Exploring the Prognostic Performance of MECKI Score in Heart Failure Patients with Non-Valvular Atrial Fibrillation Treated with Edoxaban
Abstract
1. Introduction
2. Materials and Methods
2.1. Cardiopulmonary Exercise Test and Echocardiography
2.2. Anticoagulation Therapy
2.3. Statistical Analysis
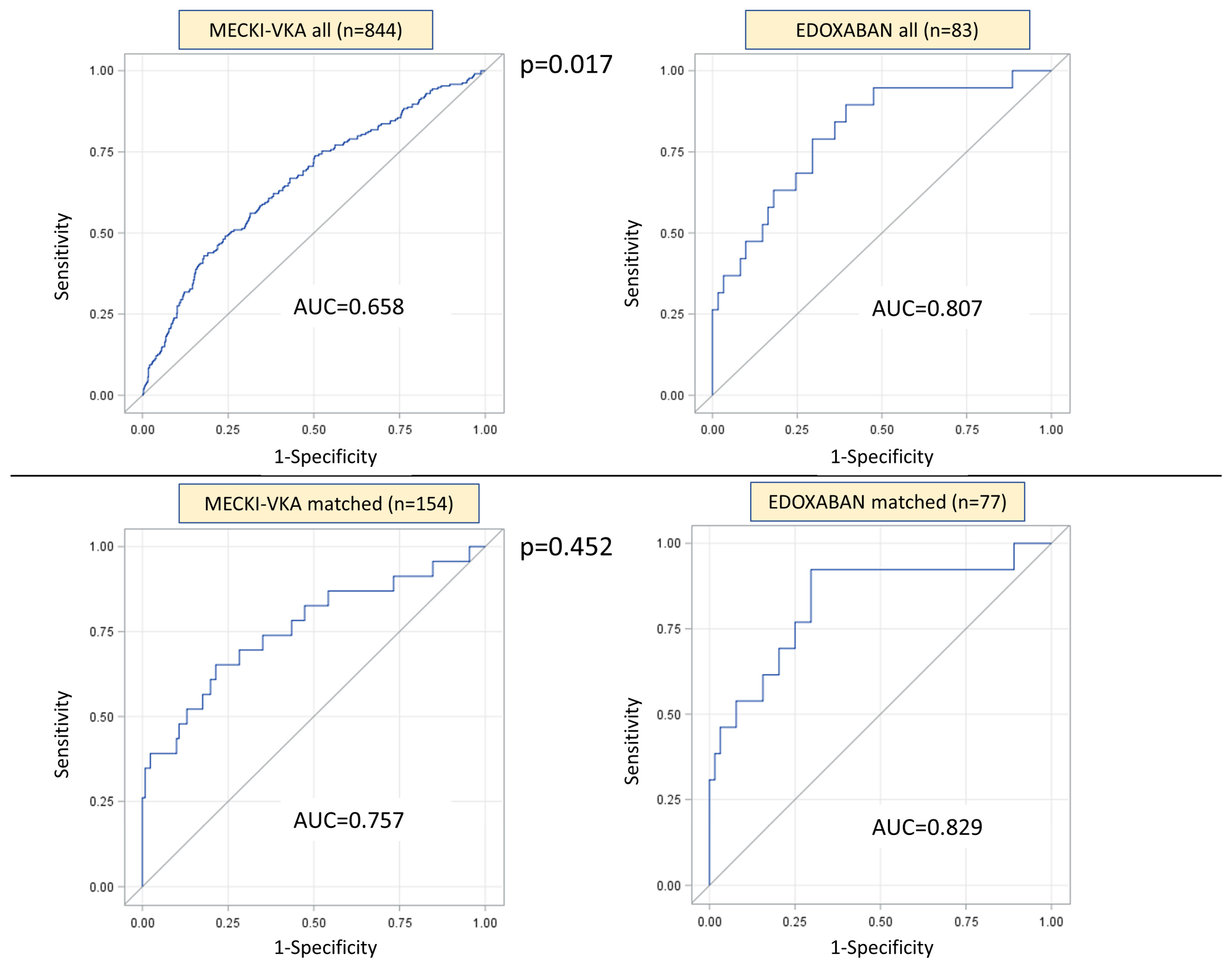
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
- Centro Cardiologico Monzino, IRCCS, Milan, Italy: Stefania Farina, Beatrice Pezzuto, Anna Apostolo, Pietro Palermo, Mauro Contini, Paola Gugliandolo, Umberto Attanasio
- Department of Clinical and Molecular Medicine, Azienda Ospedaliera Sant’Andrea, “Sapienza” Università degli Studi di Roma, Roma, Italy: Giovanna Gallo
- Dipartimento di Scienze Cardiovascolari, Respiratorie, Nefrologiche, Anestesiologiche e Geriatriche, “Sapienza”, Rome University, Rome, Italy: Federica Moscucci
- Department of Cardiology, Heart Failure and Heart Transplant Unit, Azienda Ospedaliera Papa Giovanni XXIII, Bergamo, Italy: Anita Iorio
- UOC Cardiologia, G da Saliceto Hospital, Piacenza, Italy: Geza Halasz, Bruno Capelli, Simone Binno
- Cardiologia SUN, Ospedale Monaldi (Azienda dei Colli), Seconda Università di Napoli, Napoli: Giuseppe Pacileo, Fabio Valente, Rossella Vastarella
- Cardiovascular Department, Ospedali Riuniti and University of Trieste, Trieste, Italy: Denise Zaffalon, Cosimo Carriere, Marco Masè, Marco Cittar, Andrea Di Lenarda; Maddalena Rossi; Emanuele Pestrin
- Istituto Auxologico Italiano, Milan, Italy: Sergio Caravita, Elena Viganò
- Cardiac Rehabilitation Unit, Istituti Clinici Scientifici Maugeri, Scientific Institute of Milan, Milan, Italy: Giovanni Marchese
- Cardiology Division, Santo Spirito Hospital, Roma, Italy: Roberto Ricci, Luca Arcari
- Division of Cardiology, Istituti Clinici Scientifici Maugeri, Institute of Cassano Murge, Bari, Italy: Domenico Scrutinio
- U.O. Cardiologia, S. Chiara Hospital, Trento, Italy: Elisa Battaia, Michele Moretti
- Ospedali Riuniti, Ancona, Italy: Maria Vittoria Matassini; Matilda Shkoza
- UOSD di Cardiologia/UTIC dell’IRCCS Neurolesi di Messina: Roland Herberg
- Federico II hospital, Napoli, Italy: Antonio Cittadini, Andrea Salzano, Alberto Marra
- ISMETT, Palermo, Italy: Eluisa Lafranca
- Cardiovascular Rehabilitation Unit, Buccheri La Ferla Fatebenefratelli Hospital, Palermo, Italy: Giuseppe Vitale
- Clinica Hildebrand Centro di riabilitazione Brissago, Switzerland: Davide Girola
References
