Resilience, Burnout and Mental Health in Nurses: A Latent Mediation Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedure
2.2. Instruments
2.3. Data Analysis
3. Results
3.1. Preliminary Analyses
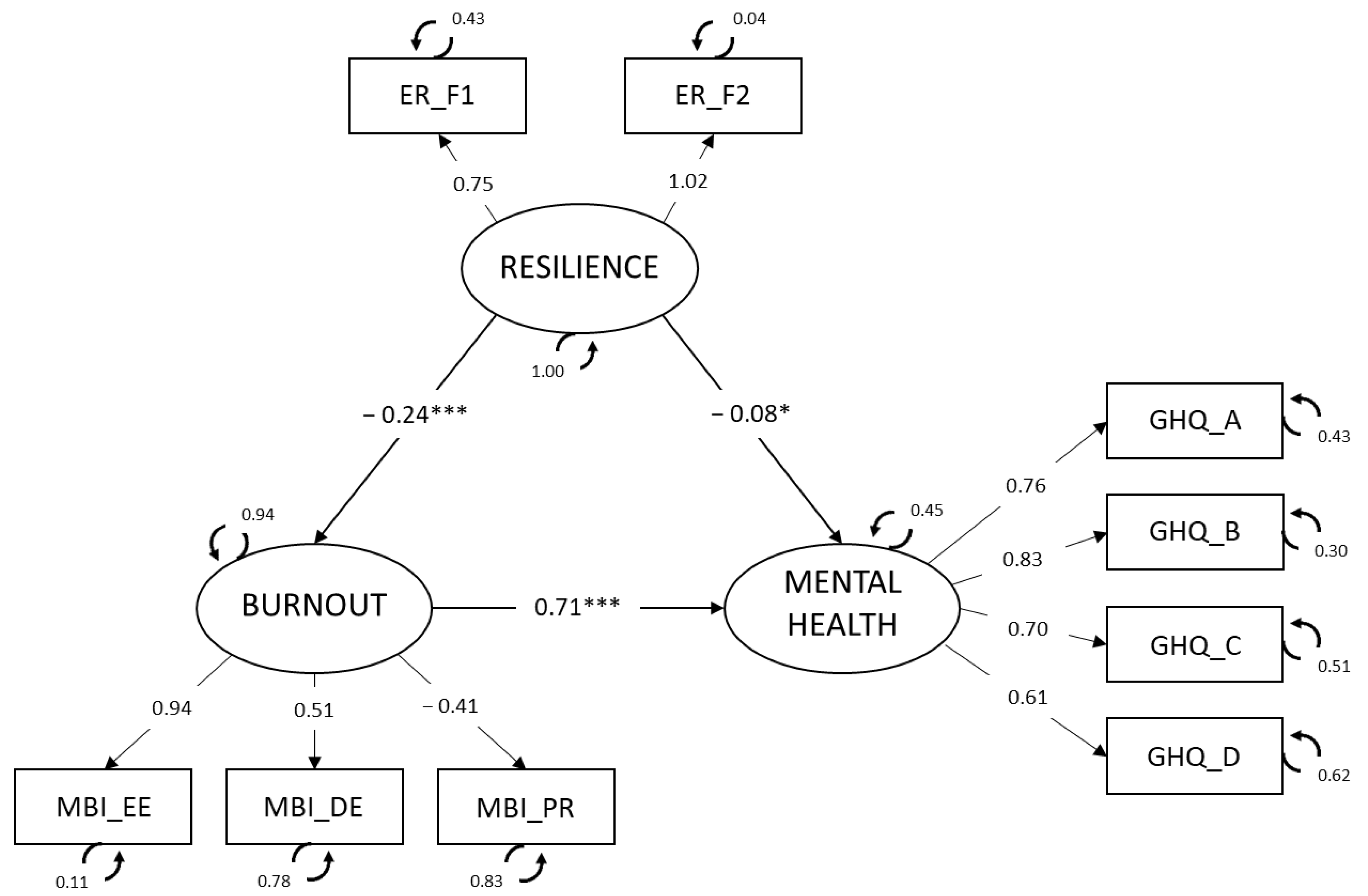
3.2. Structural Equation Model: A Latent Mediation Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Luo, M.; Guo, L.; Yu, M.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Instituto de Salud Carlos III—Informe de Evolución Diaria de la Pandemia de COVID-19 en España nº 66 [Carlos III Health Institute—Daily Evolution Report of the COVID-19 Pandemic in Spain no. 66]. 2021. Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/INFORMES%20COVID-19%202021/Informe%20COVID-19.%20N%C2%BA%2066_17%20de%20febrero%20de%202021.pdf (accessed on 17 February 2021).
