Abstract
Pulmonary vasodilators have improved pulmonary arterial hypertension (PAH) symptoms and prognosis; however, the drugs cause some side effects, including lower legs pain, which impair quality of life (QOL). The present study examined if compression stockings improved lower extremity symptoms and QOL caused by pulmonary vasodilators in PAH patients. We retrospectively enrolled consecutively ten patients with PAH treated by pulmonary vasodilators, who were regularly followed in Kurume University Hospital from January 2022 to June 2022. Oral questionnaire surveys, the Numeric Rating Scale for Pain (NRS) and the Pain Disability Assessment Scale (PDAS), were conducted regarding lower extremity symptoms before wearing elastic stockings and one month later, to evaluate how the lower extremity symptoms affected daily life. All ten patients were female, with a mean age of 50.2 ± 11.5 years, out of whom intravenous prostacyclin analogue (PGI2) was administered in five patients. In no intravenous PGI2 group, NRS score was significantly improved from 4.6 ± 2.3 to 2.8 ± 1.2 (p = 0.037), while from 9.4 ± 1.2 to 5.4 ± 1.6 (p = 0.002) in intravenous PGI2 group. PDAS score was also significantly improved [no intravenous PGI2 group; 18.0 (15.0–24.0) to 15.0 (10.0–19.0), intravenous PGI2 group; 25.0 (17.0–37.0) to 17.0 (5.0–27.0)]. Lower extremity symptoms in patients using pulmonary vasodilators were improved by wearing compression stockings.
1. Introduction
Pulmonary arterial hypertension (PAH) is a progressive disease caused by small pulmonary artery obstruction, in which increased pulmonary vascular resistance leads to progressive elevation of pulmonary artery pressure, and right heart failure to death [1]. Because there was no effective therapy in PAH until the mid 1990s, the prognosis was very poor with 1-, 2-, and 3-year survival rates of 77.4%, 51.6%, and 40.6%, respectively [1,2,3]. Since pulmonary vasodilators have been successively developed after mid-1990s, PAH symptoms, exercise tolerance, pulmonary hemodynamics, and prognosis have been significantly improved [1,3,4,5,6].
Pharmacotherapy for PAH has been developed acting on the prostacyclin-cAMP (cyclic adenosine monophosphate), nitric oxide (NO)-cGMP (cyclic guanosine monophosphate), and endothelin pathways. These pulmonary vasodilators are given by oral administration, inhalation, and continuous subcutaneous or intravenous infusion, and the doses are adjusted by escalation to determine the optimal dose for each patient, in consideration of health-related quality of life (QOL) [1]. In the follow-up assessments of PAH, patients are advised to self-monitor for adverse drug events (ADEs) [7]. It is important for patients to appropriately manage ADEs. For example, headache and pain in extremities are often observed in the treatment of PAH, [7] which affect QOL of patients. Especially, lower extremity symptoms seriously affect daily life such as work and housework. The precise mechanisms occurring in lower extremity symptoms are still unclear, and the care for these symptoms have not been developed. Lower extremity symptoms include various clinical features such as sole pain, swelling, dullness, and knee or heel pain. However, many patients have no choice but to endure their lower extremity symptoms.
In our hospital, we recommend the patients with lower extremity symptoms to wear elastic stockings, because a patient, who wore compression stockings, had better lower limbs symptoms. Compression stockings are usually used for patients with varicose veins and lymphedema, and are designed so that the compression pressure is the strongest at the ankle, decreasing toward the center. In compressed lower extremities, pressure improves venous return, heals ulcers, and alleviates symptoms. Therefore, the present study examined the hypothesis if compression stockings improve lower extremity symptoms and QOL caused by pulmonary vasodilators in PAH patients.
2. Materials and Methods
2.1. Study Design
This study was a single center, retrospective observational study to examine whether compression stockings were effective to reduce lower limbs’ symptoms caused by pulmonary vasodilators. The present study was approved by the institutional review board at Kurume University (21296) and conducted in accordance with the ethical principles of the Declaration of Helsinki. All patients provided written informed consent.
2.2. Study Population and Patient Selection
We enrolled consecutive patients aged 20 years or older, who meet the inclusion criteria. Inclusion criteria were as follows: (1) age of ≥20 years, (2) patients with PAH treated by pulmonary vasodilators, who were regularly followed in Cardiovascular Medicine, Kurume University Hospital from January 2022 to June 2022, and (3) those who provided written consent for study participation. Exclusion criteria were as follows: (1) patients with a history of arteriosclerosis obliterans, and (2) patients with varicose vein, lymphedema, and/or skin problems on the lower extremities.