- Gitt, A.K.; Wasserman, K.; Kilkowski, C.; Kleemann, T.; Kilkowski, A.; Bangert, M.; Schneider, S.; Schwarz, A.; Senges, J. Exercise anaerobic threshold and ventilatory efficiency identify heart failure patients for high risk of early death. Circulation 2002, 106, 3079–3084. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Bohm, M.; Burri, H.; Butler, J.; Celutkiene, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Agostoni, P.; Corra, U.; Cattadori, G.; Veglia, F.; La Gioia, R.; Scardovi, A.B.; Emdin, M.; Metra, M.; Sinagra, G.; Limongelli, G.; et al. Metabolic exercise test data combined with cardiac and kidney indexes, the MECKI score: A multiparametric approach to heart failure prognosis. Int. J. Cardiol. 2013, 167, 2710–2718. [Google Scholar] [CrossRef] [PubMed]
- Maisel, W.H.; Stevenson, L.W. Atrial fibrillation in heart failure: Epidemiology, pathophysiology, and rationale for therapy. Am. J. Cardiol. 2003, 91, 2D–8D. [Google Scholar] [CrossRef] [PubMed]
- Nieuwlaat, R.; Eurlings, L.W.; Cleland, J.G.; Cobbe, S.M.; Vardas, P.E.; Capucci, A.; Lopez-Sendon, J.L.; Meeder, J.G.; Pinto, Y.M.; Crijns, H.J. Atrial fibrillation and heart failure in cardiology practice: Reciprocal impact and combined management from the perspective of atrial fibrillation: Results of the Euro Heart Survey on atrial fibrillation. J. Am. Coll. Cardiol. 2009, 53, 1690–1698. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Corra, U.; Agostoni, P.G.; Belardinelli, R.; Cohen-Solal, A.; Hambrecht, R.; Vanhees, L. Statement on cardiopulmonary exercise testing in chronic heart failure due to left ventricular dysfunction: Recommendations for performance and interpretation Part II: How to perform cardiopulmonary exercise testing in chronic heart failure. Eur. J. Cardiovasc. Prev. Rehabil. 2006, 13, 300–311. [Google Scholar] [PubMed]
- Agostoni, P.; Bianchi, M.; Moraschi, A.; Palermo, P.; Cattadori, G.; La Gioia, R.; Bussotti, M.; Wasserman, K. Work-rate affects cardiopulmonary exercise test results in heart failure. Eur. J. Heart Fail. 2005, 7, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Hansen, J.E.; Sue, D.Y.; Wasserman, K. Predicted values for clinical exercise testing. Am. Rev. Respir. Dis. 1984, 129, S49–S55. [Google Scholar] [CrossRef] [PubMed]
- Agostoni, P.; Dumitrescu, D. How to perform and report a cardiopulmonary exercise test in patients with chronic heart failure. Int. J. Cardiol. 2019, 288, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Salvioni, E.; Corra, U.; Piepoli, M.; Rovai, S.; Correale, M.; Paolillo, S.; Pasquali, M.; Magri, D.; Vitale, G.; Fusini, L.; et al. Gender and age normalization and ventilation efficiency during exercise in heart failure with reduced ejection fraction. ESC Heart Fail. 2020, 7, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Bierig, M.; Devereux, R.B.; Flachskampf, F.A.; Foster, E.; Pellikka, P.A.; Picard, M.H.; Roman, M.J.; Seward, J.; Shanewise, J.; et al. Recommendations for chamber quantification. Eur. J. Echocardiogr. 2006, 7, 79–108. [Google Scholar] [CrossRef] [PubMed]
