Umbilical Vein Blood Flow in Uncomplicated Pregnancies: Systematic Review of Available Reference Charts and Comparison with a New Cohort
Abstract
1. Introduction
2. Materials and Methods
2.1. Systematic Review of the Available UV-Q Reference Ranges
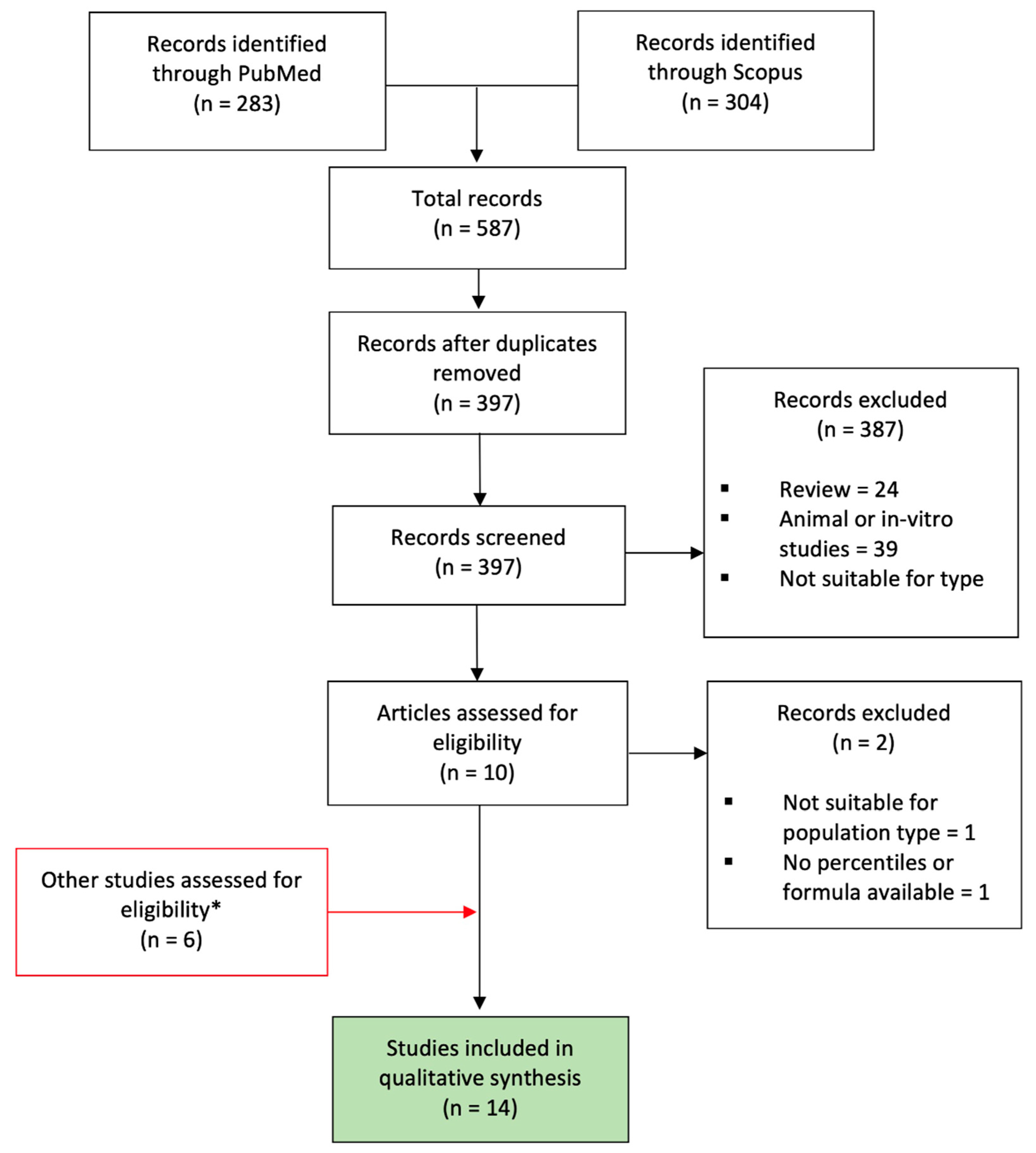
2.1.1. Study Identification and Selection
- -
- The sampling site: (a) studies investigating UV-Q on the intra-abdominal (IA) portion of the UV; and (b) studies investigating UV-Q at the free-floating (FF) portion of the UV;
- -
- The formula used to compute the UV-Q.