2.3. Compression Stockings
For elastic stockings, we measured the lower limbs size of the subjects and selected below-the-knee stockings that fit the size from several companies. Compression pressure was set at 20–29 mmHg, which was commonly used. Before wearing the compression stockings, the lower limbs were observed to check for skin troubles, and the stockings were put on under the direction of the attending cardiologists.
2.4. Data Collection
We obtained demographic and clinical information from the electronic medical records of Kurume University Hospital. The patients’ background data including age, sex, height, body weight, Nice clinical classification of PAH, WHO functional classification, blood pressure (BP), and pulse rate, etiology of PAH, 6-min walk test, echocardiography, and right heart catheterization data were collected.
2.5. Lower Limbs Symptom Evaluation
Oral questionnaire surveys were conducted regarding lower extremity symptoms, in which NRS and PDAS were used before wearing elastic stockings and one month later, to evaluate how the lower extremity symptoms affected daily life.
2.5.1. Numeric Rating Scale for Pain (NRS)
The pain NRS is an 11-point scale from 0 to 10, which is a unidimensional measure of lower extremities pain intensity [8,9].
2.5.2. Pain Disability Assessment Scale (PDAS)
PDAS was used to assess pain-related disability, on a self-reporting scale from 0 to 3 (0: pain never interfered with these activities; 3: pain completely interfered with these activities), which consists of 20 items; (1) household chores such as vacuuming and gardening, (2) slow running, (3) bending down to pick up something on the floor, (4) going out for shopping, (5) going up and down stairs, (6) visiting friends, (7) taking a bus or train, (8) going out to a restaurant or cafe, (9) carrying heavy stuffs, (10) cooking, washing dishes, (11) bending and stretching waist, (12) reaching out and picking up a heavy object (e.g., sugar bag) from the shelf, (13) washing or wiping body, (14) sitting down and standing up in rest room, (15) getting into bed, getting out of bed, (16) opening and closing car doors, (17) standing still, (18) walking on level ground, (19) hobby activities, and (20) shampoo [10,11].
2.5.3. Specific Comments before and after Compression Stockings
We asked their specific feeling about lower extremity symptoms and location, situations and frequency of lower extremity symptoms, disturbance in life, and other changes before and after compression stockings.
2.6. Endpoints
The primary endpoint was the improvement of lower limbs symptoms. The secondary endpoints included specific changes in lower limbs symptoms.
2.7. Statistical Analysis
Continuous variables were presented as means ± standard deviation (SD) or median (IQR; interquartile range), as appropriate. They were compared by the Welch’s t-test. Categorical baseline variables were presented as numbers (percentage) and compared by the Fisher’s exact test. All p values < 0.05 were considered statistically significant. All analyses were performed with the SPSS system (SPSS Inc., Chicago, IL, USA).
3. Results
3.1. Patient Characteristics
Ten patients were enrolled in the present study. All 10 patients were female, with a mean age of 50.2 ± 11.5 years. There were 6 idiopathic, 2 hereditary PAH, and 2 PAH associated with connective tissue disease (no scleroderma), who were treated by endothelin receptor antagonist (ERA) in 9, phosphadiesterase-5 (PDE-5) inhibitor in 5, soluble guanylate cyclase (sGC) stimulator in 4, prostacyclin (IP) receptor agonist in 6, oral prostacyclin in 2, and intravenous prostacyclin analogue (PGI2) in 5 (Table 1).

Table 1.
Clinical characteristics.
3.2. Effects of Compression Stockings
We divided the patients into two groups; with and without intravenous PGI2 (n = 5 each). There were no significant differences other than age in comparing baseline patients’ characteristics, including echocardiography and right heart catheterization data, between with and without intravenous PGI2 groups before compression stockings started (Table 2).

Table 2.
Comparison between with and without intravenous prostacyclin.
In no intravenous PGI2 group, all five patients noted fatigue in the lower legs. Three cases occurred while standing and two while walking. Three cases had symptoms every day and two had occasionally (Table 3). In intravenous PGI2 group, four patients had pain in the lower extremities, and one had fatigue. The lower extremity symptoms occurred on the femoral, lower leg, and foot. Lower extremity symptoms appeared in four cases when standing. All patients had symptoms every day (Table 3).

Table 3.
Patients’ clinical characteristics and symptoms.
