Lipid-Lowering Therapy in PURE Poland Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
- (1)
- Do you have high cholesterol?
- (2)
- Are you taking medications regularly to lower your cholesterol?
- (3)
- In the last 12 months, were you taking medications for lowering cholesterol but then stopped?
- (4)
- In the past month, how often did you take your cholesterol medications as the doctor prescribed?
- (1)
- Doctor advised me to stop because cholesterol was under control; Felt unwell from cholesterol medication(s) so was told to stop; Felt well, no need to take my medications.
- (2)
- Self-decision to stop because cholesterol was under control; Felt unwell from cholesterol medications so decided to stop; Felt well, no need to take my medications; Cannot afford cholesterol medications; The pharmacy is too far away from me; I have to take too many medications; My cholesterol medication is often not available in my pharmacy.
- High for moderate CKD (eGFR 30–44 mL/min/1.73 m2 and ACR (albumin-to-creatinine ratio) < 30 or eGFR 45–59 mL/min/1.73 m2 and ACR 30–300 or eGFR > 60 mL/min/1.73 m2 and ACR > 300).
- Very high for severe CKD (eGFR < 30 mL/min/1.73 m2 or eGFR 30–44 mL/min/1.73 m2 and ACR > 30).
- Moderate for well-controlled, short-lived diabetes (<10 years) without data indicating TOD (target organ damage) and without additional ASCVD risk factors.
- High for patients with DM without ASCVD and/or severe TOD [16] and do not meet criteria for moderate risk.
- Very high for DM patients with ASCVD and/or severe TOD or eGFR < 45 mL/min/1.73 m2 regardless of albuminuria or eGFR 45–59 mL/min/1.73 m2 and microalbuminuria (ACR 30–300 mg/g) or proteinuria (ACR > 300 mg/g) or presence of microvascular disease in at least 3 locations.
- Very high for documented ASCVD, either clinically or unequivocally on imaging studies. Clinically documented ASCVD includes previous AMI (acute myocardial infarction), ACS (acute coronary syndrome), coronary revascularization and other arterial revascularization procedures, stroke, TIA (transient ischemic attack), aortic aneurysm and PAD (peripheral artery disease). ASCVD found unequivocally on imaging studies includes the presence of atherosclerotic plaque found on coronary angiography or ultrasound of the carotid arteries, or on CTA (computed tomography angiography).
