Two-Stage Penile Reconstruction after Paraffin Injection: A Case Report and a Systematic Review of the Literature
Abstract
1. Introduction
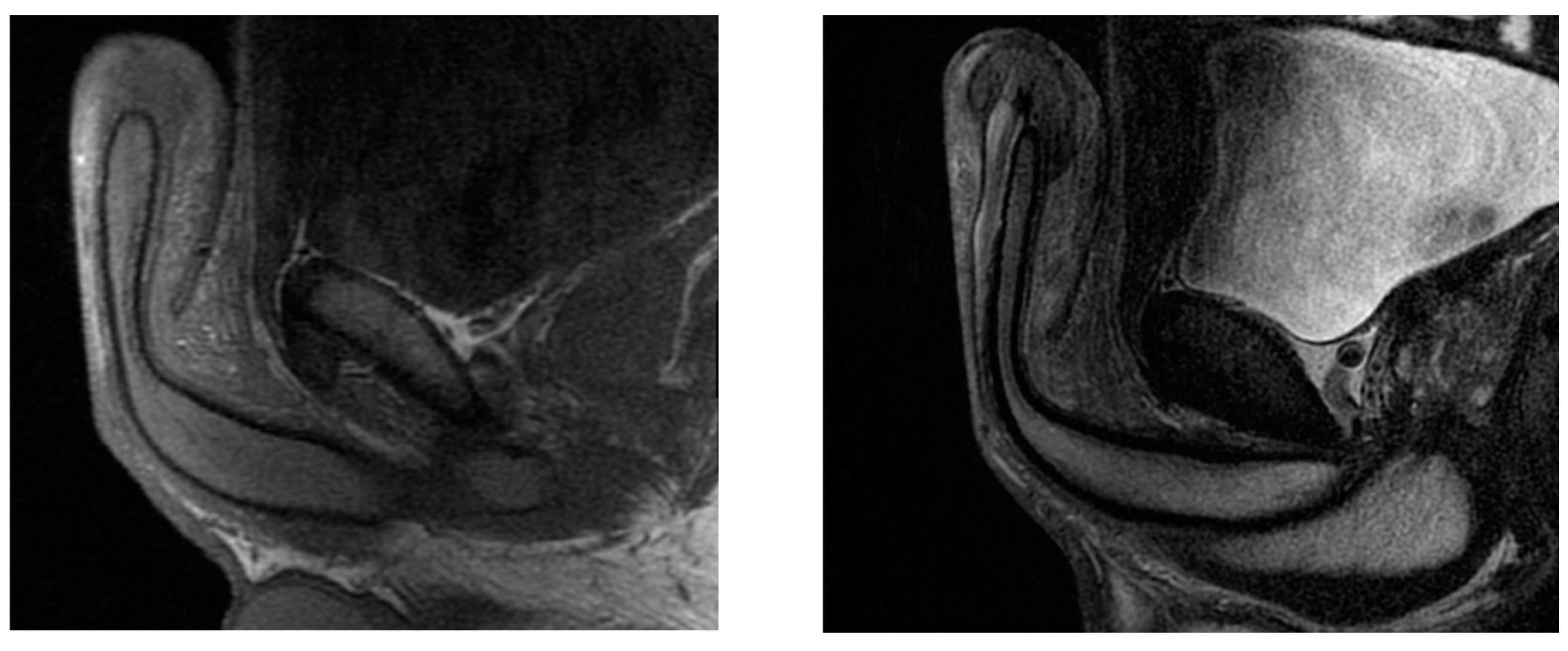
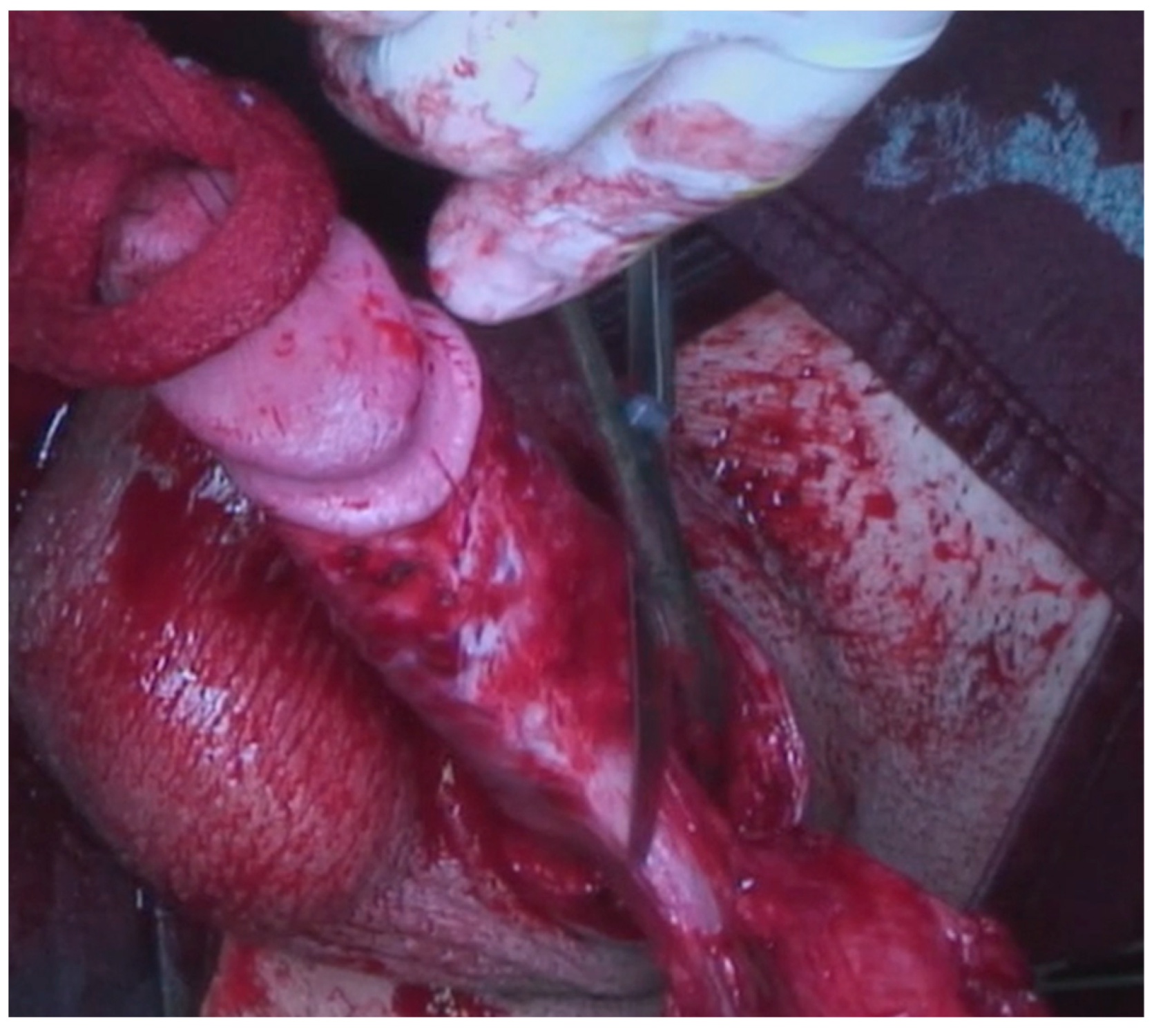
2. Case Report
3. Materials and Methods
4. Literature Search
5. Data Collection
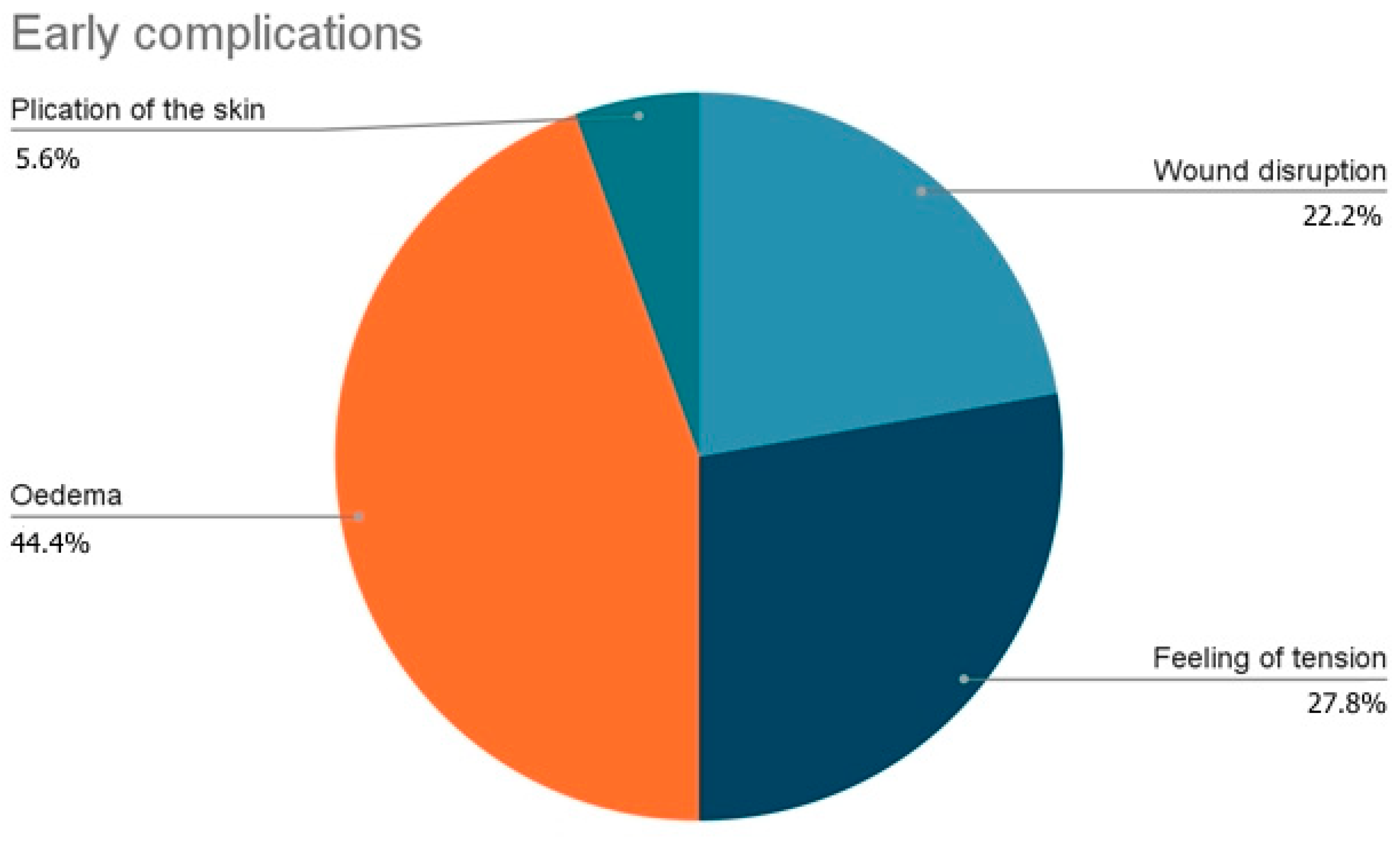
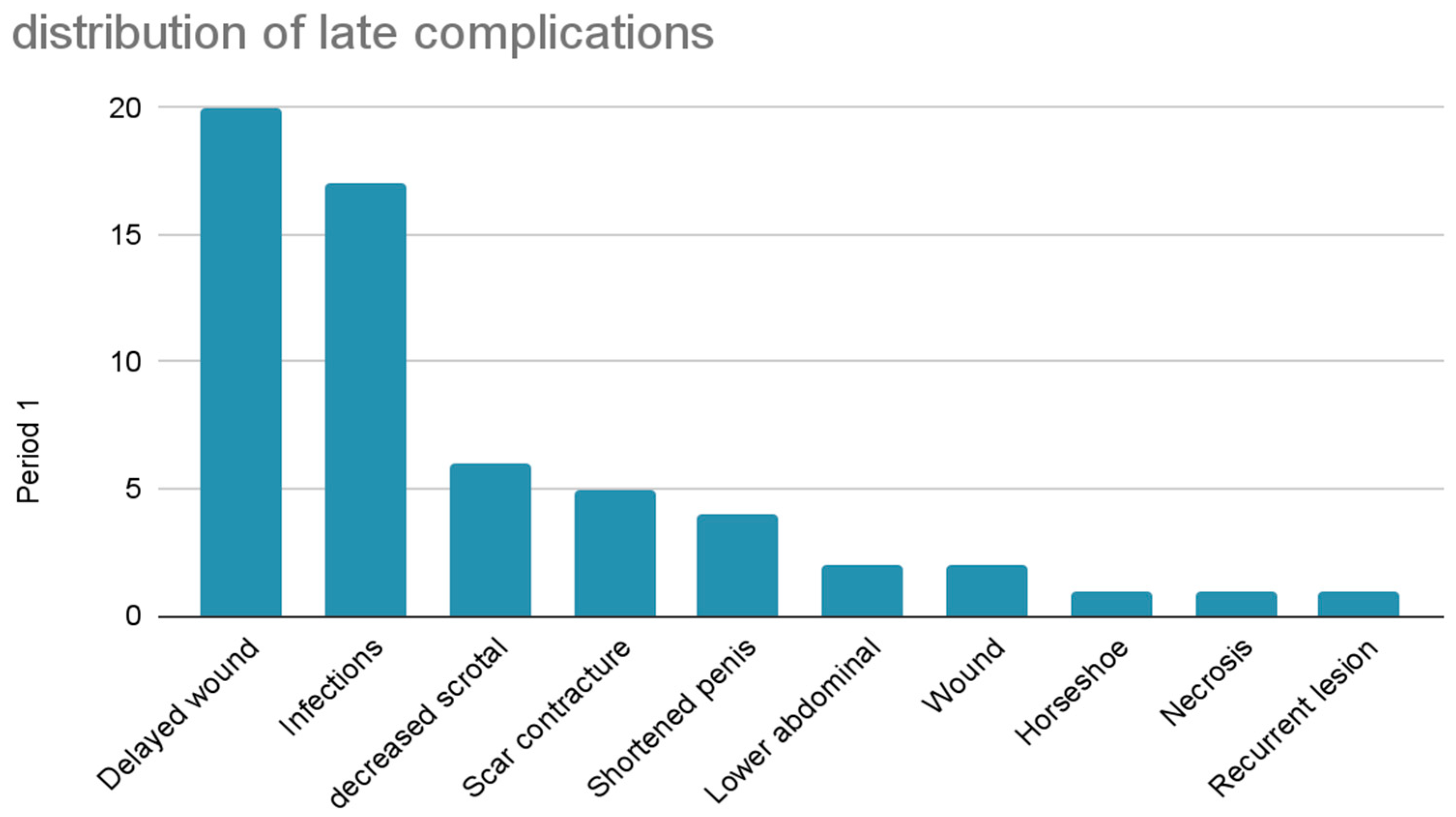
6. Results
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Downey, A.P.; Osman, N.I.; Mangera, A.; Inman, R.D.; Reid, S.V.; Chapple, C.R. Penile Paraffinoma. Eur. Urol. Focus. 2019, 5, 894–898. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.L.; Keoleian, C.M.; Krull, E.A. Penile paraffinoma: Self-injection with mineral oil. J. Am. Acad. Dermatol. 2001, 45, S222–S224. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.; Choi, H.R.; Lee, Y.T.; Lee, Y.H. Paraffinoma of the penis. Yonsei Med. J. 1994, 35, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.H.; Shin, H.J.; Woo, S.H.; Seul, J.H. A new repair technique for penile paraffinoma: Bilateral scrotal flaps. Ann. Plast. Surg. 1996, 37, 386–393. [Google Scholar] [CrossRef]
- Akkus, E.; Iscimen, A.; Tasli, L.; Hattat, H. Paraffinoma and Ulcer of the External Genitalia after Self-Injection of Vaseline. J. Sex. Med. 2006, 3, 170–172. [Google Scholar] [CrossRef]
- Carnicer-Lombarte, A.; Chen, S.-T.; Malliaras, G.G.; Barone, D.G. Foreign Body Reaction to Implanted Biomaterials and Its Impact in Nerve Neuroprosthetics. Front. Bioeng. Biotechnol. 2021, 9, 622524. [Google Scholar] [CrossRef]
- Chen, L.; Deng, H.; Cui, H.; Fang, J.; Zuo, Z.; Deng, J.; Li, Y.; Wang, X.; Zhao, L. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget 2017, 9, 7204–7218. [Google Scholar] [CrossRef]
- Sheikh, Z.; Brooks, P.J.; Barzilay, O.; Fine, N.; Glogauer, M. Macrophages, Foreign Body Giant Cells and Their Response to Implantable Biomaterials. Materials 2015, 8, 5671–5701. [Google Scholar] [CrossRef]
- Shi, C.; Pamer, E.G. Monocyte recruitment during infection and inflammation. Nat. Rev. Immunol. 2011, 11, 762–774. [Google Scholar] [CrossRef]