2.1.2. Quality Assessment
2.2. Prospective Cohort Study on UV-Q, UV-Q/AC, and UV-Q/EFW
Statistical Analysis
3. Results
3.1. Systematic Review of the Available UV-Q Reference Ranges
3.1.1. Risk of Bias within Studies According to QUADAS Criteria
3.1.2. Description of the Included Studies
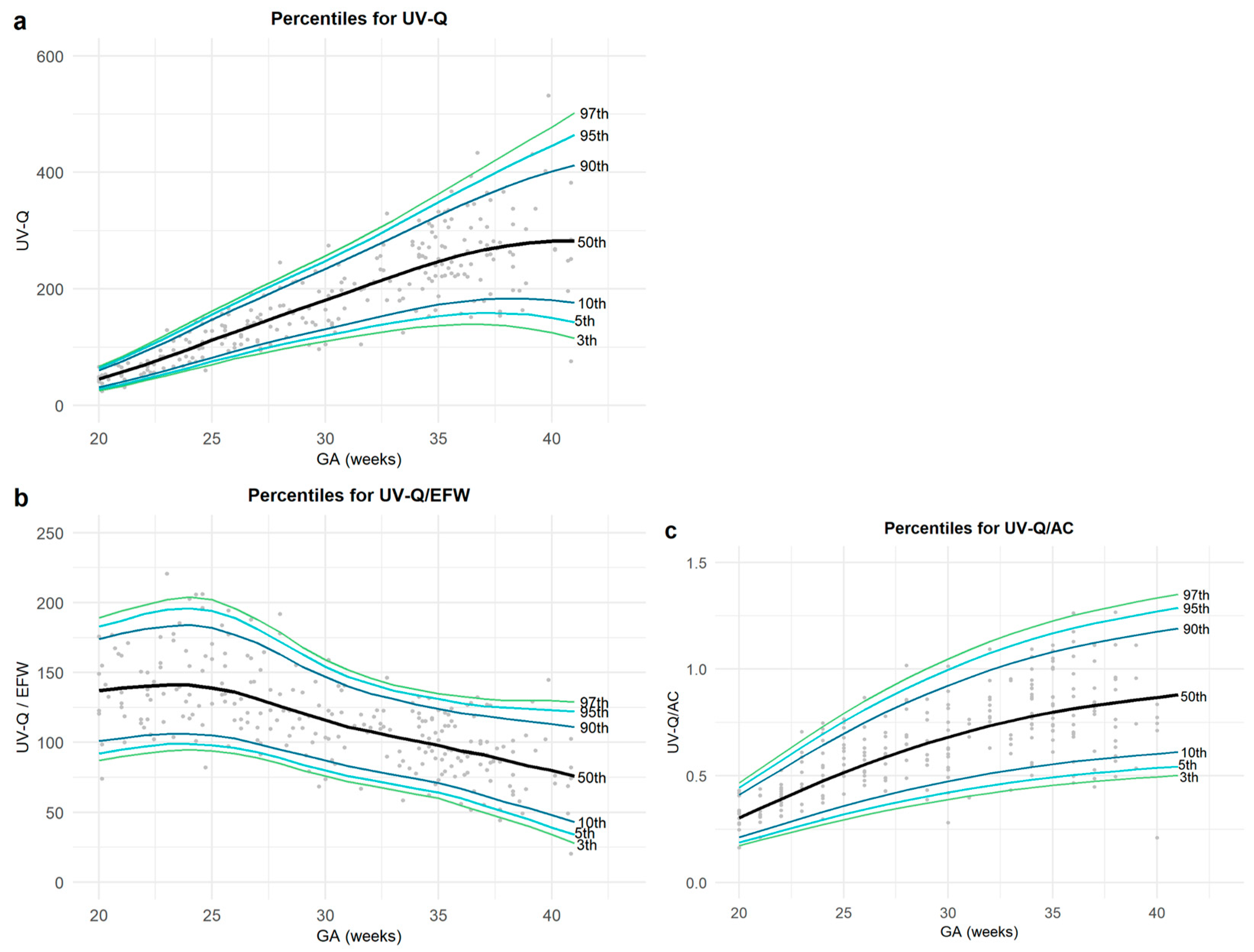
3.2. Prospective Cohort Study on UV-Q
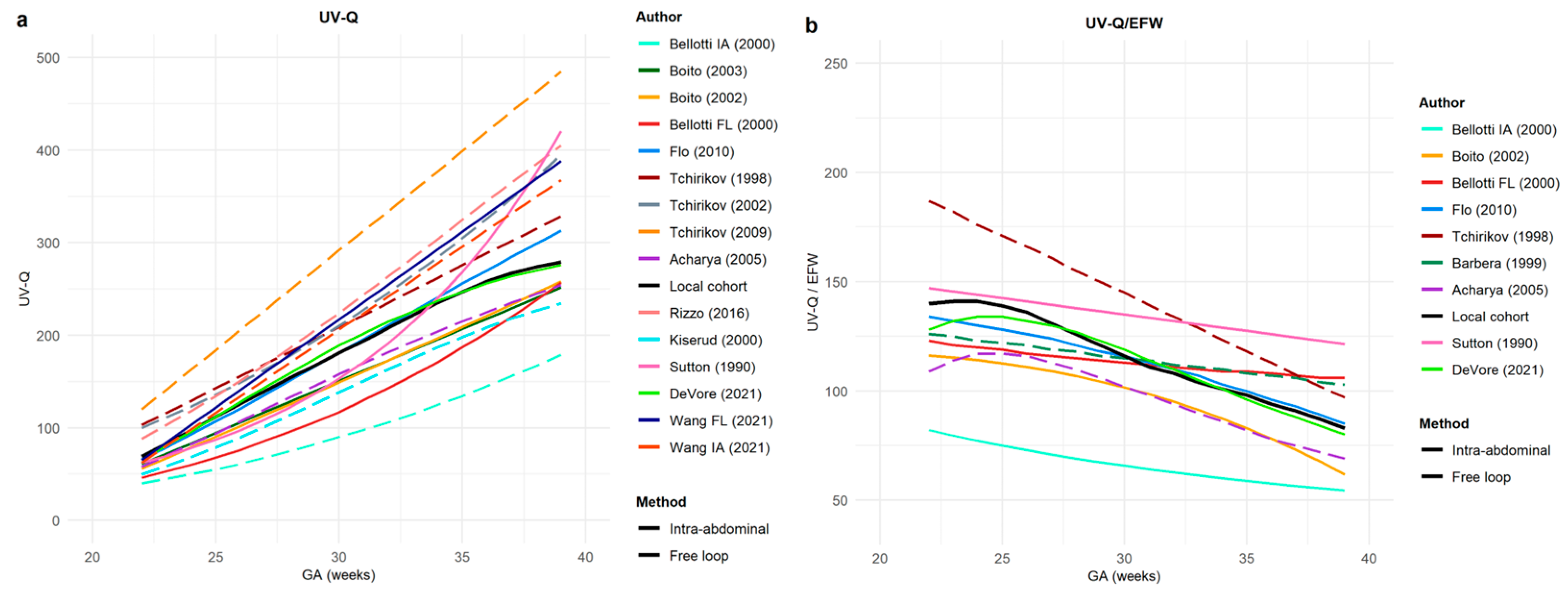
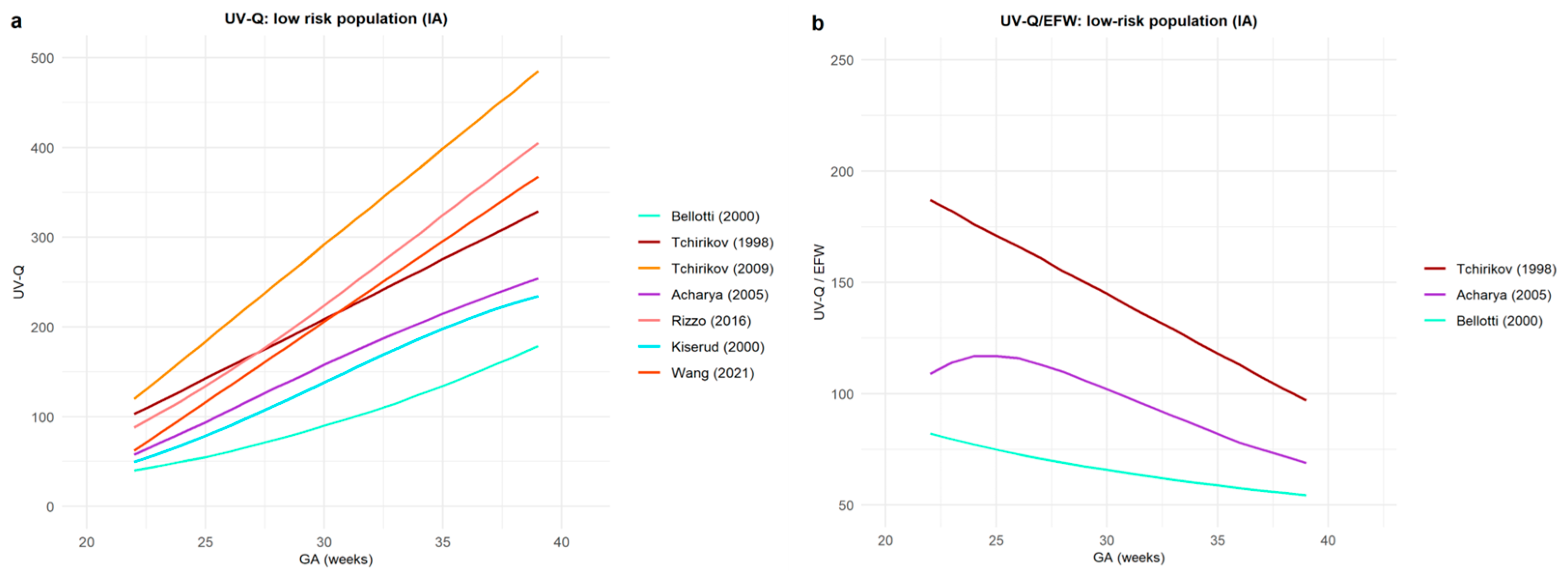
Comparison between Reference Range Values for UV-Q and UV-Q/EFW
4. Discussion
4.1. The Main Findings of the Study
4.2. Comment
4.2.1. Methodology
4.2.2. Experimental Research
4.3. Strengths and Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tchirikov, M.; Strohner, M.; Scholz, A. Cardiac output and blood flow volume redistribution during acute maternal hypoxia in fetal sheep. J. Perinat. Med. 2010, 38, 387–392. [Google Scholar] [CrossRef]
- Flo, K.; Wilsgaard, T.; Acharya, G. Agreement between umbilical vein volume blood flow measurements obtained at the intra-abdominal portion and free loop of the umbilical cord. Ultrasound Obstet. Gynecol. 2009, 34, 171–176. [Google Scholar] [CrossRef]
- Barbera, A.; Galan, H.L.; Ferrazzi, E.; Rigano, S.; Józwik, M.; Battaglia, F.C.; Pardi, G. Relationship of umbilical vein blood flow to growth parameters in the human fetus. Am. J. Obstet. Gynecol. 1999, 181, 174–179. [Google Scholar] [CrossRef]
- Flo, K.; Wilsgaard, T.; Vartun, A.; Acharya, G. A longitudinal study of the relationship between maternal cardiac output measured by impedance cardiography and uterine artery blood flow in the second half of pregnancy. BJOG 2010, 117, 837–844. [Google Scholar] [CrossRef]
- Najafzadeh, A.; Dickinson, J.E. Umbilical venous blood flow and its measurement in the human fetus. J. Clin. Ultrasound 2012, 40, 502–511. [Google Scholar] [CrossRef]
- Ferrazzi, E.; Rigano, S.; Bozzo, M.; Bellotti, M.; Giovannini, N.; Galan, H.; Battaglia, F.C. Umbilical vein blood flow in growth-restricted fetuses. Ultrasound Obstet. Gynecol. 2000, 16, 432–438. [Google Scholar] [CrossRef]
- Rizzo, G.; Mappa, I.; Bitsadze, V.; Słodki, M.; Khizroeva, J.; Makatsariya, A.; D’antonio, F. Role of Doppler ultrasound at time of diagnosis of late-onset fetal growth restriction in predicting adverse perinatal outcome: Prospective cohort study. Ultrasound Obstet. Gynecol. 2020, 55, 793–798. [Google Scholar] [CrossRef]
