Impact of the COVID-19 Pandemic on Obesity, Metabolic Parameters and Clinical Values in the South Korean Adult Population
Abstract
1. Introduction
2. Materials and Methods
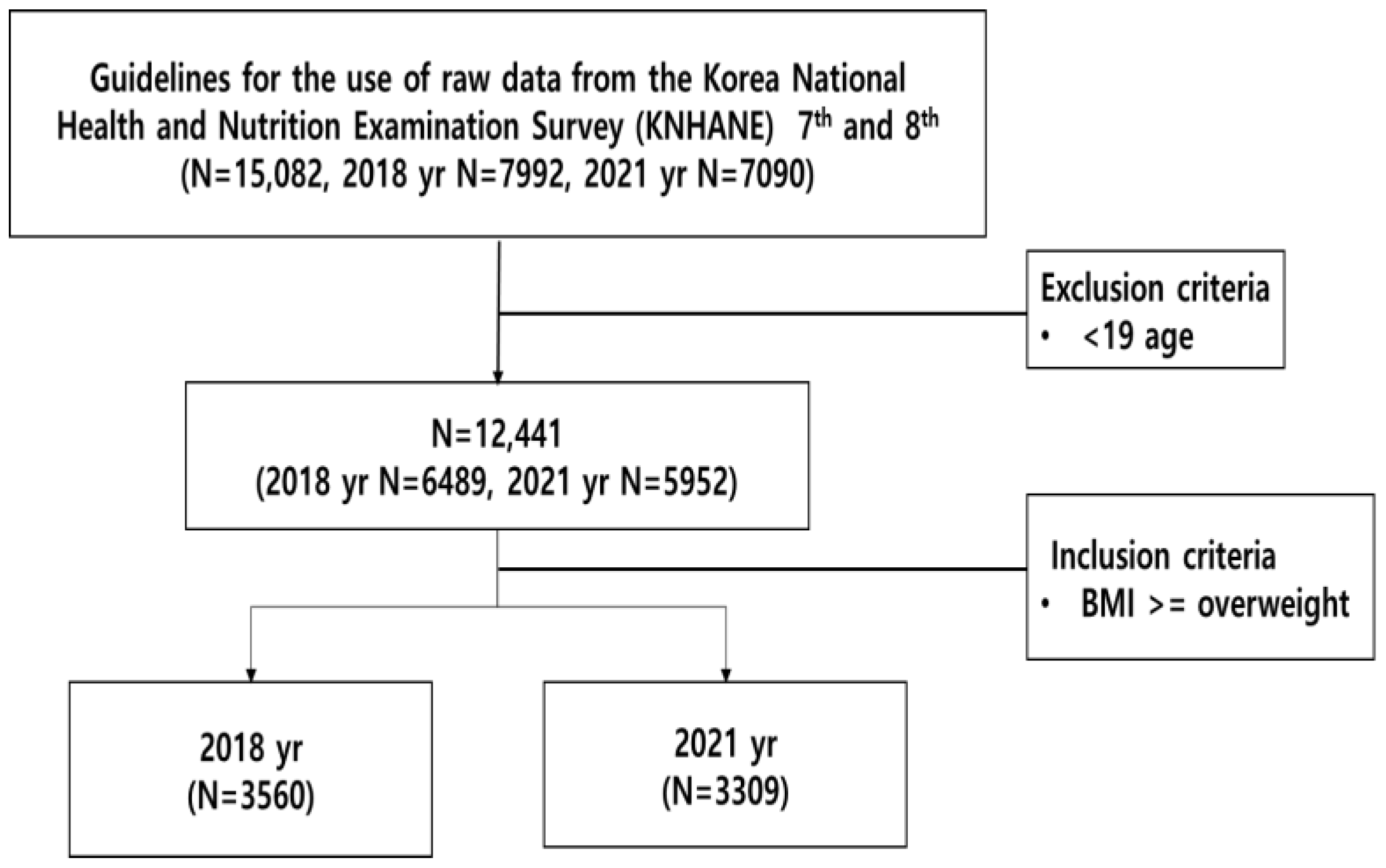
2.1. Study Designs and Sampling
2.2. Data Variables
2.3. Data Analysis
3. Results
3.1. Blood Pressure Changes in Overweight/Obese Adults Pre-/Post-COVID-19
3.2. Blood Test Changes in Overweight/Obese Adults Pre-/Post-COVID-19
3.3. Urinalysis Changes in Overweight/Obese Adults Pre/Post-COVID-19
3.4. Multivariate Analysis of Blood Test Changes Pre-/Post-COVID-19
3.5. Multivariate Analysis of Urine Test Changes Pre-/Post-COVID-19
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Afonso, P. The impact of the COVID-19 pandemic on mental health. Acta Medica Port. 2020, 33, 356–357. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Culture, Sports and Tourism. Public Perception Survey Regarding COVID-19 Self-Isolation. 2020. Available online: http://www.mcst.go.kr/english/ (accessed on 10 May 2023).