- Albendea, F.J.V.; Alcalde-Alonso, M.; Soto-Díaz, A.; Gómez-Avivar, P.; Torres-Gómez, F. Paraffinoma of the penis and scrotum (sclerosing granuloma of the male genitalia). Indian J. Dermatol. Venereol. Leprol. 2017, 83, 75–77. [Google Scholar] [CrossRef]
- Marín-Martínez, F.M.; Martínez-Valls, P.L.G.; Dekalo, S.; Weiss, J.; Haran, O. Aesthetic and Functional Results after Single- and Two-Stage Resection and Reconstruction of Penile Paraffinomas—Experience from Two Tertiary Centers and a Surgical Management Algorithm. Urology 2023, 171, 227–235. [Google Scholar] [CrossRef]
- Inn, F.X.; Imran, F.-H.; Ali, M.F.; Rizuana, I.H.; Zulkifli, Z. Penile augmentation with resultant foreign material granuloma and sequalae. Malays. J. Med. Sci. 2012, 19, 81–83. [Google Scholar] [PubMed]
- Soebhali, B.; Felicio, J.; Oliveira, P.; Martins, F.E. Sclerosing lipogranuloma of the penis: A narrative review of complications and treatment. Trans. Androl. Urol. 2021, 10, 2705. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021, 372, n71. [Google Scholar] [CrossRef]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inform. Decis. Mak. 2007, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Murad, M.H.; Sultan, S.; Haffar, S.; Bazerbachi, F. Methodological quality and synthesis of case series and case reports. BMJ Evid. Based Med. 2018, 23, 60–63. [Google Scholar] [CrossRef]
- Pehlivanov, G.; Kavaklieva, S.; Kazandjieva, J.; Kapnilov, D.; Tsankov, N. Foreign-body granuloma of the penis in sexually active individuals (penile paraffinoma). J. Eur. Acad. Dermatol. Venereol. 2008, 22, 845–851. [Google Scholar] [CrossRef]
- Pónyai, K.; Marschalkó, M.; Hársing, J.; Ostorházy, E.; Kelemen, Z.; Nyirády, P.; Várkonyi, V.; Kárpáti, S. Paraffinoma. JDDG J. Dtsch. Dermatol. Ges. 2010, 8, 686–688. [Google Scholar] [CrossRef]
- Picozzi, S.C.M.; Carmignani, L. Paraffinoma of the penis. Int. J. Emerg. Med. 2010, 3, 507–508. [Google Scholar] [CrossRef]
- Bayraktar, N.; Başar, I. Penile Paraffinoma. Case Rep. Urol. 2012, 2012, 202840. [Google Scholar] [CrossRef]