- Prior, T.; Mullins, E.; Bennett, P.; Kumar, S. Umbilical venous flow rate in term fetuses: Can variations in flow predict intrapartum compromise? Am. J. Obstet. Gynecol. 2014, 210, 61.e1–61.e8. [Google Scholar] [CrossRef]
- Prior, T.; Mullins, E.; Bennett, P.; Kumar, S. Prediction of fetal compromise in labor. Obstet. Gynecol. 2014, 123, 1263–1271. [Google Scholar] [CrossRef]
- Parra-Saavedra, M.; Crovetto, F.; Triunfo, S.; Savchev, S.; Parra, G.; Sanz, M.; Gratacos, E.; Figueras, F. Added value of umbilical vein flow as a predictor of perinatal outcome in term small-for-gestational-age fetuses. Ultrasound Obstet. Gynecol. 2013, 42, 189–195. [Google Scholar] [CrossRef]
- Jouppila, P.; Kirkinen, P. Umbilical vein blood flow as an indicator of fetal hypoxia. Br. J. Obstet. Gynaecol. 1984, 91, 107–110. [Google Scholar]
- Gill, R.W.; Kossoff, G.; Warren, P.S.; Garrett, W.J. Umbilical venous flow in normal and complicated pregnancy. Ultrasound Med. Biol. 1984, 10, 349–363. [Google Scholar] [CrossRef]
- Ferrazzi, E.; Di Martino, D.; Stampalija, T. Doppler interrogation of the umbilical venous flow. In Maulik and Lees book on Doppler Ultrasound; Springer: Cham, Switzerland, 2023. [Google Scholar]
- Ferrazzi, E.; Di Martino, D.; Stampalija, T. Blood flow volume in umbilical vein in fetal growth restriction. In Placental-Fetal Growth Restriction; University of Cambridge: Cambridge, UK, 2018; pp. 155–163. [Google Scholar]
- Giles, W.B.; Lingman, G.; Marsal, K.; Trudinger, B.J. Fetal volume blood flow and umbilical artery flow velocity waveform analysis: A comparison. Br. J. Obstet. Gynaecol. 1986, 93, 461–465. [Google Scholar] [CrossRef]
- Van Splunder, I.P.; Huisman, T.W.; Stijnen, T.; Wladimiroff, J.W. Presence of pulsations and reproducibility of waveform recording in the umbilical and left portal vein in normal pregnancies. Ultrasound Obstet. Gynecol. 1994, 4, 49–53. [Google Scholar] [CrossRef]
- Reed, K.L.; Meijboom, E.J.; Sahn, D.J.; Scagnelli, S.A.; Valdes-Cruz, L.M.; Shenker, L. Cardiac Doppler flow velocities in human fetuses. Circulation 1986, 73, 41–46. [Google Scholar] [CrossRef]
- Sutton, M.S.J.; Theard, M.A.; Bhatia, S.J.; Plappert, T.; Saltzman, D.H.; Doubilet, P. Changes in placental blood flow in the normal human fetus with gestational age. Pediatr. Res. 1990, 28, 383–387. [Google Scholar] [CrossRef]
