A Monocortical Screw for Preventing Trochanteric Escape in Extended Trochanteric Osteotomy: A Simple Solution to a Complicated Problem?
Abstract
1. Introduction
2. Surgical Technique
2.1. Extended Trochanteric Osteotomy
2.1.1. The Surgical Technique
2.1.2. The Postoperative Regime
2.2. The Problem: Trochanteric Escape after ETO
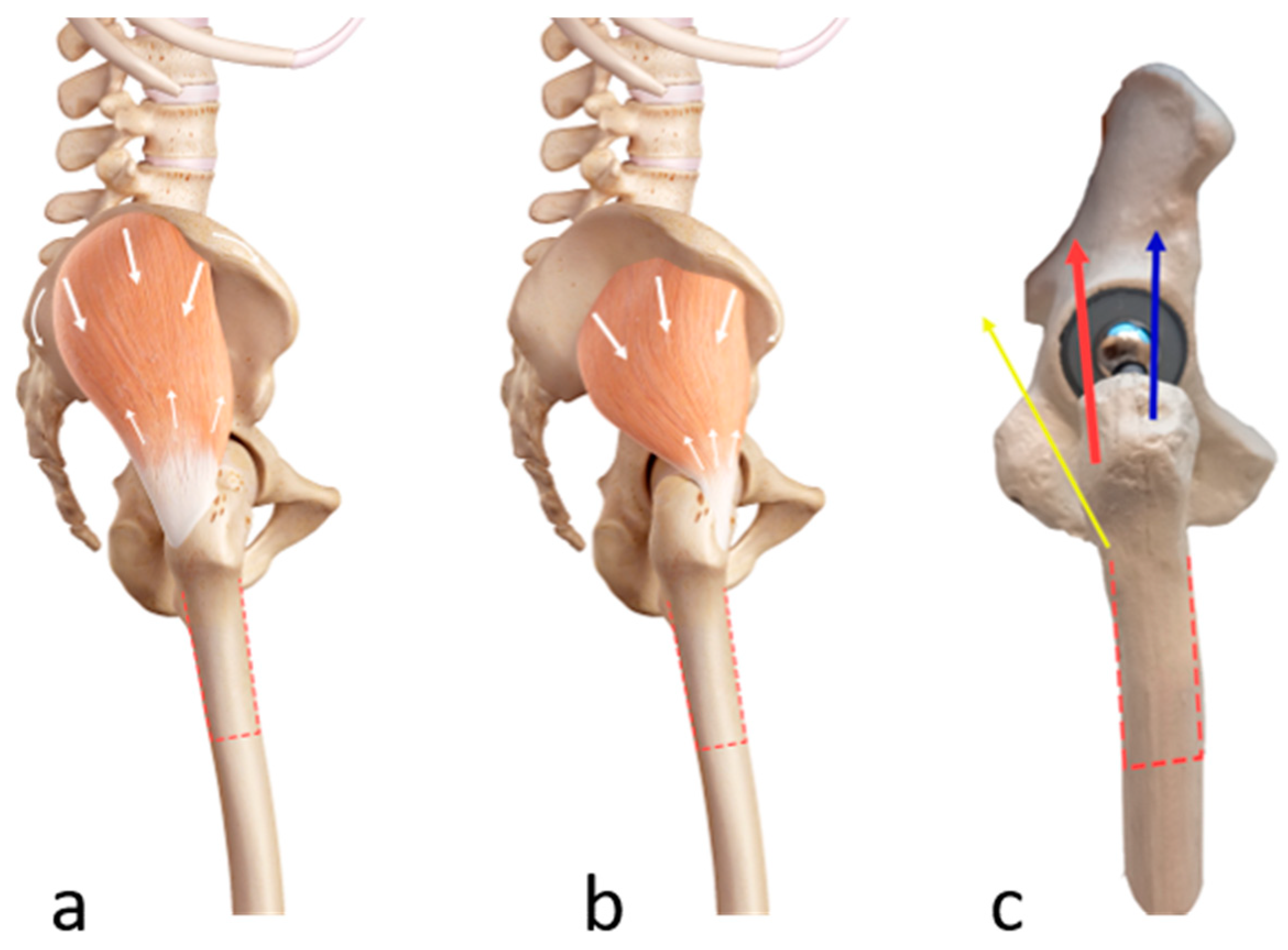
2.2.1. Biomechanical Principles of Trochanteric Escape
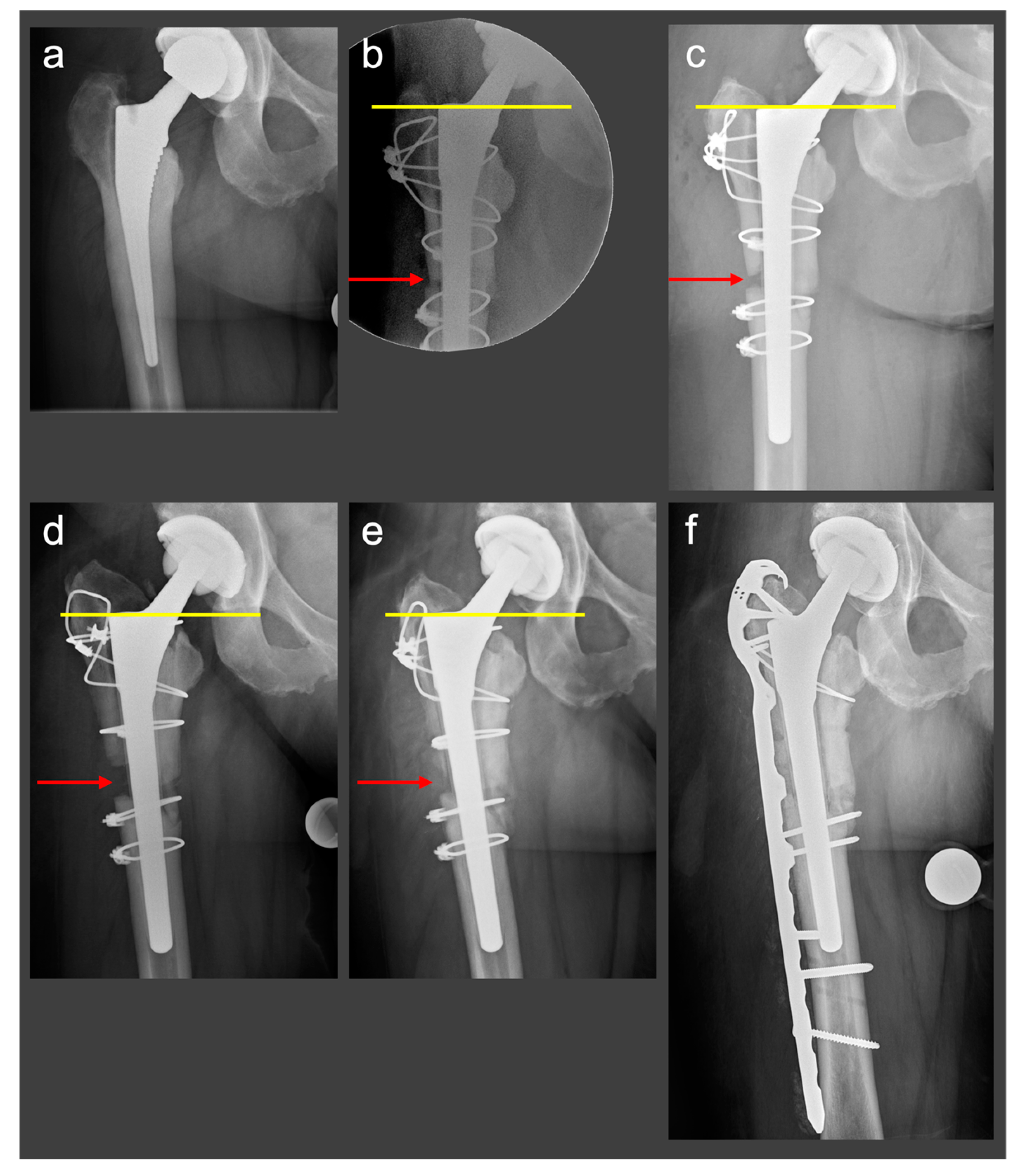
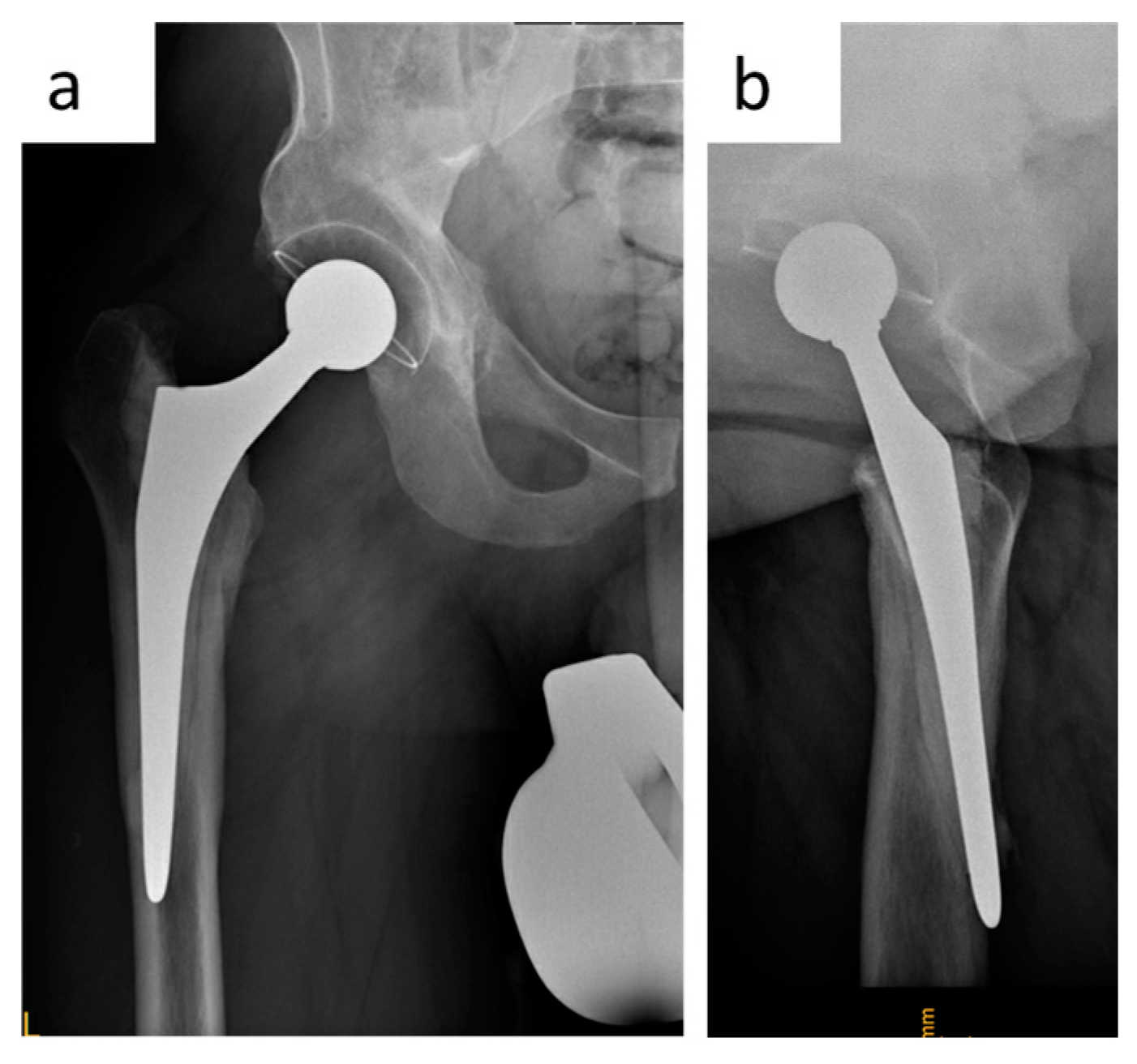
2.2.2. Clinical Case
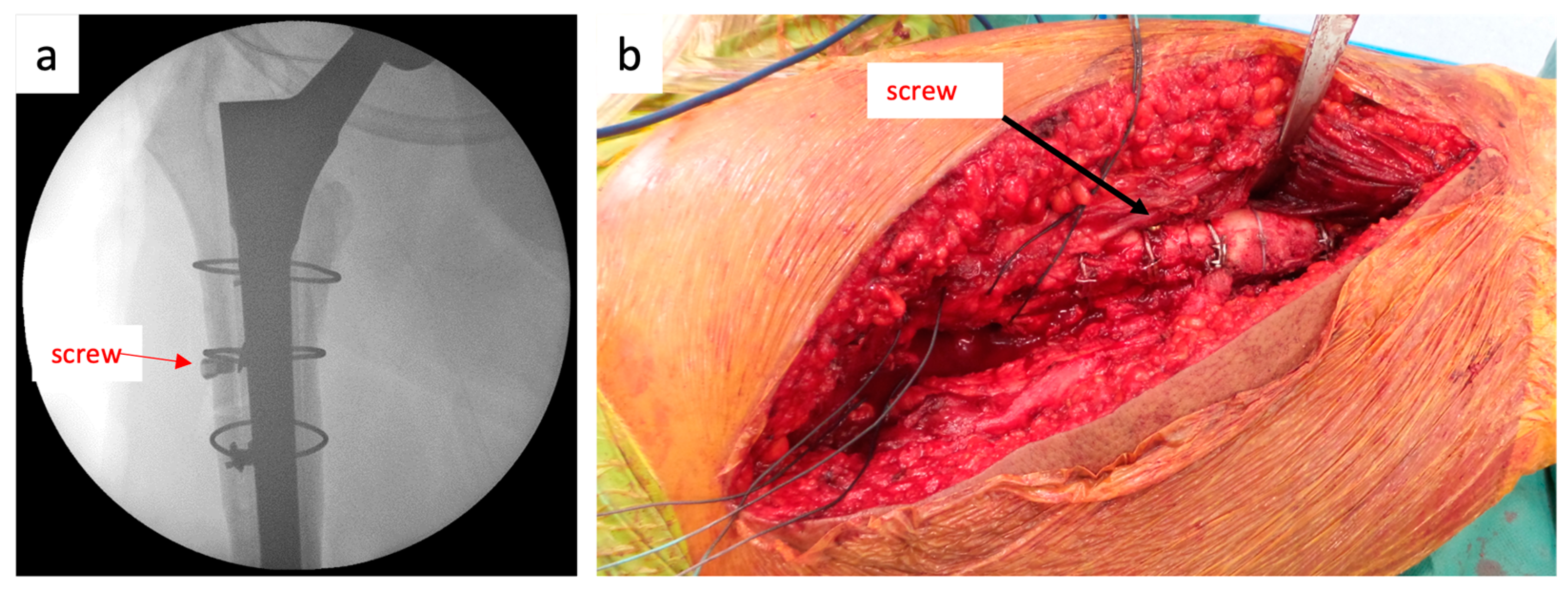
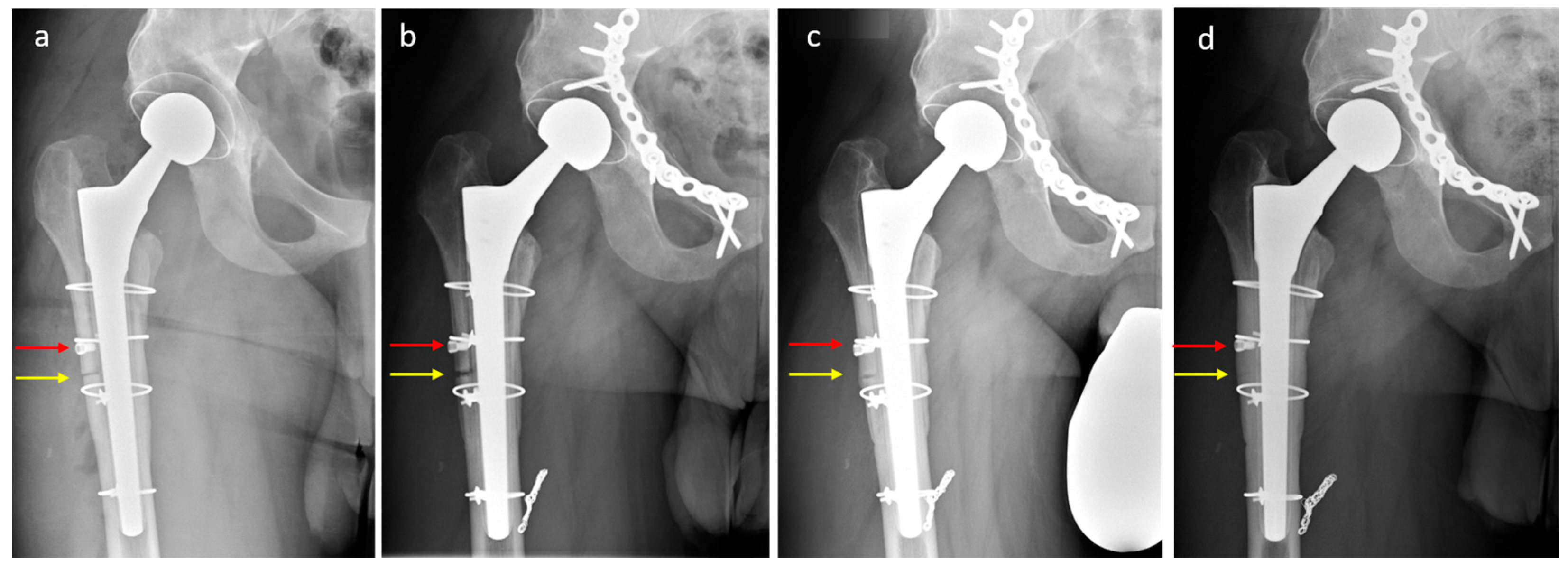
2.3. Novel Surgical Technique: A Monocortical Screw for Preventing Trochanteric Escape
2.3.1. The Surgical Technique
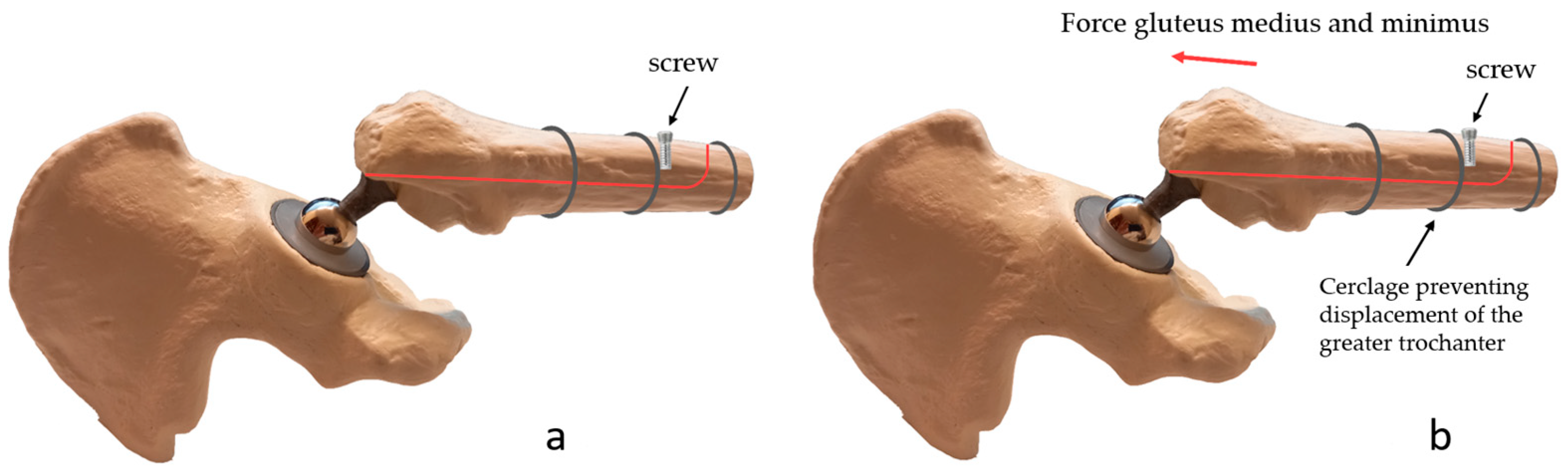
2.3.2. Biomechanical Principles
2.3.3. Clinical Case
3. Discussion
3.1. Trochanteric Escape: Available Solutions
3.1.1. Partial Weight-Bearing, Abduction Restriction
3.1.2. Surgical Options to Prevent Trochanteric Escape
3.2. A Monocortical Screw for Preventing Trochanteric Escape: Advantages and Disadvantages
3.3. The Importance of Bony Union in ETO
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef] [PubMed]