- Shin, Y.S.; Zhao, C.; Park, J.K. New Reconstructive Surgery for Penile Paraffinoma to Prevent Necrosis of Ventral Penile Skin. Urology 2013, 81, 437–441. [Google Scholar] [CrossRef] [PubMed]
- Cormio, L.; Di Fino, G.; Scavone, C.; Selvaggio, O.; Massenio, P.; Sanguedolce, F.; Macarini, L.; Carrieri, G. Magnetic resonance imaging of penile paraffinoma: Case report. BMC Med. Imaging 2014, 14, 39. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.W.; Yoon, B.I.; Ha, U.-S.; Kim, S.W.; Cho, Y.-H.; Sohn, D.W. Treatment of Paraffin-Induced Lipogranuloma of the Penis by Bipedicled Scrotal Flap With Y-V incision. Ann. Plast. Surg. 2014, 73, 692–695. [Google Scholar] [CrossRef] [PubMed]
- Manjit, S.; Vikramjit, S.; Clarence, L.C. Penile Paraffinoma. Med. J. Malays. 2015, 70, 361–362. [Google Scholar]
- Dellis, A.E.; Nastos, K.; Mastorakos, D.; Dellaportas, D.; Papatsoris, A.; Arkoumanis, P.T. Minimal surgical management of penile paraffinoma after subcutaneous penile paraffin injection. Arab. J. Urol. 2017, 15, 387–390. [Google Scholar] [CrossRef]
- Chon, W.; Koo, J.Y.; Park, M.J.; Choi, K.-U.; Park, H.J.; Park, N.C. Paraffin Granuloma Associated with Buried Glans Penis-Induced Sexual and Voiding Dysfunction. World J. Men’s Health 2017, 35, 129–132. [Google Scholar] [CrossRef]
- Salauddin, S.A.; Ghazali, H. Surgical Techniques for Correction of Penile Paraffinoma. Malays. J. Med. Sci. 2019, 26, 137–142. [Google Scholar] [CrossRef]
- Dunev, V.; Kolev, N.; Genov, P. Late results of bilateral scrotal flap. Urol. Case Rep. 2019, 27, 100920. [Google Scholar] [CrossRef]
- Kim, J.S.; Shin, Y.S.; Park, J.K. Penile skin preservation technique for reconstruction surgery of penile paraffinoma. Investig. Clin. Urol. 2019, 60, 133–137. [Google Scholar] [CrossRef]
- Danowski, K.M.; Jordan, L.; Ghaferi, J. Penile paraffinoma: Dramatic recurrence after surgical resection. Cutis 2020, 105, E17–E19. [Google Scholar]
