Decreased Risk of Knee Osteoarthritis with Taller Height in an East Asian Population: A Nationwide Cohort Study
Abstract
1. Introduction
2. Method
2.1. Data Source and Study Population
2.2. Ethics
2.3. Data Collection and Comorbidities
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
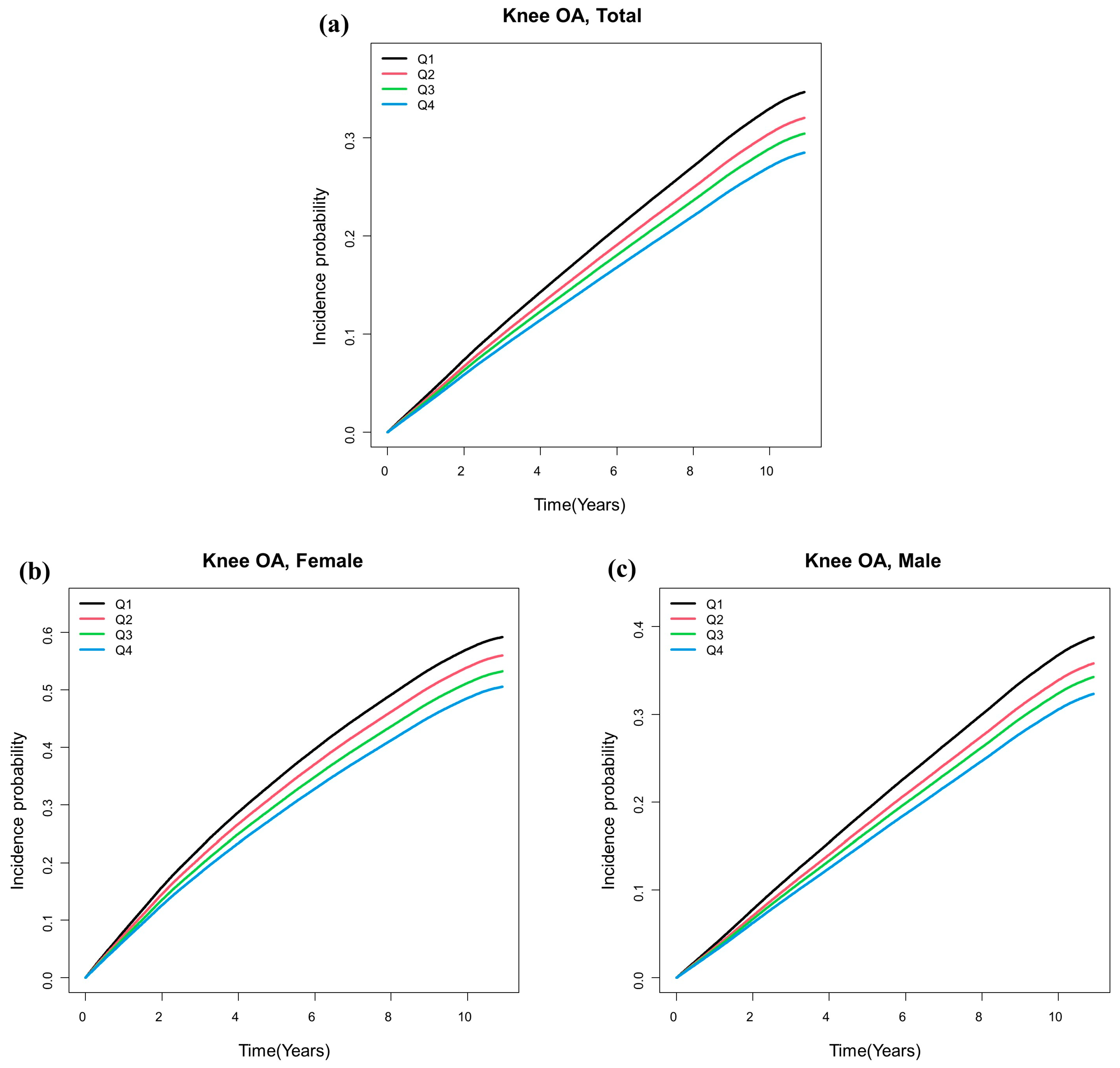
3.2. Risk of Osteoarthritis According to Height
3.3. Subgroup Analysis by Gender and Age
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fransen, M.; Bridgett, L.; March, L.; Hoy, D.; Penserga, E.; Brooks, P. The epidemiology of osteoarthritis in Asia. Int. J. Rheum. Dis. 2011, 14, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Kan, H.S.; Chan, P.K.; Chiu, K.Y.; Yan, C.H.; Yeung, S.S.; Ng, Y.L.; Shiu, K.W.; Ho, T. Non-surgical treatment of knee osteoarthritis. Hong Kong Med. J. 2019, 25, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Zhen, X.; Hu, X.; Li, Y.; Gu, S.; Gu, Y.; Dong, H. Osteoarthritis in the Middle-Aged and Elderly in China: Prevalence and Influencing Factors. Int. J. Environ. Res. Public Health 2019, 16, 4701. [Google Scholar] [CrossRef] [PubMed]
- Berenbaum, F. Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthr. Cartil. 2013, 21, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Robinson, W.H.; Lepus, C.M.; Wang, Q.; Raghu, H.; Mao, R.; Lindstrom, T.M.; Sokolove, J. Low-grade inflammation as a key mediator of the pathogenesis of osteoarthritis. Nat. Rev. Rheumatol. 2016, 12, 580–592. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.-D.; Li, G.-M.; Jin, W.; Li, Y.; Zhang, Y.-P. Positive selection on the osteoarthritis-risk and decreased-height associated variants at the GDF5 gene in East Asians. PLoS ONE 2012, 7, e42553. [Google Scholar] [CrossRef]
- Elliott, K.S.; Chapman, K.; Day-Williams, A.; Panoutsopoulou, K.; Southam, L.; Lindgren, C.M.; Arden, N.; Aslam, N.; Birrell, F.; Carluke, I. Evaluation of the genetic overlap between osteoarthritis with body mass index and height using genome-wide association scan data. Ann. Rheum. Dis. 2013, 72, 935–941. [Google Scholar] [CrossRef]
- Valdes, A.M.; Spector, T.D. Genetic epidemiology of hip and knee osteoarthritis. Nat. Rev. Rheumatol. 2011, 7, 23–32. [Google Scholar] [CrossRef]
- Park, D.; Park, Y.M.; Ko, S.H.; Hyun, K.S.; Choi, Y.H.; Min, D.U.; Han, K.; Koh, H.S. Association of general and central obesity, and their changes with risk of knee osteoarthritis: A nationwide population-based cohort study. Sci. Rep. 2023, 13, 3796. [Google Scholar] [CrossRef]
- Bailey, O.; Gronkowski, K.; Leach, W.J. Effect of body mass index and osteoarthritis on outcomes following arthroscopic meniscectomy: A prospective nationwide study. Knee 2015, 22, 95–99. [Google Scholar] [CrossRef]