- Figueras, F.; Fernandez, S.; Hernandez-Andrade, E.; Gratacos, E. Umbilical venous blood flow measurement: Accuracy and reproducibility. Ultrasound Obstet. Gynecol. 2008, 32, 587–591. [Google Scholar] [CrossRef]
- PROSPERO. International Prospective Register of Systematic Reviews [Homepage on the Internet]. Available online: https://www.crd.york.ac.uk/prospero/ (accessed on 15 December 2021).
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef]
- Whiting, P.F.; Rutjes, A.W.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.; Sterne, J.A.; Bossuyt, P.M. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Stampalija, T.; Monasta, L.; Barbieri, M.; Chiodo, A.; Quadrifoglio, M.; Fantasia, I.; Bello, L.L.; Barresi, V.; Ottaviani, C.; Di Martino, D.D.; et al. Late-term fetuses with reduced umbilical vein blood flow volume: An under-recognized population at increased risk of growth restriction. Eur. J. Obstet. Gynecol. Reprod. Biol. 2022, 272, 182–187. [Google Scholar] [CrossRef]
- Salomon, L.J.; Alfirevic, Z.; Da Silva Costa, F.; Deter, R.L.; Figueras, F.; Ghi, T.A.; Glanc, P.; Khalil, A.; Lee, W.; Napolitano, R.; et al. ISUOG Practice Guidelines: Ultrasound assessment of fetal biometry and growth. Ultrasound Obstet. Gynecol. 2019, 53, 715–723. [Google Scholar] [CrossRef]
- Bhide, A.; Acharya, G.; Bilardo, C.M.; Brezinka, C.; Cafici, D.; Hernandez-Andrade, E.; Kalache, K.; Kingdom, J.; Kiserud, T.; Lee, W.; et al. ISUOG practice guidelines: Use of Doppler ultrasonography in obstetrics. Ultrasound Obstet. Gynecol. 2013, 41, 233–239. [Google Scholar]
- Hadlock, F.P.; Harrist, R.B.; Sharman, R.S.; Deter, R.L.; Park, S.K. Estimation of fetal weight with the use of head, body, and femur measurements--a prospective study. Am. J. Obstet. Gynecol. 1985, 151, 333–337. [Google Scholar] [CrossRef]
- DeVore, G.R.; Epstein, A. Computing Z-Score Equations for Clinical Use to Measure Fetal Umbilical Vein Size and Flow Using Six Independent Variables of Age and Size. J. Ultrasound Med. 2021. [Google Scholar] [CrossRef]
- Salomon, L.J.; Duyme, M.; Crequat, J.; Brodaty, G.; Talmant, C.; Fries, N.; Althuser, M. French fetal biometry: Reference equations and comparison with other charts. Ultrasound Obstet. Gynecol. 2006, 28, 193–198. [Google Scholar] [CrossRef]
- A Language and Environment for Statistical Computing. Foundation for Statistical Computing, Vienna, Austria. Available online: https://www.R-project.org/ (accessed on 15 December 2021).
