Clinical Characteristics and In-Hospital Outcomes in Patients with Iliopsoas Abscess: A Multicenter Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Patient Selection and Data Collection
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics between Survivors and Non-Survivors
3.2. Distribution of IPA According to Origin
3.3. Microbiology Results
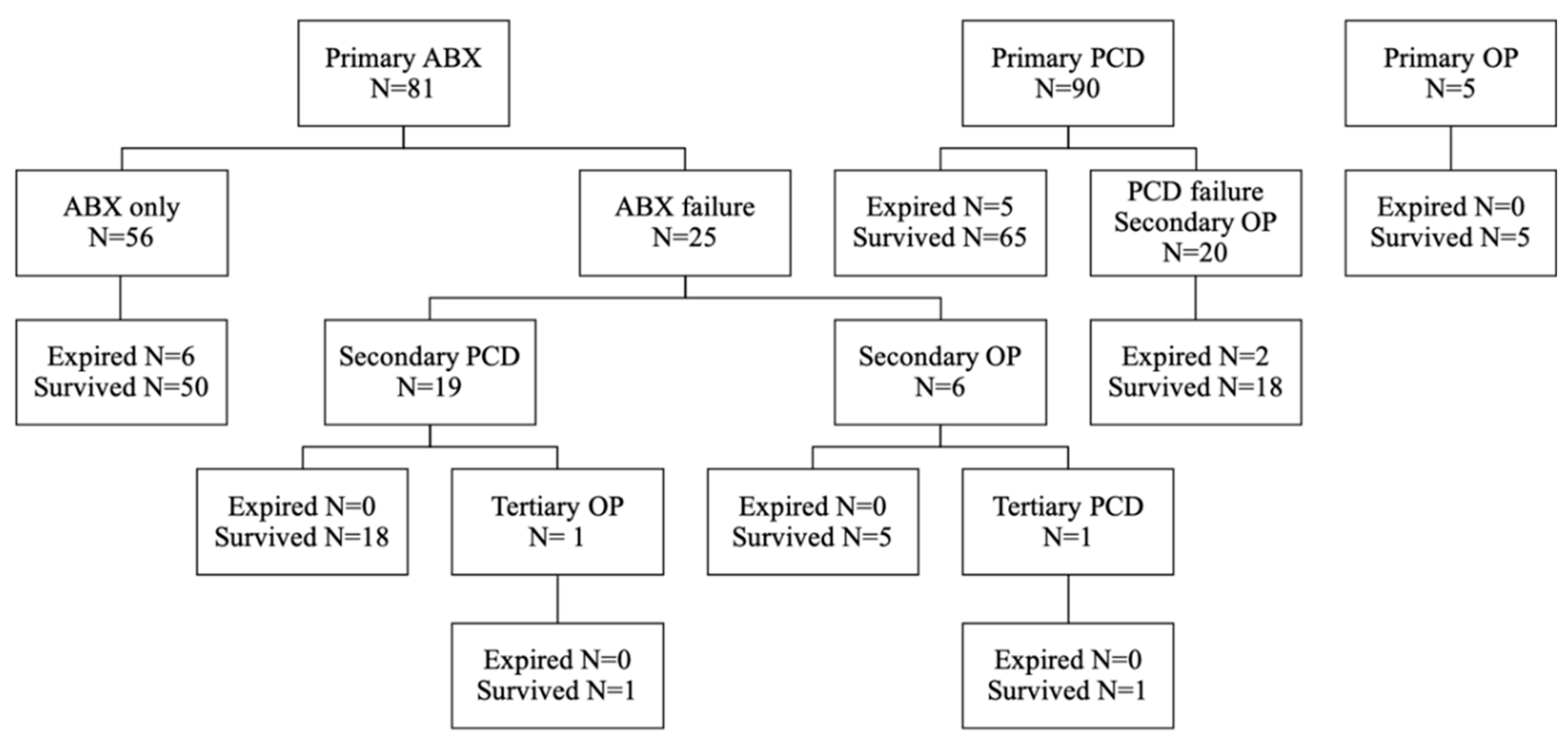
3.4. Treatment and Outcomes
3.5. Univariate and Multivariate Analyses of Predictors of In-Hospital Mortality, Longer LOS, and Recurrence
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mynter, H. Acute psoitis. Buffalo. Med. Surg. J. 1881, 2, 202–210. [Google Scholar]
- López, V.N.; Ramos, J.M.; Meseguer, V.; Arellano, J.L.P.; Serrano, R.; Ordóñez, M.A.G.; Peralta, G.; Boix, V.; Pardo, J.; Conde, A.; et al. Microbiology and outcome of iliopsoas abscess in 124 patients. Medicine 2009, 88, 120–130. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, M.S.; Huang, S.C.; Loh, E.W.; Tsai, C.A.; Hung, Y.Y.; Tsan, Y.T.; Huang, J.A.; Wang, L.M.; Hu, S.Y. Features and treatment modality of iliopsoas abscess and its outcome: A 6-year hospital-based study. BMC Infect. Dis. 2013, 9, 578. [Google Scholar] [CrossRef] [PubMed]
- Chern, C.H.; Hu, S.C.; Kao, W.F.; Tsai, J.; Yen, D.; Lee, C.H. Psoas abscess: Making an early diagnosis in the, E.D. Am. J. Emerg. Med. 1997, 15, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Ouellette, L.; Hamati, M.; Flannigan, M.; Singh, M.; Bush, C.; Jones, J. Epidemiology of and risk factors for iliopsoas abscess in a large community-based study. Am. J. Emerg. Med. 2019, 37, 158–159. [Google Scholar] [CrossRef]
- Ricci, M.A.; Rose, F.B.; Meyer, K.K. Pyogenic psoas abscess: Worldwide variations in etiology. World J. Surg. 1986, 10, 834–843. [Google Scholar] [CrossRef]
- Shields, D.; Robinson, P.; Crowley, T.P. Iliopsoas abscess—A review and update on the literature. Int. J. Surg. 2012, 10, 466–469. [Google Scholar] [CrossRef]
- Mallick, I.H.; Thoufeeq, M.H.; Rajendran, T.P. Iliopsoas abscesses. Postgrad. Med. J. 2004, 80, 459–462. [Google Scholar] [CrossRef]
- Santaella, R.O.; Fishman, E.K.; Lipsett, P.A. Primary vs secondary iliopsoas abscess. Presentation, microbiology, and treatment. Arch. Surg. 1995, 130, 1309–1313. [Google Scholar] [CrossRef]
- Laguna, P.; Moya, M. Abscess of the psoas muscle: Analysis of 11 cases and review of the literature. Enferm. Infecc. Microbiol. Clin. 1998, 16, 19–24. [Google Scholar]
- De, U.; Pal, D.K. Seventy cases of non-tubercular psoas abscess at a rural referral centre in South Bengal. Trop. Doct. 2006, 36, 53–54. [Google Scholar] [CrossRef] [PubMed]
- Thakral, A.; Prasad, D.; Katyal, S.; Kumar, A. Characteristics and Outcomes of Psoas Abscess: Experience from a Tertiary Care Center in North India. Cureus 2022, 14, e21358. [Google Scholar] [CrossRef] [PubMed]
- Hamano, S.; Kiyoshima, K.; Nakatsu, H.; Murakami, S.; Igarashi, T.; Ito, H. Pyogenic psoas abscess: Difficulty in early diagnosis. Urol. Int. 2003, 71, 178–183. [Google Scholar] [CrossRef]
- Dietrich, A.; Vaccarezza, H.; Vaccaro, C.A. Iliopsoas abscess: Presentation, management, and outcomes. Surg. Laparosc. Endosc. Percutan. Tech. 2013, 23, 45–48. [Google Scholar] [CrossRef]