- Murphy, L.B.; Helmick, C.G.; Schwartz, T.A.; Renner, J.B.; Tudor, G.; Koch, G.G.; Dragomir, A.D.; Kalsbeek, W.D.; Luta, G.; Jordan, J.M. One in four people may develop symptomatic hip osteoarthritis in his or her lifetime. Osteoarthr. Cartil. 2010, 18, 1372–1379. [Google Scholar] [CrossRef] [PubMed]
- Park, J.W.; Won, S.H.; Moon, S.Y.; Lee, Y.K.; Ha, Y.C.; Koo, K.H. Burden and future projection of revision Total hip Arthroplasty in South Korea. BMC. Musculoskelet. Disord. 2021, 22, 375. [Google Scholar] [CrossRef] [PubMed]
- Sambandam, S.N.; Duraisamy, G.; Chandrasekharan, J.; Mounasamy, V. Extended trochanteric osteotomy: Current concepts review. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 231–245. [Google Scholar] [CrossRef]
- Aribindi, R.; Paprosky, W.; Nourbash, P.; Kronick, J.; Barba, M. Extended proximal femoral osteotomy. Instr. Course Lect. 1999, 48, 19–26. [Google Scholar] [CrossRef]
- Lerch, M.; Von Lewinski, G.; Windhagen, H.; Thorey, F. Revision of total hip arthroplasty: Clinical outcome of extended trochanteric osteotomy and intraoperative femoral fracture. Technol. Health Care 2008, 16, 293–300. [Google Scholar] [CrossRef]
- Mardones, R.; Gonzalez, C.; Cabanela, M.E.; Trousdale, R.T.; Berry, D.J. Extended Femoral Osteotomy for Revision of Hip Arthroplasty: Results and Complications. J. Arthroplast. 2005, 20, 79–83. Available online: https://pubmed.ncbi.nlm.nih.gov/15660064/ (accessed on 29 November 2022). [CrossRef]
