Abstract
(1) Background: Severely compromised teeth affected by endo-periodontal lesions are often assigned a “hopeless” prognosis, however, there is only limited evidence available. (2) Methods: In a retrospective study, we evaluated the long-term effectiveness of combined endodontic and regenerative periodontal therapy in teeth with advanced endo-periodontal lesions: 35 patients (age 47–83 years) with a total of 39 teeth diagnosed with grade 3 endo-periodontal lesions were treated by endodontists using an operating microscope followed by regenerative periodontal surgery. (3) Results: Changes in radiographic bone levels (rBl) and probing pocket depths (PPDs) were evaluated after 1 year (T1) and up to 7 years postoperatively (Tfinal). Mean rBL gain was significant with 4.87 ± 3.47 mm after 1 year (T1) and stable results with a mean rBL gain of 4.70 ± 3.37 mm at Tfinal. Mean PPD was significantly reduced from 9.74 ± 2.05 mm at baseline to 5.04 ± 1.61 mm at T1 and to 4.87 ± 2.32 mm at Tfinal. Tooth loss amounted to 10.3% (n = 4) and was due to root fracture. (4) Conclusion: The results suggest that the combined endodontic and regenerative periodontal therapy of endo-periodontal lesions of “hopeless” teeth can lead to favorable long-term results with tooth retention for up to 7 years.
1. Introduction
Endo-periodontal lesions are defined as “pathologic communication between pulp and periodontal tissues” of a particular tooth appearing in acute or chronic form. They are specified regarding signs and symptoms with a direct impact on prognosis and therapy [1].
Typical signs of an endo-periodontal lesion are deep probing pocket depths extending to the apex of the tooth and altered signs of the pulp vitality. In addition, further signs and symptoms such as radiographic bone loss extending to the apical region of the tooth and furcation involvement, sensitivity to palpation/percussion, increased tooth mobility, bleeding on probing and/or pus suppuration can be apparent [1].
According to the “2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions” they are classified into endo-periodontal lesions with root damage—such as root fracture, perforation of a root canal, root resorption—or without root damage. Endo-periodontal lesions without root damage are further subdivided with regard to periodontitis and non-periodontitis patients as well as three grades of severity [1,2]. Based on this new classification, endo-periodontal lesions have a prevalence of 4.9% [3].
Teeth diagnosed with advanced endo-periodontal lesions are often considered “hopeless” and extracted without any treatment effort and replaced by an implant supported restoration. In light of the increasing prevalence of peri-implant disease, tooth extraction should not be considered as the first treatment option. Instead, tooth retention even for periodontally compromised teeth should be considered as the first treatment choice [4,5,6,7].
There is a common consensus in the recent literature that root canal treatment in teeth affected by endo-periodontal lesions should be performed first [8,9,10]. However, sole endodontic treatment has failed to prove as a highly predictable therapy for teeth affected by endo-periodontal lesions [10]. Therefore, additional periodontal therapy is indicated, in particular, regenerative procedures for grade 3 endo-periodontal lesions presenting with deep periodontal pockets at more than one tooth surface to enhance the outcome and prognosis. The time-lapse between endodontic and regenerative periodontal treatment did not show to have any effect on the healing of endo-periodontal lesions [11,12]. While the value of regenerative therapy in intra-bony defects is well known [6,13,14,15,16,17], only limited data exist on the outcomes of periodontal regenerative treatment of teeth severely compromised by endo-periodontal lesions. So far, there are only a few case reports and series [18,19,20,21] showing favorable results for this combined endodontic and periodontal therapy. Two randomized controlled clinical trials have reported that concomitant regenerative periodontal surgery enhanced the outcomes and success rate after 1 year [12,22]. A 5-year survival rate of 92.31% has been reported in a retrospective study for teeth with endo-periodontal lesions after periodontal regenerative procedures [23].
The aim of this retrospective study was to gain more evidence by evaluating the long-term effectiveness of endodontic treatment followed by regenerative periodontal surgery in teeth with advanced endo-periodontal lesions.
2. Materials and Methods
2.1. Study Design and Patients
This retrospective study was performed in a periodontal specialty practice (CT) in Aachen and the Department of Periodontology, Operative and Preventive Dentistry (KJ), University of Bonn, Germany. The study was conducted in accordance with the Helsinki Declaration (version 2008) and approved by the Ethics committee of the University of Bonn (#51/22).
Patients were selected during the period from April 2013 to September 2022 if presenting with a grade 3 endo-periodontal lesion according to the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions [1]. They were consecutively treated by endodontic specialists under an operating microscope followed by regenerative periodontal surgery using deproteinized bovine bone mineral with/without collagen membrane and/or enamel matrix derivative. Data of these patients were available for a retrospective analysis of the outcomes of this combined treatment. Patients had given their written informed consent for a retrospective evaluation of their clinical and radiographic data.
Inclusion criteria for the analysis were as follows:
- Grade 3 endo-periodontal lesion;
- Endodontic treatment was performed first and followed by periodontal regenerative surgery;
- One- or two-wall intra-bony defects suitable for periodontal regenerative surgery;
- Adequate oral hygiene and control of inflammation: full-mouth plaque score (FMPS) of ≤20% and full-mouth bleeding score (FMBS) of ≤20%;
- Clinical and radiographic data of a consecutive follow-up of at least 1 year after regenerative therapy.