- Hu, S.Y.; Hsieh, M.S.; Chang, Y.T.; Huang, C.C.; Tsai, C.A.; Tsai, C.L.; Hsu, C.Y.; Shen, C.H.; Chang, Y.Z. Clinical features, management, and outcome of iliopsoas abscess associated with cardiovascular disorders: A hospital-based observational case series study. BMC Musculoskelet. Disord. 2019, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Yoon, J.H.; Kim, S.I.; Wie, S.H.; Kim, Y.R. Etiology and outcome of iliopsoas muscle abscess in Korea; changes over a decade. Int. J. Surg. 2013, 11, 1056–1059. [Google Scholar] [CrossRef]
- Gruenwald, I.; Abrahamson, J.; Cohen, O. Psoas abscess: Case report and review of the literature. J. Urol. 1992, 147, 1624–1626. [Google Scholar] [CrossRef] [PubMed]
- Dauchy, F.-A.; Dupon, M.; Dutronc, H.; de Barbeyrac, B.; Lawson-Ayayi, S.; Dubuisson, V.; Souillac, V. Association between psoas abscess and prosthetic hip infection: A case-control study. Acta Orthop. 2009, 80, 198–200. [Google Scholar] [CrossRef]
- Huang, J.-J.; Ruaan, M.-K.; Lan, R.-R.; Wang, M.-C. Acute pyogenic iliopsoas abscess in Taiwan: Clinical features, diagnosis, treatments and outcome. J. Infect. 2000, 40, 248–255. [Google Scholar] [CrossRef]
- Alonso, C.D.; Barclay, S.; Tao, X.; Auwaerter, P.G. Increasing incidence of iliopsoas abscesses with MRSA as a predominant pathogen. J. Infect. 2011, 63, 1–7. [Google Scholar] [CrossRef]
- Navarro López, V.; López García, F.; González Escoda, E.; Gregori Colomé, J.; Muñoz Pérez, A. Psoas abscess in patients infected with the human immunodeficiency virus. Eur. J. Clin. Microbiol. Infect. Dis. 2004, 23, 661–663. [Google Scholar] [CrossRef] [PubMed]
- Heyd, J.; Meallem, R.; Schlesinger, Y.; Rudensky, B.; Hadas-Halpern, I.; Yinnon, A.M.; Raveh, D. Clinical characteristics of patients with psoas abscess due to non-typhi Salmonella. Eur. J. Clin. Microbiol. Infect. Dis. 2003, 22, 770–773. [Google Scholar] [CrossRef] [PubMed]
- Yacoub, W.N.; Sohn, H.J.; Chan, S.; Petrosyan, M.; Vermaire, H.M.; Kelso, R.L.; Towfigh, S.; Mason, R.J. Psoas abscess rarely requires surgical intervention. Am. J. Surg. 2008, 196, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Cantasdemir, M.; Kara, B.; Cebi, D.; Selcuk, N.D.; Numan, F. Computed tomography-guided percutaneous catheter drainage of primary and secondary iliopsoas abscesses. Clin. Radiol. 2003, 58, 811–815. [Google Scholar] [CrossRef]
- Afaq, A.; Jain, B.K.; Dargan, P.; Bhattacharya, S.K.; Rauniyar, R.K.; Kukreti, R. Surgical drainage of primary iliopsoas abscess—Safe and cost-effective treatment. Trop. Doct. 2002, 32, 133–135. [Google Scholar] [CrossRef]
- Tabrizian, P.; Nguyen, S.Q.; Greenstein, A.; Rajhbeharrysingh, U.; Divino, C.M. Management and treatment of iliopsoas abscess. Arch. Surg. 2009, 144, 946–949. [Google Scholar] [CrossRef]
- Nakamura, T.; Morimoto, T.; Katsube, K.; Yamamori, Y.; Mashino, J.; Kikuchi, K. Clinical characteristics of pyogenic spondylitis and psoas abscess at a tertiary care hospital: A retrospective cohort study. J. Orthop. Surg. Res. 2018, 28, 302. [Google Scholar] [CrossRef]