- January, C.T.; Wann, L.S.; Calkins, H.; Chen, L.Y.; Cigarroa, J.E.; Cleveland, J.C., Jr.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; Furie, K.L.; et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation 2019, 140, e125–e151. [Google Scholar] [CrossRef] [PubMed]
- Zafrir, B.; Lund, L.H.; Laroche, C.; Ruschitzka, F.; Crespo-Leiro, M.G.; Coats, A.J.S.; Anker, S.D.; Filippatos, G.; Seferovic, P.M.; Maggioni, A.P.; et al. Prognostic implications of atrial fibrillation in heart failure with reduced, mid-range, and preserved ejection fraction: A report from 14,964 patients in the European Society of Cardiology Heart Failure Long-Term Registry. Eur. Heart J. 2018, 39, 4277–4284. [Google Scholar] [CrossRef] [PubMed]
- Paolillo, S.; Agostoni, P.; Masarone, D.; Corra, U.; Passino, C.; Scrutinio, D.; Correale, M.; Cattadori, G.; Metra, M.; Girola, D.; et al. Prognostic role of atrial fibrillation in patients affected by chronic heart failure. Data from the MECKI score research group. Eur. J. Intern. Med. 2015, 26, 515–520. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chugh, S.S.; Blackshear, J.L.; Shen, W.K.; Hammill, S.C.; Gersh, B.J. Epidemiology and natural history of atrial fibrillation: Clinical implications. J. Am. Coll. Cardiol. 2001, 37, 371–378. [Google Scholar] [CrossRef]
- Giugliano, R.P.; Ruff, C.T.; Braunwald, E.; Murphy, S.A.; Wiviott, S.D.; Halperin, J.L.; Waldo, A.L.; Ezekowitz, M.D.; Weitz, J.I.; Spinar, J.; et al. Edoxaban versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2013, 369, 2093–2104. [Google Scholar] [CrossRef] [PubMed]
- Ruff, C.T.; Giugliano, R.P.; Braunwald, E.; Hoffman, E.B.; Deenadayalu, N.; Ezekowitz, M.D.; Camm, A.J.; Weitz, J.I.; Lewis, B.S.; Parkhomenko, A.; et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: A meta-analysis of randomised trials. Lancet 2014, 383, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Connolly, S.J.; Ezekowitz, M.D.; Yusuf, S.; Eikelboom, J.; Oldgren, J.; Parekh, A.; Pogue, J.; Reilly, P.A.; Themeles, E.; Varrone, J.; et al. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2009, 361, 1139–1151. [Google Scholar] [CrossRef] [PubMed]