- Exclusion criteria for the analysis were as follows:
- Non-compliance;
- Incomplete probing or radiographic data;
- Heavy smokers > 10 cigarettes per day;
- Resective periodontal surgery on target tooth;
- Teeth with fractures, external or internal resorption;
- Additional periodontal or maxillofacial treatment in the areas of interest;
- Systemic diseases (e.g., uncontrolled diabetes).
Patients with systemic diseases (i.e., controlled diabetes) were not excluded. Based on the criteria above, 35 patients with a total of 39 endo-periodontal lesions were included in the analysis. All patients were periodontitis patients except for 2 patients. Patient and defect characteristics are depicted in Table 1.

Table 1.
Patient demographic and defect characteristics at baseline (T0).
2.2. Treatment
2.2.1. Endodontic Therapy
All endodontic treatments were performed under local anesthesia and sterile conditions by application of rubber dam by three different endodontic specialists (EY, Bonn; PD, Aachen; VK, Aachen). Instrumentation was performed by hand and rotary files (Reciproc®, VDW GmbH, Munich, Germany) using a surgical operating microscope (ProErgo, Carl-Zeiss AG, Jena, Germany). All root canals were irrigated intermittently with sodium chloride solution (NaCl) as well as 3% sodium hypochloride solution (NaOCl). At the end of the first appointment, calcium hydroxide paste was applied into all canals. In a second appointment, at least 2 weeks later, obturation of all root canals was achieved either by thermoplastic filling or lateral condensation techniques using gutta-percha. The cavity was sealed with a resin-bonded composite material. Periapical radiographs were taken prior, during and after completion of the endodontic treatment.
2.2.2. Regenerative Periodontal Surgery
Regenerative periodontal therapy of the selected areas was performed after a mean re-evaluation time of three months after endodontic treatment by two periodontists (CT, Aachen and KJ, Bonn) if the lesion still persisted.
Following administration of local block and infiltration anesthesia, a minimally invasive microsurgical approach for incisions and flap was chosen as previously described [14]. For optimal wound stability and to maintain better blood supply of the flap, vertical releasing incisions were avoided by extending flap design to adjacent teeth.
Apical split flap preparation was only performed if needed for primary tension-free flap closure. After meticulous debridement of the defect with curettes, sonic/ultrasonic devices the biomaterial was selected depending on the configuration of the intra-bony defect [6,13,26]. To avoid a soft-tissue collapse into the defect, a bone filler was used (DBBMc, Bio Oss® Collagen; Geistlich, Wolhusen, Switzerland). If the graft material was at risk for dislocation in non-contained defects, a collagen membrane (Bio Gide®Perio; Geistlich, Wolhusen, Switzerland) was applied without pin or suture fixation. Enamel matrix derivative (EMD, Emdogain®; Straumann, Basel, Switzerland) was applied in contained defects after debridement as an adjunct to the root surface. To achieve primary tension-free closure of the coronally positioned flap, modified horizontal mattress sutures and additional single interrupted sutures for papilla adaptation (Premilene® USP6/0-DS13, B. Braun, Tuttlingen, Germany; Seralene® USP6/0-DS12 SeragWiessner, Naila, Germany; Seralene®USP6/0-DS15; SeragWiessner, Naila, Germany) were used.
Postoperatively, a strict anti-infective protocol was enforced instructing the patient to rinse with 0.12% chlorhexidine solution three times a day and to refrain from mechanical tooth cleaning in the surgically treated areas for 2 weeks or until complete wound healing.
Sutures were removed after 10–14 days depending on individual wound healing progression. In the case of advanced tooth mobility > grade I (Miller, 1938) [27], a removable acrylic splint was inserted after surgery to provide wound stability of the regeneratively treated site.
2.2.3. Supportive Periodontal Therapy
Following periodontal surgery, supportive periodontal therapy started with a strict interval of 4 weeks up to 3 months. Control of inflammation was accomplished by cautious professional tooth cleaning and oral hygiene reinforcement according to the individual patient needs with an average of three times per year.
2.3. Clinical and Radiographic Assessments
Periodontal measurements for all 39 lesions were taken at baseline (T0) before periodontal regenerative surgery with a mean observation time of 3.9 months after endodontic therapy, after 1 year (T1) and every year during supportive care up to the 7-year follow-up visit (Tfinal) using a periodontal probe (PCP11; Hu-Friedy) (Figure 1):
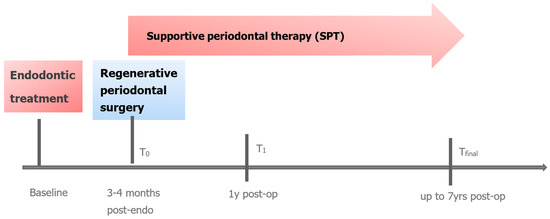
Figure 1.
Chronical sequence of treatment and examinations (T0 = baseline, T1 = 1 year, Tfinal,).
- Probing pocket depth (PPD) at 6 sites per tooth;
- Full-mouth plaque scores (FMPS), Full mouth bleeding scores (FMBS);
- Horizontal furcation class (0-III) (Hamp et al., 1975) [24] and vertical furcation subclasses A, B, C (Tarnow and Fletcher, 1984) [25];
- Tooth mobility (Miller, 1938) [27].