- Sahebi, A.; Golitaleb, M.; Moayedi, S.; Torres, M.; Sheikhbardsiri, H. Prevalence of workplace violence against health care workers in hospital and pre-hospital settings: An umbrella review of meta-analyses. Front. Public Health 2022, 10, 895818. [Google Scholar] [CrossRef]
- Gázquez, J.J.; Molero, M.M.; Martos, Á.; Jiménez-Rodríguez, D.; Pérez-Fuentes, M.C. The repercussions of perceived threat from COVID-19 on the mental health of actively employed nurses. Int. J. Ment. Health Nurs. 2021, 30, 724–732. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.C.; Quiban, C.; Sloan, C.; Montejano, A. Predictors of poor mental health among nurses during COVID-19 pandemic. Nurs. Open 2020, 8, 900–907. [Google Scholar] [CrossRef]
- Sheikhbardsiri, H.; Doustmohammadi, M.M.; Afshar, P.J.; Heidarijamebozorgi, M.; Khankeh, H.; Beyramijam, M. Anxiety, stress and depression levels among nurses of educational hospitals in Iran: Time of performing nursing care for suspected and confirmed COVID-19 patients. J. Educ. Health Promot. 2021, 10, 447. [Google Scholar] [CrossRef] [PubMed]
- Luceño-Moreno, L.; Talavera-Velasco, B.; García-Albuerne, Y.; Martín-García, J. Symptoms of Posttraumatic Stress, Anxiety, Depression, Levels of Resilience and Burnout in Spanish Health Personnel during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 5514. [Google Scholar] [CrossRef]
- Coyle, S.; Vagos, P.; Masia, C.; Silva, J.; Xavier, A.; Martin, G.; Wimmer, J.; Kalvera, A.; Jeyanayagam, B.; Lekas, H.-M.; et al. A qualitative study of social anxiety and impairment amid the COVID-19 pandemic for adolescents and young adults in Portugal and the US. Eur. J. Educ. Psychol. 2022, 15, 115–131. [Google Scholar] [CrossRef]
- Wańkowicz, P.; Szylińska, A.; Rotter, I. Assessment of Mental Health Factors among Health Professionals Depending on Their Contact with COVID-19 Patients. Int. J. Environ. Res. Public Health 2020, 17, 5849. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Greenglass, E.R. Introduction to special issue on burnout and health. Psychol. Health 2001, 16, 501–510. [Google Scholar] [CrossRef] [PubMed]
- Sanftenberg, L.; Gschwendner, M.; Grass, A.; Rottenkolber, M.; Zöllinger, I.; Sebastiao, M.; Kühlein, T.; Hindenburg, D.; Gágyor, I.; Wildgruber, D.; et al. Associations of Mental Health Issues with Health Literacy and Vaccination Readiness against COVID-19 in Long-Term Care Facilities—A Cross-Sectional Analysis. Eur. J. Investig. Health Psychol. Educ. 2024, 14, 432–446. [Google Scholar] [CrossRef]
- Walton, M.; Murray, E.; Christian, M.D. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Schaufeli, W.B.; Leiter, M.P.; Maslach, C.; Jackson, S.E. Maslach Burnout Inventory-General Survey (MBI-GS). In MBI Manual, 3rd ed.; Maslach, C., Jackson, S.E., Leiter, M.P., Eds.; Consulting Psychologists Press: Palo Alto, CA, USA, 1996; pp. 19–26. [Google Scholar]
