A Comparison of 13C-Methacetin and 13C-Octanoate Breath Test for the Evaluation of Nonalcoholic Steatohepatitis
Abstract
1. Introduction
Aim
2. Materials and Methods
2.1. Study Design
2.2. Clinical Exam
2.3. Blood Tests
2.4. Abdominal Ultrasound
2.5. Liver Biopsy
2.6. Breath Testing Protocols
2.7. Inclusion Criteria
2.8. Exclusion Criteria
2.9. Study Groups
2.10. Statistical Analysis
3. Results
3.1. Characteristics of Patients
3.2. Univariate Analysis
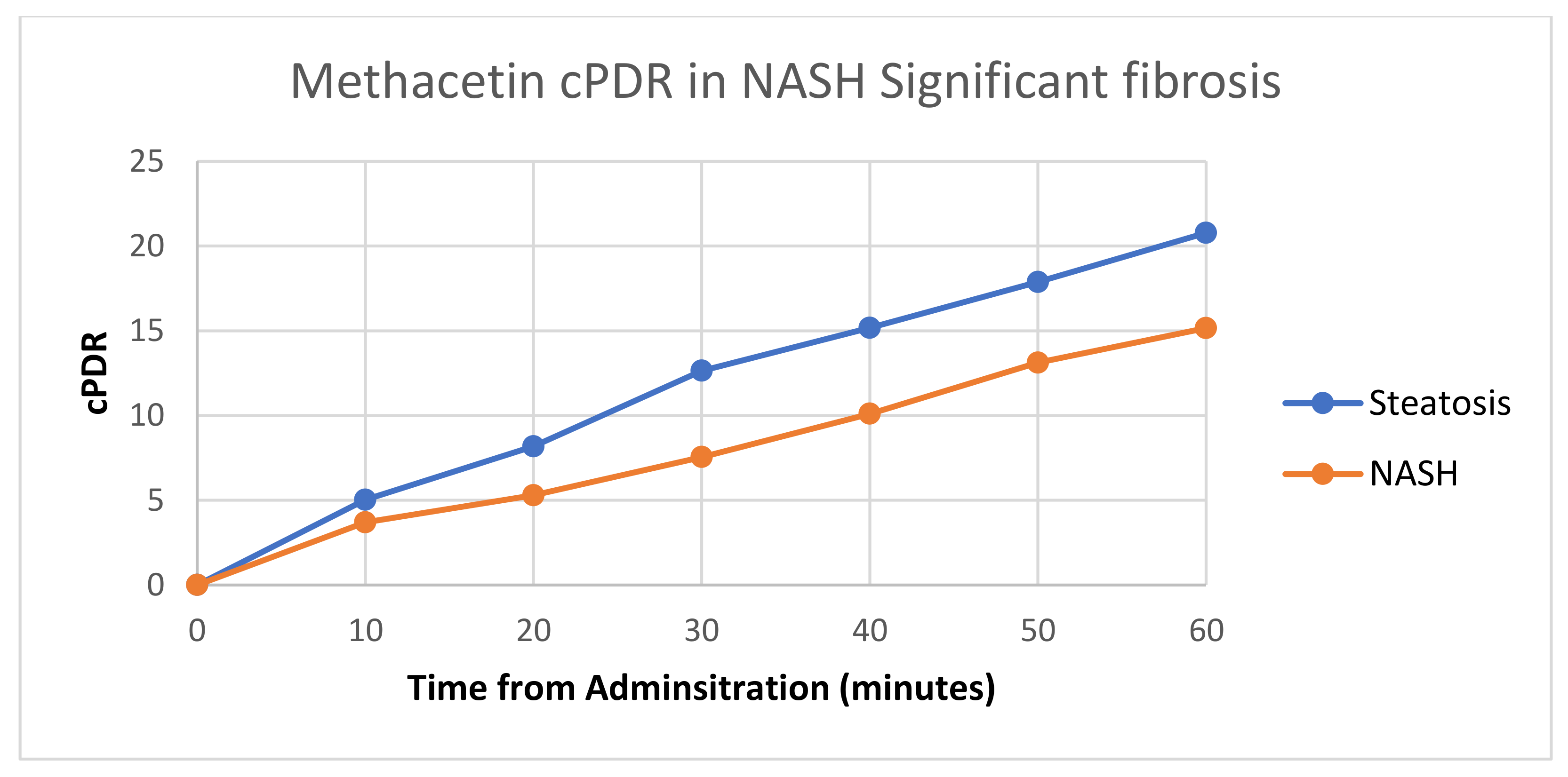
3.3. Diagnostic Performance of the 13C Breath Test
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Excluded Patients
| Exclusion Criterion | Number |
| Severe COPD | 24 |
| Severe Asthma | 6 |
| Uncontrolled diabetes | 19 |
| Severe heart failure | 23 |
| Malabsorption syndrome | 1 |
| Recent acute disease—medical | 5 |
| Recent acute disease—surgical | 2 |
| Pregnancy | 1 |
| Total | 81 |
References
- Mazzolini, G.; Sowa, J.P.; Atorrasagasti, C.; Kucukoglu, O.; Syn, W.K.; Canbay, A. Significance of Simple Steatosis: An Update on the Clinical and Molecular Evidence. Cells 2018, 43, 2458. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Koenig, A.B.; Abdelatif, D.; Fazel, Y.; Henry, L.; Wymer, M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016, 64, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Spengler, E.K.; Loomba, R. Recommendations for Diagnosis, Referral for Liver Biopsy, and Treatment of Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis. Mayo Clin. Proc. 2015, 90, 1233–1246. [Google Scholar] [CrossRef] [PubMed]
- Atwell, T.D.; Smith, R.L.; Hesley, G.K.; Callstrom, M.R.; Schleck, C.D.; Harmsen, W.S.; Charboneau, J.W.; Welch, T.J. Incidence of bleeding after 15,181 percutaneous biopsies and the role of aspirin. AJR Am. J. Roentgenol. 2010, 194, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Piccinino, F.; Sagnelli, E.; Pasquale, G.; Giusti, G. Complications following percutaneous liver biopsy. A multicentre retrospective study on 68,276 biopsies. J. Hepatol. 1986, 2, 165–173. [Google Scholar] [CrossRef]
- Ratziu, V.; Charlotte, F.; Heurtier, A.; Gombert, S.; Giral, P.; Bruckert, E.; Grimaldi, A.; Capron, F.; Poynard, T.; Group, L.S. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology 2005, 128, 1898–1906. [Google Scholar] [CrossRef]