The tooth site with the most advanced bone loss mesially or distally (distance between the cemento-enamel junction or restoration to the bottom of the defect) as measured during surgery became the target site. Intra-operative BL was used for calibration of the pre-operative periapical radiograph by using the overall tooth length as a reference length, as previously described [14]. All radiographs were analyzed using ImageJ Software (Version 1.43u, National Institutes of Health, Bethesda, MD, USA) by a trained and calibrated examiner (IT) who was not involved in the surgeries.
2.4. Statistical Analysis
Change of radiographic bone level (rBL) was the primary outcome parameter, whereas change in PPD and frequency of pocket closure (sites with PPD ≤ 4 mm) served as secondary outcomes. Descriptive analysis was outlined for radiographic bone level (rBL) and pocket probing depth (PPD) with change over time at three time points T0, T1, Tfinal using means and standard deviations per tooth.
The comparisons of radiographic bone level between time points were performed with a Wilcoxon signed-rank test. To take into account a possible clustering on patient level, a Wilcoxon signed-rank test for clustered data (Rosner et al., 2006) [28] was used with the method developed by Datta and Satten (2008) [29].
To compare the proportion of pocket closures between time points, a logistic regression with time as the fixed effect and tooth-id and, if necessary, patient as the random effect was run. The p-values for the comparison with pocket closure at baseline were adjusted with an approximation of the Dunnet-correction, while for the pairwise comparison between all three time points, a Tukey correction was used.
Although the data was of two level-nature (patient–tooth), only a few patients (n = 3) had in fact more than one tooth in this study. Hence, to investigate the impact of BOP, FMPS and smoking on RBL and PPD, a two-level model with patient as random factor was used if indicated. In all other cases, the random factor was dropped and a linear regression was used instead.
The effect of occlusal wear on tooth loss was investigated by running a logistic regression on tooth loss with occlusal wear as a factor. Adding patient as a random factor resulted in a near-singular fit due to the near zero variation within patient; however, both models showed the same estimates. Level of significance was set for p < 0.05.
Statistical analyses of the clinical and radiographic data were performed by an independent expert biostatistician with the statistical software R, version 4.1.3 (R Core Team, 2022) [30].
3. Results
3.1. Patient and Defect Characteristics
A total of 35 patients (Aachen, 28 patients; Bonn, 7 patients) with 39 teeth diagnosed with an endo-periodontal lesion were included in the study. All patients showed a history of periodontitis except for two patients. Three patients contributed more than one treated lesion. In total, 24 teeth were molars including 18 molars (11 mandibular and 7 maxillary molars) presenting with horizontal furcation class I (n = 4), class II (n = 13) and class III (n = 1) (Hamp et al., 1975) [24]. According to the vertical subclassification of molars with class I-III furcation (Tarnow and Fletcher, 1984) [25], there were 2 molars presenting with subclass A, 3 with subclass B and 13 with subclass C. Six molars did not show any furcation involvement (Table 1).
For all 39 teeth treated by the combined therapy of endodontic treatment and regenerative periodontal surgery, data were available 1 year postoperatively (T1). Data of a longer follow-up of up to 7 years (Tfinal) with a mean observation time of 31.4 months-could be obtained for 23 teeth in 23 patients.
All of the patients showed full adherence to supportive care during the observation period. At baseline, the mean radiographic bone level was 12.54 ± 3.63 mm with a mean PPD of 9.21 ± 2.15 mm. For the 23 teeth with complete follow-up data, the baseline values were a mean rBL of 13.09 ± 3.12 mm with a mean PPD of 9.74 ± 2.05 mm (Table 1 and Table 2a–c).

Table 2.
(a) Mean radiographic bone level (rBL) ± standard deviation (mm) at different time points. (b) p-values for testing rBL between time different points (statistics Wilcoxon signed-rank test from the R-library coin version 1.3.1 (Hothorn et al., 2008)) [31]. (c) Mean probing pocket depth (PPF) ± standard deviation (mm) at different time points. (d) Frequency distribution of residual PPD. (e) p-values for testing proportion of pocket closure (pc) between time points corrected for multiple testing (Tukey test).
3.2. Outcomes
Surgeries and soft tissue healing were generally uneventful with none of the patients developing any major complications or allergic reactions, suppuration or abscesses. Minor complications such as postoperative swelling and pain in the surgically treated area resolved within a few days after surgery.
Two representative examples of teeth affected by advanced endo-periodontal lesions that were included in the present analysis are illustrated in Figure 2 and Figure 3.
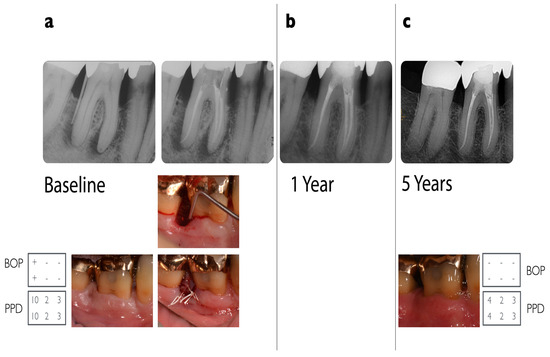
Figure 2.