- Widnes, C.; Flo, K.; Wilsgaard, T.; Odibo, A.O.; Acharya, G. Sexual Dimorphism in Umbilical Vein Blood Flow During the Second Half of Pregnancy: A Longitudinal Study. J. Ultrasound Med. 2017, 36, 2447–2458. [Google Scholar] [CrossRef]
- Lees, C.; Albaiges, G.; Deane, C.; Parra, M.; Nicolaides, K.H. Assessment of umbilical arterial and venous flow using color Doppler. Ultrasound Obstet. Gynecol. 1999, 14, 250–255. [Google Scholar] [CrossRef]
- Flo, K.; Wilsgaard, T.; Acharya, G. Longitudinal reference ranges for umbilical vein blood flow at a free loop of the umbilical cord. Ultrasound Obstet. Gynecol. 2010, 36, 567–572. [Google Scholar] [CrossRef]
- Tchirikov, M.; Strohner, M.; Forster, D.; Huneke, B. A combination of umbilical artery PI and normalized blood flow volume in the umbilical vein: Venous-arterial index for the prediction of fetal outcome. Eur. J. Obstet. Gynecol. Reprod. Biol. 2009, 142, 129–133. [Google Scholar] [CrossRef]
- Acharya, G.; Wilsgaard, T.; Rosvold Berntsen, G.K.; Maltau, J.M.; Kiserud, T. Reference ranges for umbilical vein blood flow in the second half of pregnancy based on longitudinal data. Prenat. Diagn. 2005, 25, 99–111. [Google Scholar] [CrossRef]
- Boito, S.M.; Struijk, P.C.; Ursem, N.T.; Stijnen, T.; Wladimiroff, J.W. Assessment of fetal liver volume and umbilical venous volume flow in pregnancies complicated by insulin-dependent diabetes mellitus. BJOG 2003, 110, 1007–1013. [Google Scholar] [CrossRef]
- Boito, S.; Struijk, P.C.; Ursem, N.T.; Stijnen, T.; Wladimiroff, J.W. Umbilical venous volume flow in the normally developing and growth-restricted human fetus. Ultrasound Obstet. Gynecol. 2002, 19, 344–349. [Google Scholar] [CrossRef]
- Tchirikov, M.; Rybakowski, C.; Huneke, B.; Schoder, V.; Schroder, H.J. Umbilical vein blood volume flow rate and umbilical artery pulsatility as ‘venous-arterial index’ in the prediction of neonatal compromise. Ultrasound Obstet. Gynecol. 2002, 20, 580–585. [Google Scholar] [CrossRef]
- Wang, L.; Zhou, Q.; Zhou, C.; Wang, J.; Shi, C.; Long, B.; Hu, L.; Peng, Y.; Liu, Y.; Xu, G. Response to Comment on “Z-Score Reference Ranges for Umbilical Vein Diameter and Blood Flow Volume in Normal Fetuses”. J. Ultrasound Med. 2022, 41, 2383–2385. [Google Scholar] [CrossRef]
- Rizzo, G.; Rizzo, L.; Aiello, E.; Allegra, E.; Arduini, D. Modelling umbilical vein blood flow normograms at 14-40 weeks of gestation by quantile regression analysis. J. Matern. Fetal Neonatal Med. 2016, 29, 701–706. [Google Scholar] [CrossRef]
- Kiserud, T.; Rasmussen, S.; Skulstad, S. Blood flow and the degree of shunting through the ductus venosus in the human fetus. Am. J. Obstet. Gynecol. 2000, 182, 147–153. [Google Scholar] [CrossRef]
- Bellotti, M.; Pennati, G.; De Gasperi, C.; Battaglia, F.C.; Ferrazzi, E. Role of ductus venosus in distribution of umbilical blood flow in human fetuses during second half of pregnancy. Am. J. Physiol. Heart Circ. Physiol. 2000, 279, H1256–H1263. [Google Scholar] [CrossRef]
- Tchirikov, M.; Rybakowski, C.; Huneke, B.; Schroder, H.J. Blood flow through the ductus venosus in singleton and multifetal pregnancies and in fetuses with intrauterine growth retardation. Am. J. Obstet. Gynecol. 1998, 178, 943–949. [Google Scholar] [CrossRef]
- Stampalija, T.; Ghi, T.; Rosolen, V.; Rizzo, G.; Ferrazzi, E.M.; Prefumo, F.; Dall’Asta, A.; Quadrifoglio, M.; Todros, T.; Frusca, T. Current use and performance of the different fetal growth charts in the Italian population. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 252, 323–329. [Google Scholar] [CrossRef]
- Wolf, H.; Stampalija, T.; Lees, C.C.; Group, T.S. Fetal cerebral blood-flow redistribution: Analysis of Doppler reference charts and association of different thresholds with adverse perinatal outcome. Ultrasound Obstet. Gynecol. 2021, 58, 705–715. [Google Scholar] [CrossRef]