- Sundaram, K.; Siddiqi, A.; Kamath, A.F.; Higuera-Rueda, C.A. Trochanteric osteotomy in revision total hip arthroplasty. EFORT Open Rev. 2020, 5, 477–485. [Google Scholar] [CrossRef]
- Amin, A.K.; Bergman, N. Trochanteric non-union following revision hip replacement is associated with a poor functional outcome: A matched, case-control study. Hip Int. 2013, 23, 535–540. [Google Scholar] [CrossRef]
- Hawkins, A.; Midwinter, K.; Macdonald, D.A. Trochanteric non-union in revision total hip arthroplasty: Does it matter? Ann. R. Coll. Surg. Engl. 2000, 82, 39–42. [Google Scholar]
- Mehra, A.; Hemmady, M.V.; Hodgkinson, J.P. Trochanteric non-union—Does it influence the rate of revision following primary total hip replacement? A minimum of 15 years follow-up. Surgeon 2008, 6, 79–82. [Google Scholar] [CrossRef]
- Malahias, M.A.; Gkiatas, I.; Selemon, N.A.; De Filippis, R.; Gu, A.; Greenberg, A.; Sculco, P.K. Outcomes and Risk Factors of Extended Trochanteric Osteotomy in Aseptic Revision Total Hip Arthroplasty: A Systematic Review. J. Arthroplasty 2020, 35, 3410–3416. [Google Scholar] [CrossRef]
- Huffman, G.R.; Ries, M.D. Combined vertical and horizontal cable fixation of an extended trochanteric osteotomy site. J. Bone Jt. Surg. 2003, 85, 273–277. [Google Scholar] [CrossRef]
