Outcomes of Acute Coronary Syndrome Patients Who Presented with Cardiogenic Shock versus Patients Who Developed Cardiogenic Shock during Hospitalization
Abstract
1. Introduction
2. Methods
2.1. Data Collection and Study Population
2.2. Outcomes
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Clinical Presentation and Management
3.3. Complications
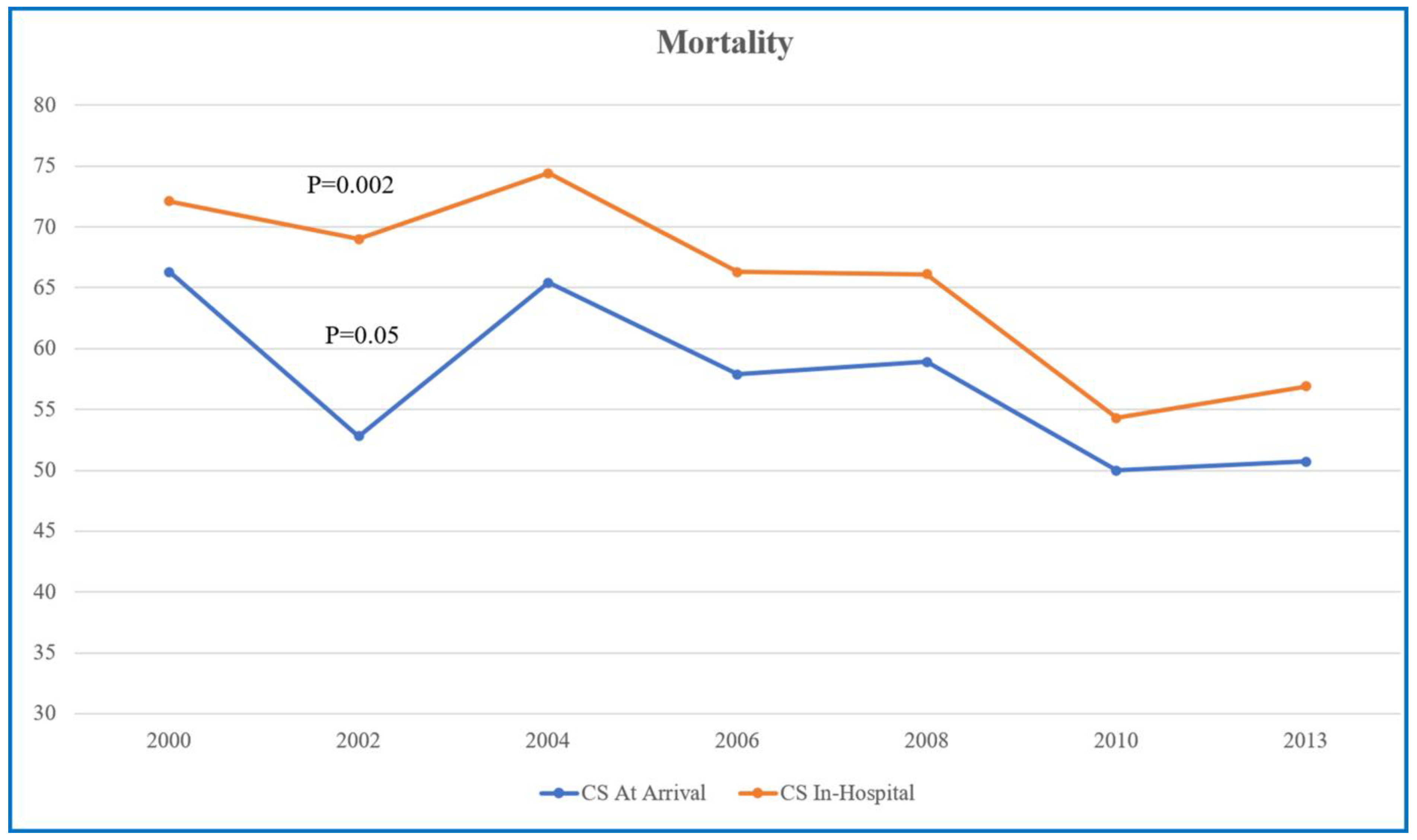
3.4. Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Noaman, S.; Vogrin, S.; Dinh, D.; Lefkovits, J.; Brennan, A.L.; Reid, C.M.; Walton, A.; Kaye, D.; Bloom, J.E.; Stub, D.; et al. Percutaneous Coronary Intervention Volume and Cardiac Surgery Availability Effect on Acute Coronary Syndrome-Related Cardiogenic Shock. JACC Cardiovasc. Interv. 2022, 15, 876–886. [Google Scholar] [CrossRef] [PubMed]
- Vahdatpour, C.; Collins, D.; Goldberg, S. Cardiogenic Shock. J. Am. Heart Assoc. 2019, 8, e011991. [Google Scholar] [CrossRef] [PubMed]
- Hochman, J.S.; Sleeper, L.A.; Webb, J.G.; Dzavik, V.; Buller, C.E.; Aylward, P.; Col, J.; White, H.D.; SHOCK Investigators. Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction. JAMA 2006, 295, 2511–2515. [Google Scholar] [CrossRef] [PubMed]
- Hochman, J.S.; Sleeper, L.A.; Webb, J.G.; Sanborn, T.A.; White, H.D.; Talley, J.D.; Buller, C.E.; Jacobs, A.K.; Slater, J.N.; Col, J.; et al. Early revascularization in acute myocardial infarction complicated by cardiogenic shock. N. Engl. J. Med. 1999, 341, 625–634. [Google Scholar] [CrossRef]
- Thiele, H.; Ohman, E.M.; Desch, S.; Eitel, I.; de Waha, S. Management of cardiogenic shock. Eur. Heart J. 2015, 36, 1223–1230. [Google Scholar] [CrossRef]
- Osman, M.; Syed, M.; Patibandla, S.; Sulaiman, S.; Kheiri, B.; Shah, M.K.; Bianco, C.; Balla, S.; Patel, B. Fifteen-Year Trends in Incidence of Cardiogenic Shock Hospitalization and In-Hospital Mortality in the United States. J. Am. Heart Assoc. 2021, 10, e021061. [Google Scholar] [CrossRef]
- Basir, M.B.; Kapur, N.K.; Patel, K.; Salam, M.A.; Schreiber, T.; Kaki, A.; Hanson, I.; Almany, S.; Timmis, S.; Dixon, S.; et al. Improved outcomes associated with the use of shock protocols: Updates from the national cardiogenic shock initiative. Catheter. Cardiovasc. Interv. 2019, 93, 1173–1183. [Google Scholar] [CrossRef]
- Garan, A.R.; Kanwar, M.; Thayer, K.L.; Whitehead, E.; Zweck, E.; Hernandez-Montfort, J.; Mahr, C.; Haywood, J.L.; Harwani, N.M.; Wencker, D.; et al. Complete hemodynamic profiling with pulmonary artery catheters in cardiogenic shock is associated with lower in-hospital mortality. JACC Heart Fail. 2020, 8, 903–913. [Google Scholar] [CrossRef]