- Giuliani, F.; Ohuma, E.; Spada, E.; Bertino, E.; Al Dhaheri, A.S.; Altman, D.G.; Conde-Agudelo, A.; Kennedy, S.H.; Villar, J.; Cheikh Ismail, L. Systematic review of the methodological quality of studies designed to create neonatal anthropometric charts. Acta Paediatr. 2015, 104, 987–996. [Google Scholar] [CrossRef]
- Pennati, G.; Bellotti, M.; De Gasperi, C.; Rognoni, G. Spatial velocity profile changes along the cord in normal human fetuses: Can these affect Doppler measurements of venous umbilical blood flow? Ultrasound Obstet. Gynecol. 2004, 23, 131–137. [Google Scholar] [CrossRef]
- Galan, H.L.; Jozwik, M.; Rigano, S.; Regnault, T.R.; Hobbins, J.C.; Battaglia, F.C.; Ferrazzi, E. Umbilical vein blood flow determination in the ovine fetus: Comparison of Doppler ultrasonographic and steady-state diffusion techniques. Am. J. Obstet. Gynecol. 1999, 181, 1149–1153. [Google Scholar] [CrossRef]
- Galan, H.L.; Anthony, R.V.; Rigano, S.; Parker, T.A.; de Vrijer, B.; Ferrazzi, E.; Wilkening, R.B.; Regnault, T.R. Fetal hypertension and abnormal Doppler velocimetry in an ovine model of intrauterine growth restriction. Am. J. Obstet. Gynecol. 2005, 192, 272–279. [Google Scholar] [CrossRef]
- Kiserud, T.; Saito, T.; Ozaki, T.; Rasmussen, S.; Hanson, M.A. Validation of diameter measurements by ultrasound: Intraobserver and interobserver variations assessed in vitro and in fetal sheep. Ultrasound Obstet. Gynecol. 1999, 13, 52–57. [Google Scholar] [CrossRef]
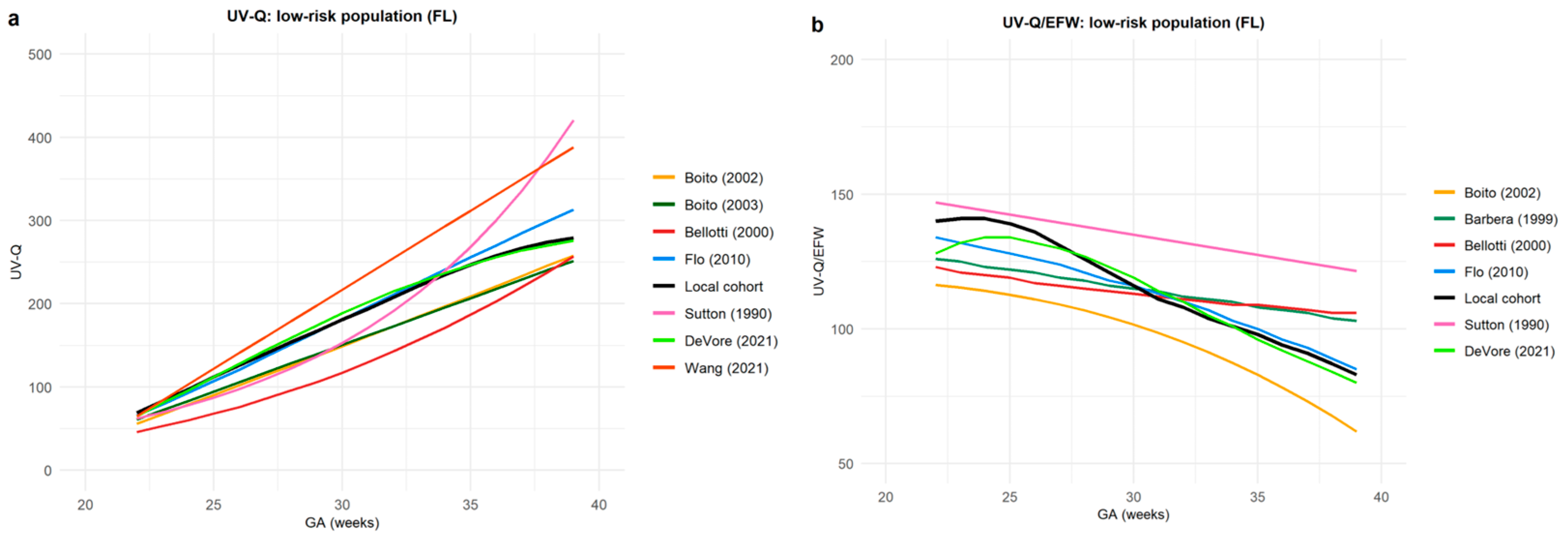

| First Author, Year of Publication | Study Type | Population (N) | Gestational Age | Description of Population | Available Percentiles | Formula for Q-UV Measurement | Mean Values of Q UV (mL/min) | Mean Values of Q-UV Normalized to EFW (mL/min/kg) | |
|---|---|---|---|---|---|---|---|---|---|
| Free-floating portion | |||||||||
| 1 | DeVore et al., 2021 [28] | Prospective cross-sectional study | 240 | 20 to 40 weeks | Singleton low-risk pregnancies | Yes | 0.5 × TaMXV × π(D/2)2 × 60 | ||
| 2 | Flo et al., 2010 [33] | Prospective longitudinal study | 53 | 22 to 39+6 weeks | Singleton low-risk pregnancies | Yes | Two formulae used separately: (1) 0.5 × TaMXV × π(D/2)2 × 60 (2) Vwmean × π(D/2)2 × 60 | 1st formula: from 53 to 250 (22–39+6 weeks) 2nd formula: from 66 to 313 (22–39+6 weeks) | 1st formula: from 110 to 68 (22–39+6 weeks) |
| 3 | Boito et al., 2003 [36] | Cross-sectional matched control study | 64 | 18 to 36 weeks | 32 low-risk £ and 32 diabetic women | No | 0.06 × TaMXV × π × (D/2)2 | 100.5 (in diabetic women) versus 106.2 (in controls) | 94.2 (in diabetic women) versus 109.4 (in controls) |
| 4 | Boito et al., 2002 [37] | Prospective cross-sectional study | 133 | 20 to 36 weeks | 100 low-risk £ and 33 SGA | No | TaMXV × π × (D/2)2 | 33.2 (at 20 weeks) 221.0 (at 36 weeks) | 117.5 (at 20 weeks) 78.3 (at 36 weeks) |
| 5 | Barbera et al., 1999 [3] | Prospective cross-sectional study | 70 | 20 to 38 weeks | Singleton low-risk pregnancies | No | 0.5 × TaMXV × π × (D/2)2 × 60 | 54 (at 23 weeks) 320 (at 38 weeks) | 125 (at 23 weeks) 104 (at 38 weeks) |
| 6 | Sutton et al., 1990 [18] | Prospective cross-sectional study | 74 | 19 to 42 weeks | Singleton low-risk pregnancies | No | FVIUV/s × π × (D/2)2 × 60 | 105–130 | |
| Intra-abdominal portion | |||||||||
| 7 | Rizzo et al., 2016 [40] | Prospective cross-sectional study | 852 | 14 to 40 weeks | Singleton low-risk pregnancies | No | 0.5 × TaMXV × π(D/2)2 × 60 | ||
| 8 | Tchirikov et al., 2009 [34] | Prospective cross-sectional study | 181 | 17 to 41 weeks | 148 low-risk and 33 with poor fetal outcome | No | TaMXV × π × (D/2)2 | 160.2 (in compromised fetuses) versus 253.3 (in controls) | 115.1 (in compromised fetuses) versus 200.3 (in controls) |