- Park, M.G. Corona 19 Crisis’ and Seeking Socio-Economic Transformation. Labor Rev. 2020, 187, 19–40. [Google Scholar]
- Korea Disease Control and Prevention Agency. Press Release. Korea Disease Control and Prevention Agency: Cheongju-si, Republic of Korea, 2020. Available online: https://www.kdca.go.kr/board/board.es?mid=a30402000000&bid=0030 (accessed on 10 May 2023).
- Kim, E.Y.; Kim, J.Y. Adult’s Perception of Every Day Life Change After COVID-19. J. Korea Acad.-Ind. Coop. Soc. 2022, 23, 377–385. [Google Scholar]
- Rotter, M.; Brandmaier, S.; Prehn, C.; Adam, J.; Rabstein, S. Stability of targeted metabolite profiles of urine samples under different storage conditions. Metabolomics 2017, 13, 4. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. (2.23) Briefing on the Pan-Governmental Meeting for COVID-19. Ministry of Health and Welfare: Sejong, Republic of Korea, 2020. Available online: https://www.mohw.go.kr/board.es?mid=a20401000000&bid=0032&tag=&act=view&list_no=353124 (accessed on 11 May 2023).
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard; World Health Organization: Geneva, Switzerland, 2021; [cited 18 October 2021]; Available online: https://covid19.who.int/ (accessed on 11 May 2023).
- Park, S.M. The impact of the COVID-19 pandemic on mental health among population. J. Health Educ. Promot. 2020, 37, 83–91. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. COVID-19 Pan-Government Preparedness Conference Briefing; Ministry of Health and Welfare: Sejong, Republic of Korea, 2020. Available online: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PARMENU_ID=04&MENU_ID=0403&page=2&CONT_SEQ=353064&SEARCHKEY=TITLE&SEARCHVALUE=23%EC%9D%BC (accessed on 11 May 2023).