Radiographic and clinical situation of a lower right molar (#46) in a 55-year-old otherwise healthy patient. Five-year follow-up of a grade 3 endo-periodontal lesion treated with combined endodontic and regenerative periodontal therapy. (a) The patient came for his regular 3-monthly re-evaluation visit for his periodontitis stage III. Deep probing depths at tooth #46 distal of 10 mm (visualized by a gutta-percha point) not evident at his last visit. The furcation was not involved. Radiograph with evidence of extensive vertical and peri-apical bone loss. Pulp sensitivity testing was negative when exposed to chlorethylene and to electric (Vitality Scanner™) scanning. Root canal treatment was performed under an operating microscope. For the regenerative procedure, a papilla preservation flap technique was performed, using DBBM (BioOss-Collagen®Geistlich) and EMD (Emdogain®, Straumann, Basel, Switzerland) as supportive materials. Healing was uneventful, and monofilic sutures (6/0) were used. (b) One-year follow-up with no evidence of radiographic pathologies. (c) Five-year follow-up after regenerative surgery: probing depths: 2–4 mm; recession: up to 3 mm, with a radiograph showing stable radiographic bone fill in the vertical defect area.
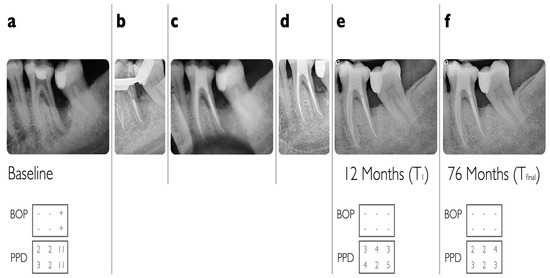
Figure 3.
(a) Radiographic situation of a lower left molar (#36) in a 47-year-old otherwise healthy patient; (b) endodontic treatment/downpack; (c) radiographic control immediately after endodontic treatment; (d) 3 months after endodontic treatment: radiographic improvement but still persisting deep probing pocket depths (food impaction visible); (e) at 12-month follow-up (T1); (f) at 76-month follow-up (Tfinal).
Radiographic bone level improved significantly from 12.54 ± 3.36 mm at baseline to 7.95 ± 2.65 mm after 1 year (p < 0.0001). Analysis of change in radiographic BL over time of 23 teeth with available data over all time points revealed a statistically significant mean gain in radiographic bone level of 4.8 ± 3.47 mm (p < 0.0001) at T1 and 4.70 ± 3.37 mm at Tfinal (p < 0.0001) (Figure 4a and Table 2a,b).
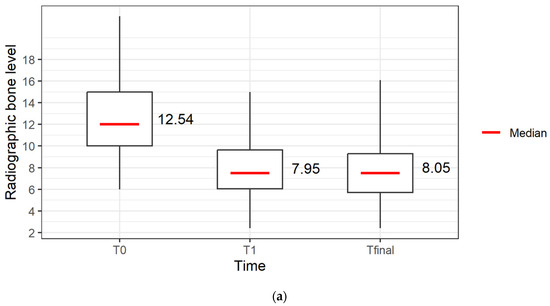
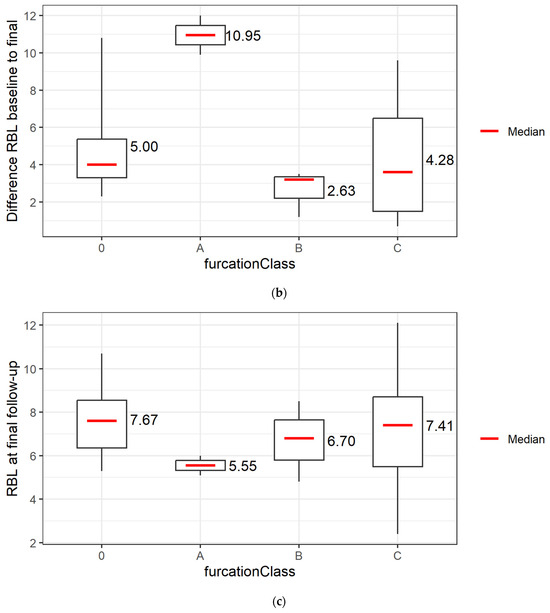
Figure 4.
(a) Radiographic bone level over time (T0 = baseline), 1 year after regenerative surgery (T1) and up to 7 years after regenerative therapy (Tfinal) of 39 teeth in 34 patients. (b) Radiographic bone level gain and (c) radiographic bone level at Tfinal of 24 molars in 23 patients without furcation involvement (n = 6) or vertical furcation subclasses A (n = 2), B (n = 3), C (n = 13) from T0 = baseline and of 21 molars in 20 patients up to 7 years after regenerative surgery (Tfinal) without furcation involvement (n = 6) or vertical furcation subclasses A (n = 6), B (n = 11), C (n = 0), and 3 molars lost due to root fracture.
Mean PPD was significantly reduced from 9.21 ± 2.15 mm at baseline to 5.21 ± 1.79 mm after 1 year. For 23 teeth with available data over all time points, a significant reduction of 4.70 ± 2.42 mm (p < 0.0001) at T1 was achieved and remained stable with 4.87 ± 2.93 mm at Tfinal (p < 0.0001) (Table 2c).