- Kuruvalli, R.R.; Landsmeer, R.; Debnath, U.K.; Suresh, S.P.; Thomas, T.L. A new technique to reattach an extended trochanteric osteotomy in revision THA using suture cord. Clin. Orthop. Relat. Res. 2008, 466, 1444–1448. [Google Scholar] [CrossRef]
- Smith, E.B. Save the Greater Trochanter: A Novel Modification to the Extended Trochanteric Osteotomy. Arthroplast. Today 2022, 16, 107–111. [Google Scholar] [CrossRef]
- Tang, J.; Wu, T.; Shao, H.; Zhou, Y. Greater trochanter fixed with a claw plate and cable system in complex primary and revision total hip arthroplasty: Long-term follow-up. Int. Orthop. 2022, 46, 2553–2560. [Google Scholar] [CrossRef]
- Younger, T.I.; Bradford, M.S.; Magnus, R.E.; Paprosky, W.G. Extended proximal femoral osteotomy: A new technique for femoral revision arthroplasty. J. Arthroplasty 1995, 10, 329–338. [Google Scholar] [CrossRef]
- Gandbhir, V.N.; Lam, J.C.; Rayi, A. Trendelenburg Gait; StatPearls: Tampa, FL, USA, 2022. [Google Scholar]
- Hersh, C.K.; Williams, R.P.; Trick, L.W.; Lanctot, D.; Athanasiou, K. Comparison of the mechanical performance of trochanteric fixation devices. Clin. Orthop. Relat. Res. 1996, 329, 317–325. [Google Scholar] [CrossRef]
- Kendall, F.P.; McCreary, E.K.; Provance, P.G.; Rodgers, M.M.; Romani, W.A. Muscles: Testing and Function with Posture and Pain; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2005; Volume 5. [Google Scholar]