- Gascon, S.; Leiter, M.P.; Andrés, E.; Santed, M.A.; Pereira, J.P.; Cunha, M.J.; Albesa, A.; Montero-Marín, J.; García-Campayo, J. The role of aggressions suffered by healthcare workers as predictors of burnout. J. Clin. Nurs. 2013, 22, 3120–3129. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Bradley, K.A.; Wipf, J.E.; Back, A.L. Burnout and self-reported patient care in an internal medicine residency program. Ann. Intern. Med. 2002, 136, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Alimoglu, M.K.; Donmez, L. Daylight exposure and the other predictors of burnout among nurses in a University Hospital. Int. J. Nurs. Stud. 2005, 42, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Gallego, V.; Albaladejo, N.M.; Roldan, V.; Cuines, M.C.; Gracia, A.B. Percepción de personal sanitario y pacientes sobre el ruido hospitalario [Perception of healthcare personnel and patients about hospital noise]. Eur. J. Health. Res. 2023, 9, 1–14. [Google Scholar] [CrossRef]
- Quevedo-Blasco, R.; Pérez, M.J.; Guillén-Riquelme, A.; Hess, T. Civil Liability for Clinical Misdiagnosis of Suicidal Intention: Procedure and Guidelines to Minimize Fatal Diagnostic Error. Eur. J. Psychol. Appl. Leg. Context. 2023, 15, 73–81. [Google Scholar] [CrossRef]
- Gao, T.; Ding, X.; Chai, J.; Zhang, Z.; Zhang, H.; Kong, Y.; Mei, S. The influence of resilience on mental health: The role of general well-being. Int. J. Nurs. Pract. 2017, 23, e12535. [Google Scholar] [CrossRef] [PubMed]
- Kaviani, F.; Aliakbari, F.; Sheikhbardsiri, H.; Arbon, P. Nursing Students’ Competency to Attend Disaster Situations: A Study in Western Iran. Disaster Med. Public Health Prep. 2022, 16, 2044–2048. [Google Scholar] [CrossRef]
- Nejadshafiee, M.; Nekoei-Moghadam, M.; Bahaadinbeigy, K.; Khankeh, H.; Sheinkhbardsiri, H. Providing telenursing care for victims: A simulated study for introducing of possibility nursing interventions in disasters. BMC Med. Inform Decis. Mak. 2022, 22, 54. [Google Scholar] [CrossRef]
- Rushton, C.H.; Batcheller, J.; Schroeder, K.; Donohue, P. Burnout and resilience among nurses practicing in high-intensity settings. Am. J. Respir. Crit. Care Med. 2016, 24, 412–420. [Google Scholar] [CrossRef]
- Jenaro, C.; Flores, N.; Orgaz, M.B.; Cruz, M. Vigour and dedication in nursing professionals: Towards a better understanding of work engagement. J. Adv. Nurs. 2011, 67, 865–875. [Google Scholar] [CrossRef] [PubMed]
- Molero, M.M.; Martos, Á.; Pérez-Fuentes, M.C.; Tortosa, B.M.; Sisto, M.; Simón, M.M.; Gázquez, J.J. Humanization, Adaptation to Change, and Mental Health in Teachers in Three European Countries. Eur. J. Psychol. Appl. Leg. Context. 2024, 16, 17–25. [Google Scholar] [CrossRef]
- Molero, M.M.; Pérez-Fuentes, M.C.; Gázquez, J.J.; Barragán, A.B. Burnout in Health Professionals According to Their Self-Esteem, Social Support and Empathy Profile. Front. Psychol. 2018, 9, 424. [Google Scholar] [CrossRef]
- McKinley, N.; McCain, R.S.; Convie, L.; Clarke, M.; Dempster, M.; Campbell, W.J.; Kirk, S.J. Resilience, burnout and coping mechanisms in UK doctors: A cross-sectional study. BMJ Open 2020, 10, e031765. [Google Scholar] [CrossRef] [PubMed]
- Jackson, D.; Firtko, A.; Edenborough, M. Personal resilience as a strategy for surviving and thriving in the face of workplace adversity: A literature review. J. Adv. Nurs. 2007, 60, 1–9. [Google Scholar] [CrossRef]
- Young, P.D.; Rushton, C.H. A concept analysis of moral resilience. Nurs. Outlook 2017, 65, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Delgado, C.; Upton, D.; Ranse, K.; Furness, T.; Foster, K. Nurses’ resilience and the emotional labour of nursing work: An integrative review of empirical literature. Int. J. Nurs. Stud. 2017, 70, 71–88. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, B.; Brewer, M. What do we know about student resilience in health professional education? A scoping review of the literature. Nurse Educ. Today 2017, 58, 65–71. [Google Scholar] [CrossRef]