- Vladislav, D.; Vladislav, M.; Pencho, G. Early result of meshed split-tickness skin graft in patient with paraffinoma of penis. Urol. Case Rep. 2020, 34, 101499. [Google Scholar] [CrossRef] [PubMed]
- Boucher, F.; Bayoux, R.; Allepot, K.; Braye, F.; Mojallal, A.; Morel-Journel, N.; Lari, A. The bilateral scrotal flap: Anatomical study and it’s use for the management of inflammatory granulomas following custom-made injections. Annales de Chirurgie Plastique Esthétique 2021, 66, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Ismy, J.; Amirsyah, M.; Palgunadi, I.N.; Firdaus, G.I.; Fakhrulrizal, F.; Khalilullah, S.A. One-stage Reconstruction of Penile Paraffinoma Using Spiral Stitches FTSG and Evaluation of Sexual Function. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4048. [Google Scholar] [CrossRef]
- De Siati, M.; Selvaggio, O.; Di Fino, G.; Liuzzi, G.; Massenio, P.; Sanguedolce, F.; Carrieri, G.; Cormio, L. An unusual delayed complication of paraffin self-injection for penile girth augmentation. BMC Urol. 2013, 13, 66. [Google Scholar] [CrossRef] [PubMed]
- Dellis, A.E.; Arkoumanis, T.; Kyprianou, C.; Papatsoris, A.G. Paraffinoma, siliconoma and Co: Disastrous consequences of failed penile augmentation—A single-centre successful surgical management of a challenging entity. Andrologia 2018, 50, e13109. [Google Scholar] [CrossRef]
- Takeshima, Y.; Suzuki, M.; Ikegaya, H.; Idota, N.; Kawai, T.; Sato, Y.; Kume, H. A cross-sectional cadaveric study of the correlation between genital organ measurements, serum testosterone, and serum prostate-specific antigen levels in Japanese male subjects. Int. J. Physiol. Pathophysiol. Pharmacol. 2021, 13, 36–42. [Google Scholar]
- Karakan, T.; Ersoy, E.; Hasçiçek, M.; Özgür, B.C.; Özcan, S.; Aydın, A. Injection of Vaseline under Penis Skin for the Purpose of Penis Augmentation. Case Rep. Urol. 2012, 2012, 510612. [Google Scholar] [CrossRef]
- Grassetti, L.; Torresetti, M.; Scalise, A.; Lazzeri, D.; Di Benedetto, G. Acellular Dermal Matrices and Paraffinoma: A Modern Tool for a Nearly Obsolete Disease. Arch. Plast. Surg. 2017, 44, 234–237. [Google Scholar] [CrossRef]