- Fromenty, B.; Robin, M.A.; Igoudjil, A.; Mansouri, A.; Pessayre, D. The ins and outs of mitochondrial dysfunction in NASH. Diabetes Metab. 2004, 30, 121–138. [Google Scholar] [CrossRef]
- Ghoos, Y.F.; Maes, B.D.; Geypens, B.J.; Mys, G.; Hiele, M.I.; Rutgeerts, P.J.; Vantrappen, G. Measurement of gastric emptying rate of solids by means of a carbon-labeled octanoic acid breath test. Gastroenterology 1993, 104, 1640–1647. [Google Scholar] [CrossRef]
- DeLany, J.P.; Windhauser, M.M.; Champagne, C.M.; Bray, G.A. Differential oxidation of individual dietary fatty acids in humans. Am. J. Clin. Nutr. 2000, 72, 905–911. [Google Scholar] [CrossRef]
- Karvonen, I.; Stengard, J.H.; Saarni, H.U.; Stenback, F.; Sotaniemi, E.A. Hepatic mixed function oxidase system and enzymatic glucose metabolism in rats. Diabetes. Res. 1987, 4, 195–200. [Google Scholar]
- Braden, B.; Faust, D.; Sarrazin, U.; Zeuzem, S.; Dietrich, C.F.; Caspary, W.F.; Sarrazin, C. 13C-methacetin breath test as liver function test in patients with chronic hepatitis C virus infection. Aliment. Pharmacol. Ther. 2005, 21, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Gorowska-Kowolik, K.; Chobot, A.; Kwiecien, J. (13)C Methacetin Breath Test for Assessment of Microsomal Liver Function: Methodology and Clinical Application. Gastroenterol. Res. Pract. 2017, 2017, 7397840. [Google Scholar] [CrossRef] [PubMed]
- Holtmeier, J.; Leuschner, M.; Schneider, A.; Leuschner, U.; Caspary, W.F.; Braden, B. 13C-methacetin and 13C-galactose breath tests can assess restricted liver function even in early stages of primary biliary cirrhosis. Scand. J. Gastroenterol. 2006, 41, 1336–1341. [Google Scholar] [CrossRef] [PubMed]
- Klatt, S.; Taut, C.; Mayer, D.; Adler, G.; Beckh, K. Evaluation of the 13C-methacetin breath test for quantitative liver function testing. Z. Gastroenterol. 1997, 35, 609–614. [Google Scholar] [PubMed]
- Murgia, A.; Ahmed, Y.; Sweeney, K.; Nicholson-Scott, L.; Arthur, K.; Allsworth, M.; Boyle, B.; Gandelman, O.; Smolinska, A.; Ferrandino, G. Breath-Taking Perspectives and Preliminary Data toward Early Detection of Chronic Liver Diseases. Biomedicines 2021, 9, 1563. [Google Scholar] [CrossRef]