Pocket closure could be achieved in 34.8% after 1 year and 52.2% at Tfinal and was statistically significant (Table 2d,e).
Fourteen out of eighteen molars with horizontal furcation involvement showed an improvement by conversion to a lower furcation class, revealed by a decrease in the frequency of horizontal furcation class II of 54% at baseline to 13% and an increase in the frequency of furcation classes I and 0 to 46% and 42%, respectively, after 1 year. For molars (n = 16) with available data for all three time points, the horizontal furcation class remained stable from T1 to T (Table 3a).

Table 3.
(a,b). Horizontal and vertical furcation subclasses at different timepoints, conversion of horizontal and vertical furcation subclass.
If the 18 molars affected by horizontal furcation involvement were subdivided according to vertical furcation subclasses, the change in rBL at Tfinal showed a gain of 10.95 mm in vertical subclass A (n = 2, 11%), a gain of 2.63 mm in subclass B (n = 3, 17%) and a gain of 4.28 mm in subclass C (n = 13, 72%) with a final radiographic bone level of 5.55 mm in subclass A, 6.70 mm in subclass B and 7.41 mm in subclass C (Table 3b and Figure 4b,c).
Overall, 89% of the furcations showed improvement in vertical subclassification throughout the study period. All vertical subclasses C were resolved at T1, showing a conversion to subclass B (56%) or to subclass A (17%) and stable results at Tfinal (Table 3b).
A representative example of teeth affected by advanced endo-periodontal lesions with vertical subclass that were included in the present analysis is illustrated in Figure 5.
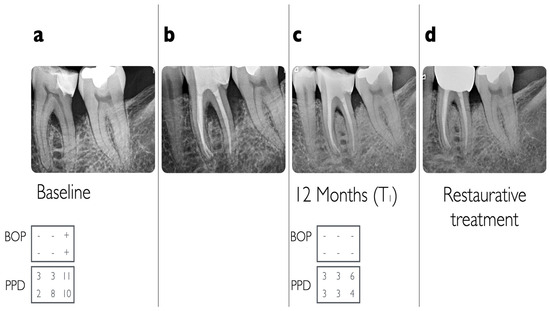
Figure 5.
(a) Baseline radiographic situation of a lower right molar (#36) with horizontal furcation involvement class III with vertical furcation subclass B component, (b) 3 months after endodontic treatment, (c) at 12-month follow-up (T1) with conversion to horizontal furcation class I, and (d) after restorative treatment.
No tooth loss was observed after one year, whereas at Tfinal tooth loss amounted to 10.3%, namely four teeth (one premolar and three molars) in three patients due to root fracture; three of them were in patients with bruxism. All three molars that were lost—two maxillary and one mandibular molar—had presented with vertical subclass C at the time of surgery, two of them with horizontal furcation class II and one with class I.
Due to the low proportion of teeth per patient, a multilevel analysis could only be run as a simple one-level regression model, demonstrating a slight impact of rBL at baseline on the outcomes, whereas smoking and BOP did not show any effect on the outcomes.
The results of the final model are presented as Table S1 in the Supplementary Materials.
4. Discussion
The data of this retrospective clinical cohort study reveal the long-term effectiveness of a combined endodontic and periodontal regenerative treatment in patients with advanced endo-periodontal lesions. Teeth diagnosed as “hopeless” due to advanced endo-periodontal lesions could be retained in 89% up to 7 years using the combination of endodontic and regenerative periodontal therapy. These findings are novel and of high clinical relevance.
The results of this investigation cannot be easily compared to previously published studies due to differences in study protocols with regard to regenerative procedures, performed endodontic treatment, baseline clinical severity, selection of outcome measures and length of follow-up.
A recent retrospective long-term study has shown that root canal treatment is a valid option for long-term tooth survival with 97% to 68% after 10 and up to 37 years [32]. However, the presence of endo-periodontal lesions with deep periodontal pockets ≥ 6 mm and the presence of periapical radiolucencies [32], as well as furcation involvement [1,33], seem to have a negative impact on long-term prognosis. Thus, the slightly lower retention rate of 89.7% for up to 7 years in our study on teeth with endo-periodontal lesions is probably due to the complexity of pre-existing risk factors such as furcation involvement and advanced bone destruction of the affected teeth [1,32,33]. Interestingly, the results are similar to the 92.3% tooth retention observed in a retrospective study on the combined treatment of endo-periodontal lesions after 5 years [23]. In that study, 45 out of 52 regeneratively treated teeth had received endodontic prior to regenerative periodontal treatment [23]. With regard to the mean radiographic bone level gain, the authors reported 1-year data. Their findings of a rBL gain of 5.30 mm and PPD reduction of 4.44 mm after 1 year (teeth with endodontic treatment in combination with bovine mineral with/without membrane) are similar to the outcomes of our study (4.87 mm of rBL gain and 4.7 mm PPD reduction).
The achieved bone level gain in the present study compares well to the outcomes of 3.9 mm mean bone level gain 1 year after regenerative surgery that remained stable for 10 years observed in a former study performed with a similar regenerative protocol in the same practice [14]. In contrast to the present study, however, no endo-periodontal lesions were included.