- Tehrani, B.N.; Truesdell, A.G.; Sherwood, M.W.; Desai, S.; Tran, H.A.; Epps, K.C.; Singh, R.; Psotka, M.; Shah, P.; Cooper, L.B.; et al. Standardized team-based care for cardiogenic shock. J. Am. Coll. Cardiol. 2019, 73, 1659–1669. [Google Scholar] [CrossRef]
- Alkhouli, M.; Osman, M.; Elsisy, M.F.A.; Kawsara, A.; Berzingi, C.O. Mechanical circulatory support in patients with cardiogenic shock. Curr. Treat. Options Cardiovasc. Med. 2020, 22, 4. [Google Scholar] [CrossRef]
- Blatt, A.; Kalmanovich, E.; Karny-Rahkovich, O.; Brener, S.; Shlezinger, M.; Shlomo, N.; Vered, Z.; Hod, H.; Goldenberg, I.; Elbaz-Greener, G. Comparison of Noninvasively and Invasively Managed Patients, With or Without Revascularization in Non-ST Elevation Myocardial Infarction (from the Acute Coronary Syndrome Israeli Survey). Am. J. Cardiol. 2016, 118, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Lubovich, A.; Hamood, H.; Behar, S.; Rosenschein, U. Bypassing the emergency room to reduce door-to-balloon time and improve outcomes of patients with ST elevation myocardial infarction: The Acute Coronary Syndrome Israeli Survey experience. Isr. Med. Assoc. J. 2011, 13, 216–219. [Google Scholar] [PubMed]
- Ben-Dor, I.; Hasdai, D.; Behar, S.; Zahger, D.; Leor, J.; Hammerman, H.; Sandach, A.; Hod, H.; Gottlieb, S.; Working Group on Intensive Cardiac Care, Israel Heart Society. Prognostic implications of increased cardiac biomarkers and ST segment depression in non-ST elevation acute coronary syndromes: Lessons from the acute coronary syndrome Israeli survey (ACSIS) 2002. Heart 2006, 92, 547–548. [Google Scholar] [CrossRef] [PubMed]
- Killip, T., 3rd; Kimball, J.T. Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients. Am. J. Cardiol. 1967, 20, 457–464. [Google Scholar] [CrossRef]
- DeGeare, V.S.; Boura, J.A.; Grines, L.L.; O’Neill, W.W.; Grines, C.L. Predictive value of the Killip classification in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Am. J. Cardiol. 2001, 87, 1035–1038. [Google Scholar] [CrossRef] [PubMed]
- Damluji, A.A.; Forman, D.E.; van Diepen, S.; Alexander, K.P.; Page, R.L., 2nd; Hummel, S.L.; Menon, V.; Katz, J.N.; Albert, N.M.; Afilalo, J.; et al. Adults in the Cardiac Intensive Care Unit: Factoring Geriatric Syndromes in the Management, Prognosis, and Process of Care: A Scientific Statement From the American Heart Association. Circulation 2020, 141, e6–e32. [Google Scholar] [CrossRef]