- Lee, B.J.; Yang, S.; Kwon, S.; Choi, K.H.; Kim, W. Association between metabolic syndrome and knee osteoarthritis: A cross-sectional nationwide survey study. J. Rehabil. Med. 2019, 51, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Apold, H.; Meyer, H.; Nordsletten, L.; Furnes, O.; Baste, V.; Flugsrud, G. Weight gain and the risk of knee replacement due to primary osteoarthritis: A population based, prospective cohort study of 225,908 individuals. Osteoarthr. Cartil. 2014, 22, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Shim, H.Y.; Park, M.; Kim, H.J.; Kyung, H.S.; Shin, J.Y. Physical activity status by pain severity in patients with knee osteoarthritis: A nationwide study in Korea. BMC Musculoskelet. Disord. 2018, 19, 380. [Google Scholar] [CrossRef] [PubMed]
- Park, H.M.; Kim, H.J.; Lee, B.; Kwon, M.; Jung, S.M.; Lee, S.W.; Park, Y.B.; Song, J.J. Decreased muscle mass is independently associated with knee pain in female patients with radiographically mild osteoarthritis: A nationwide cross-sectional study (KNHANES 2010–2011). Clin. Rheumatol. 2018, 37, 1333–1340. [Google Scholar] [CrossRef] [PubMed]
- Ojemolon, P.E.; Shaka, H.; Edigin, E.; Gomez, T.M.A.; Eseaton, P.; Bello, J.; Azubuike, C.; Adekola, O.P. Impact of Diabetes Mellitus on Outcomes of Patients with Knee Osteoarthritis Who Underwent Knee Arthroplasty: An Analysis of the Nationwide Inpatient Sample. Cureus 2020, 12, e8902. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.H.; Chung, C.H.; Lee, C.H.; Hsieh, C.H.; Hung, Y.J.; Lin, F.H.; Tsao, C.H.; Hsieh, P.S.; Chien, W.C. Combination COX-2 inhibitor and metformin attenuate rate of joint replacement in osteoarthritis with diabetes: A nationwide, retrospective, matched-cohort study in Taiwan. PLoS ONE 2018, 13, e0191242. [Google Scholar] [CrossRef] [PubMed]
- Park, D.; Park, Y.M.; Ko, S.H.; Choi, Y.H.; Min, D.U.; Ahn, J.H.; Kim, B.; Koh, H.S.; Han, K. Association between knee osteoarthritis and the risk of cardiovascular disease and the synergistic adverse effects of lack of exercise. Sci. Rep. 2023, 13, 2777. [Google Scholar] [CrossRef]
- Huang, S.-W.; Wang, W.-T.; Chou, L.-C.; Liao, C.-D.; Liou, T.-H.; Lin, H.-W. Osteoarthritis increases the risk of dementia: A nationwide cohort study in Taiwan. Sci. Rep. 2015, 5, 10145. [Google Scholar] [CrossRef]
- Park, H.M.; Kim, H.S.; Lee, Y.J. Knee osteoarthritis and its association with mental health and health-related quality of life: A nationwide cross-sectional study. Geriatr. Gerontol. Int. 2020, 20, 379–383. [Google Scholar] [CrossRef]
- Kluzek, S.; Rubin, K.H.; Sanchez-Santos, M.; O’Hanlon, M.S.; Andersen, M.; Glintborg, D.; Abrahamsen, B. Accelerated osteoarthritis in women with polycystic ovary syndrome: A prospective nationwide registry-based cohort study. Arthritis Res. Ther. 2021, 23, 225. [Google Scholar] [CrossRef]