With regard to the complexity of defect morphology and severity of risk factors, three studies may serve for comparison for the retention of “hopeless” teeth, even though they did not focus specifically on endodontic-periodontal lesions [4,5,34]. Cortellini et al. (2011, 2020a) [4,5] in a prospective study reported 5- and 10-year follow-up data of teeth initially presenting with attachment loss to the apex that had been treated using regenerative periodontal surgery. In their study, 20 out of 25 teeth had been endodontically treated, 12 teeth associated with defects extending beyond the apex were endodontically treated as a prophylactic measure prior to surgery and eight teeth already presented with previous endodontic treatment. However, it has to be emphasized that one major difference to our study was that only teeth with clearly detectable peaks of bone/attachment on the adjacent teeth were included in these studies, thus enabling a higher radiographic bone level gain of 8.5 ± 3.1 mm in comparison to our outcomes of 4.87 ± 3.47 mm after 1 year in periodontitis patients. Moreover, the initial mean radiographic bone level (16.00 ± 2.3 mm) was greater than 13.09 ± 3.12 mm in our study and therefore adding to the possibility of a higher radiographic bone level gain. The same applies to the possibility of a higher PPD gain: mean PPD gain after 1 year with 4.31 mm (baseline PPD 9.74 mm with 4.87 mm at Tfinal) in our study was less than data in the named study with 8.7 mm. In addition, PPD at baseline (12.7 mm) in the study of Cortellini et al., 2011, 2020a [4,5], was much higher than in our study (9.74 mm), thus more favorable for a higher PPD gain. However, our findings of residual probing pocket depths (5.04 ± 1.61 mm after 1 year vs. 4.0 ± 1.7 mm) and tooth retention (89.7% after up to 7 years vs. 88% after 10 years) compare well with the results by Cortellini et al. (2011, 2020 a) [4,5].
A retrospective analysis evaluated the results of periodontal regeneration of 49 molars severely compromised by combined furcation and intra-bony defects [34]. Here, 10 molars had received prophylactic endodontic treatment prior to regenerative surgery. Besides the improvement in horizontal furcation involvement, furcation vertical subclassification improved 1 year after periodontal regenerative surgery in 87.5% (maxillary) and 84.6% (mandibular) of molars, respectively, which compares well to the observed 89% improvement in vertical furcation subclass in the present study. The same applies to the survival rate based on vertical subclassification: the findings of 100% at 1-year follow-up and 88% up to 7 years compare well to the reported survival rates ranging from 100% after 1 year and 95% after an average follow-up of 5.7 years in the study of Cortellini et al. (2020b) [34].
Previous studies have indicated [15,33] that the severity of furcation involvement and vertical subclassification seem to be an important predictor of tooth survival. A shift of a vertical subclass C or B to a subclass A or B can reduce premature extraction of teeth diagnosed with “hopeless prognosis” and prolonging the time of a more costly implant placement or tooth-supported fixed partial denture [5,33].
Therefore, the improvement in vertical subclasses, as shown in the present study by the elimination of subclass C and shift to subclass B (56%), respectively, and subclass A (17%) at T1 by regenerative surgery, indicates an increased periodontal support and thus a more favorable long-term prognosis. In addition, the improvement to horizontal furcation class I and 0 after 1 year (46% and 42%) and stable conditions for up to 7 years also add to a better long-term prognosis [15,35,36]. These findings—the improvement in bone level in different furcation subclasses in regeneratively treated molars with endo-periodontal lesions—are novel and of high clinical relevance.
Pocket closure could be achieved in 34.8% after 1 year and 52.17% at Tfinal. The rather low proportion of pocket closure is due to the severity of bone loss in teeth diagnosed with endo-periodontal lesions, and therefore, a PPD reduction of more than 50% can be considered a successful treatment in endo-periodontal lesions [10]. Tooth loss of 10.3%, due to root fracture as a consequence of compromised tooth structure and to occlusal wear (75%), is in agreement with the literature [32].
The gain in radiographic bone level and probing pocket depth reduction indicate that even severely compromised teeth diagnosed with endo-periodontal lesions can be retained for a long period of time by the treatment protocol presented in the present study.
The present study has strengths and limitations. Adding to the strengths, all patients were treated by the same two experienced surgeons, and postoperative data measurements and radiographs were evaluated by the same blinded examiner, who was not involved in the clinical evaluation. Data analysis was performed by an independent expert statistician. Furthermore, the study was accomplished independent from industrial support. However, the present study also has inherent limitations due to its retrospective character and the lack of a comparison group. Therefore, it has to be regarded as an extensive feasibility study that may be of great value for the design of future prospective randomized clinical trials.
In the future, well planned prospective randomized controlled clinical trials will further refine the most suitable protocol for the combined endodontic and regenerative periodontal treatment of severely compromised teeth with endo-periodontal lesions.
5. Conclusions
Within the limitations of the retrospective study design, the results of this study indicate that the combined therapy of endo-periodontal lesions of “hopeless” teeth with endodontic and regenerative periodontal therapy followed by a strict maintenance protocol can lead to favorable long-term results for tooth retention up to 7 years.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm13010093/s1. Table S1: Results from final model for the change of radiographic bone level from T0 to Tfinal.