Before compression stockings, the NRS score showed 10 (worst score) in four patients in intravenous PGI2 group. Compression stockings significantly improved NRS score in both groups, where NRS score was significantly improved from 4.6 ± 2.3 to 2.8 ± 1.2 (p = 0.037) in no intravenous PGI2 group and from 9.4 ± 1.2 to 5.4 ± 1.6 (p = 0.002) in intravenous PGI2 group (Figure 1).
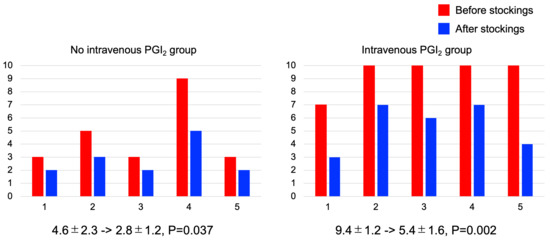
Figure 1.
Effects of compression stockings evaluated by Numeric Rating Scale for Pain (NRS). In intravenous prostacyclin analogue (PGI2) group, four of five patients had score 10 (worst) before stockings. Wearing compression stockings significantly improved NRS score in both groups.
The PDAS score also showed similar results (Figure 2). In both groups, PDAS score was significantly improved [no intravenous PGI2 group; 18.0 (15.0–24.0) to 15.0 (10.0–19.0), p = 0.018, intravenous PGI2 group; 25.0 (17.0–37.0) to 17.0 (5.0–27.0), p = 0.046]. In terms of the specific comments of the PDAS, all five subjects in no intravenous PGI2 group showed difficulty in performing “chores such as vacuuming and gardening”, “carrying heavy stuffs”, and “walking on level ground”, and four patients improved in the difficulty of “walking on a level ground” after compression stockings. In the intravenous PGI2 group, all five patients felt difficulty in the following items: “going out for shopping”, “going up and down stairs”, “carrying heavy stuffs”, and “walking on level ground”. After compression stockings, all five patients improved in “going out for shopping” and “walking on level ground”, and four of them improved in “going up and down stairs”.
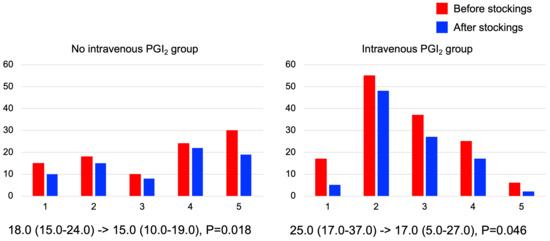
Figure 2.
Effects of compression stockings evaluated by Pain Disability Assessment Scale (PDAS). Wearing compression stockings significantly improved PDAS score in both groups.
3.3. Specific Symptoms before and after Compression Stockings
Before compression stockings, their complaints were “It is hard to stand up. Shopping is pain.”, “I can’t play with my kids after I pick up from kindergarten. It is hard to prepare dinner.”, and “I work standing. In 30 min, my legs start to hurt, and I cry.” For patient-specific symptom relief, we have recommended self-care such as resting, sitting down, resting with legs up, or massage. After the patients started compression stockings, they have changed to “At the moment I put them on, I feel my legs light, completely different! Edema and leg cramp have reduced.”, “I feel less pain when working. I can come home after shopping.”, and “I can walk!”, suggesting reduction of pain when shopping or working, as well as leg edema. However, there was no change in knee or heel pain. In addition, there were some complaints from patients that it was some difficult to wear compression stockings and also that it was stuffy. During the observational period, no varicose vein, lymphedema, or skin problems were observed in the lower extremities in the enrolled patients.
4. Discussion
This is the first report to demonstrate the favorable effects of compression stockings on lower limbs symptoms in PAH patients. Pulmonary vasodilators for PAH treatment often cause side effects in their lower extremities, but the patients have always given them up. We have usually recommended only self-care such as resting, sitting down, or massage. Many PAH patients have had difficulties in shopping, housework, and working out, due to lower extremity symptoms. Now, we are able to recommend the compression stockings to relieve the lower limbs symptom caused by pulmonary vasodilators.
4.1. Lower Limbs Symptoms in PAH Patients
Although the prognosis of PAH has been remarkably improved as therapeutic options have developed more and more for these two decades, [6] ADEs caused by pulmonary vasodilators commonly occurred in PAH patients, which might be dose-dependent and dose-related [12]. However, ADEs in early phase of PAH treatment was not associated with the improved mortality [12]. Therefore, ADEs, which impair the patients’ QOL, are not welcome and should be avoided. ADEs caused by pulmonary vasodilators have been reported as headache, gastrointestinal symptoms, jaw pain, and extremity pain [7,13,14]. Especially, pain in lower limbs brings big problems in daily lives, which should be relieved.