- Neumann, D.A. Kinesiology of the hip: A focus on muscular actions. J. Orthop. Sports Phys. Ther. 2010, 40, 82–94. [Google Scholar] [CrossRef]
- Palastanga, N.; Field, D.; Soames, R. Anatomy and Human Movement: Structure and Function; Elsevier Health Sciences: Amsterdam, The Netherlands, 2006; Volume 20056. [Google Scholar]
- Michalik, R.; Essing, K.; Rohof, B.; Gatz, M.; Migliorini, F.; Betsch, M. Do hip-abduction braces work? A biomechanical evaluation of a commercially available hip brace. Arch. Orthop. Trauma Surg. 2022, 142, 1275–1281. [Google Scholar] [CrossRef]
- Dewal, H.; Maurer, S.L.; Tsai, P.; Su, E.; Hiebert, R.; Di Cesare, P.E. Efficacy of abduction bracing in the management of total hip arthroplasty dislocation. J. Arthroplasty 2004, 19, 733–738. [Google Scholar] [CrossRef] [PubMed]
- Murray, T.G.; Wetters, N.G.; Moric, M.; Sporer, S.M.; Paprosky, W.G.; Della Valle, C.J. The use of abduction bracing for the prevention of early postoperative dislocation after revision total hip arthroplasty. J. Arthroplasty 2012, 27, 126–129. [Google Scholar] [CrossRef] [PubMed]
- Vincent, H.K.; Dejong, G.; Mascarenas, D.; Vincent, K.R. The effect of body mass index and hip abductor brace use on inpatient rehabilitation outcomes after total hip arthroplasty. Am. J. Phys. Med. Rehabil. 