- Bakalova, D.; Nacheva, I.; Panchelieva, T. Psychological Predictors of COVID-19-Related Anxiety in Vulnerable Groups. Eur. J. Investig. Health Psychol. Educ. 2023, 13, 1815–1830. [Google Scholar] [CrossRef]
- Guo, Y.; Luo, Y.; Lam, L.; Cross, W.; Plummer, V.; Zhang, J. Burnout and its association with resilience in nurses: A cross-sectional study. J. Clin. Nurs. 2018, 27, 441–449. [Google Scholar] [CrossRef]
- McDonald, G.; Jackson, D.; Wilkes, L.; Vickers, H.M. Personal resilience in nurses and midwives: Effects of a work-based educational intervention. Contemp. Nurse 2013, 45, 134–143. [Google Scholar] [CrossRef] [PubMed]
- The Joint Commission. Quick Safety Issue 50: Developing Resilience to Combat Nurse Burnout. 2019. Available online: https://www.jointcommission.org/resources/news-and-multimedia/newsletters/newsletters/quick-safety/quick-safety-50-developing-resilience-to-combat-nurse-burnout/ (accessed on 22 February 2021).
- West, C.P.; Dyrbye, L.N.; Sinsky, C.; Trockel, M.; Tutty, M.; Nedelec, L.; Carlasare, L.E.; Shanafelt, T.D. Resilience and Burnout Among Physicians and the General US Working Population. JAMA Netw. Open 2020, 3, e209385. [Google Scholar] [CrossRef]
- Arrogante, O.; Aparicio-Zaldivar, E. Burnout and health among critical care professionals: The mediational role of resilience. Intensive Crit. Care Nurs. 2017, 42, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Ertem, M.; Capa, S.; Karakas, M.; Ensari, H.; Koc, A. Investigation of the Relationship Between Nurses’ Burnout and Psychological Resilience Levels. Clin. Exp. Health Sci. 2020, 1, 9–15. [Google Scholar] [CrossRef]
- Treglown, L.; Palaiou, K.; Zarola, A.; Furnham, A. The Dark Side of Resilience and Burnout: A Moderation-Mediation Model. PLoS ONE 2016, 11, e0156279. [Google Scholar] [CrossRef] [PubMed]
- Wagnild, G.M. The Resilience Scale User’s Guide for the US English Version of the Resilience Scale and the 14-Item Resilience Scale; The Resilience Center: Worden, MT, USA, 2009. [Google Scholar]
- Moon, Y.; Shin, S.Y. Moderating Effects of Resilience on the Relationship Between Emotional Labor and Burnout in Care Workers. J. Gerontol. Nurs. 2018, 44, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Yu, F.; Raphael, D.; Mackay, L.; Smith, M.; King, A. Personal and work-related factors associated with nurse resilience: A systematic review. Int. J. Nurs. Stud. 2019, 93, 129–140. [Google Scholar] [CrossRef]
- Deldar, K.; Froutan, R.; Dalvand, S.; Ghanei, R.; Mazloum, S.R. The Relationship between Resiliency and Burnout in Iranian Nurses: A Systematic Review and Meta-Analysis. Open Access Maced J. Med. Sci. 2018, 6, 2250–2256. [Google Scholar] [CrossRef] [PubMed]
- Foster, K.; Roche, M.; Delgado, C.; Cuzzillo, C.; Giandinoto, J.A.; Furness, T. Resilience and mental health nursing: An integrative review of international literature. Int. J. Mental Health Nurs. 2019, 28, 71–85. [Google Scholar] [CrossRef]
- Badu, E.; O’Brien, A.P.; Mitchell, R.; Rubin, M.; James, C.; McNeil, K.; Nguyen, K.; Giles, M. Workplace stress and resilience in the Australian nursing workforce: A comprehensive integrative review. Int. J. Ment. Health Nurs 2020, 29, 5–34. [Google Scholar] [CrossRef]