3. Results
3.1. Overall Results
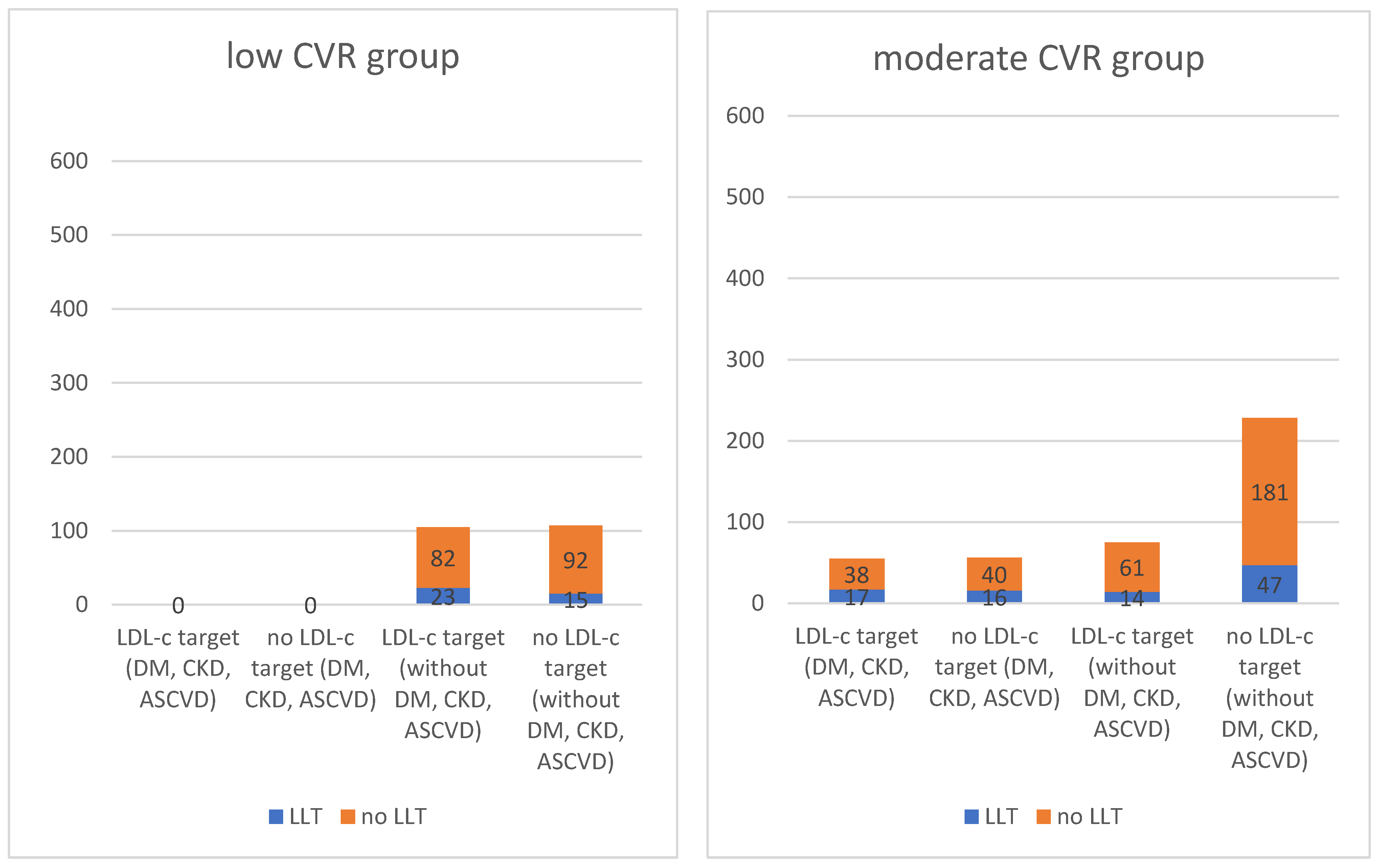
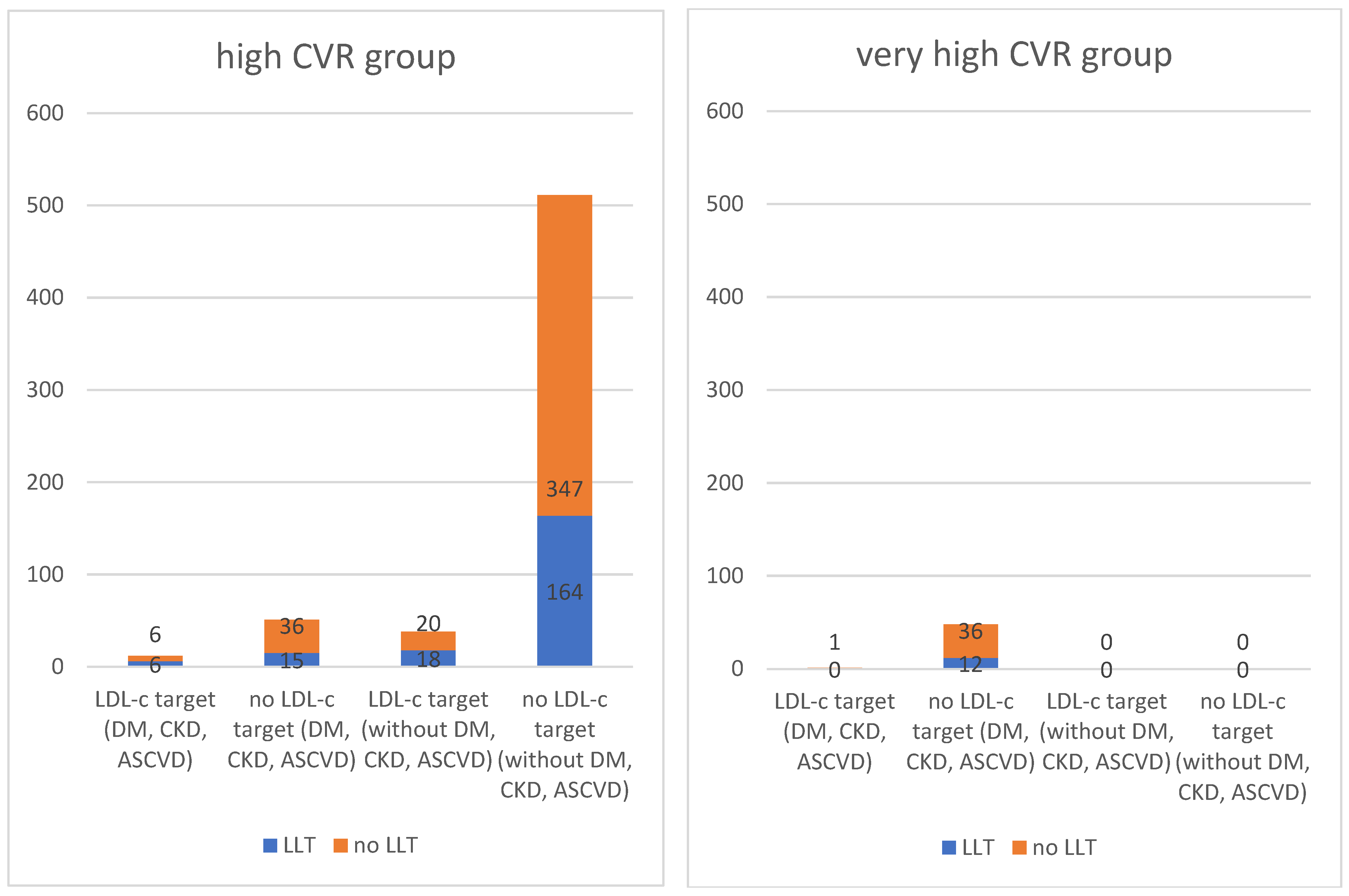
3.2. Outcomes in Specific Cardiovascular Risk Groups
3.2.1. Patients Classified in the Low CVR Group
3.2.2. Patients with Moderate CVR
3.2.3. Patients Classified in the High CVR Group
3.2.4. Patients Classified as Having a Very High CVR
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raport: Sytuacja Zdrowotna Ludności Polski i Jej Uwarunkowania. Available online: https://www.pzh.gov.pl/raport-sytuacja-zdrowotna-ludnosci-polski-i-jej-uwarunkowania (accessed on 3 April 2023).
- SCORE2 Working Group and ESC Cardiovascular risk Collaboration. SCORE2 risk prediction algorithms: New models to estimate 10-year risk of cardiovascular disease in Europe. Eur. Heart J. 2021, 42, 2439–2454. [Google Scholar] [CrossRef]
- SCORE2-OP Working Group and ESC Cardiovascular Risk Collaboration. SCORE2-OP risk prediction algorithms: Estimating incident cardiovascular event risk in older persons in four geographical risk regions. Eur. Heart J. 2021, 42, 2455–2467. [Google Scholar] [CrossRef] [PubMed]
- Dudina, A.; Cooney, M.T.; Bacquer, D.D.; Backer, G.D.; Ducimetière, P.; Jousilahti, P.; Keil, U.; Menotti, A.; Njølstad, I.; Oganov, R.; et al. Relationships between body mass index, cardiovascular mortality, and risk factors: A report from the SCORE investigators. Eur. J. Cardiovasc. Prev. Rehabil. 2011, 18, 731–742. [Google Scholar] [CrossRef] [PubMed]
- Cornelius, M.E.; Wang, T.W.; Jamal, A.; Loretan, C.G.; Neff, L.J. Tobacco Product Use Among Adults—United States, 2019. MMWR Morb. Mortal Wkly. Rep. 2020, 69, 1736–1742. [Google Scholar] [CrossRef] [PubMed]
- Ward, S.; Lloyd Jones, M.; Pandor, A.; Holmes, M.; Ara, R.; Ryan, A.; Yeo, W.; Payne, N. A systematic review and economic evaluation of statins for the prevention of coronary events. Health Technol. Assess. 2007, 11, 1–160. [Google Scholar] [CrossRef] [PubMed]
- Aznaouridis, K.; Masoura, C.; Vlachopoulos, C.; Tousoulis, D. Statins in Stroke. Curr. Med. Chem. 2019, 26, 6174–6185. [Google Scholar] [CrossRef] [PubMed]