2009, 88, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Jeong, D.E.; Lee, S.K.; Kim, K. Comparison of the activity of the gluteus medius according to the angles of inclination of a treadmill with vertical load. J. Phys. Ther. Sci. 2014, 26, 251–253. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.K.; Weiss, L.; Lehmkuhl, L.D. Brunnstrom’s Clinical Kinesiology; F.A. Davis Company: Philadelphia, PA, USA, 1996. [Google Scholar]
- Eickhoff, A.M.; Cintean, R.; Fiedler, C.; Gebhard, F.; Schütze, K.; Richter, P.H. Analysis of partial weight bearing after surgical treatment in patients with injuries of the lower extremity. Arch. Orthop. Trauma Surg. 2022, 142, 77–81. [Google Scholar] [CrossRef]
- Mei, X.Y.; Gong, Y.J.; Safir, O.A.; Gross, A.E.; Kuzyk, P.R. Fixation Options Following Greater Trochanteric Osteotomies and Fractures in Total Hip Arthroplasty: A Systematic Review. JBJS Rev. 2018, 6, e4. [Google Scholar] [CrossRef]
- Fakih, R.R.; Treacy, R.B.C. Articular interposition of broken trochanteric wires. Bull. Hosp. Jt. Dis. 1998, 57, 108–110. [Google Scholar]
- Makki, D.Y.; Goru, P.; Prakash, V.; Aldam, C.H. Migration of a broken trochanteric wire to the popliteal fossa. J. Arthroplasty 2011, 26, 504.e1–504.e3. [Google Scholar] [CrossRef]
- Leonardi, F.; Rivera, F. Intravascular migration of a broken cerclage wire into the left heart. Orthopedics 2014, 37, e932–e935. [Google Scholar] [CrossRef]