- Apold, H.; Meyer, H.E.; Nordsletten, L.; Furnes, O.; Baste, V.; Flugsrud, G.B. Risk factors for knee replacement due to primary osteoarthritis, a population based, prospective cohort study of 315,495 individuals. BMC Musculoskelet. Disord. 2014, 15, 217. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Balkwill, A.; Banks, E.; Cooper, C.; Green, J.; Beral, V. Relationship of height, weight and body mass index to the risk of hip and knee replacements in middle-aged women. Rheumatology 2007, 46, 861–867. [Google Scholar] [CrossRef] [PubMed]
- Lohmander, L.S.; De Verdier, M.G.; Rollof, J.; Nilsson, P.M.; Engström, G. Incidence of severe knee and hip osteoarthritis in relation to different measures of body mass: A population-based prospective cohort study. Ann. Rheum. Dis. 2009, 68, 490–496. [Google Scholar] [CrossRef] [PubMed]
- Welling, M.; Auvinen, J.; Lehenkari, P.; Männikkö, M.; Karppinen, J.; Eskola, P.J. Association between height and osteoarthritis of the knee and hip: The Northern Finland Birth Cohort 1966 Study. Int. J. Rheum. Dis. 2017, 20, 1095–1104. [Google Scholar] [CrossRef]
- Wilder, F.; Hall, B.; Barrett, J., Jr.; Lemrow, N. History of acute knee injury and osteoarthritis of the knee: A prospective epidemiological assessment: The Clearwater Osteoarthritis Study. Osteoarthr. Cartil. 2002, 10, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Lau, E.; Cooper, C.; Lam, D.; Chan, V.; Tsang, K.; Sham, A. Factors associated with osteoarthritis of the hip and knee in Hong Kong Chinese: Obesity, joint injury, and occupational activities. Am. J. Epidemiol. 2000, 152, 855–862. [Google Scholar] [CrossRef] [PubMed]
- Sanna, S.; Jackson, A.U.; Nagaraja, R.; Willer, C.J.; Chen, W.-M.; Bonnycastle, L.L.; Shen, H.; Timpson, N.; Lettre, G.; Usala, G. Common variants in the GDF5-UQCC region are associated with variation in human height. Nat. Genet. 2008, 40, 198–203. [Google Scholar] [CrossRef]
- Valdes, A.M.; Evangelou, E.; Kerkhof, H.J.; Tamm, A.; Doherty, S.A.; Kisand, K.; Tamm, A.; Kerna, I.; Uitterlinden, A.; Hofman, A. The GDF5 rs143383 polymorphism is associated with osteoarthritis of the knee with genome-wide statistical significance. Ann. Rheum. Dis. 2011, 70, 873–875. [Google Scholar] [CrossRef]
- Song, S.O.; Jung, C.H.; Song, Y.D.; Park, C.-Y.; Kwon, H.-S.; Cha, B.S.; Park, J.-Y.; Lee, K.-U.; Ko, K.S.; Lee, B.-W. Background and data configuration process of a nationwide population-based study using the korean national health insurance system. Diabetes Metab. J. 2014, 38, 395–403. [Google Scholar] [CrossRef]
- Park, H.R.; Im, S.; Kim, H.; Jung, S.Y.; Kim, D.; Jang, E.J.; Sung, Y.K.; Cho, S.K. Validation of algorithms to identify knee osteoarthritis patients in the claims database. Int. J. Rheum. Dis. 2019, 22, 890–896. [Google Scholar] [CrossRef]