- Almeida, S.O.; Budoff, M. Effect of statins on atherosclerotic plaque. Trends Cardiovasc. Med. 2019, 29, 451–455. [Google Scholar] [CrossRef] [PubMed]
- Zatońska, K.; Zatoński, W.A.; Szuba, A. Prospective urban and rural epidemiology Poland—Study design. J. Health Inequalities 2016, 2, 136–141. [Google Scholar] [CrossRef]
- Polskie Towarzystwo. Diabetologiczne. Zalecenia kliniczne dotyczące postępowania u chorych na cukrzycę 2019. Diabetol. Prakt. 2019, 5, 7–10. [Google Scholar]
- Teo, K.; Chow, C.K.; Vaz, M.; Rangarajan, S.; Yusuf, S.; PURE Investigators-Writing Group. The Prospective Urban Rural Epidemiology (PURE) study: Examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am. Heart J. 2009, 158, 1–7.e1. [Google Scholar] [CrossRef]
- Szuba, A.; Martynowicz, H.; Zatońska, K.; Ilow, R.; Regulska-Ilow, B.; Różańska, D.; Wołyniec, M.; Połtyn-Zaradna, K.; Zatoński, W. Prevalence of hypertension in Polish population of PURE Poland study. J. Health Inequalities 2016, 2, 157–162. [Google Scholar] [CrossRef]
- World Health Organization. Disease Burden and Mortality Estimates. Available online: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates (accessed on 5 April 2023).
- Visseren, F.L.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Back, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, S.J.; Looker, H.C.; Hothersall, E.J.; Wild, S.H.; Lindsay, R.S.; Chalmers, J.; Cleland, S.; Leese, G.P.; McKnight, J.; Morris, A.D.; et al. Risk of cardiovascular disease and total mortality in adults with type 1 diabetes: Scottish registry linkage study. PLoS Med. 2012, 9, e1001321. [Google Scholar] [CrossRef] [PubMed]
- Sattar, N.; Rawshani, A.; Franzén, S.; Rawshani, A.; Svensson, A.M.; Rosengren, A.; McGuire, D.K.; Eliasson, B.; Gudbjörnsdottir, S. Age at diagnosis of type 2 diabetes mellitus and associations with cardiovascular and mortality risks. Circulation 2019, 139, 2228–2237. [Google Scholar] [CrossRef] [PubMed]
- Pischon, T.; Girman, C.J.; Sacks, F.M.; Rifai, N.; Stampfer, M.J.; Rimm, E.B. Non-high-density lipoprotein cholesterol and apolipoprotein B in the prediction of coronary heart disease in men. Circulation 2005, 112, 3375–3383. [Google Scholar] [CrossRef] [PubMed]