- Fromenty, B.; Roden, M. Mitochondrial alterations in fatty liver diseases. J. Hepatol. 2023, 78, 415–429. [Google Scholar] [CrossRef]
- Nascimbeni, F.; Bedossa, P.; Fedchuk, L.; Pais, R.; Charlotte, F.; Lebray, P.; Poynard, T.; Ratziu, V.; Group, L.S. Clinical validation of the FLIP algorithm and the SAF score in patients with non-alcoholic fatty liver disease. J. Hepatol. 2020, 72, 828–838. [Google Scholar] [CrossRef]
- Chen, Z.; Tian, R.; She, Z.; Cai, J.; Li, H. Role of oxidative stress in the pathogenesis of nonalcoholic fatty liver disease. Free Radic. Biol. Med. 2020, 152, 116–141. [Google Scholar] [CrossRef]
- Miele, L.; Grieco, A.; Armuzzi, A.; Candelli, M.; Forgione, A.; Gasbarrini, A.; Gasbarrini, G. Hepatic mitochondrial beta-oxidation in patients with nonalcoholic steatohepatitis assessed by 13C-octanoate breath test. Am. J. Gastroenterol. 2003, 98, 2335–2336. [Google Scholar] [CrossRef]
- Fierbinteanu-Braticevici, C.; Calin-Necula, A.M.; Enciu, V.T.; Goran, L.; Pantea Stoian, A.; Ancuta, I.; Viasu, O.; Moldoveanu, A.C. The Role of Noninvasive (13)C-Octanoate Breath Test in Assessing the Diagnosis of Nonalcoholic Steatohepatitis. Diagnostics 2022, 12, 2935. [Google Scholar] [CrossRef]
- Hughey, C.C.; Puchalska, P.; Crawford, P.A. Integrating the contributions of mitochondrial oxidative metabolism to lipotoxicity and inflammation in NAFLD pathogenesis. Biochim. Biophys. Acta (BBA) Mol. Cell Biol. Lipids 2022, 1867, 159209. [Google Scholar] [CrossRef] [PubMed]
- Molina-Molina, E.; Shanmugam, H.; Di Ciaula, A.; Grattagliano, I.; Di Palo, D.M.; Palmieri, V.O.; Portincasa, P. ((13)C)-Methacetin breath test provides evidence of subclinical liver dysfunction linked to fat storage but not lifestyle. JHEP Rep. 2021, 3, 100203. [Google Scholar] [CrossRef] [PubMed]
- Di Ciaula, A.; Shanmugam, H.; Ribeiro, R.; Pina, A.; Andrade, R.; Bonfrate, L.; Raposo, J.F.; Macedo, M.P.; Portincasa, P. Liver fat accumulation more than fibrosis causes early liver dynamic dysfunction in patients with non-alcoholic fatty liver disease. Eur. J. Intern. Med. 2023, 107, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Moldoveanu, A.C.; Fierbinteanu-Braticevici, C. A Primer into the Current State of Artificial Intelligence in Gastroenterology. J. Gastrointest. Liver Dis. 2022, 31, 244–253. [Google Scholar] [CrossRef] [PubMed]