- Schmidt, M.; Bøtker, H.E.; Pedersen, L.; Sørensen, H.T. Adult height and risk of ischemic heart disease, atrial fibrillation, stroke, venous thromboembolism, and premature death: A population based 36-year follow-up study. Eur. J. Epidemiol. 2014, 29, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Lai, F.Y.; Nath, M.; Hamby, S.E.; Thompson, J.R.; Nelson, C.P.; Samani, N.J. Adult height and risk of 50 diseases: A combined epidemiological and genetic analysis. BMC Med. 2018, 16, 187. [Google Scholar] [CrossRef] [PubMed]
- Ben-Zion Berliner, M.; Katz, L.H.; Derazne, E.; Levine, H.; Keinan-Boker, L.; Benouaich-Amiel, A.; Gal, O.; Kanner, A.A.; Laviv, Y.; Honig, A.; et al. Height as a risk factor in meningioma: A study of 2 million Israeli adolescents. BMC Cancer 2020, 20, 786. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Liang, L.; Feng, Y.A.; De Vivo, I.; Giovannucci, E.; Tang, J.Y.; Han, J. Height, height-related SNPs, and risk of non-melanoma skin cancer. Br. J. Cancer 2017, 116, 134–140. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ikegawa, S. New gene associations in osteoarthritis: What do they provide, and where are we going? Curr. Opin. Rheumatol. 2007, 19, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Wang, J.; Ji, H.; Jia, H.; Guan, D. Interaction between GDF5 gene polymorphisms and environment factors increased the risk of knee osteoarthritis: A case-control study. Biosci. Rep. 2019, 39, BSR20182423. [Google Scholar] [CrossRef]
- García-Alvarado, F.; Rosales-González, M.; Arellano-Pérez-Vertti, D.; Espino-Silva, P.; Meza-Velazquez, M.; Ruiz-Flores, P. Association Between the SNP rs143383 + 104T/C in the GDF5 Gene and the Risk of Knee Osteoarthritis in a Population from Northern Mexico-A Case-Control Study. Genet. Test. Mol. Biomark. 2018, 22, 503–506. [Google Scholar] [CrossRef]
- Vaes, R.B.; Rivadeneira, F.; Kerkhof, J.M.; Hofman, A.; Pols, H.A.; Uitterlinden, A.G.; van Meurs, J.B. Genetic variation in the GDF5 region is associated with osteoarthritis, height, hip axis length and fracture risk: The Rotterdam study. Ann. Rheum. Dis. 2009, 68, 1754–1760. [Google Scholar] [CrossRef]
- Pan, F.; Tian, J.; Winzenberg, T.; Ding, C.; Jones, G. Association between GDF5 rs143383 polymorphism and knee osteoarthritis: An updated meta-analysis based on 23,995 subjects. BMC Musculoskelet. Disord. 2014, 15, 404. [Google Scholar] [CrossRef][Green Version]

| Age (years) | 50–59 | 60–69 | 70–79 | 80– |
| Male | Height quartile cut-off values (cm) | |||
| Q1 | –164 | –162 | –160 | –158 |
| Q2 | 165–168 | 163–166 | 161–164 | 159–162 |
| Q3 | 169–171 | 167–169 | 165–168 | 163–166 |
| Q4 | 172– | 170– | 169– | 167– |
| Female | Height quartile cut-off values (cm) | |||
| Q1 | –152 | –149 | –146 | –142 |