- Jung, C.H.; Son, J.W.; Kang, S.; Kim, W.J.; Kim, H.S.; Kim, H.S.; Seo, M.; Shin, H.-J.; Lee, S.-S.; Jeong, S.J.; et al. Diabetes fact sheets in Korea, 2020: An appraisal of current status. J. Diabetes Metab. 2021, 45, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Korean Diabetes Association. Diabetes Fact Sheet in Korea; Korean Diabetes Association: Seoul, Republic of Korea, 2020. [Google Scholar]
- Kim, H.S. Importance of Target Blood Pressure Management in Diabetic Kidney Disease. J. Korea Contents Assoc. 2019, 19, 461–470. [Google Scholar]
- Kim, J.Y. The Study of Physical Activity Level on Serum BDNF and Cognitive Function in Adolescence. J. Growth Dev. 2014, 22, 119–125. [Google Scholar]
- Oh, J.W.; Woo, S.S.; Kwon, H.J.; Kim, Y.S. Examining the Association of Physical Activity and PAPS Health-related Physical Fitness on the Physical Self-Description of a Specialized Male Highschool Students. J. Phys. Educ. 2013, 52, 97–108. [Google Scholar]
- Lee, B.S. A Comparative Study on Dietary Life and Recognition of Diet Related Factors in Elementary, Middle and High School Students. Korean J. Diet. Assoc. 2004, 10, 364–374. [Google Scholar]
- Lee, A.; Tsang, C.K. Youth risk behavior in a Chinese population: A territory wide youth risk behavioral surveillance in Hong Kong. J. Public Health 2004, 118, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Kim, J.H. A Study Analyzing the Relationship among Impaired Fasting Glucose (IFG), Obesity Index, Physical Activity, and Beverage and Alcohol Consumption Frequency in 20s and 30s: The Korea National Health and Nutrition Examination Survey (KNHANES) 2013–2015. J. Community Living Sci. 2022, 33, 19–38. [Google Scholar] [CrossRef]
- Korea Diabetes Association (KDA). Clinical Practice Guidelines for Diabetes, 7th ed.; Korea Diabetes Association: Seoul, Republic of Korea, 2021; pp. 8–10. [Google Scholar]
- Blair, S.N.; Broney, S. Effects of physical inactivity and obesity on morbidity and mortality: Current evidence and research issues. Med. Sci. Sports Exerc. 1999, 31, S646. [Google Scholar] [CrossRef] [PubMed]
- Jekal, Y.; Lee, M.K.; Kim, E.S.; Park, J.H.; Lee, H.J.; Han, S.J.; Kang, E.S.; Lee, H.C.; Kim, S.Y.; Jeon, J.Y. Effects of walking and physical activity on glucose regulation among type 2 diabetics. J. Korean Diabetes 2008, 2, 60–67. [Google Scholar] [CrossRef]
- Singh, G.M.; Micha, R.; Khatibzadeh, S.; Lim, S.; Ezzati, M.; Mozaffarian, D. Chronic Diseases Expert G (2015) Estimated global, regional, and national disease burdens related to sugarsweetened beverage consumption in 2010. Circulation 2015, 132, 639–666. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Park, S.; Oh, K.; Choi, H.; Jeong, E.K. Changes in the management of hypertension, diabetes mellitus, and hypercholesterolemia in Korean adults before and during the coronavirus disease 2019 pandemic: Data from the 2010–2020 Korea National Health and Nutrition Examination Survey. Epidemiol. Health 2023, 45, e2023014. [Google Scholar] [CrossRef] [PubMed]
- Han, I.H.; Chong, M.Y. The Study on the Difference of Blood Level of HDL-Cholesterol by Obesity and Health Behavior from the Seventh (2016) Korea National Health and Nutrition Examination Survey. Korean Soc. Food Sci. Nutr. 2020, 49, 1377–1388. [Google Scholar] [CrossRef]
- Committee for Guidelines for Management of Dyslipidemia. Korean guidelines for management of dyslipidemia. J. Lipid Atheroscler. 2015, 4, 61–92. [Google Scholar] [CrossRef][Green Version]