| Variable | F0 | F1 | F2 | F3 | F4 | Method | p-Value |
|---|---|---|---|---|---|---|---|
| Number | 32 (40%) | 10 (12%) | 8 (10%) | 12 (15%) | 19 (23%) | ||
| Age | 44.62 (SD = 13.45) | 57.1 (SD = 12.52) | 50.25 (SD = 9.04) | 51.83 (SD = 7.31) | 54.21 (SD = 11.46) | ANOVA | 0.016 |
| BMI | 28.81 (SD = 6.2) | 31.5 (SD = 6.55) | 30.88 (SD = 6.49) | 30.58 (SD = 4.42) | 31.16 (SD = 5.53) | ANOVA | 0.575 |
| Glucose | 110.0 [66–173] | 106.0 [71–124] | 118.0 [95–153] | 112.0 [92–143] | 138.0 [69–205] | KW | 0.170 |
| HOMA | 2.9 [1.7–3.89] | 2.84 [2.4–3.09] | 2.86 [2.12–3.5] | 3.24 [2.76–4.34] | 3.28 [2.27–5.19] | KW | 0.027 |
| Triglycerides | 167.0 [99–315] | 185.0 [105–293] | 186.0 [152–347] | 200.0 [123–327] | 201.0 [74–302] | KW | 0.073 |
| Cholesterol | 226.0 (SD = 95.0) | 191.0 (SD = 46.0) | 200.0 (SD = 35.0) | 227.0 (SD = 74.0) | 230.0 (SD = 51.0) | ANOVA | 0.590 |
| HDL | 35.25 (SD = 7.45) | 39.4 (SD = 2.76) | 33.5 (SD = 13.72) | 35.08 (SD = 7.32) | 33.53 (SD = 7.56) | ANOVA | 0.404 |
| ALT | 64.0 [21–133] | 61.0 [40–204] | 100.0 [46–158] | 96.0 [58–126] | 99.0 [59–157] | KW | 0.002 |
| AST | 74.0 [48–127] | 74.0 [51–114] | 84.0 [53–116] | 80.0 [66–138] | 86.0 [51–134] | KW | 0.349 |
| ALB | 4.0 [3–5] | 3.0 [2–5] | 3.0 [3–4] | 3.0 [2–4] | 3.0 [2–4] | KW | 0.002 |
| INR | 1.0 [0.8–1.3] | 1.1 [0.9–1.2] | 1.0 [0.9–1.2] | 0.95 [0.9–1.3] | 1.0 [0.9–1.1] | KW | 0.388 |
| γGT | 78.0 [38–185] | 96.0 [41–127] | 103.0 [84–192] | 119.0 [78–233] | 114.0 [69–279] | KW | <0.001 |
| FERITIN | 147.0 [114–228] | 145.0 [111–185] | 134.0 [106–264] | 160.0 [127–390] | 177.0 [129–284] | KW | 0.065 |
| CRP | 1.62 [0.6–6.11] | 3.54 [1.58–7.03] | 4.54 [1.99–8.46] | 5.16 [3.6–7.8] | 5.52 [3.25–8.33] | KW | <0.001 |
| URIC ACID | 5.07 [3.06–8.36] | 4.92 [4.24–9.85] | 6.18 [2.84–8.65] | 7.27 [5.53–9.35] | 6.36 [4.58–8.6] | KW | <0.001 |
| Spleen Diameter | 105.0 (SD = 12.0) | 108.0 (SD = 10.0) | 111.0 (SD = 10.0) | 121.0 (SD = 11.0) | 124.0 (SD = 15.0) | ANOVA | <0.001 |
| Abdominal circumference | 91.0 [65–104] | 91.0 [82–107] | 95.0 [74–131] | 94.0 [76–131] | 92.0 [64–110] | KW | 0.697 |