| Q2 | 153–155 | 150–153 | 147–150 | 143–146 |
| Q3 | 156–159 | 154–156 | 151–153 | 147–150 |
| Q4 | 160– | 157– | 154– | 151– |
| Male | |||||
|---|---|---|---|---|---|
| Q1 (n = 172,404) | Q2 (n = 179,332) | Q3 (n = 137,611) | Q4 (n = 173,542) | p Value | |
| Age, years (%) | <0.0001 | ||||
| 50–59 | 98,749 (57.28) | 102,159 (56.97) | 75,291 (54.71) | 99,367 (57.26) | |
| 60–69 | 53,061 (30.78) | 55,217 (30.79) | 40,572 (29.48) | 54,307 (31.29) | |
| 70–79 | 18,335 (10.63) | 19,597 (10.93) | 19,490 (14.16) | 17,535 (10.1) | |
| ≥80 | 2259 (1.31) | 2359 (1.32) | 2258 (1.64) | 2333 (1.34) | |
| Income, low 25 (%) | 40,539 (23.51) | 39,360 (21.95) | 28,573 (20.76) | 34,817 (20.06) | <0.0001 |
| DM (%) | 29,629 (17.19) | 31,253 (17.43) | 24,120 (17.53) | 30,456 (17.55) | 0.0211 |
| Hypertension (%) | 75,394 (43.73) | 77,580 (43.26) | 59,601 (43.31) | 72,828 (41.97) | <0.0001 |
| Dyslipidemia (%) | 37,831 (21.94) | 39,585 (22.07) | 30,148 (21.91) | 37,013 (21.33) | <0.0001 |
| Smoking (%) | <0.0001 | ||||
| Non | 62,433 (36.21) | 60,707 (33.85) | 45,611 (33.14) | 55,081 (31.74) | |
| Ex | 48,440 (28.1) | 55,977 (31.21) | 45,108 (32.78) | 59,786 (34.45) | |
| Current | 61,531 (35.69) | 62,648 (34.93) | 46,892 (34.08) | 58,675 (33.81) | |
| Drinking (%) | <0.0001 | ||||
| Non | 72,807 (42.23) | 72,643 (40.51) | 55,105 (40.04) | 67,246 (38.75) | |
| Mild | 78,318 (45.43) | 84,052 (46.87) | 65,070 (47.29) | 83,509 (48.12) | |
| Heavy | 21,279 (12.34) | 22,637 (12.62) | 17,436 (12.67) | 22,787 (13.13) | |
| Regular exercise (%) | 38,707 (22.45) | 43,676 (24.35) | 34,745 (25.25) | 45,292 (26.1) | <0.0001 |
| Mean age, years | 59.66 ± 7.57 | 59.4 ± 7.61 | 59.78 ± 8.05 | 58.82 ± 7.61 | <0.0001 |
| Weight, kg | 61.09 ± 7.94 | 65.58 ± 8 | 68.22 ± 8.31 | 72.66 ± 9.08 | <0.0001 |
| BMI, kg/m² | 23.87 ± 2.9 | 23.95 ± 2.82 | 23.94 ± 2.82 | 24.02 ± 2.83 | <0.0001 |
| Female | |||||
| Q1 (n = 119,651) | Q2 (n = 115,897) | Q3 (n = 123,090) | Q4 (n = 117,377) | p Value | |
| Age, years (%) | <0.0001 | ||||
| 50–59 | 78,922 (65.96) | 65,530 (56.54) | 84,097 (68.32) | 67,618 (57.61) | |
| 60–69 | 28,187 (23.56) | 36,502 (31.5) | 28,114 (22.84) | 35,889 (30.58) | |
| 70–79 | 10,800 (9.03) | 12,113 (10.45) | 9012 (7.32) | 11,982 (10.21) | |
| ≥80 | 1742 (1.46) | 1752 (1.51) | 1867 (1.52) | 1888 (1.61) | |
| Income, low 25 (%) | 33,147 (27.7) | 28,872 (24.91) | 29,917 (24.3) | 26,090 (22.23) | <0.0001 |
| DM (%) | 12,353 (10.32) | 12,560 (10.84) | 11,932 (9.69) | 12,478 (10.63) | <0.0001 |
| Hypertension (%) | 44,005 (36.78) | 43,059 (37.15) | 41,543 (33.75) | 41,234 (35.13) | <0.0001 |
| Dyslipidemia (%) | 36,010 (30.1) | 35,231 (30.4) | 35,614 (28.93) | 34,012 (28.98) | <0.0001 |
| Smoking (%) | <0.0001 | ||||
| Non | 115,408 (96.45) | 111,507 (96.21) | 117,920 (95.8) | 112,263 (95.64) | |