- Ahmed, U.; Freeman, A.; Kirkham, A.; Ralph, D.; Minhas, S.; Muneer, A. Self injection of foreign materials into the penis. Ind. Mark. Manag. 2017, 99, e78–e82. [Google Scholar] [CrossRef]
- Eandi, J.A.; Yao, A.P.; Javidan, J. Penile paraffinoma: The delayed presentation. Int. Urol. Nephrol. 2007, 39, 553–555. [Google Scholar] [CrossRef]
- Pang, K.H.; Randhawa, K.; Tang, S.; Fallara, G.; Katelaris, A.; Castiglione, F.; Ahmed, K.; Blecher, G.; Christopher, N.; Ralph, D.J.; et al. Complications and outcomes following injection of foreign material into the male external genitalia for augmentation: A single-centre experience and systematic review. Int. J. Impot. Res. 2023. [Google Scholar] [CrossRef] [PubMed]
- Naik, H.; Abuabara, K. Systematic reviews of case reports and case series: From anecdote to evidence. Br. J. Dermatol. 2018, 178, 317–318. [Google Scholar] [CrossRef] [PubMed]
- Creta, M.; Sica, A.; Napolitano, L.; Celentano, G.; La Rocca, R.; Capece, M.; Calogero, A.; Califano, G.; Vanni, L.; Mangiapia, F.; et al. Fournier’s Gangrene in Patients with Oncohematological Diseases: A Systematic Review of Published Cases. Healthcare 2021, 9, 1123. [Google Scholar] [CrossRef] [PubMed]
- Moon, D.G.; Yoo, J.W.; Bae, J.H.; Han, C.S.; Kim, Y.K.; Kim, J.J. Sexual function and psychological characteristics of penile paraffinoma. Asian J. Androl. 2003, 5, 191–194. [Google Scholar] [PubMed]
- Del Rosario, R.N.; Barr, R.J.; Graham, B.S.; Kaneshiro, S. Exogenous and endogenous cutaneous anomalies and curiosities. Am. J. Dermatopathol. 2005, 27, 259–267. [Google Scholar] [CrossRef]







| Domains | Selection | Ascertainment | Causality | Reporting | ||||
|---|---|---|---|---|---|---|---|---|
| Leading Explanatory Questions | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| Track Lee [3] | yes | no | no | no | no | no | no | yes |
| Jeong [4] | yes | yes | yes | yes | no | no | yes | yes |
| Pehlivanov [17] | yes | yes | no | yes | no | no | no | yes |
| Katinka [18] | no | yes | yes | yes | no | no | no | yes |