- Dichtl, W.; Nilsson, L.; Goncalves, I.; Ares, M.; Banfi, C.; Calara, F.; Hamsten, A.; Erilsson, P.; Nilsson, J. Very low-density lipoprotein activates nuclear factor-κB in endothelial cells. Circ. Res. 1999, 84, 1085–1094. [Google Scholar] [CrossRef]
- Lutgens, E.; Van Suylen, R.J.; Faber, B.C.; Gijbels, M.J.; Eurlings, P.M.; Bijnens, A.P.; Cleutjens, K.B.; Heeneman, S.; Daemen, M. Atherosclerotic plaque rupture: Local or systemic process? Arterioscler. Thromb. Vasc. Biol. 2003, 23, 2123–2130. [Google Scholar] [CrossRef]
- Gordon, T.; Castelli, W.P.; Hjortland, M.C.; Kannel, W.B.; Dawber, T.R. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am. J. Med. 1977, 62, 707–714. [Google Scholar] [CrossRef] [PubMed]
- Song, S.O.; Hwang, Y.C.; Kahn, S.E.; Leonetti, D.L.; Fujimoto, W.Y.; Boyko, E.J. Intra-abdominal fat and high density lipoprotein cholesterol are associated in a non-linear pattern in Japanese Americans. Diabetes Metab. J. 2020, 44, 277–285. [Google Scholar] [CrossRef]
- de Melo, L.G.P.; Nunes, S.O.V.; Anderson, G.; Vargas, H.O.; Barbosa, D.S.; Galecki, P.; Carvalho, A.F.; Maes, M. Shared metabolic and immune-inflammatory, oxidative and nitrosative stress pathways in the metabolic syndrome and mood disorders. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2017, 78, 34–50. [Google Scholar] [CrossRef] [PubMed]
- Atti, A.R.; Valente, S.; Iodice, A.; Caramella, I.; Ferrari, B.; Albert, U.; Mandelli, L.; De Ronchi, D. Metabolic syndrome, mild cognitive impairment, and dementia: A meta-analysis of longitudinal studies. Am. J. Geriatr. Psychiatry 2019, 27, 625–637. [Google Scholar] [CrossRef]
- Jin, S.H. The Relation of Impaired Fasting Glucose and HDL-Cholesterol by Gender and Body Mass Index. J. Health Inform. Stat. 2019, 44, 8–13. [Google Scholar] [CrossRef][Green Version]
- Pal, K.; Mukadam, N.; Petersen, I.; Cooper, C. Mild cognitive impairment and progression to dementia in people with diabetes, prediabetes and metabolic syndrome: A systematic review and meta-analysis. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Rashid, S.; Genest, J. Effect of obesity on high-density lipoprotein metabolism. Obesity 2007, 15, 2875–2888. [Google Scholar] [CrossRef]
- Seo, J.B.; Chung, W.Y. The importance of treatment of low HDL cholesterolemia in cardiovascular disease. J. Lipid Atheroscler. 2008, 18, 270–276. [Google Scholar]
- Dufour, D.R.; Lott, J.A.; Nolte, F.S.; Gretch, D.R.; Koff, R.S.; Seeff, L.B. Diagnosis and monitoring of hepatic injury. II. recommendations for use of laboratory tests in screening, diagnosis, and monitoring. Clin. Chem. 2000, 46, 2050–2068. [Google Scholar] [CrossRef]
- Weiss, G.; Goodnough, L.T. Anemia of chronic disease. N. Engl. J. Med. 2005, 352, 1011–1023. [Google Scholar] [CrossRef]
- Sharrett, A.R.; Ballantyne, C.M.; Coady, S.A.; Heiss, G.; Sorlie, P.D.; Catellier, D.; Patsch, W. Coronary heart disease prediction from lipoprotein cholesterol levels, triglycerides, lipoprotein(a), apolipoproteins A-I and B, and HDL density subfractions: The Atherosclerosis Risk in Communities (ARIC) study. Circulation 2001, 104, 1108–1113. [Google Scholar] [CrossRef] [PubMed]
- Cavezzi, A.; Emidio, T.; Salvatore, C. COVID-19: Hemoglobin, iron, and hypoxia beyond inflammation. A narrative review. Clin. Pract. 2020, 10, 1271. [Google Scholar] [PubMed]
- Medical Information on the National Health Information Portal. Available online: https://health.kdca.go.kr/healthinfo/ (accessed on 21 May 2023).