- Chang, A.; Hayes, K.; Dunlop, D.; Song, J.; Hurwitz, D.; Cahue, S.; Sharma, L. Hip abduction moment and protection against medial tibiofemoral osteoarthritis progression. Arthritis Rheum. 2005, 52, 3515–3519. [Google Scholar] [CrossRef]
- Cinnamon, C.C.; Longworth, J.A.; Brunner, J.H.; Chau, V.K.; Ryan, C.A.; Dapiton, K.R.; Foucher, K.C. Static and dynamic abductor function are both associated with physical function 1 to 5 years after total hip arthroplasty. Clin. Biomech. 2019, 67, 127–133. [Google Scholar] [CrossRef]
- Piva, S.R.; Goodnite, E.A.; Childs, J.D. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J. Orthop. Sports Phys. Ther. 2005, 35, 793–801. [Google Scholar] [CrossRef]
- Cooper, N.A.; Scavo, K.M.; Strickland, K.J.; Tipayamongkol, N.; Nicholson, J.D.; Bewyer, D.C.; Sluka, K.A. Prevalence of gluteus medius weakness in people with chronic low back pain compared to healthy controls. Eur. Spine J. 2016, 25, 1258–1265. [Google Scholar] [CrossRef]
- Horstmann, T.; Listringhaus, R.; Brauner, T.; Grau, S.; Mündermann, A. Minimizing preoperative and postoperative limping in patients after total hip arthroplasty: Relevance of hip muscle strength and endurance. Am. J. Phys. Med. Rehabil. 2013, 92, 1060–1069. [Google Scholar] [CrossRef]