- Damluji, A.A.; van Diepen, S.; Katz, J.N.; Menon, V.; Tamis-Holland, J.E.; Bakitas, M.; Cohen, M.G.; Balsam, L.B.; Chikwe, J.; American Heart Association Council on Clinical Cardiology; et al. Mechanical Complications of Acute Myocardial Infarction: A Scientific Statement From the American Heart Association. Circulation 2021, 144, e16–e35. [Google Scholar] [CrossRef]
- Schumann, J.; Henrich, E.C.; Strobl, H.; Prondzinsky, R.; Weiche, S.; Thiele, H.; Werdan, K.; Frantz, S.; Unverzagt, S. Inotropic agents and vasodilator strategies for the treatment of cardiogenic shock or low cardiac output syndrome. Cochrane Database Syst. Rev. 2018, 1, CD009669. [Google Scholar] [CrossRef]
- Samsky, M.D.; Morrow, D.A.; Proudfoot, A.G.; Hochman, J.S.; Thiele, H.; Rao, S.V. Cardiogenic shock after acute myocardial infarction: A review. JAMA 2021, 326, 1840–1850. [Google Scholar] [CrossRef]
- Ayman, A.-A.; Zaidan, M.; Abdalwahab, A.; Asswad, A.G.; Egred, M.; Zaman, A.; Alkhalil, M. Mechanical circulatory support in acute myocardial infarction complicated by cardiogenic shock. Rev. Cardiovasc. Med. 2022, 23, 71. [Google Scholar]
- Berg, D.D.; Bohula, E.A.; Morrow, D.A. Epidemiology and causes of cardiogenic shock. Curr. Opin. Crit. Care 2021, 27, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, F.; Rogers, J.G. Left ventricular assist device therapy in advanced heart failure: Patient selection and outcomes. Eur. J. Heart Fail. 2017, 19, 595–602. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Vallabhajosyula, S.; Ya’Qoub, L.; Kumar, V.; Verghese, D.; Subramaniam, A.V.; Patlolla, S.H.; Desai, V.K.; Sundaragiri, P.R.; Cheungpasitporn, W.; Deshmukh, A.J.; et al. Contemporary National Outcomes of Acute Myocardial Infarction-Cardiogenic Shock in Patients with Prior Chronic Kidney Disease and End-Stage Renal Disease. J. Clin. Med. 2020, 9, 3702. [Google Scholar] [CrossRef] [PubMed]
- Krisanapan, P.; Pattharanitima, P.; Thongprayoon, C.; Cheungpasitporn, W. Recent Advances in Understanding of Cardiovascular Diseases in Patients with Chronic Kidney Disease. J. Clin. Med. 2022, 11, 4653. [Google Scholar] [CrossRef]
- Han, J.H.; Chandra, A.; Mulgund, J.; Roe, M.T.; Peterson, E.D.; Szczech, L.A.; Patel, U.; Ohman, E.M.; Lindsell, C.J.; Gibler, W.B. Chronic kidney disease in patients with non-ST-segment elevation acute coronary syndromes. Am. J. Med. 2006, 119, 248–254. [Google Scholar] [CrossRef]

| Variable n, (%) | CS at Arrival (N = 224) | CS during Hospitalization (N = 341) | p-Value |
|---|---|---|---|
| Gender (female) | 67 (29.9) | 118 (34.6) | 0.24 |
| Mean age ± SD | 69.7 ± 13.10 | 71.67 ± 12.84 | 0.25 |