| Sex | 21 F (26%)/11 M (11%) | 7 F (9%)/3 M (4%) | 6 F (7%)/2 M (2%) | 3 F (4%)/9 M (11%) | 8 F (10%)/11 M (14%) | Chi | 0.054 |
| MDose10 | 32.32 [27.68–43.06] | 33.29 [10.67–41.45] | 24.7 [16.83–43.77] | 10.83 [5.36–23.67] | 9.92 [6.48–43.44] | KW | <0.001 |
| MDose20 | 29.56 [23.73–36.31] | 30.41 [8.73–36.45] | 30.74 [10.1–52.75] | 10.87 [9.53–31.68] | 11.1 [8.35–32.0] | KW | <0.001 |
| MDose30 | 23.64 [20.12–27.61] | 26.03 [14.16–30.57] | 29.3 [13.63–32.15] | 14.3 [12.66–35.1] | 14.72 [11.81–31.77] | KW | 0.001 |
| MDose40 | 19.35 [16.08–24.35] | 20.74 [17.08–27.91] | 26.12 [17.0–32.33] | 18.97 [14.58–30.87] | 16.99 [13.66–27.63] | KW | 0.014 |
| MDose50 | 16.02 [13.71–17.99] | 16.74 [13.9–23.25] | 20.96 [13.4–24.79] | 13.9 [11.47–25.94] | 13.43 [11.34–24.27] | KW | 0.002 |
| MDose60 | 13.62 [11.85–15.23] | 13.66 [10.23–20.32] | 15.16 [10.69–20.15] | 11.25 [8.85–17.94] | 11.61 [8.58–16.41] | KW | 0.001 |
| cMDose10 | 5.21 [4.09–6.2] | 5.02 [2.33–6.11] | 3.47 [2.74–10.18] | 3.08 [2.52–3.52] | 2.92 [2.51–8.06] | KW | <0.001 |
| cMDose20 | 8.52 [6.34–10.82] | 7.78 [3.36–10.12] | 5.42 [3.58–13.7] | 4.01 [3.47–5.31] | 4.9 [3.12–12.17] | KW | <0.001 |
| cMDose30 | 13.33 [10.3–15.15] | 12.54 [3.96–14.6] | 8.36 [5.75–21.61] | 5.76 [4.12–9.93] | 6.24 [3.34–16.64] | KW | <0.001 |
| cMDose40 | 15.46 [12.79–17.5] | 15.58 [4.82–17.96] | 10.36 [9.26–25.61] | 8.24 [6.25–11.05] | 8.49 [5.33–21.61] | KW | <0.001 |
| cMDose50 | 18.12 [14.87–21.17] | 18.28 [7.33–20.49] | 13.15 [12.09–26.96] | 11.28 [8.89–14.83] | 11.25 [8.76–25.17] | KW | <0.001 |
| cMDose60 | 21.26 [17.7–24.83] | 20.77 [7.94–24.58] | 14.18 [13.25–30.66] | 12.09 [9.72–18.92] | 13.8 [9.27–28.44] | KW | <0.001 |
| ODose15 | 20.26 [8.39–24.68] | 16.75 [13.06–22.63] | 15.69 [13.67–20.5] | 22.82 [16.02–29.11] | 22.97 [15.9–28.87] | KW | <0.001 |
| ODose30 | 16.74 [13.05–25.45] | 18.37 [15.28–20.04] | 18.8 [16.7–26.47] | 22.91 [19.66–29.2] | 23.81 [18.21–29.06] | KW | <0.001 |
| ODose45 | 15.73 [12.91–22.59] | 18.08 [15.39–20.26] | 18.37 [15.86–22.37] | 19.92 [17.25–26.02] | 21.84 [18.84–27.41] | KW | <0.001 |
| ODose60 | 13.48 [11.14–20.5] | 15.43 [14.69–17.48] | 16.12 [13.82–19.19] | 15.79 [13.9–17.55] | 17.02 [13.17–22.65] | KW | <0.001 |
| ODose120 | 8.37 [3.17–14.26] | 9.34 [6.27–11.24] | 9.84 [6.69–10.6] | 8.7 [7.09–13.03] | 10.03 [8.01–14.86] | KW | 0.033 |