- Inacio, M.; Ryan, A.S.; Bair, W.N.; Prettyman, M.; Beamer, B.A.; Rogers, M.W. Gluteal muscle composition differentiates fallers from non-fallers in community dwelling older adults. BMC Geriatr. 2014, 14, 37. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ismailidis, P.; Mündermann, A.; Stoffel, K. A Monocortical Screw for Preventing Trochanteric Escape in Extended Trochanteric Osteotomy: A Simple Solution to a Complicated Problem? J. Clin. Med. 2023, 12, 2947. https://doi.org/10.3390/jcm12082947
Ismailidis P, Mündermann A, Stoffel K. A Monocortical Screw for Preventing Trochanteric Escape in Extended Trochanteric Osteotomy: A Simple Solution to a Complicated Problem? Journal of Clinical Medicine. 2023; 12(8):2947. https://doi.org/10.3390/jcm12082947
Chicago/Turabian StyleIsmailidis, Petros, Annegret Mündermann, and Karl Stoffel. 2023. "A Monocortical Screw for Preventing Trochanteric Escape in Extended Trochanteric Osteotomy: A Simple Solution to a Complicated Problem?" Journal of Clinical Medicine 12, no. 8: 2947. https://doi.org/10.3390/jcm12082947
APA StyleIsmailidis, P., Mündermann, A., & Stoffel, K. (2023). A Monocortical Screw for Preventing Trochanteric Escape in Extended Trochanteric Osteotomy: A Simple Solution to a Complicated Problem? Journal of Clinical Medicine, 12(8), 2947. https://doi.org/10.3390/jcm12082947