4.2. Compression Stockings
Compression stockings are used for lower extremity varicose veins, lymphedema, and other venous and lymphatic diseases, which are effective in relieving symptoms such as lower extremity swelling and dullness [15]. As the present study indicated, pulmonary vasodilators impair the activities of daily lives in many patients with PAH due to lower extremity symptoms, such as walking, shopping, childcare, housework, and working. It has been shown that compression stockings are effective in reducing pain and symptoms in patients suffering from chronic venous insufficiency, [16] because the compression therapy improves venous pumping by reducing the venous cross sectional diameters, the contraction of the calf muscles to press the veins of the lower extremities, and squeezing out the blood flow, all of which improve venous return [17]. Compression therapy may also work on leg edema improvement, which is caused by right heart failure in PAH patients [18]. Congestion in the lower extremities causes various subjective symptoms such as dullness, hot flushes, pain, swelling, itching, and cramps during sleep, which can be improved by compression stockings. In particular, the intravenous PGI2 group had worse symptoms and difficulties, in whom wearing elastic stockings were also able to alleviate the symptoms and to reduce the difficulties in daily lives.
We have a patient experience first that wearing elastic stockings has reduced the pain in her lower limbs and made her easier to work, and then confirmed the effects in ten patients. The adverse effects of pulmonary vasodilators have not been focused much; however, now that the prognosis of PAH has been improved, [4,5,6] we have to look at the ADEs of pulmonary vasodilators.
There are some contraindications in compression stockings, which should not be offered to patients with severe congestive cardiac failure, due to a risk that systemic fluid overload might be developed [15]. However, reducing moderate edemas, without shifting larger blood volumes toward the right heart, can be achieved using light compression stockings [15]. Further in patients with critical limb ischemia, with systolic ankle pressure below 70 mmHg or following arterial bypass grafting, compression stockings are contraindicated as there is a risk of ischemia or local skin necrosis, especially if the limb is elevated [15]. Other damages, which may be caused by stockings, include advanced peripheral neuropathy, fragile tissue paper skin over the bony prominences, dermatitis, and allergic reactions to the fabric [15]. In such cases, compression stockings should be used and customized to the individual limb measurements.
4.3. Limitations
The present study has several limitations. First, the present study had a small number of enrolled subjects, and the effect of elastic stockings could not be sufficiently clarified. Second, this was a single-arm, open label, and retrospective study, with a potential bias. Third, we need to prospectively clarify the beneficial effects of compression stockings in a larger population. We are planning to perform the multi-center, prospective study, considering careful indication of compression stockings [15].
5. Conclusions
Lower limbs symptoms were strong in PAH patients treated by pulmonary vasodilators. Compression stockings attenuated their lower extremities symptoms and improved their quality of lives.
Author Contributions
Conceptualization, N.N.; methodology, N.N. and Y.F.; formal analysis, N.T.; investigation, C.G. and S.T.; data curation, Y.S., M.B., S.M.-O. and A.H.; writing—original draft preparation, N.N.; writing—review and editing, Y.F.; supervision, Y.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The present study was approved by the institutional review board at Kurume University (21296) and conducted in accordance with ethical principals in the Declaration of Helsinki.