| Diabetes mellitus | 78 (35.1) | 142 (41.9) | 0.15 |
| Hypertension | 128 (57.9) | 339 (65.8) | 0.06 |
| Dyslipidemia | 104 (47.9) | 180 (53.7) | 0.18 |
| Mean body mass index (kg/m2) | 27.24 | 28.37 | 0.65 |
| Prior myocardial infarction | 70 (31.8) | 131 (38.8) | 0.1 |
| Prior percutaneous coronary intervention | 38 (17.3) | 66 (19.5) | 0.5 |
| Prior coronary artery bypass graft | 14 (6.3) | 31 (9.1) | 0.23 |
| Prior stroke/transient ischemic attack | 31 (14) | 38 (14.2) | 0.95 |
| Congestive heart failure | 40 (18.2) | 58 (17.2) | 0.76 |
| Chronic renal failure | 32 (14.4) | 74 (21.8) | 0.03 |
| Peripheral vascular disease | 26 (11.8) | 56 (16.5) | 0.13 |
| Chronic treatment | |||
| Aspirin | 80 (47.6) | 139 (49.8) | 0.65 |
| Clopidogrel | 7 (4.1) | 24 (8.6) | 0.06 |
| Anti-coagulation | 9 (5.3) | 14 (5) | 0.88 |
| Renin angiotensin system inhibitors | 61 (34.7) | 122 (43.4) | 0.06 |
| Beta blockers | 67 (39.2) | 100 (35.8) | 0.47 |
| Calcium channel blockers | 32 (19) | 50 (18.1) | 0.79 |
| Nitrates | 28 (16.6) | 53 (19.1) | 0.5 |
| Statins | 56 (33.3) | 117 (42.1) | 0.06 |
| Insulin | 7 (4) | 27 (9.7) | 0.03 |
| Variable | CS at Arrival (N = 224) | CS during Hospitalization (N = 341) | p-Value |
|---|---|---|---|
| Presentation at arrival n, (%) | |||
| Typical angina | 101 (45.1) | 220 (64.5) | 0.0001 |
| Angina > 24 h before admission | 54 (24.9) | 124 (36.7) | 0.003 |
| Atypical angina | 19 (10.1) | 48 (15.8) | 0.07 |
| Dyspnea | 82 (36.6) | 107 (31.4) | 0.12 |
| Sudden cardiac death | 52 (23.2) | 37 (10.9) | 0.0001 |
| Arrythmia | 33 (14.7) | 25 (7.3) | 0.004 |
| Non-ST-segment elevation MI | 52 (26.13) | 76 (23.82) | 0.6 |
| ST-segment elevation MI | 147 (73.87) | 243 (76.18) | 0.06 |
| Hospitalization units | 0.003 | ||
| Intensive cardiac units | 192 (85.7) | 269 (78.8) | |
| Internal medicine and other | 31 (13.8) | 70 (20.5) | |
| Blood lab tests at arrival | |||
| CK (IU/L) peak value | 2573 ± 3428 | 2374 ± 2559 | 0.27 |
| Troponin I (ng/mL) | 33.20 ± 61.17 | 41.76 ± 69.7 | 0.04 |
| Creatinine (mg/dL) | 1.76 ± 1.13 | 1.97 ± 1.39 | 0.20 |
| Glucose (mg/dL) | 246 ± 132.8 | 225.5 ± 130 | 0.07 |
| Hemoglobin (g/dL) | 12.6 ± 2.2 | 12.6 ± 2.28 | 0.83 |
| Total cholesterol (mg/dL) | 157 ± 50 | 172 ± 53.7 | 0.006 |
| Low-density lipoprotein (mg/dL) | 93.6 ± 40.2 | 100.3 ± 42.5 | 0.2 |
| Variable % | CS at Arrival (N = 224) | CS during Hospitalization (N = 341) | p-Value |
|---|---|---|---|
| Primary PCI | 68.7 | 67.9 | 0.88 |
| Total PCI | 87 | 74 | 0.007 |
| Thrombolysis | 10.4 | 23.2 | 0.005 |