| Picozzi [19] | no | yes | no | no | no | no | no | no |
| Bayraktar [20] | no | no | yes | yes | no | no | yes | no |
| Xeng Inn [12] | no | yes | no | yes | no | no | no | no |
| Seob Shin [21] | no | yes | yes | yes | no | no | yes | yes |
| De Siati [22] | no | yes | yes | yes | no | no | yes | yes |
| Cormio [22] | no | yes | yes | yes | no | no | yes | yes |
| Sun wook kim [23] | no | yes | yes | yes | no | no | yes | yes |
| Manjit Sigh [24] | no | yes | yes | yes | no | no | no | yes |
| Dellis [25] | no | yes | yes | no | no | no | yes | yes |
| Chon [26] | no | yes | yes | yes | no | no | yes | yes |
| Salaudin [27] | yes | yes | yes | yes | no | no | no | yes |
| Dunev Vladislav [28] | no | yes | yes | yes | no | no | no | yes |
| Jong Sung Kim [29] | no | no | yes | yes | no | no | no | yes |
| K.M. Danowsky [30] | no | no | yes | yes | no | no | no | yes |
| Vladislav [31] | no | yes | yes | yes | no | no | yes | yes |
| Boucher [32] | no | yes | yes | yes | no | no | no | yes |
| Ismy [33] | no | yes | yes | yes | no | no | yes | yes |
| Title | Key Words | Abstract | Introduction | Patient Information | Clinical Findings | Timeline | Diagnostic Assessment | Therapautic Intervention | Follow-Up and Outcomes | Discussion | Patients Pepspective | Informed Conent | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3a | 3b | 3c | 3d | 4 | 5a | 5b | 5c | 5d | 6 | 7 | 8a | 8b | 8c | 8d | 9a | 9b | 9c | 10a | 10b | 10c | 10d | 11a | 11b | 11c | 11d | 12 | 13 | |
| Thack Lee [3] | - | - | - | - | - | X | X | X | X | X | - | X | - | X | - | X | - | X | - | - | X | X | - | - | X | - | - | - | - | - |
| Jae Jo Jeong [4] | - | - | X | - | - | - | - | X | - | - | X | - | - | - | - | - | - | X | - | X | X | - | X | X | - | - | - | - | - | |
| G Pehlivanov [17] | - | X | X | X | - | X | X | X | X | - | - | X | X | X | X | - | - | X | - | - | - | - | - | - | - | - | X | - | - | X |
| Katinka [18] | X | X | - | X | X | X | - | X | X | - | - | X | X | X | - | X | - | X | X | - | X | X | - | - | - | X | X | - | - | - |