Author Contributions
C.T. conceived the idea of the study, performed the surgeries, interpretation of the results and manuscript writing. K.J. performed the surgeries and contributed with S.J. to supervision, interpretation of the results and writing/revising of the manuscript. I.T. collected and analyzed the data. E.Y. performed the endodontic treatments in Bonn. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee, University of Bonn (#51/22 on 7 February 2022).
Informed Consent Statement
Written informed consent has been obtained from all participating patients involved in the study and to publish this paper.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon request.
Acknowledgments
We thank Peter Dolezel and Vadim Konoval, Aachen Germany, for their endodontic treatment and Udo Wittmann, Bern/Switzerland, for his expert statistical analysis.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Herrera, D.; Retamal-Valdes, B.; Alonso, B.; Feres, M. Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endo-periodontal lesions. J. Clin. Periodontol. 2018, 45 (Suppl. 20), 578–594. [Google Scholar] [CrossRef] [PubMed]
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F.; et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45 (Suppl. 20), 162–170. [Google Scholar] [CrossRef] [PubMed]
- Ruetters, M.; Gehrig, H.; Kronsteiner, D.; Schuessler, D.L.; Kim, T.S. Prevalence of endo-perio lesions according to the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Disease in a university hospital. Quintessence Int. 2022, 53, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Cortellini, P.; Stalpers, G.; Mollo, A.; Tonetti, M.S. Periodontal regeneration versus extraction and prosthetic replacement of teeth severely compromised by attachment loss to the apex: 5-year results of an ongoing randomized clinical trial. J. Clin. Periodontol. 2011, 38, 915–924. [Google Scholar] [CrossRef] [PubMed]
- Cortellini, P.; Stalpers, G.; Mollo, A.; Tonetti, M.S. Periodontal regeneration versus extraction and dental implant or prosthetic replacement of teeth severely compromised by attachment loss to the apex: A randomized controlled clinical trial reporting 10-year outcomes, survival analysis and mean cumulative cost of recurrence. J. Clin. Periodontol. 2020, 47, 768–776. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; Herrera, D.; Kebschull, M.; Chapple, I.; Jepsen, S.; Berglundh, T.; Sculean, A.; Tonetti, M.S.; EFP Workshop Participants and Methodological Consultants. Treatment of stage I–III periodontitis—The EFP S3 level clinical practice guideline. J. Clin. Periodontol. 2020, 47 (Suppl. 22), 4–60. [Google Scholar] [CrossRef] [PubMed]
- Herrera, D.; Sanz, M.; Kebschull, M.; Jepsen, S.; Sculean, A.; Berghlund, T.; Papapanou, P.N.; Chapple, I.; Tonetti, M.S.; EFP Workshop Participants and Methodological Consultants. Treatment of stage IV periodontitis: The EFP S3 level clinical practice guideline. J. Clin. Periodontol. 2022, 49 (Suppl. 24), 4–71. [Google Scholar] [CrossRef]
- Zehnder, M.; Gold, S.I.; Hasselgren, G. Pathologic interactions in pulpal and periodontal tissues. J. Clin. Periodontol. 2002, 29, 663–671. [Google Scholar] [CrossRef]
- Schmidt, J.C.; Walter, C.; Amato, M.; Weiger, R. Treatment of periodontal-endodontic lesions—A systematic review. J. Clin. Periodontol. 2014, 41, 779–790. [Google Scholar] [CrossRef]
- Ruetters, M.; Kim, T.S.; Krisam, J.; El-Sayed, S.; El Sayed, N. Effect of endodontic treatment on periodontal healing of grade 3 endo-periodontal lesions without root damage in periodontally compromised patients—A retrospective pilot study. Clin. Oral Investig. 2021, 25, 2373–2380. [Google Scholar] [CrossRef]
- Gupta, S.; Tewari, S.; Tewari, S.; Mittal, S. Effect of Time Lapse between Endodontic and Periodontal Therapies on the Healing of Concurrent Endodontic-Periodontal Lesions without Communication: A Prospective Randomized Clinical Trial. J. Endod. 2015, 41, 785–790. [Google Scholar] [CrossRef] [PubMed]
- Dong, T.; Zhang, Y.; Li, X. Time-lapse between periodontal regeneration surgery and root canal therapy in severe combined periodontal-endodontic lesions. Saudi Dent J. 2023, 35, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Cortellini, P.; Tonetti, M.S. Clinical concepts for regenerative therapy in intrabony defects. Periodontol 2000 2015, 68, 282–307. [Google Scholar] [CrossRef] [PubMed]
- Bröseler, F.; Tietmann, C.; Hinz, A.; Jepsen, S. Long-term results of periodontal regenerative therapy: A retrospective practice-based cohort study. J. Clin. Periodontol. 2017, 44, 520–529. [Google Scholar] [CrossRef] [PubMed]