- Platania, S.; Gruttadauria, S.V.; Morando, M. Dispositional Resilience as Mediator in Psychological Stress on Healthcare Workers: A Multi-Group Analysis of Frontline and Non-Frontline Workers. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 1285–1299. [Google Scholar] [CrossRef]
- Yörük, S.; Güler, D. The relationship between psychological resilience, burnout, stress, and sociodemographic factors with depression in nurses and midwives during the COVID-19 pandemic: A cross-sectional study in Turkey. Perspect Psychiatr. Care 2021, 57, 390–398. [Google Scholar] [CrossRef] [PubMed]
- Serrão, C.; Duarte, I.; Castro, L.; Teixeira, A. Burnout and Depression in Portuguese Healthcare Workers during the COVID-19 Pandemic—The Mediating Role of Psychological Resilience. Int. J. Environ. Res. Public Health 2021, 18, 636. [Google Scholar] [CrossRef]
- Grabbe, L.; Higgins, M.K.; Baird, M.; Craven, P.A.; San Fratello, S. The Community Resiliency Model (R) to promote nurse well-being. Nurs. Outlook 2020, 68, 324–336. [Google Scholar] [CrossRef] [PubMed]
- Mealer, M.; Jones, J.; Newman, J.; McFann, K.K.; Rothbaum, B.; Moss, M. The Presence of Resilience is Associated with a Healthier Psychological Profile in Intensive Care Unit (ICU) Nurses: Results of a National Survey. Int. J. Nurs. Stud. 2012, 49, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, P.; Gomes, S. The Role of Resilience in Reducing Burnout: A Study with Healthcare Workers during the COVID-19 Pandemic. Soc. Sci. 2021, 10, 317. [Google Scholar] [CrossRef]
- Sánchez-Teruel, D.; Robles-Bello, M.A. Escala de resiliencia 14 ítems (RS-14): Propiedades psicométricas de la versión en español. Rev. Iberoam Diagn Ev. 2015, 2, 103–113. [Google Scholar]
- Maslach, C.; Jackson, S. MBI: Maslach Burnout Inventory Manual; Consulting Psychologists Press: Palo Alto, CA, USA, 1981. [Google Scholar]
- Gil-Monte, P.R.; Peiró, J.M. Desgaste Psíquico en el Trabajo: El Síndrome de Quemarse [Psychological Exhaustion at Work: Burnout Syndrome]; Sínteis: Madrid, Spain, 1997. [Google Scholar]
- Goldberg, D.; Hillier, V. A scaled version of the General Health Questionnaire. Psychol. Med. 1979, 9, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Lobo, A.; Pérez-Echeverría, M.J.; Artal, J. Validity of the scaled version of the General Health Questionnaire (GHQ-28) in a Spanish population. Psychol. Med. 1986, 16, 135–140. [Google Scholar] [CrossRef]
- IBM Corp. Released. IBM SPSS Statistics for Windows, Version 24.0.; IBM Corp.: Armonk, NY, USA, 2016. [Google Scholar]
- McDonald, R.P. Test Theory: A Unified Approach; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1999. [Google Scholar]
- Ventura-León, J.L.; Caycho, T. El coeficiente Omega: Un método alternativo para la estimación de la confiabilidad [The Omega coefficient: An alternative method for estimating reliability]. Rev. Latinoam. Cienc. Soc. Niñez Juv. 2017, 15, 625–627. [Google Scholar]
- Rosseel, Y. Lavaan: An R package for structural equation modeling and more. Version 0.5–12 (BETA). J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- JASP Team. JASP, Version 0.14; Computer Software; JASP Team: Amsterdam, The Netherlands, 2020.
