis in a Tertiary Care Hospital in Pakistan. Cureus 2019, 11, e3921. [Google Scholar] [CrossRef]
- Lu, Y.-T.; Lan, M.-Y.; Liu, J.-S.; Chen, W.-H. An unusual presentation of hypokalemic paralysis with evolving pure motor hemiparesis. J. Clin. Neurosci. 2011, 18, 716–719. [Google Scholar] [CrossRef]
- Bailey, B.; Gaudreault, P.; Thivierge, R.L. Neurologic and neuropsychological symptoms during the first year after an electric shock: Results of a prospective multicenter study. Am. J. Emerg. Med. 2008, 26, 413–418. [Google Scholar] [CrossRef]
- Duff, K.; McCaffrey, R.J. Electrical injury and lightning injury: A review of their mechanisms and neuropsychological, psychiatric, and neurological sequelae. Neuropsychol. Rev. 2001, 11, 101–116. [Google Scholar] [CrossRef] [PubMed]
- Poole-Wilson, P.A. Potassium and the heart. Clin. Endocrinol. Metab. 1984, 13, 249–268. [Google Scholar] [CrossRef] [PubMed]
- Kyaw, M.T.; Maung, Z.M. Hypokalemia-Induced Arrhythmia: A Case Series and Literature Review. Cureus 2022, 14, e22940. [Google Scholar] [CrossRef]
- Viera, A.J.; Wouk, N. Potassium Disorders: Hypokalemia and Hyperkalemia. Am. Fam. Physician 2015, 92, 487–495. [Google Scholar]
- Frenkel, A.; Hassan, L.; Segal, A.; Israeli, A.; Binyamin, Y.; Zlotnik, A.; Novack, V.; Klein, M. Estimation of Potassium Changes Following Potassium Supplements in Hypokalemic Critically Ill Adult Patients-A Patient Personalized Practical Treatment Formula. J. Clin. Med. 2021, 10, 1986. [Google Scholar] [CrossRef]
- Adrogué, H.J.; Madias, N.E. The impact of sodium and potassium on hypertension risk. Semin. Nephrol. 2014, 34, 257–272. [Google Scholar] [CrossRef]
- Molina, P.E. Neurobiology of the stress response: Contribution of the sympathetic nervous system to the neuroimmune axis in traumatic injury. Shock 2005, 24, 3–10. [Google Scholar] [CrossRef]
- Woolf, P.D.; McDonald, J.V.; Feliciano, D.V.; Kelly, M.M.; Nichols, D.; Cox, C. The catecholamine response to multisystem trauma. Arch. Surg. 1992, 127, 899–903. [Google Scholar] [CrossRef]
- Zagales, I.; Selvakumar, S.; Ngatuvai, M.; Fanfan, D.; Kornblith, L.; Santos, R.G.; Ibrahim, J.; Elkbuli, A. Beta-Blocker Therapy in Patients With Severe Traumatic Brain Injury: A Systematic Review and Me-ta-Analysis. Am. Surg. 2022, 89, 2020–2029. [Google Scholar] [CrossRef]
- Rizoli, S.B.; Jaja, B.N.R.; Di Battista, A.P.; Rhind, S.G.; Neto, A.C.; da Costa, L.; Inaba, K.; da Luz, L.T.; Nascimento, B.; Perez, A.; et al. Catecholamines as outcome markers in isolated traumatic brain injury: The COMA-TBI study. Crit. Care 2017, 21, 1–10. [Google Scholar] [CrossRef]
- Karlsberg, R.P.; Cryer, P.E.; Roberts, R. Serial plasma catecholamine response early in the course of clinical acute myocardial infarction: Relationship to infarct extent and mortality. Am. Hear. J. 1981, 102, 24–29. [Google Scholar] [CrossRef]
- Mueller, H.S.; Ayres, S.M. Propranolol decreases sympathetic nervous activity reflected by plasma catecholamines during evolution of myocardial infarction in man. J. Clin. Investig. 1980, 65, 338–346. [Google Scholar] [CrossRef]
- Wakade, A.R.; Wakade, T.D. Secretion of catecholamines from adrenal gland by a single electrical shock: Electronic depolarization of medullary cell membrane. Proc. Natl. Acad. Sci. USA 1982, 79, 3071–3074. [Google Scholar] [CrossRef]
- Brown, M.J.; Brown, D.C.; Murphy, M.B. Hypokalemia from Beta2-Receptor Stimulation by Circulating Epinephrine. N. Engl. J. Med. 1983, 309, 1414–1419. [Google Scholar] [CrossRef]
- Chen, W.; Lee, R.C. Electromediated permeabilization of frog skeletal muscle cell membrane: Effect of voltage-gated ion channels. Bioelectrochem. Bioenerg. 1994, 34, 157–167. [Google Scholar] [CrossRef]
- Gennari, F.J. Hypokalemia. N. Engl. J. Med. 1998, 339, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Palmer, B.F. Regulation of Potassium Homeostasis. Clin. J. Am. Soc. Nephrol. 2015, 10, 1050–1060. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.-H.; Halperin, M.L. Hypokalemia: A practical approach to diagnosis and its genetic basis. Curr. Med. Chem. 2007, 14, 1551–1565. [Google Scholar] [CrossRef]
- Huang, C.-L.; Kuo, E. Mechanism of hypokalemia in magnesium deficiency. J. Am. Soc. Nephrol. 2007, 18, 2649–2652. [Google Scholar] [CrossRef]
| Authors | Mechanism of Injury | Loss of Consciousness | Initial K (mmol/L) | Extremity Findings | Cardiac Arrest | ECG Abnormalities |
|---|---|---|---|---|---|---|
| Baker et al. | Lightning strike | Yes | 2.5 | Numbness and paresthesia of bilateral lower extremities | No | Mildly Prolonged QTc, small U wave |
| Rotariu and Manole [2] | Lightning strike | Yes | 3.1 | Not reported | Yes | Not reported |
| Bird et al. [10] | Power line | No | 1.6 | Weakness of bilateral upper and lower extremities | No | Prolonged QTc, T wave abnormalities |
| Dasgupta et al. [11] | 115 kV live wire | Yes | 1.7 | Flaccid paralysis of bilateral lower extremities | No | Not reported |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baker, M.B.; Binda, D.D.; Nozari, A.; Baker, W.E. The Silent Threat of Hypokalemia after High Voltage Electrical Injuries: A Case Study and Review of the Literature. J. Clin. Med. 2024, 13, 2852. https://doi.org/10.3390/jcm13102852
Baker MB, Binda DD, Nozari A, Baker WE. The Silent Threat of Hypokalemia after High Voltage Electrical Injuries: A Case Study and Review of the Literature. Journal of Clinical Medicine. 2024; 13(10):2852. https://doi.org/10.3390/jcm13102852
Chicago/Turabian StyleBaker, Maxwell B., Dhanesh D. Binda, Ala Nozari, and William E. Baker. 2024. "The Silent Threat of Hypokalemia after High Voltage Electrical Injuries: A Case Study and Review of the Literature" Journal of Clinical Medicine 13, no. 10: 2852. https://doi.org/10.3390/jcm13102852
APA StyleBaker, M. B., Binda, D. D., Nozari, A., & Baker, W. E. (2024). The Silent Threat of Hypokalemia after High Voltage Electrical Injuries: A Case Study and Review of the Literature. Journal of Clinical Medicine, 13(10), 2852. https://doi.org/10.3390/jcm13102852