- Paolone, G.; Mazzitelli, C.; Formiga, S.; Kaitsas, F.; Breschi, L.; Mazzoni, A.; Tete, G.; Polizzi, E.; Gherlone, E.; Cantatore, G. One-year impact of COVID-19 pandemic on Italian dental professionals: A cross-sectional survey. Minerva Dent. Oral. Sci. 2022, 71, 212–222. [Google Scholar] [CrossRef] [PubMed]
- Gherlone, E.; Polizzi, E.; Tete, G.; Cappare, P. Dentistry and Covid-19 pandemic: Operative indications post-lockdown. New Microbiol. 2021, 44, 1–11. [Google Scholar] [PubMed]
| Characteristic | Before the COVID-19 Outbreak (2018) | After the COVID-19 Outbreak (2021) | Z 2/4X2 | p-Value 3 | |||||
|---|---|---|---|---|---|---|---|---|---|
| N 5/Mean 1 | % 5/SD 1 | N/Mean | %/SD | ||||||
| Sex 4 | Male | 1817 | 51.0 | 1687 | 51.0 | 0.002 | 0.962 | ||
| Female | 1743 | 49.0 | 1622 | 49.0 | |||||
| Age 1 | 53.54 | 15.97 | 54.73 | 16.39 | −3.382 | 0.001 | |||
| Height (cm) 1 | 163.81 | 9.85 | 163.97 | 10.03 | −0.501 | 0.617 | |||
| Weight (kg) 1 | 70.79 | 11.58 | 71.26 | 12.02 | −1.363 | 0.173 | |||
| Waist circumference 1 | 88.41 | 7.95 | 90.35 | 8.20 | −9.694 | <0.001 | |||
| Body mass index (BMI) 1 | 26.28 | 2.77 | 26.39 | 2.88 | −1.499 | 0.134 | |||
| Pulse (60 s) 1 | 56.68 | 10.60 | 57.62 | 13.00 | −0.711 | 0.477 | |||
| Systole 1, 6 | 122.12 | 16.29 | 123.32 | 15.12 | −3.593 | <0.001 | |||
| Diastole 1, 6 | 77.39 | 10.45 | 75.56 | 9.60 | −8.255 | <0.001 | |||
| BMI 4 (weight control for 1 year) | BMI 23.0~24.9 (overweight) | Loss effort | 545 | 39.0 | 529 | 41.6 | 3.908 | 0.272 | |
| Maintenance effort | 313 | 22.4 | 299 | 23.5 | |||||
| Gain effort | 28 | 2.0 | 23 | 1.8 | |||||
| Never effort | 510 | 36.5 | 420 | 33.0 | |||||
| BMI 25.0~29.9 (obesity) | Loss effort | 992 | 55.3 | 931 | 55.8 | 10.432 | 0.015 | ||
| Maintenance effort | 241 | 13.4 | 279 | 16.7 | |||||
| Gain effort | 6 | 0.3 | 5 | 0.3 | |||||
| Never effort | 554 | 30.9 | 453 | 27.2 | |||||
| BMI 30.0 over (high obesity) | Loss effort | 219 | 64.4 | 228 | 65.3 | 0.249 | 0.883 | ||
| Maintenance effort | 32 | 9.4 | 35 | 10.0 | |||||
| Gain effort | 0 | 0.0 | 0 | 0.0 | |||||
| Never effort | 89 | 26.2 | 86 | 24.6 | |||||
| Characteristic | Before the COVID-19 Outbreak (2018) | After the COVID-19 Outbreak (2021) | Z 2/4X2 | p-Value 3 | |||
|---|---|---|---|---|---|---|---|
| N 5/Mean 1 | % 5/SD 1 | N/Mean | %/SD | ||||
| Fasting blood sugar (FBS) 1 | 104.84 | 24.24 | 106.60 | 25.98 | −4.508 | <0.001 | |