| Coronary angiography | 90.1 | 92.1 | 0.06 |
| CABG | 5.8 | 4.1 | 0.35 |
| CPR | 40.7 | 47.4 | 0.12 |
| DC Shock | 23.1 | 28 | 0.19 |
| Mechanical ventilation | 66.5 | 66.5 | 0.99 |
| IABP | 35.7 | 49.1 | 0.001 |
| Medication at admission | |||
| Aspirin | 83.5 | 87.9 | 0.13 |
| Clopidogrel | 45 | 60.7 | 0.0002 |
| Heparin | 69.2 | 78.9 | 0.009 |
| Low-molecular-weight heparin | 30.8 | 34.3 | 0.39 |
| Beta blockers | 45.7 | 46.7 | 0.82 |
| Renin angiotensin system inhibitors | 45.3 | 49 | 0.39 |
| Nitrates | 25.3 | 39.1 | 0.001 |
| Statins | 45.2 | 50.4 | 0.22 |
| Diuretics | 56.8 | 68.5 | 0.004 |
| Digoxin | 9.5 | 11 | 0.56 |
| Glycoprotein IIb/IIIa inhibitors | 25.6 | 25.1 | 0.89 |
| Variable | CS at Arrival (N = 224) | CS during Hospitalization (N = 341) | p-Value |
|---|---|---|---|
| In-hospital mortality | 36.3 | 55.1 | <0.001 |
| 7-day mortality | 37.7 | 57.1 | 0.004 |
| 30-day mortality | 50.2 | 64.1 | 0.001 |
| 1-year mortality | 59.3 | 72.9 | 0.002 |
| MACEs | 51.3 | 73.0 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abu Ghosh, Z.; Amir, O.; Carasso, S.; Planer, D.; Alcalai, R.; Golomb, M.; Dagan, G.; Kalmanovich, E.; Blatt, A.; Elbaz-Greener, G. Outcomes of Acute Coronary Syndrome Patients Who Presented with Cardiogenic Shock versus Patients Who Developed Cardiogenic Shock during Hospitalization. J. Clin. Med. 2023, 12, 2603. https://doi.org/10.3390/jcm12072603
Abu Ghosh Z, Amir O, Carasso S, Planer D, Alcalai R, Golomb M, Dagan G, Kalmanovich E, Blatt A, Elbaz-Greener G. Outcomes of Acute Coronary Syndrome Patients Who Presented with Cardiogenic Shock versus Patients Who Developed Cardiogenic Shock during Hospitalization. Journal of Clinical Medicine. 2023; 12(7):2603. https://doi.org/10.3390/jcm12072603
Chicago/Turabian StyleAbu Ghosh, Zahi, Offer Amir, Shemy Carasso, David Planer, Ronny Alcalai, Mordechai Golomb, Gil Dagan, Eran Kalmanovich, Alex Blatt, and Gabby Elbaz-Greener. 2023. "Outcomes of Acute Coronary Syndrome Patients Who Presented with Cardiogenic Shock versus Patients Who Developed Cardiogenic Shock during Hospitalization" Journal of Clinical Medicine 12, no. 7: 2603. https://doi.org/10.3390/jcm12072603
APA StyleAbu Ghosh, Z., Amir, O., Carasso, S., Planer, D., Alcalai, R., Golomb, M., Dagan, G., Kalmanovich, E., Blatt, A., & Elbaz-Greener, G. (2023). Outcomes of Acute Coronary Syndrome Patients Who Presented with Cardiogenic Shock versus Patients Who Developed Cardiogenic Shock during Hospitalization. Journal of Clinical Medicine, 12(7), 2603. https://doi.org/10.3390/jcm12072603