Informed Consent Statement
All patients provided written informed consent.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Fukuda, K.; Date, H.; Doi, S.; Fukumoto, Y.; Fukushima, N.; Hatano, M.; Ito, H.; Kuwana, M.; Matsubara, H.; Momomura, S.I.; et al. Guidelines for the Treatment of Pulmonary Hypertension (JCS 2017/JPCPHS 2017). Circ. J. 2019, 83, 842–945. [Google Scholar] [CrossRef] [PubMed]
- Barst, R.J.; Rubin, L.J.; McGoon, M.D.; Caldwell, E.J.; Long, W.A.; Levy, P.S. Survival in primary pulmonary hypertension with long-term continuous intravenous prostacyclin. Ann. Intern. Med. 1994, 121, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Fukumoto, Y.; Shimokawa, H. Recent progress in the management of pulmonary hypertension. Circ. J. 2011, 75, 1801–1810. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, A.; Ejiri, K.; Matsubara, H. Long-term patient survival with idiopathic/heritable pulmonary arterial hypertension treated at a single center in Japan. Life Sci. 2014, 118, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Tamura, Y.; Kumamaru, H.; Satoh, T.; Miyata, H.; Ogawa, A.; Tanabe, N.; Hatano, M.; Yao, A.; Abe, K.; Tsujino, I.; et al. Effectiveness and Outcome of Pulmonary Arterial Hypertension-Specific Therapy in Japanese Patients With Pulmonary Arterial Hypertension. Circ. J. 2017, 82, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, Y.; Tahara, N.; Bekki, M.; Tahara, A.; Honda, A.; Maeda-Ogata, S.; Sun, J.; Igata, S.; Fukumoto, Y. Long-term survival outcome for pre-capillary pulmonary hypertension at a Japanese single center. Can. J. Physiol. Pharmacol. 2020, 98, 644–652. [Google Scholar] [CrossRef] [PubMed]
- Burks, M.; Stickel, S.; Galie, N. Pulmonary Arterial Hypertension: Combination Therapy in Practice. Am. J. Cardiovasc. Drugs 2018, 18, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Downie, W.W.; Leatham, P.A.; Rhind, V.M.; Wright, V.; Branco, J.A.; Anderson, J.A. Studies with pain rating scales. Ann. Rheum. Dis. 1978, 37, 378–381. [Google Scholar] [CrossRef] [PubMed]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis. Care Res. 2011, 63 (Suppl. 11), S240–S252. [Google Scholar] [CrossRef]
- Yamashiro, K.; Arimura, T.; Iwaki, R.; Jensen, M.P.; Kubo, C.; Hosoi, M. A multidimensional measure of pain interference: Reliability and validity of the pain disability assessment scale. Clin. J. Pain 2011, 27, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Shinohara, Y.; Wakaizumi, K.; Ishikawa, A.; Ito, M.; Hoshino, R.; Tanaka, C.; Takaoka, S.; Kawakami, M.; Tsuji, O.; Fujisawa, D.; et al. Improvement in Disability Mediates the Effect of Self-Efficacy on Pain Relief in Chronic Low Back Pain Patients with Exercise Therapy. Pain Res. Manag. 2022, 2022, 4203138. [Google Scholar] [CrossRef] [PubMed]
- Leary, P.J.; Kang, S.; Kolb, T.M.; Maron, B.A.; Ralph, D.D.; Rao, Y.; Tedford, R.J.; Zamanian, R.T. What’s in a side effect? The association between pulmonary vasodilator adverse drug events and clinical outcomes in patients with pulmonary arterial hypertension. Int. J. Cardiol. 2017, 240, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Kataoka, M.; Satoh, T.; Matsubara, H.; Yamamoto, K.; Inada, T.; Umezawa, K.; Takahashi, T.; Nakano, A.; Fukuda, K. Safety and Efficacy of Ambrisentan-Phosphodiesterase Type 5 (PDE5) Inhibitor Combination Therapy for Japanese Pulmonary Arterial Hypertension Patients in Real-World Clinical Practice. Circ. Rep. 2019, 1, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Galie, N.; Gaine, S.; Channick, R.; Coghlan, J.G.; Hoeper, M.M.; Lang, I.M.; McLaughlin, V.V.; Lassen, C.; Rubin, L.J.; Hsu Schmitz, S.F.; et al. Long-Term Survival, Safety and Tolerability with Selexipag in Patients with Pulmonary Arterial Hypertension: Results from GRIPHON and its Open-Label Extension. Adv. Ther. 2022, 39, 796–810. [Google Scholar] [CrossRef] [PubMed]
- Rabe, E.; Partsch, H.; Hafner, J.; Lattimer, C.; Mosti, G.; Neumann, M.; Urbanek, T.; Huebner, M.; Gaillard, S.; Carpentier, P. Indications for medical compression stockings in venous and lymphatic disorders: An evidence-based consensus statement. Phlebology 2018, 33, 163–184. [Google Scholar] [CrossRef] [PubMed]
- Dahm, K.T.; Myrhaug, H.T.; Stromme, H.; Fure, B.; Brurberg, K.G. Effects of preventive use of compression stockings for elderly with chronic venous insufficiency and swollen legs: A systematic review and meta-analysis. BMC Geriatr. 2019, 19, 76. [Google Scholar] [CrossRef] [PubMed]
- Partsch, H. Compression therapy: Clinical and experimental evidence. Ann. Vasc. Dis. 2012, 5, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Cassady, S.J.; Ramani, G.V. Right Heart Failure in Pulmonary Hypertension. Cardiol. Clin. 2020, 38, 243–255. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).