- Lai, Y.-C.; Lin, P.-C.; Wang, W.-S.; Lai, J.-I. An Update on Psoas Muscle Abscess: An 8-Year Experience and Review of Literature. Int. J. Gerontol. 2011, 5, 75–79. [Google Scholar] [CrossRef]
- Yeh, H.-T.; Liau, S.-K.; Niu, K.-Y.; Hsiao, C.-H.; Yeh, C.-C.; Lu, J.-X.; Ng, C.-J.; Yen, C.-C. Clinical Characteristics and In-Hospital Outcomes in Dialysis Patients with Septic Arthritis. Medicina 2022, 58, 401. [Google Scholar] [CrossRef]
- Sato, M.; Iwasa, Y.; Otsubo, S.; Kimata, N.; Takei, T.; Miwa, N.; Akiba, T.; Nitta, K. Psoas abscess in hemodialysis patients. Int. Urol. Nephrol. 2010, 42, 1113–1116. [Google Scholar] [CrossRef]
- Syed-Ahmed, M.; Narayanan, M. Immune dysfunction and risk of infection in chronic kidney disease. Adv. Chronic Kidney Dis. 2019, 26, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Chuang, F.-R.; Lee, C.-H.; Chen, J.-B.; Cheng, Y.-F.; Yang, B.-Y.; Hsu, K.-T.; Wu, M.-S. Extra-renal abscess in chronic hemodialysis patients. Ren. Fail. 2002, 24, 511–521. [Google Scholar] [CrossRef] [PubMed]
- Kawai, Y.; Banshodani, M.; Moriishi, M.; Sato, T.; Shintaku, S.; Masaki, T.; Kawanishi, H. Iliopsoas Abscess in Hemodialysis Patients with End-Stage Kidney Disease. Ther. Apher. Dial. 2019, 23, 534–541. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total (n = 176) | Survivor (n = 163) | Non-Survivor (n = 13) | p Value |
|---|---|---|---|---|
| Age (year) | 63.0 ± 16.4 | 61.9 ± 13.6 | 76.2 ± 13.3 | 0.002 * |
| Male | 114 (64.8) | 107 (65.6) | 7 (53.8) | 0.385 |
| Systolic blood pressure (mmHg) | 130.3 ± 31.1 | 129.8 ± 30.5 | 136.9 ± 38.8 | 0.425 |
| Diastolic blood pressure (mmHg) | 73.1 ± 17.1 | 72.9 ± 16.9 | 76.0 ± 20.2 | 0.527 |
| Heart rate (beats/min) | 101.7 ± 19.5 | 101.8 ± 19.3 | 100.5 ± 23.0 | 0.823 |
| Body temperature (°C) | 37.1 ± 1.0 | 37.1 ± 1.1 | 36.5 ± 0.9 | 0.029 * |
| Respiratory rate (breaths/min) | 19.4 ± 2.9 | 19.2 ± 2.8 | 21.2 ± 3.5 | 0.020 * |
| Bedridden status | 12 (6.8) | 9 (5.5) | 3 (23.1) | 0.047 * |
| Mechanical ventilation | 32 (18.2) | 22 (13.5) | 10 (76.9) | <0.001 * |
| Intensive care unit admission | 38 (21.6) | 28 (17.2) | 10 (76.9) | <0.001 * |
| Renal replacement therapy | 21 (11.9) | 15 (9.2) | 6 (46.2) | 0.001 * |
| Length of hospital stay (day) | 32.4 ± 26.9 | 33.0 ± 26.6 | 26.1 ± 30.3 | 0.371 |
| Recurrence | 34 (19.3) | 34 (20.9) | 0 (0) | |
| Sepsis | 86 (48.9) | 73 (44.8) | 13 (100) | <0.001 * |
| Septic shock | 30 (17.0) | 18 (11) | 12 (92.3) | <0.001 * |
| Abscess features | ||||
| Gas-forming | 71 (40.3) | 63 (38.7) | 8 (61.5) | 0.105 |
| Multiple lobulated | 89 (50.6) | 83 (50.9) | 6 (46.2) | 0.781 |
| Size (cm) | 7.4 ± 4.1 | 7.4 ± 4.0 | 8.1 ± 3.3 | 0.554 |
| Involvement | 0.996 | |||
| Right | 67 (38.1) | 62 (38.0) | 5 (38.5) | |
| Left | 56 (31.8) | 52 (31.9) | 4 (30.8) | |
| Bilateral | 53 (30.1) | 49 (30.1) | 4 (30.8) | |
| Initial presentations | ||||
| Fever | 96 (54.5) | 92 (56.4) | 4 (30.8) | 0.074 |
| Abdominal pain | 40 (22.7) | 35 (21.5) | 5 (38.5) | 0.175 |
| Flank/back pain | 130 (73.9) | 125 (76.7) | 5 (38.5) | 0.006 * |
| Limp | 90 (51.1) | 86 (52.8) | 4 (30.8) | 0.127 |
| Mass | 3 (1.7) | 3 (1.8) | 0 (0) | 1.000 |
| Malaise | 70 (39.8) | 62 (38.0) | 8 (61.5) | 0.096 |