| Ex | 1154 (0.96) | 1240 (1.07) | 1540 (1.25) | 1622 (1.38) | |
| Current | 3089 (2.58) | 3150 (2.72) | 3630 (2.95) | 3492 (2.98) | |
| Drinking (%) | <0.0001 | ||||
| Non | 102,496 (85.66) | 99,507 (85.86) | 103,995 (84.49) | 100,400 (85.54) | |
| Mild | 16,478 (13.77) | 15,729 (13.57) | 18,299 (14.87) | 16,250 (13.84) | |
| Heavy | 677 (0.57) | 661 (0.57) | 796 (0.65) | 727 (0.62) | |
| Regular exercise (%) | 19,863 (16.6) | 21,781 (18.79) | 24,659 (20.03) | 24,830 (21.15) | <0.0001 |
| Mean age, years | 58.56 ± 7.72 | 59.23 ± 7.79 | 57.52 ± 7.35 | 58.57 ± 7.74 | <0.0001 |
| Weight, kg | 52.5 ± 7.18 | 55.42 ± 7.18 | 57.7 ± 7.28 | 60.66 ± 7.82 | <0.0001 |
| BMI, kg/m² | 23.98 ± 3.09 | 23.8 ± 3 | 23.61 ± 2.92 | 23.43 ± 2.91 | <0.0001 |
| Height | Number | Knee OA | IR/1000 (Person Years) | Hazard Ratio (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||
| Total | ||||||||
| Q1 | 292,055 | 121,065 | 54.8360 | 1 (ref.) | 1 (ref.) | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Q2 | 295,229 | 120,743 | 53.5730 | 0.977 (0.969, 0.985) | 0.985 (0.977, 0.993) | 0.985 (0.978, 0.993) | 0.99 (0.982, 0.998) | 0.908 (0.9, 0.915) |
| Q3 | 260,701 | 109,290 | 55.0482 | 1.004 (0.996, 1.012) | 0.975 (0.967, 0.983) | 0.976 (0.968, 0.984) | 0.988 (0.979, 0.996) | 0.853 (0.846, 0.86) |
| Q4 | 290,919 | 118,414 | 52.8754 | 0.964 (0.956, 0.972) | 0.979 (0.971, 0.987) | 0.98 (0.973, 0.988) | 0.996 (0.988, 1.004) | 0.787 (0.781, 0.795) |
| Gender | ||||||||
| Male | ||||||||
| Q1 | 172,404 | 56,517 | 40.9737 | 1 (ref.) | 1 (ref.) | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Q2 | 179,332 | 57,798 | 39.7050 | 0.968 (0.957, 0.979) | 0.974 (0.963, 0.985) | 0.973 (0.962, 0.985) | 0.971 (0.96, 0.983) | 0.904 (0.893, 0.915) |
| Q3 | 137,611 | 44,354 | 39.8483 | 0.972 (0.96, 0.984) | 0.966 (0.954, 0.978) | 0.965 (0.953, 0.977) | 0.963 (0.951, 0.975) | 0.855 (0.844, 0.866) |
| Q4 | 173,542 | 55,229 | 38.8388 | 0.947 (0.936, 0.958) | 0.968 (0.957, 0.979) | 0.967 (0.955, 0.978) | 0.964 (0.952, 0.975) | 0.796 (0.786, 0.807) |
| Female | ||||||||
| Q1 | 119,651 | 64,548 | 77.9174 | 1 (ref.) | 1 (ref.) | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Q2 | 115,897 | 62,945 | 78.8670 | 1.012 (1.001, 1.023) | 0.998 (0.987, 1.009) | 0.999 (0.989, 1.011) | 1.013 (1.002, 1.024) | 0.917 (0.907, 0.927) |
| Q3 | 123,090 | 64,936 | 74.4442 | 0.956 (0.946, 0.966) | 0.977 (0.966, 0.988) | 0.98 (0.969, 0.99) | 1.005 (0.995, 1.017) | 0.848 (0.839, 0.858) |
| Q4 | 117,377 | 63,185 | 77.2917 | 0.992 (0.981, 1.003) | 0.992 (0.981, 1.002) | 0.996 (0.985, 1.007) | 1.035 (1.023, 1.046) | 0.787 (0.778, 0.796) |
| Total | Hazard Ratio (95% CI) | ||||||
|---|---|---|---|---|---|---|---|
| Age | Height | Number | Knee OA | IR/1000 (Person-Years) | Model 3 (p < 0.0001) | Model 4 (p < 0.0001) | Model 5 (p < 0.0001) |