- Ridker, P.M.; Rifai, N.; Cook, N.R.; Bradwin, G.; Buring, J.E. Non-HDL cholesterol, apolipoproteins A-I and B100, standard lipid measures, lipid ratios, and CRP as risk factors for cardiovascular disease in women. JAMA 2005, 294, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Burgess, S. Appraising the causal role of smoking in multiple diseases: A systematic review and meta-analysis of Mendelian randomization studies. EBioMedicine 2022, 82, 104154. [Google Scholar] [CrossRef]
- Samson, R.; Ennezat, P.V.; Le Jemtel, T.H.; Oparil, S. Cardiovascular Disease Risk Reduction and Body Mass Index. Curr. Hypertens. Rep. 2022, 24, 535–546. [Google Scholar] [CrossRef]
- Whelton, S.P.; McEvoy, J.W.; Shaw, L.; Psaty, B.M.; Lima, J.A.; Budoff, M.; Nasir, K.; Szklo, M.; Blumenthal, R.S.; Blaha, M.J. Association of normal systolic blood pressure level with cardiovascular disease in the absence of risk factors. JAMA Cardiol. 2020, 5, 1011–1018. [Google Scholar] [CrossRef]
- Duarte Lau, F.; Giugliano, R.P. Lipoprotein(a) and its Significance in Cardiovascular Disease: A Review. JAMA Cardiol. 2022, 7, 760–769. [Google Scholar] [CrossRef]
- Klop, B.; Elte, J.W.; Cabezas, M.C. Dyslipidemia in obesity: Mechanisms and potential targets. Nutrients 2013, 5, 1218–1240. [Google Scholar] [CrossRef] [PubMed]
- Pająk, A.; Szafraniec, K.; Polak, M.; Polakowska, M.; Kozela, M.; Piotrowski, W.; Kwaśniewska, M.; Podolecka, E.; Kozakiewicz, K.; Tykarski, A.; et al. Changes in the prevalence, treatment, and control of hypercholesterolemia and other dyslipidemias over 10 years in Poland: The WOBASZ study. Pol. Arch. Med. Wewn. 2016, 126, 642–652. [Google Scholar] [CrossRef] [PubMed]
- Anza-Ramirez, C.; Lazo, M.; Zafra-Tanaka, J.H.; Avila-Palencia, I.; Bilal, U.; Hernández-Vásquez, A.; Knoll, C.; Lopez-Olmedo, N.; Mazariegos, M.; Moore, K.; et al. The urban built environment and adult BMI, obesity, and diabetes in Latin American cities. Nat. Commun. 2022, 13, 7977. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Shon, C.; Yi, S. The Relationship between Obesity and Urban Environment in Seoul. Int. J. Environ. Res. Public Health 2017, 14, 898. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-Larco, R.M.; Bernabé-Ortiz, A.; Pillay, T.D.; Gilman, R.H.; Sanchez, J.F.; Poterico, J.A.; Quispe, R.; Smeeth, L.; Miranda, J.J. Obesity risk in rural, urban and rural-to-urban migrants: Prospective results of the PERU MIGRANT study. Int. J. Obes. 2016, 40, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Kohli-Lynch, C.N.; Lewsey, J.; Boyd, K.A.; French, D.D.; Jordan, N.; Moran, A.E.; Sattar, N.; Preiss, D.; Briggs, A.H. Beyond 10-Year Risk: A Cost-Effectiveness Analysis of Statins for the Primary Prevention of Cardiovascular Disease. Circulation 2022, 145, 1312–1323. [Google Scholar] [CrossRef]
- Choudhry, N.K.; Setoguchi, S.; Levin, R.; Winkelmayer, W.C.; Shrank, W.H. Trends in adherence to secondary prevention medications in elderly post-myocardial infarction patients. Pharmacoepidemiol. Drug Saf. 2008, 17, 1189–1196. [Google Scholar] [CrossRef]
- Nieuwkerk, P.T.; Nierman, M.C.; Vissers, M.N.; Locadia, M.; Greggers-Peusch, P.; Knape, L.P.; Kastelein, J.J.; Sprangers, M.A.; de Haes, H.C.; Stroes, E.S. Intervention to improve adherence to lipid-lowering medication and lipid-levels in patients with an increased cardiovascular risk. Am. J. Cardiol. 2012, 110, 666–672. [Google Scholar] [CrossRef]
- Haynes, R.B.; McKibbon, K.A.; Kanani, R. Systematic review of randomised trials of interventions to assist patients to follow prescriptions for medications. Lancet 1996, 348, 383–386. [Google Scholar] [CrossRef]
- Hagström, E.; Steg, P.G.; Szarek, M.; Bhatt, D.L.; Bittner, V.A.; Danchin, N.; Diaz, R.; Goodman, S.G.; Harrington, R.A.; Jukema, J.W.; et al. Apolipoprotein B, Residual Cardiovascular Risk After Acute Coronary Syndrome, and Effects of Alirocumab. Circulation 2022, 146, 657–672. [Google Scholar] [CrossRef]
- Khan, S.U.; Yedlapati, S.H.; Lone, A.N.; Hao, Q.; Guyatt, G.; Delvaux, N.; Bekkering, G.E.T.; Vandvik, P.O.; Riaz, I.B.; Li, S.; et al. PCSK9 inhibitors and ezetimibe with or without statin therapy for cardiovascular risk reduction: A systematic review and network meta-analysis. BMJ 2022, 377, e069116. [Google Scholar] [CrossRef] [PubMed]