| Comorbidities | ||||
| Hypertension | 83 (47.2) | 78 (47.9) | 5 (38.5) | 0.514 |
| Diabetes mellitus | 66 (37.5) | 62 (38.0) | 4 (30.8) | 0.769 |
| CAD | 15 (8.5) | 14 (8.6) | 1 (7.7) | 1.000 |
| CKD | 32 (18.2) | 28 (17.2) | 4 (30.8) | 0.258 |
| CHF | 9 (5.1) | 5 (3.1) | 4 (30.8) | 0.002 * |
| Malignancy | 21 (11.9) | 19 (11.7) | 2 (15.4) | 0.656 |
| Prior stroke | 11 (6.3) | 10 (6.1) | 1 (7.7) | 0.581 |
| Intravenous drug abuse | 21 (11.9) | 21 (12.9) | 0 (0) | 0.370 |
| HIV infection | 4 (2.3) | 4 (2.5) | 0 (0) | 1.000 |
| Liver cirrhosis | 12 (6.8) | 11 (6.7) | 1 (7.7) | 1.000 |
| Prior TB history | 1 (0.6) | 3 (1.8) | 0 (0) | 1.000 |
| Imaging modalities | ||||
| Computed tomography | 172 (97.7) | 159 (97.5) | 13 (100.0) | 1.000 |
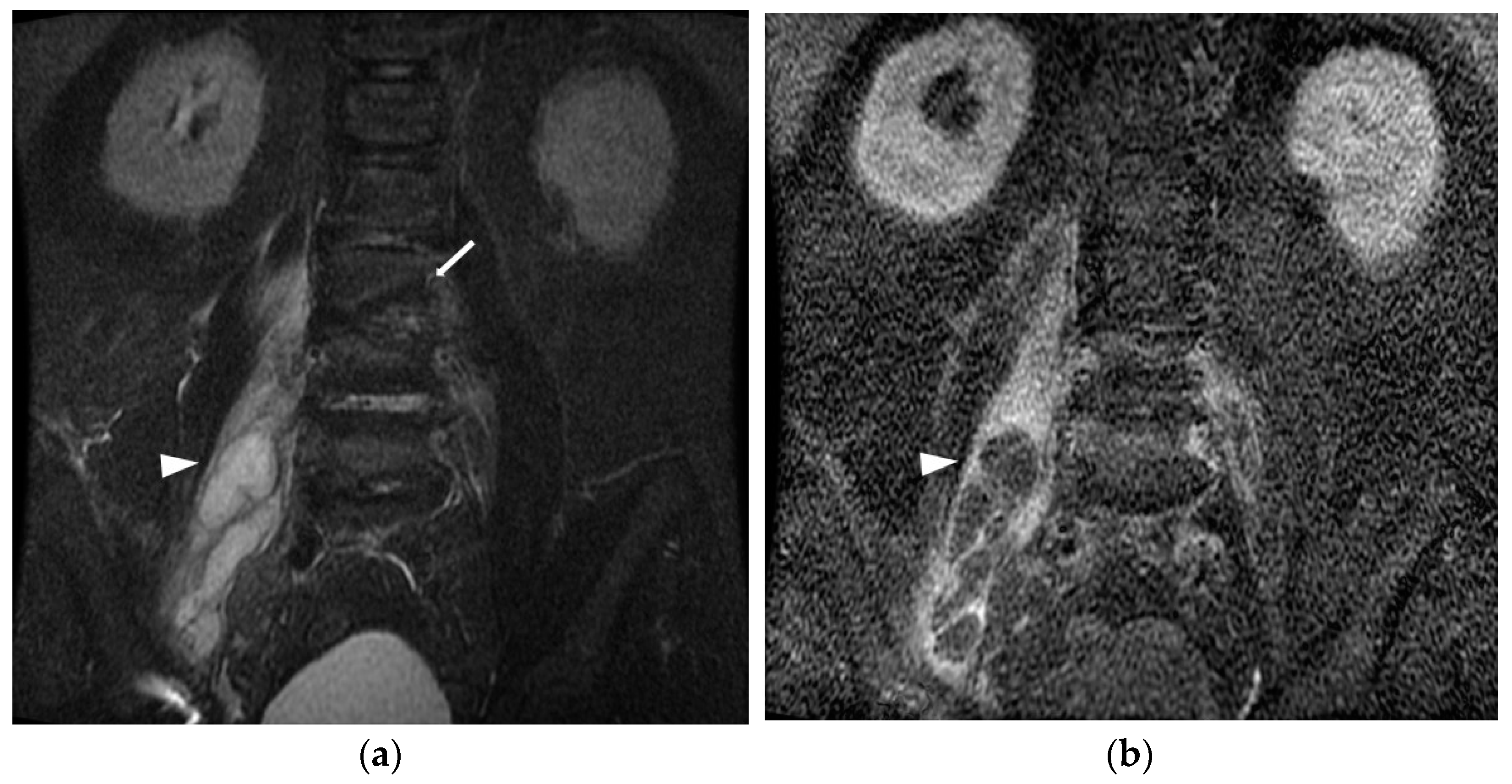
| Magnetic resonance imaging | 71 (40.3) | 65 (39.9) | 6 (46.2) | 0.657 |
| Blood test | ||||
| White blood count (103/μL) n = 17 | 16.6 ± 9.6 | 16.9 ± 9.8 | 13.1 ± 5.9 | 0.178 |
| Hemoglobin (g/dL) n = 175 | 11.3 ± 5.6 | 11.4 ± 5.7 | 10.8 ± 3.4 | 0.552 |
| Platelet (103/μL) n = 46 | 264.8 ± 144.0 | 273.1 ± 142.1 | 162.5 ± 133.0 | 0.007 * |
| INR n = 18 | 1.2 ± 0.4 | 1.2 ± 0.4 | 1.3 ± 0.3 | 0.354 |
| Creatinine (mg/dL) n = 176 | 2.1 ± 5.3 | 2.1 ± 5.5 | 2.7 ± 2.2 | 0.730 |
| C-reactive protein (mg/L) n = 41 | 187.8 ± 121.9 | 189.4 ± 120.0 | 166.6 ± 151.9 | 0.534 |
| Positive culture n = 176 | 93 (52.8) | 85 (52.1) | 8 (61.5) | 0.514 |
| Treatment | ||||
| Antibiotics alone | 56 (31.8) | 50 (30.7) | 6 (46.2) | 0.352 |
| Percutaneous drainage | 88 (50.0) | 83 (50.9) | 5 (38.5) | 0.387 |
| Surgery | 32 (18.2) | 30 (18.4) | 2 (15.4) | 1.000 |
| Variable | Total (n = 176) | Survivor (n = 163) | Non-Survivor (n = 13) | p Value |
|---|---|---|---|---|
| Primary IPA | 50 (28.4) | 45 (27.6) | 5 (38.5) | 0.523 |
| Secondary IPA | ||||
| Skeletal origin | 92 (52.3) | 88 (54.0) | 4 (30.8) | 0.107 |
| Spondylitis | 79 (44.9) | 75 (46.0) | 4 (30.8) | |
| Septic arthritis | 14 (8.0) | 14 (8.6) | 0 (0) | |
| Intra-abdominal origin | 12 (6.8) | 11 (6.7) | 1 (7.7) | 1.000 |
| Intestinal perforation | 4 (2.3) | 3 (1.8) | 1 (7.7) | |
| Intestinal ischemia | 1 (0.6) | 1 (0.6) | 0 (0) | |
| Enteric fistula | 2 (1.1) | 2 (1.2) | 0 (0) | |
| Diverticulitis | 1 (0.6) | 1 (0.6) | 0 (0) | |
| Appendicitis | 4 (2.3) | 4 (2.5) | 0 (0) | |
| Colon cancer | 1 (0.6) | 1 (0.6) | 0 (0) | |
| Endometrial cancer | 1 (0.6) | 1 (0.6) | 0 (0) | |
| Urinary tract origin | 9 (5.1) | 7 (4.3) | 2 (15.4) | 0.135 |
| Pyelonephritis | 5 (2.8) | 3 (1.9) | 2 (15.4) | |
| Renal abscess | 4 (2.3) | 4 (2.5) | 0 (0) | |
| Soft tissue origin | 6 (3.4) | 5 (3.1) | 1 (7.7) | 0.373 |
| Necrotizing fasciitis | 2 (1.1) | 2 (1.2) | 0 (0) | |
| Wound infection | 1 (0.6) | 1 (0.6) | 0 (0) | |
| Pressure sore | 3 (1.7) | 2 (1.2) | 1 (7.7) | |
| Cardiovascular origin | 7 (4.0) | 7 (4.3) | 0 (0) | 1.000 |
| Abdominal aortic aneurysm post stent insertion | 1 (0.6) | 1 (0.6) | 0 (0) | |
| Infected aortic aneurysm | 3 (1.7) | 3 (1.8) | 0 (0) | |
| Infective endocarditis | 3 (1.7) | 3 (1.8) | 0 (0) |