| cODose15 | 2.0 [1.12–3.15] | 2.25 [1.1–3.9] | 2.07 [1.11–3.75] | 2.8 [2.16–5.89] | 3.32 [1.29–4.72] | KW | <0.001 |
| cODose30 | 7.36 [4.39–9.68] | 6.87 [5.08–8.09] | 7.29 [5.94–8.38] | 8.32 [6.22–12.17] | 9.0 [6.18–10.62] | KW | <0.001 |
| cODose45 | 11.32 [9.52–15.85] | 9.48 [8.8–14.18] | 9.54 [8.36–14.3] | 13.64 [8.75–18.25] | 13.81 [10.12–18.83] | KW | 0.002 |
| cODose60 | 15.58 [12.39–19.69] | 15.72 [14.2–17.91] | 17.14 [15.05–20.23] | 17.88 [16.2–21.38] | 18.49 [15.24–22.84] | KW | <0.001 |
| cODose120 | 25.7 [20.43–34.07] | 28.02 [24.71–32.4] | 27.64 [26.22–35.11] | 30.6 [26.35–33.73] | 31.85 [27.6–39.98] | KW | <0.001 |
| Variable | Group 1 | Group 2 | Group 3 | Method | p-Value |
|---|---|---|---|---|---|
| Number | 31 (38%) | 11 (14%) | 39 (48%) | ||
| Age | 47.26 (SD = 15.11) | 48.55 (SD = 11.6) | 52.67 (SD = 9.77) | ANOVA | 0.179 |
| BMI | 28.13 (SD = 5.94) | 33.18 (SD = 6.08) | 30.92 (SD = 5.29) | ANOVA | 0.024 |
| Glucose | 107.0 [66–168] | 110.0 [78–173] | 117.0 [69–205] | KW | 0.065 |
| HOMA | 2.85 [1.7–3.69] | 2.85 [2.56–3.89] | 3.18 [2.12–5.19] | KW | 0.03 |
| Triglycerides | 174.0 [130–293] | 163.0 [99–315] | 201.0 [74–347] | KW | 0.013 |
| Cholesterol | 212.0 (SD = 94.0) | 234.0 (SD = 63.0) | 223.0 (SD = 57.0) | ANOVA | 0.662 |
| HDL | 35.55 (SD = 6.6) | 38.18 (SD = 7.47) | 34.0 (SD = 8.82) | ANOVA | 0.285 |
| ALT | 57.0 [21–133] | 78.0 [54–204] | 98.0 [46–158] | KW | <0.001 |
| AST | 74.0 [48–117] | 83.0 [51–127] | 84.0 [51–138] | KW | 0.063 |
| ALB | 4.0 [2–5] | 3.0 [3–4] | 3.0 [2–4] | KW | 0.001 |
| INR | 1.0 [0.9–1.3] | 1.0 [0.8–1.1] | 1.0 [0.9–1.3] | KW | 0.455 |
| γGT | 77.0 [38–121] | 122.0 [41–185] | 114.0 [69–279] | KW | <0.001 |
| FERITIN | 146.0 [111–203] | 154.0 [119–228] | 162.0 [106–390] | KW | 0.039 |
| CRP | 2.06 [0.6–5.71] | 5.52 [0.63–7.03] | 5.33 [1.99–8.46] | KW | <0.001 |
| URIC ACID | 4.88 [3.06–7.26] | 6.09 [4.51–9.85] | 6.84 [2.84–9.35] | KW | <0.001 |
| Spleen Diameter | 104.0 (SD = 11.0) | 110.0 (SD = 11.0) | 121.0 (SD = 13.0) | ANOVA | <0.001 |
| Abdominal circumference | 89.0 [65–104] | 95.0 [88–107] | 93.0 [64–131] | KW | 0.01 |
| Sex | 22 F/9 M | 6 F/5 M | 17 F/22 M | Chi | 0.072 |
| MDose10 | 32.87 [10.67–43.06] | 32.62 [27.68–37.84] | 16.34 [5.36–43.77] | KW | <0.001 |