- Agostoni, P.; Pluchinotta, F.R.; Salvioni, E.; Mapelli, M.; Galotta, A.; Bonomi, A.; Magri, D.; Perna, E.; Paolillo, S.; Corra, U.; et al. Heart failure patients with improved ejection fraction: Insights from the MECKI score database. Eur. J. Heart Fail. 2023. [Google Scholar] [CrossRef] [PubMed]
- Pezzuto, B.; Piepoli, M.; Galotta, A.; Sciomer, S.; Zaffalon, D.; Filomena, D.; Vignati, C.; Contini, M.; Alimento, M.; Baracchini, N.; et al. The importance of re-evaluating the risk score in heart failure patients: An analysis from the Metabolic Exercise Cardiac Kidney Indexes (MECKI) score database. Int. J. Cardiol. 2023, 376, 90–96. [Google Scholar] [CrossRef] [PubMed]

| Pre-Match | 2:1 Propensity Score Matching | |||||
|---|---|---|---|---|---|---|
| Variable | MECKI-VKA Total (n = 844) | Edoxaban (n = 83) | p-Value | MECKI-VKA Matched (n = 154) | Edoxaban Matched (n = 77) | p-Value |
| Ischemic etiology (n %) | 316 (38.3%) | 36 (45.6%) | 0.20574 | 66 (43%) | 35 (46%) | 0.707 |
| Females (n %) | 144 (17.1%) | 10 (11.9%) | 0.226 | 17 (11%) | 8 (10%) | 0.881 |
| Males (n %) | 700 (82.9%) | 74 (88.1%) | 137 (89%) | 69 (90%) | ||
| Age (years) | 69 (61;76) | 73.5 (66.5;80) | 0.0001 | 71 (64;78) | 72 (65;80) | 0.491 |
| BMI (kg/m2) | 26.58 (24.09;29.63) | 25.97 (24.18;29.18) | 0.562 | 27.26 ± 4.06 | 26.84 ± 3.93 | 0.460 |
| LVEF (%) | 34.14 ± 10.74 | 34.23 ± 10.26 | 0.941 | 33.3 ± 10.1 | 33.9 ± 9.9 | 0.703 |
| Hemoglobin (m/dL) | 13.47 ± 1.76 | 13.75 ± 2.02 | 0.168 | 13.8 ± 1.8 | 13.8 ± 2.0 | 0.878 |
| Creatinine (mg/dL) | 1.19 (0.98;1.50) | 1.29 (1.04;1.61) | 0.012 | 1.25 (1.03;1.6) | 1.28 (1.04;1.58) | 0.795 |
| MDRD (mL/min/1.73 m2) | 63.5 (47.7;79.2) | 57.5 (43.86;70.03) | 0.0140 | 58.8 (45.0;74.1) | 58.1 (44.8;71.6) | 0.804 |
| Na+ (mmol/L) | 139.22 ± 3.53 | 140.18 ± 3.14 | 0.0171 | 140.2 ± 3.3 | 140.1 ± 3.1 | 0.779 |
| Peak VO2 (mL/min) | 989 (743.2;1223.8) | 1081 (862;1318) | 0.031 | 1018 (791;1260) | 1081 (862;1385) | 0.458 |
| Peak VO2 (mL/min/kg) | 12.30 (10;15.13) | 14.1 (10.9;15.8) | 0.035 | 13.2 (10.2;16.0) | 14.1 (10.9;15.9) | 0.369 |
| Peak VO2 (% pred) | 50.42 (40.81;62.13) | 57.35 (45.7;64.03) | 0.009 | 55.65 ± 18.18 | 56.07 ± 14.32 | 0.858 |
| VE/VCO2 slope | 34 (29;40) | 38.3 (33.9;43.8) | <0.0001 | 37.32 (32;45) | 38.0 (33.5;43.4) | 0.517 |
| VE/VCO2 slope (% pred) | 127 (110;149) | 143 (126;159) | <0.0001 | 137 (119;168) | 142 (125;157) | 0.5303 |
| ACE Inhibitors (n %) | 531 (62.9%) | 18(22.5%) | <0.0001 | 94 (61%) | 18 (23.4%) | <0.0001 |
| AT1 inhibitors (n %) | 182 (21.9%) | 5 (6.3%) | <0.001 | 33 (21.7%) | 5 (6.5%) | 0.003 |
| Allopurinol (n %) | 276 (32.7%) | 22 (27.5%) | 0.342 | 58 (37.7%) | 21 (27.3%) | 0.117 |
| Amiodarone (n %) | 253 (30.8%) | 49 (61.3%) | <0.0001 | 39 (25.8%) | 47 (61%) | <0.0001 |