| Total | Primary | Secondary | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Skeletal | GI | GU | Soft Tissue | CV | ||||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | |
| Blood culture | 93 | 25 | 56 | 1 | 4 | 4 | 3 | |||||||
| Gram-positive | ||||||||||||||
| MSSA | 41 | (44.1) | 13 | (52.0) | 26 | (46.4) | 1 | (25.0) | 1 | (33.3) | ||||
| MRSA | 15 | (16.1) | 3 | (12.0) | 9 | (16.1) | 1 | (25.0) | 1 | (25.0) | 1 | (33.3) | ||
| CoNS | 6 | (6.5) | 1 | (4.0) | 2 | (3.6) | 1 | (25.0) | 2 | (50.0) | ||||
| GBS | 3 | (3.2) | 1 | (4.0) | 2 | (3.6) | ||||||||
| Streptococcus intermedius | 2 | (2.2) | 2 | (3.6) | ||||||||||
| Group D Streptococcus | 1 | (1.1) | 1 | (4.0) | ||||||||||
| Streptococcus gordonii | 1 | (1.1) | 1 | (1.8) | ||||||||||
| Streptococcus mitis | 1 | (1.1) | 1 | (4.0) | ||||||||||
| Anaerococcus sp. | 1 | (1.1) | 1 | (1.8) | ||||||||||
| Peptostreptococcus sp. | 1 | (1.1) | 1 | (4.0) | ||||||||||
| Gram-negative | ||||||||||||||
| Klebsiella pneumoniae | 6 | (6.5) | 2 | (8.0) | 4 | (7.1) | ||||||||
| Escherichia coli | 6 | (6.5) | 5 | (8.9) | 1 | (25.0) | ||||||||
| Salmonella enterica serogroup B | 2 | (2.2) | 1 | (1.8) | 1 | (33.3) | ||||||||
| Salmonella enterica serogroup D | 1 | (1.1) | 1 | (100.0) | ||||||||||
| Serratia marcescens | 1 | (1.1) | 1 | (25.0) | ||||||||||
| Actinobacillus actinomycetemcomitans | 1 | (1.1) | 1 | (4.0) | ||||||||||
| Aeromonas spp. | 1 | (1.1) | 1 | (1.8) | ||||||||||
| Burkholderia pseudomallei | 1 | (1.1) | 1 | (1.8) | ||||||||||
| Fungus | ||||||||||||||
| Candida albicans | 1 | (1.1) | 1 | (4.0) | ||||||||||
| Polymicrobial | 1 | (1.1) | 1 | (1.8) | ||||||||||
| Tissue culture | 94 | 25 | 50 | 7 | 6 | 4 | 2 | |||||||
| Gram-positive | ||||||||||||||
| MSSA | 26 | (27.7) | 7 | (28.0) | 19 | (38.0) | ||||||||
| MRSA | 14 | (14.9) | 6 | (24.0) | 7 | (14.0) | 1 | (16.7) | ||||||
| CoNS | 3 | (3.2) | 3 | (6.0) | ||||||||||
| GBS | 2 | (2.1) | 1 | (4.0) | 1 | (2.0) | ||||||||
| Enterococcus faecalis | 1 | (1.1) | 1 | (2.0) | ||||||||||
| Streptococcus intermedius | 1 | (1.1) | 1 | (2.0) | ||||||||||
| Viridans streptococcus | 1 | (1.1) | 1 | (4.0) | ||||||||||
| Gram-negative | ||||||||||||||
| Escherichia coli | 10 | (10.6) | 5 | (10.0) | 2 | (28.6) | 2 | (33.3) | 1 | (25.0) | ||||
| Klebsiella pneumoniae | 7 | (7.4) | 4 | (16.0) | 3 | (6.0) | ||||||||
| Salmonella enterica serogroup B | 2 | (2.1) | 2 | (4.0) | ||||||||||
| Salmonella enterica serogroup D | 1 | (1.1) | 1 | (2.0) | ||||||||||
| Bacteroides fragilis | 1 | (1.1) | 1 | (2.0) | ||||||||||
| Pseudomonas aeruginosa CR strain | 1 | (1.1) | 1 | (2.0) | ||||||||||
| Serratia marcescens | 1 | (1.1) | 1 | (2.0) | ||||||||||
| Polymicrobial | 22 | (23.4) | 6 | (24.0) | 3 | (6.0) | 5 | (71.4) | 3 | (50.0) | 3 | (75.0) | 2 | (100.0) |
| Tuberculosis | 1 | (1.1) | 1 | (2.0) | ||||||||||
| No. | Age | Sex | Underlying Diseases | Clinical Presentation | Blood Culture | Pus Culture | Location | Percutaneous Drainage | Surgical Debridement | Antibiotics Treatment |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 78 | M | DM, HTN, ESRD, gout, HIVD | abdominal pain | N/A | Mycobacterium tuberculosis complex | L | Y | Y | Teicoplanin + Ceftriaxone (10), Piperacillin/Tazobactam + Daptomycin (8), Teicoplanin + Piperacillin/Tazobactam (7), Rifinah + Pyrazinamide (26), Teicoplanin + Cefepime (5) |