| HbA1c 1 | 5.83 | 0.84 | 5.97 | 0.90 | −9.984 | <0.001 | |
| Total cholesterol 1 | 193.81 | 39.21 | 189.07 | 40.17 | −4.845 | <0.001 | |
| HDL cholesterol 1 | 48.02 | 11.26 | 49.17 | 11.66 | −4.114 | <0.001 | |
| Triglycerides 1 | 154.60 | 118.50 | 141.33 | 106.48 | −6.643 | <0.001 | |
| LDL cholesterol 1 | 115.86 | 33.96 | 116.24 | 35.98 | −0.075 | 0.940 | |
| Hypercholesterolemia 4 | No | 2370 | 70.6 | 2092 | 66.6 | 12.557 | <0.001 |
| Yes | 985 | 29.4 | 1051 | 33.4 | |||
| Hypertriglyceridemia 4 | No | 2233 | 79.8 | 2388 | 84.5 | 21.389 | <0.001 |
| Yes | 566 | 20.2 | 438 | 15.5 | |||
| AST(SGOT) 1 | 25.23 | 14.37 | 26.41 | 12.88 | −5.977 | <0.001 | |
| ALT(SGPT) 1 | 26.40 | 19.20 | 27.45 | 21.28 | −2.622 | 0.009 | |
| Hepatitis B surface antigen 4 | Negative | 3354 | 97.1 | 3141 | 97.1 | 0.002 | 0.966 |
| Positive | 101 | 2.9 | 94 | 2.9 | |||
| Hepatitis C antibody 4 | Negative | 3429 | 99.2 | 3203 | 99.0 | 1.089 | 0.297 |
| Positive | 26 | 0.8 | 32 | 1.0 | |||
| Hemoglobin 1 | 14.37 | 1.60 | 14.03 | 1.58 | −8.663 | <0.001 | |
| Hematocrit 1 | 43.00 | 4.30 | 42.56 | 4.28 | −4.074 | <0.001 | |
| Anemia 4 | Negative | 3234 | 93.8 | 2906 | 89.9 | 33.283 | <0.001 |
| Positive | 215 | 6.2 | 326 | 10.1 | |||
| Blood urea nitrogen 1 | 15.74 | 4.89 | 15.25 | 4.73 | −4.590 | <0.001 | |
| Blood creatinine 1 | 0.83 | 0.21 | 0.82 | 0.22 | −1.650 | 0.099 | |
| WBC 1 | 6.35 | 1.74 | 6.26 | 1.66 | −2.205 | 0.027 | |
| RBC 1 | 4.66 | 0.50 | 4.63 | 0.51 | −2.563 | 0.010 | |
| Platelets 1 | 262.32 | 64.45 | 253.84 | 62.79 | −5.251 | <0.001 | |
| Characteristic | Before the COVID-19 Outbreak (2018) | After the COVID-19 Outbreak (2021) | Z 2/4X2 | p-Value 3 | |||
|---|---|---|---|---|---|---|---|
| N/Mean 1 | %/SD 1 | N/Mean | %/SD | ||||
| Uric acid 1 | 5.44 | 1.41 | 5.47 | 1.43 | −0.970 | 0.332 | |
| Uric acidity 1 | 5.87 | 0.74 | 5.90 | 0.77 | −0.940 | 0.347 | |
| Nitrate 4 | No | 3334 | 97.5 | 3172 | 97.7 | 0.490 | 0.484 |
| Yes | 87 | 2.5 | 74 | 2.3 | |||
| Urine protein 4 | Negative | 2743 | 80.2 | 2950 | 90.9 | 171.090 | <0.001 |
| Trace | 510 | 14.9 | 197 | 6.1 | |||
| 1 + | 131 | 3.8 | 65 | 2.0 | |||
| 2 + | 33 | 1.0 | 28 | 0.9 | |||
| 3 + | 1 | 0.0 | 4 | 0.1 | |||
| 4 + | 3 | 0.1 | 2 | 0.1 | |||
| Urine glucose 4 | Negative | 3241 | 94.7 | 2984 | 91.9 | 40.045 | <0.001 |
| Trace | 44 | 1.3 | 66 | 2.0 | |||
| 1 + | 23 | 0.7 | 35 | 1.1 | |||