| MDose20 | 29.21 [8.73–36.31] | 30.74 [26.34–36.45] | 11.36 [8.35–52.75] | KW | 0.001 |
| MDose30 | 23.72 [14.16–30.57] | 25.47 [20.63–27.61] | 15.12 [11.81–35.1] | KW | 0.29 |
| MDose40 | 19.55 [16.08–27.91] | 19.54 [16.61–26.33] | 19.08 [13.66–32.33] | KW | 0.777 |
| MDose50 | 15.77 [13.84–23.25] | 17.2 [13.71–22.72] | 14.04 [11.34–25.94] | KW | 0.192 |
| MDose60 | 13.57 [10.23–17.36] | 13.74 [12.33–20.32] | 11.74 [8.58–20.15] | KW | 0.005 |
| cMDose10 | 5.3 [2.33–6.11] | 5.05 [4.61–6.2] | 3.11 [2.51–10.18] | KW | <0.001 |
| cMDose20 | 8.5 [3.36–10.82] | 7.76 [6.34–9.49] | 4.27 [3.12–13.7] | KW | <0.001 |
| cMDose30 | 13.12 [3.96–15.15] | 13.29 [11.95–14.6] | 6.42 [3.34–21.61] | KW | <0.001 |
| cMDose40 | 15.68 [4.82–17.96] | 15.14 [14.26–16.36] | 9.26 [5.33–25.61] | KW | <0.001 |
| cMDose50 | 18.47 [7.33–21.17] | 17.74 [17.04–19.19] | 12.15 [8.76–26.96] | KW | <0.001 |
| cMDose60 | 21.7 [7.94–24.83] | 20.68 [17.7–23.94] | 13.69 [9.27–30.66] | KW | <0.001 |
| ODose15 | 19.83 [8.39–22.63] | 20.68 [12.59–24.68] | 21.42 [13.67–29.11] | KW | 0.014 |
| ODose30 | 16.86 [13.05–25.45] | 17.66 [15.78–25.35] | 22.57 [16.7–29.2] | KW | <0.001 |
| ODose45 | 17.95 [12.91–22.44] | 17.52 [13.25–22.59] | 21.16 [15.86–27.41] | KW | <0.001 |
| ODose60 | 14.36 [11.14–20.5] | 14.69 [11.28–17.36] | 16.24 [13.17–22.65] | KW | <0.001 |
| ODose120 | 9.18 [3.17–14.26] | 8.42 [7.02–11.52] | 9.75 [6.69–14.86] | KW | 0.056 |
| cODose15 | 2.29 [1.1–3.9] | 1.83 [1.22–3.15] | 2.85 [1.11–5.89] | KW | 0.005 |
| cODose30 | 7.17 [4.39–9.68] | 7.45 [5.77–9.1] | 8.47 [5.94–12.17] | KW | <0.001 |
| cODose45 | 11.31 [8.92–15.85] | 10.94 [8.8–14.43] | 12.64 [8.36–18.83] | KW | 0.036 |
| cODose60 | 15.63 [12.68–19.69] | 16.09 [12.39–18.59] | 18.14 [15.05–22.84] | KW | <0.001 |
| cODose120 | 26.08 [20.43–34.07] | 27.91 [20.91–30.96] | 30.97 [26.22–39.98] | KW | <0.001 |
| Variable | F0 | F1 | F2 | F3 | F4 | Total |
|---|---|---|---|---|---|---|
| A0 | 20 | 6 | 0 | 0 | 0 | 26 |
| A1 | 5 | 0 | 0 | 0 | 0 | 5 |
| A2 | 5 | 2 | 5 | 10 | 12 | 34 |
| A3 | 2 | 2 | 3 | 1 | 7 | 15 |
| A4 | 0 | 0 | 0 | 1 | 0 | 1 |
| Total | 32 | 10 | 8 | 12 | 19 | 81 |
| NASH | Significant Fibrosis | Cirrhosis | |
|---|---|---|---|