| 2 | 50 | F | cirrhosis | fever, abdominal pain, seizure | N/A | N/A | R | N | N | Piperacillin/Tazobactam (5) |
| 3 | 87 | F | HTN, asthma | flank/back pain, limp, cold sweating, chillness, SOB, conscious unclear, urine/stool retention | MSSA | N/A | B | N | N | Teicoplanin + Cefoperazone/Sulbactam + Clindamycin (2), Cefepime + Vancomycin + Metronidazole (3) |
| 4 | 81 | F | dementia, bedridden, s/p pacemaker | fever, malaise | MSSA | MSSA | L | Y | N | Piperacillin/Tazobactam (1), Cefazolin + Ciprofloxacin (6), Vancomycin + Piperacillin/Tazobactam (4), Oxacillin (9) |
| 5 | 87 | F | CHF, CKD | fever, conscious drowsy | N/A | N/A | R | Y | N | Piperacillin/Tazobactam (21), Levofloxacin (3), Cefepime (7), Tigecycline |
| 6 | 74 | M | DM | fever, abdominal pain, malaise, anorexia, body weight loss, disoriented | N/A | Klebsiella pneumoniae | L | N | N | Ceftriaxone + Metronidazole (6), Teicoplanin + Imipenem/Cilastatin (1) |
| 7 | 82 | M | HTN, CVA, bedridden, CO intoxication-related HIE, SDH/SAH/EDH Hx | malaise, limbs edema | MSSA | MSSA, Proteus mirabilis, Escherichia coli | B | N | N | Piperacillin/Tazobactam (6), Teicoplanin (3) |
| 8 | 66 | M | DM, HTN, hyperparathyroidism | flank/back pain, conscious disturbance, SOB | Escherichia coli | N/A | R | N | N | Piperacillin/Tazobactam + Vancomycin(1), Ertapenem (1), Doripenem + Doxycycline (9) |
| 9 | 83 | F | CHF, DM, ESRD, breast cancer, Af | abdominal pain, left calf erythema, conscious drowsy | MSSA | MSSA | L | Y | N | Imipenem/Cilastatin + Vancomycin (5), Oxacillin (8), Ceftriaxone(5), Ertapenem (2) |
| 10 | 83 | M | CHF, HTN, CKD, gout | flank/back pain, limp | MRSA | N/A | B | N | N | Ertapenem(2), Daptomycin(2), Teicoplanin + Cefepime(10), Teicoplanin (4), Teicoplanin + Cefepime (3), Teicoplanin + Levofloxacin (8), Vancomycin (23), Vancomycin + Meropenem (3), Ertapenem (5), Daptomycin + Meropenem (15), Levofloxacin + Micafungin + Daptomycin (8), Piperacillin/Tazobactam+ Amikacin + Amphotericin B (4) |
| 11 | 89 | F | CHF, VHD, Af | flank/back pain, limp | N/A | Escherichia coli, Bacteroides fragilis, Streptococcus anginosus, Bacteroides thetaiotaomicron, Yeast-like | R | Y | Y | Piperacillin/Tazobactam (11), Ampicillin + Sulbactam (10), Piperacillin/Tazobactam (3) |
| 12 | 49 | M | oropharyngeal cancer | flank/back pain, limp, malaise | MSSA | Escherichia coli, Enterococcus faecium, Bacteroides fragilis, Bacteroides thetaiotaomicron | B | Y | Y | Cefoperazone/Sulbactam + Vancomycin (2), Meropenem + Teicoplanin (2), Doxycycline + Ceftriaxone + Vancomycin (3), Oxacillin (12), Flomoxef (3), Ceftriaxone (6), Ertapenem (11), Ciprofloxacin (6), Teicoplanin (4), Ceftazidime (5), Teicoplanin + Ampicillin + Sulbactam + Doripenem (4) Oxacillin + Doripenem (5), Oxacillin + Metronidazole (10), Oxacillin + Piperacillin/Tazobactam (14) |
| 13 | 81 | M | asthma | abdominal pain | Peptostreptococcus sp | Bacteroides sp, Pseudomonas aeruginosa | R | Y | N | Ceftriaxone, Metronidazole (1) |