| Picozzi [19] | - | - | - | - | - | - | - | X | X | X | - | X | - | X | - | X | - | X | - | - | - | - | - | - | - | - | - | X | - | - |
| Bayraktar [20] | - | - | X | - | - | - | X | X | X | - | - | X | - | X | - | X | - | X | - | - | X | X | - | - | X | X | - | X | - | - |
| Xeng Inn [12] | - | - | X | - | X | - | X | X | X | - | - | X | - | - | - | - | - | X | - | - | X | - | - | - | - | X | X | - | - | - |
| Seob Shin [21] | - | - | X | - | X | X | X | X | X | - | - | - | - | - | - | - | - | X | - | - | X | - | - | X | X | - | - | - | - | - |
| De Siati [34] | - | X | - | X | X | X | X | X | X | - | X | X | X | X | - | - | - | X | - | - | X | - | - | X | X | - | X | - | X | |
| Cormio [22] | - | X | - | X | X | - | - | X | X | - | - | X | X | X | - | X | - | X | - | - | X | X | - | - | - | X | X | - | - | - |
| Sun wook kim [23] | - | X | - | X | X | - | X | - | X | - | - | - | X | - | - | - | - | X | - | - | X | - | - | - | X | X | X | X | - | - |
| Manjit Sigh [24] | - | X | - | - | X | - | X | X | X | - | - | X | - | X | - | - | - | X | - | - | X | X | - | - | - | - | - | X | - | - |
| Dellis [25] | - | - | X | X | X | X | X | X | X | - | X | X | - | - | - | X | - | X | - | - | X | X | - | - | X | X | X | X | - | - |
| Chon [26] | - | X | X | - | - | - | X | X | X | - | - | X | X | X | - | - | - | X | - | - | X | - | - | - | - | X | X | - | - | - |
| Salaudin [27] | - | X | X | - | X | X | X | - | X | - | - | X | - | - | - | - | - | X | - | - | - | X | - | - | - | - | X | X | - | - |
| Dunev Vladislav [28] | - | X | X | - | X | X | X | X | X | - | - | X | X | - | - | - | - | X | - | - | X | - | - | - | X | - | - | X | - | - |
| Jong Sung Kim [29] | - | X | X | X | X | X | X | X | X | - | - | - | - | - | - | - | - | X | - | - | X | X | X | X | X | X | X | X | - | - |
| K.M. Danowsky [35] | - | - | - | - | - | - | - | X | X | X | - | X | - | X | - | X | - | X | - | - | - | - | - | - | X | X | X | - | - | - |
| Dunev Vladislav [31] | - | X | X | X | - | - | X | X | X | - | X | X | X | - | - | - | - | X | - | - | X | X | - | X | - | X | - | X | - | - |