- Mihaylova, B.; Emberson, J.; Blackwell, L.; Keech, A.; Simes, J.; Barnes, E.H.; Voysey, M.; Gray, A.; Collins, R.; Baigent, C. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: Meta-analysis of individual data from 27 randomised trials. Lancet 2012, 380, 581–590. [Google Scholar] [CrossRef] [PubMed]
| Polish Cohort of the PURE Study | 2035 |
|---|---|
| participants analysed | 1287 |
| patients with DM, ASCVD, CKD | 223 |
| other patients | 1064 |
| urban residents/rural residents | 877/410 |
| men/women | 441/846 |
| patients with low CVR | 212 |
| patients with moderate CVR | 414 |
| patients with high CVR | 612 |
| patients with very high CVR | 49 |
| Low CVR | Moderate CVR | High CVR | Very High CVR | |
|---|---|---|---|---|
| number of people | 212 | 414 | 612 | 49 |
| urban residents | 155 (73.1%) | 275 (66.4%) | 416 (68%) | 31 (67.2%) |
| men | 63 (29.7%) | 147 (35.5%) | 205 (33.55%) | 26 (53.1%) |
| have achieved the target LDL-c | 105 (49.5%) | 130 (31.4%) | 50 (8.2%) | 1 (2%) |
| were taking LLT | 23 (21.9%) | 31 (23.8%) | 24 (48%) | 0 (0%) |
| were not taking LLT | 82 (78.1%) | 99 (76.2%) | 26 (52%) | 1 (100%) |
| have not achieved the target LDL-c concentration | 107 (50.5%) | 284 (68.6%) | 562 (91.8%) | 48 (98%) |
| were taking LLT | 15 (14%) | 63 (22.2%) | 179 (31.9%) | 12 (25%) |
| were not taking LLT | 92 (86%) | 221 (77.8%) | 383 (68.1%) | 36 (75%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lubieniecki, P.; Wołyniec, M.; Połtyn-Zaradna, K.; Zatońska, K.; Szuba, A. Lipid-Lowering Therapy in PURE Poland Cohort Study. J. Clin. Med. 2024, 13, 60. https://doi.org/10.3390/jcm13010060
Lubieniecki P, Wołyniec M, Połtyn-Zaradna K, Zatońska K, Szuba A. Lipid-Lowering Therapy in PURE Poland Cohort Study. Journal of Clinical Medicine. 2024; 13(1):60. https://doi.org/10.3390/jcm13010060
Chicago/Turabian StyleLubieniecki, Paweł, Maria Wołyniec, Katarzyna Połtyn-Zaradna, Katarzyna Zatońska, and Andrzej Szuba. 2024. "Lipid-Lowering Therapy in PURE Poland Cohort Study" Journal of Clinical Medicine 13, no. 1: 60. https://doi.org/10.3390/jcm13010060
APA StyleLubieniecki, P., Wołyniec, M., Połtyn-Zaradna, K., Zatońska, K., & Szuba, A. (2024). Lipid-Lowering Therapy in PURE Poland Cohort Study. Journal of Clinical Medicine, 13(1), 60. https://doi.org/10.3390/jcm13010060