| Univariate | Multivariate (Model A) | Multivariate (Model B) | ||||
|---|---|---|---|---|---|---|
| HR (95%CI) | p Value | HR (95%CI) | p Value | HR (95%CI) | p Value | |
| Age > 65 (year) | 6.68 (1.48, 30.16) | 0.013 | 5.12 (1.03,25.53) | 0.046 * | 6.06 (1.22,30.23) | 0.028 * |
| Male | 0.62 (0.21, 1.84) | 0.389 | ||||
| BT > 38 or <36 °C | 0.48 (0.11, 2.18) | 0.343 | ||||
| Heart rate > 100 (beats/min) | 1.08 (0.36, 3.22) | 0.887 | ||||
| SBP < 100 (mmHg) | 1.18 (0.26, 5.29) | 0.836 | ||||
| RR > 22 (breaths/min) | 4.98 (1.63, 15.23) | 0.005 | 1.41 (0.34, 5.95) | 0.637 | ||
| Septic shock | 71.49 (9.28, 550.63) | <0.001 | 61.90 (7.37, 519.46) | <0.001 * | ||
| Renal replacement therapy | 6.87 (2.31, 20.44) | 0.001 | 3.81 (0.94, 15.49) | 0.062 | 1.21 (0.39, 3.73) | 0.745 |
| Bedridden status | 4.42 (1.22, 16.07) | 0.024 | 2.37 (0.56, 10.08) | 0.243 | 1.37 (0.33, 5.70) | 0.669 |
| Gas-forming abscess | 2.44 (0.80, 7.44) | 0.119 | ||||
| Hypertension | 0.69 (0.23, 2.11) | 0.517 | ||||
| Diabetes mellitus | 0.73 (0.23, 2.38) | 0.604 | ||||
| Congestive heart failure | 9.20 (2.82, 29.97) | <0.001 | 5.13 (1.29, 20.45) | 0.021 * | 2.04 (0.51, 8.10) | 0.313 |
| Coronary artery disease | 0.87 (0.11, 6.70) | 0.895 | ||||
| Chronic kidney disease | 1.99 (0.61, 6.46) | 0.253 | ||||
| HIV | 0.31 (0.04, 2.24) | 0.244 | ||||
| WBC > 11 (103/μL) | 0.52 (0.17, 1.54) | 0.234 | ||||
| Hb < 8 (g/dL) | 2.33 (0.64, 8.48) | 0.198 | ||||
| Plt < 150 (103/μL) | 4.94 (1.66, 14.71) | 0.004 | 9.26 (2.59, 33.09) | 0.001 * | ||
| IPA origin | ||||||
| Primary origin | Reference | |||||
| Skeletal origin | 0.42 (0.11, 1.55) | 0.190 | ||||
| Intra-abdominal origin | 0.81 (0.09, 6.92) | 0.846 | ||||
| Urinary tract origin | 2.42 (0.47, 12.46) | 0.292 | ||||
| Soft tissue origin | 1.76 (0.21, 15.05) | 0.607 | ||||
| Cardiovascular origin | 0.55 (0.03, 11.04) | 0.985 | ||||
| Treatment | ||||||
| Antibiotics alone | Reference | |||||
| Percutaneous drainage | 0.55 (0.11, 2.74) | 0.467 | ||||
| Surgery | 0.51 (0.16, 1.67) | 0.266 | ||||
| Univariate | Multivariate | |||
|---|---|---|---|---|
| OR (95%CI) | p Value | OR (95%CI) | p Value | |
| Age > 65 (year) | 1.63 (0.89, 2.96) | 0.112 | ||
| Male | 1.06 (0.57, 1.96) | 0.866 | ||
| BT > 38 or <36 °C | 0.99 (0.51, 1.93) | 0.975 | ||
| Heart rate > 100 (beats/min) | 1.21 (0.67, 2.20) | 0.521 | ||
| SBP < 100 (mmHg) | 0.82 (0.34, 1.95) | 0.645 | ||
| RR > 22 (breaths/min) | 2.86 (1.10, 7.40) | 0.031 | 3.33 (1.09, 10.20) | 0.035 * |
| Renal replacement therapy | 2.08 (0.82, 5.30) | 0.125 | ||
| Bedridden status | 0.83 (0.25, 2.71) | 0.754 | ||
| Gas-forming abscess | 2.45 (1.32, 4.54) | 0.004 | 2.15 (1.03, 4.46) | 0.041 * |
| Hypertension | 0.90 (0.49, 1.62) | 0.716 | ||
| Diabetes mellitus | 1.42 (0.77, 2.63) | 0.258 | ||
| Congestive heart failure | 1.50 (0.39, 5.77) | 0.558 | ||
| Coronary artery disease | 1.85 (0.63, 5.45) | 0.262 | ||
| Chronic kidney disease | 3.79 (1.64, 8.77) | 0.002 | 5.23 (1.91, 14.31) | 0.001 * |
| HIV | 1.18 (0.16, 8.55) | 0.872 | ||
| WBC > 11 (103/μL) | 1.50 (0.78, 2.85) | 0.222 | ||
| Hb < 8 (g/dL) | 1.34 (0.54, 3.33) | 0.534 | ||
| Plt < 150 (103/μL) | 1.87 (0.89, 3.92) | 0.099 | ||