| 2 + | 33 | 1.0 | 25 | 0.8 | |||
| 3 + | 38 | 1.1 | 33 | 1.0 | |||
| 4 + | 42 | 1.2 | 103 | 3.2 | |||
| Urine ketone 4 | Negative | 3370 | 98.5 | 3209 | 98.9 | 20.122 | <0.001 |
| Trace | 17 | 0.5 | 0 | 0.0 | |||
| 1 + | 20 | 0.6 | 28 | 0.9 | |||
| 2 + | 12 | 0.4 | 9 | 0.3 | |||
| 3 + | 2 | 0.1 | - | - | |||
| 4 + | - | - | - | - | |||
| Urine bilirubin 4 | Negative | 3397 | 99.3 | 3246 | 100.0 | 22.855 | <0.001 |
| trace | - | - | - | - | |||
| 1 + | 24 | 0.7 | - | - | |||
| 2 + | - | - | - | - | |||
| 3 + | - | - | - | - | |||
| 4 + | - | - | - | - | |||
| Urine occult blood 4 | Negative | 2831 | 82.8 | 3034 | 93.5 | 191.933 | <0.001 |
| trace | 336 | 9.8 | 122 | 3.8 | |||
| 1 + | 138 | 4.0 | 32 | 1.0 | |||
| 2 + | 67 | 2.0 | 30 | 0.9 | |||
| 3 + | 43 | 1.3 | 28 | 0.9 | |||
| 4 + | 6 | 0.2 | - | - | |||
| Urine bilinogen 4 | Negative | 3405 | 99.5 | 3222 | 99.3 | 8.533 | 0.014 |
| trace | 4 | 0.1 | - | - | |||
| 1 + | 12 | 0.4 | 23 | 0.7 | |||
| 2 + | - | - | 1 | 0.0 | |||
| 3 + | - | - | - | - | |||
| 4 + | - | - | - | - | |||
| Urine creatinine 1 | 147.08 | 80.10 | 125.89 | 74.77 | −11.726 | 0.000 | |
| Urine sodium 1 | 116.79 | 48.09 | 113.66 | 47.75 | −3.212 | 0.001 | |
| Urine potassium 1 | 52.66 | 23.22 | 41.51 | 20.75 | −19.034 | 0.000 | |
| Urine cotinine 1 | 346.22 | 718.56 | 783.69 | 826.45 | −23.264 | 0.000 | |
| Blood Test * | Urine Test * | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| ORs | 95% CI | p-Value | ORs | 95% CI | p-Value | ||||
| Systole | 1 + 0.019 | 1.014 | 1.024 | <0.001 | Systole | 1.018 | 1.010 | 1.025 | <0.001 |
| Diastole | 0.958 | 0.948 | 0.969 | < 0.001 | |||||
| Diastole | 0.964 | 0.956 | 0.972 | <0.001 | Protein No | <0.001 | |||
| Ttrace | 0.385 | 0.276 | 0.537 | <0.001 | |||||
| FBS | 1.000 | 0.995 | 1.004 | 0.910 | Protein 1+ | 0.597 | 0.340 | 1.049 | 0.073 |
| Protein 2+ | 1.281 | 0.487 | 3.371 | 0.616 | |||||
| HbA1c | 1.062 | 0.934 | 1.206 | 0.359 | Protein 3+ | 5.83 × 109 | 0.000 | 0.999 | |
| Total cholesterol | 0.999 | 0.997 | 1.001 | 0.201 | Protein 4+ | 0.000 | 0.000 | 0.999 | |
| Glucose No | 0.001 | ||||||||
| HDL cholesterol | 1.010 | 1.004 | 1.016 | 0.001 | Trace | 1.832 | 0.980 | 3.425 | 0.058 |
| Glucose 1+ | 1.949 | 0.807 | 4.710 | 0.138 | |||||
| Triglycerides | 1.000 | 0.999 | 1.000 | 0.322 | Glucose 2+ | 0.420 | 0.171 | 1.028 | 0.057 |
| Glucose 3+ | 0.630 | 0.280 | 1.415 | 0.263 | |||||