- Iacobucci, D. Structural equations modeling: Fit indices, sample size, and advanced topics. J. Consum. Psychol. 2010, 20, 90–98. [Google Scholar] [CrossRef]
- Bentler, P. EQS Structural Equations Program Manual; BMDP Statistical Software: Los Angeles, CA, USA, 1989. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
| Resilience M = 79.74, SD = 13.05 | Burnout (MBI) | |||||
|---|---|---|---|---|---|---|
| Exhaustion | Depersonalization | Accomplishment | ||||
| Burnout (MBI) | Exhaustion | Pearson’s r | −0.121 *** | — | ||
| M = 29.76 | Upper 95% CI | −0.060 | — | |||
| SD = 12.33 | Lower 95% CI | −0.182 | — | |||
| Depersonalization | Pearson’s r | −0.114 *** | 0.495 *** | — | ||
| M = 9.56 | Upper 95% CI | −0.053 | 0.540 | — | ||
| SD = 6.04 | Lower 95% CI | −0.175 | 0.447 | — | ||
| Accomplishment | Pearson’s r | 0.439 *** | −0.304 *** | −0.303 *** | — | |
| M = 37.57 | Upper 95% CI | 0.488 | −0.247 | −0.246 | — | |
| SD = 6.27 | Lower 95% CI | 0.388 | −0.359 | −0.358 | — | |
| Mental Health (GHQ-28) | Somatic symptoms | Pearson’s r | −0.090 ** | 0.571 *** | 0.239 *** | −0.162 *** |
| M = 10.83 | Upper 95% CI | −0.028 | 0.611 | 0.296 | −0.102 | |
| SD = 5.20 | Lower 95% CI | −0.150 | 0.528 | 0.180 | −0.222 | |
| Anxiety/insomnia | Pearson’s r | −0.122 *** | 0.617 *** | 0.285 *** | −0.166 *** | |
| M = 10.73 | Upper 95% CI | −0.061 | 0.654 | 0.340 | −0.105 | |
| SD = 5.59 | Lower 95% CI | −0.182 | 0.578 | 0.227 | −0.225 | |
| Social dysfunction | Pearson’s r | −0.195 *** | 0.486 *** | 0.240 *** | −0.267 *** | |
| M = 8.70 | Upper 95% CI | −0.135 | 0.531 | 0.297 | −0.209 | |
| SD = 3.06 | Lower 95% CI | −0.254 | 0.437 | 0.181 | −0.324 | |
| Depression | Pearson’s r | −0.289 *** | 0.402 *** | 0.242 *** | −0.255 *** | |
| M = 2.40 | Upper 95% CI | −0.231 | 0.452 | 0.300 | −0.196 | |
| SD = 3.61 | Lower 95% CI | −0.344 | 0.349 | 0.184 | −0.312 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suazo Galdames, I.; Molero Jurado, M.d.M.; Fernández Martínez, E.; Pérez-Fuentes, M.d.C.; Gázquez Linares, J.J. Resilience, Burnout and Mental Health in Nurses: A Latent Mediation Model. J. Clin. Med. 2024, 13, 2769. https://doi.org/10.3390/jcm13102769
Suazo Galdames I, Molero Jurado MdM, Fernández Martínez E, Pérez-Fuentes MdC, Gázquez Linares JJ. Resilience, Burnout and Mental Health in Nurses: A Latent Mediation Model. Journal of Clinical Medicine. 2024; 13(10):2769. https://doi.org/10.3390/jcm13102769
Chicago/Turabian StyleSuazo Galdames, Iván, María del Mar Molero Jurado, Elena Fernández Martínez, María del Carmen Pérez-Fuentes, and José Jesús Gázquez Linares. 2024. "Resilience, Burnout and Mental Health in Nurses: A Latent Mediation Model" Journal of Clinical Medicine 13, no. 10: 2769. https://doi.org/10.3390/jcm13102769
APA StyleSuazo Galdames, I., Molero Jurado, M. d. M., Fernández Martínez, E., Pérez-Fuentes, M. d. C., & Gázquez Linares, J. J. (2024). Resilience, Burnout and Mental Health in Nurses: A Latent Mediation Model. Journal of Clinical Medicine, 13(10), 2769. https://doi.org/10.3390/jcm13102769