- Nibali, L.; Sun, C.; Akcalı, A.; Yeh, Y.-C.; Tu, Y.; Donos, N. The effect of horizontal and vertical furcation involvement on molar survival: A retrospective study. J. Clin. Periodontol. 2017, 45, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Nibali, L.; Koidou, V.; Nieri, M.; Barbato, L.; Pagliaro, U.; Cairo, F. Regenerative surgery versus access flap for the treatment of intrabony periodontal defects. A systematic review and meta-analysis. J. Clin. Periodontol. 2020, 47 (Suppl. 22), 320–351. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulos, A.; Bertl, K.; Spinelli, L.; Sculean, A.; Cortellini, P.; Tonetti, M.S. Medium- and long-term clinical benefits of periodontal regenerative/reconstructive procedures in intrabony defects: Systematic review and network meta-analysis of randomized controlled clinical studies. J. Clin. Periodontol. 2021, 48, 410–430. [Google Scholar] [CrossRef] [PubMed]
- Ghezzi, C.; Virzì, M.; Schupbach, P.; Broccaioli, A.; Simion, M. Treatment of combined endodontic-periodontic lesions using guided tissue regeneration: Clinical case and histology. Int. J. Periodontics Restorative Dent. 2012, 32, 433–439. [Google Scholar]
- Aksel, H.; Serper, A. A case series associated with different kinds of endo-perio lesions. J. Clin. Exp. Dent. 2014, 6, e91–e95. [Google Scholar] [CrossRef]
- Pico-Blanco, A.; Castelo-Baz, P.; Caneiro-Queija, L.; Liñares-González, A.; Martin-Lancharro, P.; Blanco-Carrión, J. Saving Single-rooted Teeth with Combined Endodontic-periodontal Lesions. J. Endod. 2016, 42, 1859–1864. [Google Scholar] [CrossRef]
- Arx, T.; Bosshardt, D. The use of Enamel Matrix Derivative (Emd) for Treatment of Combined Apicomarginal Lesions in Apical Surgery: A Retrospecitve Analysis. Eur. Endod. J. 2018, 3, 146–152. [Google Scholar]
- AlJasser, R.; Bukhary, S.; AlSarhan, M.; Alotaibi, D.; AlOraini, S.; Habib, S.R. Regenerative Therapy Modality for Treatment of True Combined Endodontic-Periodontal Lesions: A Randomized Controlled Clinical Trial. Int. J. Environ. Res. Public Health 2021, 18, 6220. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.; Chung, S.H.; Han, J.Y. Periodontal regenerative therapy in endo-periodontal lesions: A retrospective study over 5 years. J. Periodont. Impl. Sci. 2019, 49, 90–104. [Google Scholar] [CrossRef] [PubMed]
- Hamp, S.; Nyman, S.; Lindhe, J. Periodontal treatment of multirooted teeth. Results after 5 years. J. Clin. Periodontol. 1975, 49, 225–237. [Google Scholar]
- Tarnow, D.; Fletcher, P. Classification of the vertical component of furcation involvement. J. Periodontol. 1984, 55, 283–284. [Google Scholar] [CrossRef] [PubMed]
- Jepsen, K.; Sculean, A.; Jepsen, S. Complications and treatment errors related to regenerative periodontal surgery. Periodontol 2000 2023, 92, 120–134. [Google Scholar] [CrossRef] [PubMed]
- Miller, S. Textbook of Periodontia; Blakiston Company: Philadelphia, PA, USA, 1950. [Google Scholar]
- Rosner, B.; Glynn, R.; Lee, M.L. The Wilcoxon signed rank test for paired comparisons of clustered data. Biometrics 2006, 62, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Datta, S.; Satten, G.A. A signed-Rank Test for Clustered Data. Biometrics 2008, 64, 501–507. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 23 December 2022).
- Hothorn, T.; Hornik, K.; van den Weil, M.A.; Zeileis, A. Implementing a class of permutation tests: The coin package. J. Stat. Softw. 2008, 28, 1–23. [Google Scholar] [CrossRef]
- López-Valverde, I.; Vignoletti, F.; Vignoletti, G.; Martin, C.; Sanz, M. Long-term tooth survival and success following primary root canal treatment: A 5-to 37-year retrospective observation. Clin. Oral Investig. 2023, 27, 3233–3244. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Christiansen, A.L.; Cortellini, P. Vertical subclassification predicts survival of molars with class II furcation involvement during supportive periodontal care. J. Clin. Periodontol. 2017, 44, 1140–1144. [Google Scholar] [CrossRef]
- Cortellini, P.; Cortellini, S.; Tonetti, M.S. Papilla preservation flaps for periodontal regeneration of molars severely compromised by combined furcation and intrabony defects: Retrospective analysis of a registry-based cohort. J. Periodontol. 2020, 91, 165–173. [Google Scholar] [CrossRef]
- Salvi, G.; Mischler, D.; Schmidlin, K.; Matuliene, G.; Pjetursson, B.; Brägger, U.; Lang, N.P. Risk factors associated with the longevity of multi-rooted teeth. Long-term outcomes after active and supportive periodontal therapy. J. Clin. Periodontol. 2014, 41, 701–707. [Google Scholar] [CrossRef]
- Jepsen, S.; Gennai, S.; Hirschfeld, S.; Kalemai, Z.; Buti, J.; Graziani, F. Regenerative surgical treatment of furcation defects: A systematic review and Bayesian network meta-analysis of randomized clinical trials. J. Clin Periodontol. 2020, 47 (Suppl. 22), 352–374. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).