| 50–59 | Q1 | 177,671 | 69,410 | 48.5214 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Q2 | 167,689 | 61,536 | 44.7085 | 0.967 (0.956, 0.977) | 0.974 (0.963, 0.984) | 0.894 (0.884, 0.904) | |
| Q3 | 159,388 | 62,514 | 48.5412 | 0.963 (0.953, 0.974) | 0.979 (0.968, 0.99) | 0.848 (0.838, 0.857) | |
| Q4 | 166,985 | 60,853 | 44.2354 | 0.965 (0.954, 0.975) | 0.983 (0.972, 0.994) | 0.778 (0.769, 0.787) | |
| 60–69 | Q1 | 81,248 | 37,765 | 65.4846 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Q2 | 91,719 | 43,477 | 66.3163 | 0.987 (0.974, 1.001) | 0.99 (0.976, 1.003) | 0.905 (0.893, 0.918) | |
| Q3 | 68,686 | 32,848 | 66.7852 | 0.989 (0.975, 1.004) | 0.995 (0.981, 1.01) | 0.859 (0.847, 0.872) | |
| Q4 | 90,196 | 42,413 | 64.9676 | 0.978 (0.964, 0.992) | 0.991 (0.977, 1.005) | 0.785 (0.774, 0.797) | |
| 70–79 | Q1 | 29,135 | 12,751 | 70.3615 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Q2 | 31,710 | 14,429 | 71.9773 | 1.036 (1.011, 1.061) | 1.036 (1.012, 1.061) | 0.949 (0.927, 0.972) | |
| Q3 | 28,502 | 12,604 | 68.4241 | 1.039 (1.014, 1.065) | 1.043 (1.017, 1.069) | 0.898 (0.876, 0.921) | |
| Q4 | 29,517 | 13,711 | 72.7004 | 1.044 (1.019, 1.07) | 1.049 (1.024, 1.074) | 0.83 (0.81, 0.851) | |
| ≥80 | Q1 | 4001 | 1139 | 58.8918 | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Q2 | 4111 | 1301 | 60.9286 | 1.067 (0.986, 1.156) | 1.065 (0.984, 1.153) | 0.976 (0.901, 1.057) | |
| Q3 | 4125 | 1324 | 61.7391 | 1.066 (0.985, 1.154) | 1.064 (0.983, 1.151) | 0.919 (0.849, 0.995) | |
| Q4 | 4221 | 1437 | 64.1502 | 1.127 (1.043, 1.218) | 1.125 (1.041, 1.216) | 0.891 (0.824, 0.963) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, D.H.; Lee, H.S.; Jang, S.H.; Heu, J.-Y.; Han, K.; Lee, S.-W. Decreased Risk of Knee Osteoarthritis with Taller Height in an East Asian Population: A Nationwide Cohort Study. J. Clin. Med. 2024, 13, 92. https://doi.org/10.3390/jcm13010092
Lee DH, Lee HS, Jang SH, Heu J-Y, Han K, Lee S-W. Decreased Risk of Knee Osteoarthritis with Taller Height in an East Asian Population: A Nationwide Cohort Study. Journal of Clinical Medicine. 2024; 13(1):92. https://doi.org/10.3390/jcm13010092
Chicago/Turabian StyleLee, Dong Hwan, Hwa Sung Lee, Soo Hyun Jang, Jun-Young Heu, Kyungdo Han, and Se-Won Lee. 2024. "Decreased Risk of Knee Osteoarthritis with Taller Height in an East Asian Population: A Nationwide Cohort Study" Journal of Clinical Medicine 13, no. 1: 92. https://doi.org/10.3390/jcm13010092
APA StyleLee, D. H., Lee, H. S., Jang, S. H., Heu, J.-Y., Han, K., & Lee, S.-W. (2024). Decreased Risk of Knee Osteoarthritis with Taller Height in an East Asian Population: A Nationwide Cohort Study. Journal of Clinical Medicine, 13(1), 92. https://doi.org/10.3390/jcm13010092