| IPA origin | ||||
| Primary origin | Reference | Reference | ||
| Skeletal origin | 3.82 (1.82, 8.05) | <0.001 | 4.92 (1.98, 12.22) | 0.001 * |
| Intra-abdominal origin | 0.23 (0.03, 1.98) | 0.183 | 0.24 (0.03, 2.18) | 0.202 |
| Urinary tract origin | 2.06 (0.48, 8.79) | 0.330 | 2.05 (0.38, 11.01) | 0.402 |
| Soft tissue origin | 1.29 (0.21, 7.83) | 0.785 | 2.52 (0.37, 17.08) | 0.343 |
| Cardiovascular origin | 6.43 (1.12, 37.07) | 0.037 | 7.18 (0.90, 57.51) | 0.063 |
| Treatment | ||||
| Antibiotics alone | Reference | Reference | ||
| Percutaneous drainage | 2.95 (1.20, 7.26) | 0.019 | 2.95 (1.01, 8.62) | 0.048 * |
| Surgery | 2.51 (1.24, 5.09) | 0.011 | 3.77 (1.58, 8.99) | 0.003 * |
| Univariate | ||
|---|---|---|
| HR (95%CI) | p Value | |
| Age > 65 (year) | 1.68 (0.34, 1.37) | 0.279 |
| Male | 0.89 (0.44, 1.79) | 0.733 |
| BT > 38 or <36 °C | 0.56 (0.23, 1.36) | 0.200 |
| Heart rate > 100 (beats/min) | 1.07 (0.55, 2.11) | 0.840 |
| SBP < 100 (mmHg) | 1.48 (0.61, 3.58) | 0.384 |
| RR > 22 (breaths/min) | 1.07 (0.38, 3.04) | 0.903 |
| Renal replacement therapy | 1.03 (0.36, 2.92) | 0.958 |
| Bedridden status | 2.40 (0.73, 7.88) | 0.148 |
| Gas-forming abscess | 1.15 (0.58, 2.26) | 0.690 |
| Hypertension | 1.10 (0.56, 2.15) | 0.786 |
| Diabetes mellitus | 1.14 (0.58, 2.25) | 0.698 |
| Congestive heart failure | 0.69 (0.09, 5.05) | 0.715 |
| Coronary artery disease | 2.14 (0.88, 5.16) | 0.092 |
| Chronic kidney disease | 0.56 (196, 1.58) | 0.271 |
| HIV | 4.69 (1.41, 15.57) | 0.012 * |
| WBC > 11 (103/μL) | 0.84 (0.41, 1.72) | 0.626 |
| Hb < 8 (g/dL) | 0.61 (0.15, 2.56) | 0.501 |
| Plt < 150 (103/μL) | 1.71 (0.80, 3.67) | 0.168 |
| IPA origin | ||
| Primary origin | Reference | |
| Skeletal origin | 0.73 (0.32, 1.70) | 0.466 |
| Intra-abdominal origin | 2.21 (0.72, 6.75) | 0.166 |
| Urinary tract origin | 1.12 (0.24, 5.31) | 0.884 |
| Soft tissue origin | 0.03 (0.002, 0.53) | 0.978 |
| Cardiovascular origin | 1.44 (0.30, 6.80) | 0.647 |
| Treatment | ||
| Antibiotics alone | Reference | |
| Percutaneous drainage | 0.66 (0.23, 1.94) | 0.454 |
| Surgery | 1.02 (0.48, 2.20) | 0.952 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.-C.; Li, J.-J.; Hsiao, C.-H.; Yen, C.-C. Clinical Characteristics and In-Hospital Outcomes in Patients with Iliopsoas Abscess: A Multicenter Study. J. Clin. Med. 2023, 12, 2760. https://doi.org/10.3390/jcm12082760
Lee Y-C, Li J-J, Hsiao C-H, Yen C-C. Clinical Characteristics and In-Hospital Outcomes in Patients with Iliopsoas Abscess: A Multicenter Study. Journal of Clinical Medicine. 2023; 12(8):2760. https://doi.org/10.3390/jcm12082760
Chicago/Turabian StyleLee, Yi-Chih, Jhih-Jin Li, Chien-Han Hsiao, and Chieh-Ching Yen. 2023. "Clinical Characteristics and In-Hospital Outcomes in Patients with Iliopsoas Abscess: A Multicenter Study" Journal of Clinical Medicine 12, no. 8: 2760. https://doi.org/10.3390/jcm12082760
APA StyleLee, Y.-C., Li, J.-J., Hsiao, C.-H., & Yen, C.-C. (2023). Clinical Characteristics and In-Hospital Outcomes in Patients with Iliopsoas Abscess: A Multicenter Study. Journal of Clinical Medicine, 12(8), 2760. https://doi.org/10.3390/jcm12082760