| Boucher [32] | - | X | X | - | X | X | X | X | X | - | X | - | - | X | - | - | - | - | - | - | X | X | - | X | X | X | X | X | - | - |
| Ismy [33] | - | - | X | - | X | X | X | X | X | - | - | X | - | - | - | - | - | X | X | - | X | X | X | X | - | - | X | X | - | X |
| Grade | Type of Complication |
|---|---|
| I | Oedema, penile rugae, scar contracture, decreased scrotal size |
| II | Delayed wound healing, wound disruption, wound deiscence, infection |
| IIIa | Necrosis, shortnered penis |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Napolitano, L.; Marino, C.; Di Giovanni, A.; Zimarra, A.; Giordano, A.; D’Alterio, C.; Califano, G.; Creta, M.; Celentano, G.; La Rocca, R.; et al. Two-Stage Penile Reconstruction after Paraffin Injection: A Case Report and a Systematic Review of the Literature. J. Clin. Med. 2023, 12, 2604. https://doi.org/10.3390/jcm12072604
Napolitano L, Marino C, Di Giovanni A, Zimarra A, Giordano A, D’Alterio C, Califano G, Creta M, Celentano G, La Rocca R, et al. Two-Stage Penile Reconstruction after Paraffin Injection: A Case Report and a Systematic Review of the Literature. Journal of Clinical Medicine. 2023; 12(7):2604. https://doi.org/10.3390/jcm12072604
Chicago/Turabian StyleNapolitano, Luigi, Claudio Marino, Angelo Di Giovanni, Assunta Zimarra, Alessandro Giordano, Carlo D’Alterio, Gianluigi Califano, Massimiliano Creta, Giuseppe Celentano, Roberto La Rocca, and et al. 2023. "Two-Stage Penile Reconstruction after Paraffin Injection: A Case Report and a Systematic Review of the Literature" Journal of Clinical Medicine 12, no. 7: 2604. https://doi.org/10.3390/jcm12072604
APA StyleNapolitano, L., Marino, C., Di Giovanni, A., Zimarra, A., Giordano, A., D’Alterio, C., Califano, G., Creta, M., Celentano, G., La Rocca, R., Mirone, C., Spena, G., Palmieri, A., Longo, N., Imbimbo, C., & Capece, M. (2023). Two-Stage Penile Reconstruction after Paraffin Injection: A Case Report and a Systematic Review of the Literature. Journal of Clinical Medicine, 12(7), 2604. https://doi.org/10.3390/jcm12072604