| Hypercholesterolemia, yes | 1.131 | 0.993 | 1.287 | 0.063 | Glucose 4+ | 2.311 | 1.350 | 3.955 | 0.002 |
| Ketone No | 0.699 | ||||||||
| Hypertriglyceridemia, yes | 0.917 | 0.741 | 1.134 | 0.422 | Trace | 0.000 | 0.000 | 0.998 | |
| Ketone 1+ | 1.460 | 0.556 | 3.829 | 0.442 | |||||
| AST (SGOT) | 1.004 | 0.998 | 1.011 | 0.189 | Ketone 2+ | 1.861 | 0.498 | 6.945 | 0.355 |
| Urine bilirubin Trace | 0.000 | 0.000 | 0.999 | ||||||
| ALT (SGPT) | 1.003 | 0.998 | 1.008 | 0.245 | Urine occult blood No | <0.001 | |||
| Trace | 0.374 | 0.246 | 0.568 | <0.001 | |||||
| Hemoglobin | 0.280 | 0.240 | 0.326 | <0.001 | Occult blood 1+ | 0.203 | 0.085 | 0.481 | <0.001 |
| Occult blood 2+ | 0.477 | 0.193 | 1.178 | 0.108 | |||||
| Hematocrit | 1.476 | 1.386 | 1.572 | <0.001 | Occult blood 3+ | 0.963 | 0.408 | 2.274 | 0.931 |
| Occult blood 4+ | 0.000 | 0.000 | 0.999 | ||||||
| Blood urea nitrogen | 0.963 | 0.950 | 0.975 | <0.001 | Urobilinogen No | - | - | - | 0.660 |
| Trace | 0.000 | 0.000 | - | 0.999 | |||||
| WBC | 0.964 | 0.928 | 1.001 | 0.056 | Urobilinogen 1+ | 1.584 | 0.589 | 4.261 | 0.362 |
| Urine creatinine | 1.003 | 1.001 | 1.005 | <0.001 | |||||
| RBC | 1.352 | 1.016 | 1.801 | 0.039 | Urine sodium | 1.000 | 0.998 | 1.002 | 0.776 |
| Urine potassium | 0.973 | 0.968 | 0.977 | <0.001 | |||||
| Platelets | 0.996 | 0.995 | 0.997 | <0.001 | Urine cotinine | 1.001 | 1.001 | 1.001 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, A.; Kim, E.-y.; Kim, J. Impact of the COVID-19 Pandemic on Obesity, Metabolic Parameters and Clinical Values in the South Korean Adult Population. J. Clin. Med. 2024, 13, 2814. https://doi.org/10.3390/jcm13102814
Kim A, Kim E-y, Kim J. Impact of the COVID-19 Pandemic on Obesity, Metabolic Parameters and Clinical Values in the South Korean Adult Population. Journal of Clinical Medicine. 2024; 13(10):2814. https://doi.org/10.3390/jcm13102814
Chicago/Turabian StyleKim, Anna, Eun-yeob Kim, and Jaeyoung Kim. 2024. "Impact of the COVID-19 Pandemic on Obesity, Metabolic Parameters and Clinical Values in the South Korean Adult Population" Journal of Clinical Medicine 13, no. 10: 2814. https://doi.org/10.3390/jcm13102814
APA StyleKim, A., Kim, E.-y., & Kim, J. (2024). Impact of the COVID-19 Pandemic on Obesity, Metabolic Parameters and Clinical Values in the South Korean Adult Population. Journal of Clinical Medicine, 13(10), 2814. https://doi.org/10.3390/jcm13102814