| 9 | Acharya et al., 2005 [35] | Prospective longitudinal study | 130 | 19 to 42 weeks | Singleton low-risk pregnancies | Yes | Two formulae used separately: (1) 0.5 × Vmax × π(D/2)2 × 60 (2) Vwmean × π(D/2)2 × 60 | 1st formula: from 27.6 to 271.1 (19–41 weeks) 2nd formula: from 27.13 to 273.4 (19–41 weeks) | 1st formula: from 74.7 to 63.2 (19–41 weeks) 2nd formula: from 73.5 to 63.3 (19–41 weeks) |
| 10 | Tchirikov et al., 2002 [38] | Retrospective, cross- sectional clinical study | 85 | 17 to 41 weeks | of whom 15 had poor fetal outcomes | No | iVmean × π(D/2)2 | 17 * | −2.2 ** |
| 11 | Kiserud et al., 2000 [41] | Prospective cross-sectional study | 197 | 18 to 41 weeks | Singleton low-risk pregnancies | No | Vwmean × π × (D/2)2 | ||
| 12 | Tchirikov et al., 1998 [43] | Prospective cross-sectional study | −75 (singleton) −10 (twin pregnancies) | 100 to 300 days | Singleton: −55 low-risk £ −20 FGR | No | |||
| Both at free-floating and intra-abdominal portions | |||||||||
| 13 | Wang et al., 2021 [39] | Prospective cross-sectional study | 907 | 20 to 39 weeks | Singleton low-risk pregnancies | No | iVmean × 60 × π(D/2)2 | FL: from 32.6 to 381.9 (20–39 weeks) IA: from 31.5 to 360.1 (20–39 weeks) | |
| 14 | Bellotti et al., 2000 [42] | Prospective cross-sectional study | 137 | 20 to 38 weeks | Singleton low-risk pregnancies | No | 0.5 × TaMXV × π × (D/2)2 | ||
| Population (n = 255) | |
|---|---|
| Maternal age (years) | 33 (29–36) |
| Non-Caucasian ethnicity | 3 (1.2%) |
| Maternal pre-pregnancy BMI (kg/m2) | 22 (20–24) |
| Nulliparous | 122 (47.7%) |
| EFW percentile | 50 (36–63) |
| GA at delivery | 40+3 (39+1–40+5) |
| Birthweight (g) | 3420 (3175–3645) |
| Male fetuses | 133 (52.2%) |
| UV-Q | UV-Q/EFW | UV-Q/AC | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GA (Weeks) | 5th | 10th | 50th | 90th | 95th | 5th | 10th | 50th | 90th | 95th | 5th | 10th | 50th | 90th | 95th |
| 20 | 28 | 31 | 45 | 60 | 64 | 92 | 101 | 137 | 174 | 51 | 0.19 | 0.21 | 0.30 | 0.41 | 0.44 |
| 21 | 36 | 40 | 57 | 75 | 80 | 95 | 103 | 139 | 178 | 66 | 0.21 | 0.24 | 0.35 | 0.47 | 0.51 |
| 22 | 45 | 50 | 69 | 92 | 98 | 97 | 105 | 140 | 181 | 95 | 0.24 | 0.27 | 0.39 | 0.53 | 0.57 |
| 23 | 55 | 60 | 83 | 109 | 117 | 99 | 106 | 141 | 183 | 112 | 0.27 | 0.30 | 0.43 | 0.59 | 0.63 |
| 24 | 65 | 71 | 97 | 128 | 136 | 99 | 106 | 141 | 184 | 132 | 0.29 | 0.33 | 0.48 | 0.64 | 0.70 |
| 25 | 76 | 82 | 112 | 147 | 156 | 98 | 105 | 139 | 182 | 154 | 0.32 | 0.36 | 0.52 | 0.70 | 0.75 |
| 26 | 85 | 93 | 129 | 165 | 175 | 96 | 103 | 136 | 177 | 176 | 0.34 | 0.38 | 0.55 | 0.75 | 0.81 |
| 27 | 95 | 103 | 140 | 182 | 194 | 93 | 99 | 131 | 171 | 198 | 0.36 | 0.41 | 0.59 | 0.80 | 0.86 |
| 28 | 104 | 113 | 154 | 200 | 212 | 89 | 95 | 126 | 163 | 220 | 0.38 | 0.43 | 0.62 | 0.84 | 0.91 |
| 29 | 112 | 122 | 167 | 217 | 230 | 84 | 91 | 121 | 154 | 241 | 0.40 | 0.45 | 0.65 | 0.88 | 0.96 |
| 30 | 120 | 131 | 181 | 234 | 248 | 80 | 87 | 116 | 147 | 261 | 0.42 | 0.47 | 0.68 | 0.92 | 1.00 |
| 31 | 127 | 140 | 194 | 252 | 267 | 76 | 83 | 111 | 140 | 281 | 0.44 | 0.49 | 0.71 | 0.96 | 1.04 |
| 32 | 135 | 149 | 208 | 270 | 286 | 73 | 80 | 108 | 135 | 300 | 0.45 | 0.51 | 0.73 | 0.99 | 1.07 |
| 33 | 142 | 158 | 222 | 289 | 307 | 70 | 77 | 104 | 131 | 319 | 0.47 | 0.53 | 0.76 | 1.03 | 1.11 |
| 34 | 148 | 166 | 235 | 307 | 328 | 67 | 74 | 101 | 127 | 337 | 0.48 | 0.54 | 0.78 | 1.05 | 1.14 |
| 35 | 153 | 173 | 247 | 326 | 349 | 64 | 71 | 98 | 124 | 355 | 0.49 | 0.55 | 0.80 | 1.08 | 1.17 |
| 36 | 157 | 178 | 258 | 344 | 369 | 60 | 67 | 94 | 121 | 371 | 0.50 | 0.57 | 0.81 | 1.1 | 1.19 |
| 37 | 159 | 182 | 267 | 360 | 389 | 55 | 62 | 91 | 119 | 385 | 0.51 | 0.58 | 0.83 | 1.12 | 1.21 |
| 38 | 158 | 184 | 274 | 376 | 409 | 50 | 57 | 87 | 117 | 397 | 0.52 | 0.59 | 0.84 | 1.14 | 1.23 |