| Antiplatelets (n %) | 159 (18.8%) | 35 (43.8%) | <0.0001 | 29 (18.8%) | 34 (44.2%) | <0.0001 |
| Betablockers (n %) | 708 (83.9%) | 70 (87.5%) | 0.397 | 126 (81.8%) | 68 (88.3%) | 0.205 |
| Digitalis (n %) | 317 (38.2%) | 8 (10%) | <0.0001 | 63 (41.4%) | 8 (10.4%) | <0.0001 |
| Diuretics (n %) | 757 (89.7%) | 71 (88.8%) | 0.782 | 141 (91.6%) | 68 (88.3%) | 0.428 |
| Sacubitril/Valsartan (n %) | 26 (3.1%) | 52 (61.9%) | <0.0001 | 4 (2.6%) | 50 (64.9%) | <0.0001 |
| MRA (n %) | 537 (63.6%) | 57 (71.3%) | 0.174 | 103 (66.9%) | 55 (71.4%) | 0.484 |
| Statin | 332 (39.3%) | 48 (60%) | <0.0001 | 71 (46.1%) | 46 (59.7%) | 0.484 |
| Follow-up (days) | 1428.5 (566;2614) | 818 (588.5;1070) | <0.0001 | 1181.5 (545;2312) | 825 (585;1083) | 0.001 |
| MECKI score | 0.068 (0.026;0.15) | 0.066 (0.029;0.175) | 0.606 | 0.08 (0.03;0.17) | 0.06 (0.03;0.17) | 0.7981 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mapelli, M.; Mattavelli, I.; Salvioni, E.; Capra, N.; Bonomi, A.; Cattadori, G.; Pezzuto, B.; Campodonico, J.; Piotti, A.; Nava, A.; et al. Exploring the Prognostic Performance of MECKI Score in Heart Failure Patients with Non-Valvular Atrial Fibrillation Treated with Edoxaban. J. Clin. Med. 2024, 13, 94. https://doi.org/10.3390/jcm13010094
Mapelli M, Mattavelli I, Salvioni E, Capra N, Bonomi A, Cattadori G, Pezzuto B, Campodonico J, Piotti A, Nava A, et al. Exploring the Prognostic Performance of MECKI Score in Heart Failure Patients with Non-Valvular Atrial Fibrillation Treated with Edoxaban. Journal of Clinical Medicine. 2024; 13(1):94. https://doi.org/10.3390/jcm13010094
Chicago/Turabian StyleMapelli, Massimo, Irene Mattavelli, Elisabetta Salvioni, Nicolò Capra, Alice Bonomi, Gaia Cattadori, Beatrice Pezzuto, Jeness Campodonico, Arianna Piotti, Alessandro Nava, and et al. 2024. "Exploring the Prognostic Performance of MECKI Score in Heart Failure Patients with Non-Valvular Atrial Fibrillation Treated with Edoxaban" Journal of Clinical Medicine 13, no. 1: 94. https://doi.org/10.3390/jcm13010094
APA StyleMapelli, M., Mattavelli, I., Salvioni, E., Capra, N., Bonomi, A., Cattadori, G., Pezzuto, B., Campodonico, J., Piotti, A., Nava, A., Piepoli, M., Magrì, D., Paolillo, S., Corrà, U., Raimondo, R., Lagioia, R., Vignati, C., Badagliacca, R., Perrone Filardi, P., ... Agostoni, P., on behalf of MECKI Score Research Group. (2024). Exploring the Prognostic Performance of MECKI Score in Heart Failure Patients with Non-Valvular Atrial Fibrillation Treated with Edoxaban. Journal of Clinical Medicine, 13(1), 94. https://doi.org/10.3390/jcm13010094