| MDose10 | 0.800 | 0.860 | 0.869 |
| MDose20 | 0.662 | 0.726 | 0.866 |
| MDose30 | 0.548 | 0.596 | 0.793 |
| MDose40 | 0.495 | 0.520 | 0.745 |
| MDose50 | 0.552 | 0.588 | 0.742 |
| MDose60 | 0.619 | 0.702 | 0.811 |
| cMDose10 | 0.791 | 0.833 | 0.844 |
| cMDose20 | 0.817 | 0.848 | 0.823 |
| cMDose30 | 0.825 | 0.891 | 0.889 |
| cMDose40 | 0.823 | 0.868 | 0.895 |
| cMDose50 | 0.808 | 0.849 | 0.897 |
| cMDose60 | 0.818 | 0.825 | 0.858 |
| ODose15 | 0.652 | 0.687 | 0.786 |
| ODose30 | 0.855 | 0.887 | 0.882 |
| ODose45 | 0.760 | 0.774 | 0.879 |
| ODose60 | 0.754 | 0.776 | 0.880 |
| ODose120 | 0.611 | 0.652 | 0.778 |
| cODose15 | 0.648 | 0.711 | 0.791 |
| cODose30 | 0.734 | 0.783 | 0.889 |
| cODose45 | 0.624 | 0.666 | 0.754 |
| cODose60 | 0.789 | 0.763 | 0.882 |
| cODose120 | 0.756 | 0.794 | 0.807 |
| Test 1 | Test 2 | z | p-Value | |
|---|---|---|---|---|
| NASH | ODose30 | CMDose30 | 9.091 | <0.001 |
| Significant Fibrosis | CODose30 | CMDose30 | 9.470 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fierbinteanu-Braticevici, C.; Enciu, V.-T.; Calin-Necula, A.-M.; Papacocea, I.R.; Moldoveanu, A.C. A Comparison of 13C-Methacetin and 13C-Octanoate Breath Test for the Evaluation of Nonalcoholic Steatohepatitis. J. Clin. Med. 2023, 12, 2158. https://doi.org/10.3390/jcm12062158
Fierbinteanu-Braticevici C, Enciu V-T, Calin-Necula A-M, Papacocea IR, Moldoveanu AC. A Comparison of 13C-Methacetin and 13C-Octanoate Breath Test for the Evaluation of Nonalcoholic Steatohepatitis. Journal of Clinical Medicine. 2023; 12(6):2158. https://doi.org/10.3390/jcm12062158
Chicago/Turabian StyleFierbinteanu-Braticevici, Carmen, Vlad-Teodor Enciu, Ana-Maria Calin-Necula, Ioana Raluca Papacocea, and Alexandru Constantin Moldoveanu. 2023. "A Comparison of 13C-Methacetin and 13C-Octanoate Breath Test for the Evaluation of Nonalcoholic Steatohepatitis" Journal of Clinical Medicine 12, no. 6: 2158. https://doi.org/10.3390/jcm12062158
APA StyleFierbinteanu-Braticevici, C., Enciu, V.-T., Calin-Necula, A.-M., Papacocea, I. R., & Moldoveanu, A. C. (2023). A Comparison of 13C-Methacetin and 13C-Octanoate Breath Test for the Evaluation of Nonalcoholic Steatohepatitis. Journal of Clinical Medicine, 12(6), 2158. https://doi.org/10.3390/jcm12062158