| 39 | 156 | 183 | 279 | 389 | 428 | 45 | 53 | 83 | 115 | 406 | 0.53 | 0.60 | 0.86 | 1.16 | 1.25 |
| 40 | 150 | 181 | 282 | 402 | 446 | 39 | 48 | 80 | 113 | 415 | 0.54 | 0.60 | 0.87 | 1.17 | 1.27 |
| 41 | 143 | 176 | 283 | 412 | 464 | 34 | 43 | 76 | 111 | 422 | 0.54 | 0.61 | 0.88 | 1.19 | 1.29 |
| UV-Q | UV-Q/EFW | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GA (Weeks) | Sutton 1990 | Bellotti 2000 | Boito 2003 | Flo 2010 | DeVore 2021 | Wang 2021 | GA (Weeks) | Sutton 1990 | Barbera 1999 | Bellotti 2000 | Flo 2010 | DeVore 2021 |
| 22 | −0.56 | −1.92 | −0.67 | −0.25 | −0.33 | −0.34 | 22 | 0.32 | −0.65 | −0.79 | −0.28 | −0.56 |
| 23 | −0.60 | −1.36 | −0.50 | −0.18 | −0.09 | 0.04 | 23 | 0.13 | −0.45 | −0.56 | −0.25 | −0.25 |
| 24 | −0.68 | −1.32 | −0.50 | −0.14 | −0.04 | 0.21 | 24 | 0.07 | −0.45 | −0.52 | −0.27 | −0.17 |
| 25 | −1.18 | −2.10 | −0.83 | −0.24 | 0.00 | 0.48 | 25 | 0.13 | −0.63 | −0.74 | −0.41 | −0.18 |
| 26 | −1.05 | −1.85 | −0.75 | −0.19 | 0.07 | 0.56 | 26 | 0.21 | −0.63 | −0.79 | −0.42 | −0.17 |
| 27 | −1.02 | −1.80 | −0.76 | −0.13 | 0.13 | 0.67 | 27 | 0.39 | −0.55 | −0.69 | −0.32 | −0.05 |
| 28 | −0.86 | −1.57 | −0.70 | −0.08 | 0.14 | 0.68 | 28 | 0.40 | −0.27 | −0.37 | −0.17 | 0.03 |
| 29 | −0.69 | −1.39 | −0.63 | −0.02 | 0.16 | 0.70 | 29 | 0.64 | −0.21 | −0.29 | −0.12 | 0.08 |
| 30 | −0.61 | −1.39 | −0.66 | 0.00 | 0.17 | 0.78 | 30 | 0.76 | −0.04 | −0.12 | 0.00 | 0.12 |
| 31 | −0.53 | −1.49 | −0.75 | 0.05 | 0.19 | 0.98 | 31 | 1.07 | 0.14 | 0.05 | 0.10 | 0.14 |
| 32 | −0.39 | −1.55 | −0.83 | 0.07 | 0.17 | 1.12 | 32 | 1.67 | 0.28 | 0.21 | 0.14 | 0.14 |
| 33 | −0.14 | −1.18 | −0.68 | 0.07 | 0.07 | 0.95 | 33 | 1.09 | 0.29 | 0.25 | 0.12 | 0.04 |
| 34 | 0.10 | −1.36 | −0.84 | 0.13 | 0.04 | 1.23 | 34 | 1.55 | 0.50 | 0.44 | 0.11 | 0.00 |
| 35 | 0.43 | −1.20 | −0.80 | 0.18 | 0.00 | 1.30 | 35 | 1.72 | 0.58 | 0.64 | 0.12 | −0.12 |
| 36 | 0.53 | −0.69 | −0.50 | 0.15 | −0.03 | 0.91 | 36 | 1.33 | 0.54 | 0.58 | 0.08 | −0.08 |
| 37 | 1.00 | −0.68 | −0.55 | 0.26 | −0.04 | 1.20 | 37 | 1.42 | 0.64 | 0.68 | 0.08 | −0.13 |
| 38 | 1.79 | −0.63 | −0.59 | 0.44 | −0.07 | 1.67 | 38 | 1.89 | 0.89 | 1.00 | 0.11 | −0.16 |
| 39 | 1.75 | −0.27 | −0.34 | 0.42 | −0.04 | 1.35 | 39 | 1.67 | 0.87 | 1.00 | 0.09 | −0.13 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbieri, M.; Zamagni, G.; Fantasia, I.; Monasta, L.; Lo Bello, L.; Quadrifoglio, M.; Ricci, G.; Maso, G.; Piccoli, M.; Di Martino, D.D.; et al. Umbilical Vein Blood Flow in Uncomplicated Pregnancies: Systematic Review of Available Reference Charts and Comparison with a New Cohort. J. Clin. Med. 2023, 12, 3132. https://doi.org/10.3390/jcm12093132
Barbieri M, Zamagni G, Fantasia I, Monasta L, Lo Bello L, Quadrifoglio M, Ricci G, Maso G, Piccoli M, Di Martino DD, et al. Umbilical Vein Blood Flow in Uncomplicated Pregnancies: Systematic Review of Available Reference Charts and Comparison with a New Cohort. Journal of Clinical Medicine. 2023; 12(9):3132. https://doi.org/10.3390/jcm12093132
Chicago/Turabian StyleBarbieri, Moira, Giulia Zamagni, Ilaria Fantasia, Lorenzo Monasta, Leila Lo Bello, Mariachiara Quadrifoglio, Giuseppe Ricci, Gianpaolo Maso, Monica Piccoli, Daniela Denis Di Martino, and et al. 2023. "Umbilical Vein Blood Flow in Uncomplicated Pregnancies: Systematic Review of Available Reference Charts and Comparison with a New Cohort" Journal of Clinical Medicine 12, no. 9: 3132. https://doi.org/10.3390/jcm12093132
APA StyleBarbieri, M., Zamagni, G., Fantasia, I., Monasta, L., Lo Bello, L., Quadrifoglio, M., Ricci, G., Maso, G., Piccoli, M., Di Martino, D. D., Ferrazzi, E. M., & Stampalija, T. (2023). Umbilical Vein Blood Flow in Uncomplicated Pregnancies: Systematic Review of Available Reference Charts and Comparison with a New Cohort. Journal of Clinical Medicine, 12(9), 3132. https://doi.org/10.3390/jcm12093132









