Effect of Hypercholesterolemia, Systemic Arterial Hypertension and Diabetes Mellitus on Peripapillary and Macular Vessel Density on Superficial Vascular Plexus in Glaucoma
Abstract
1. Introduction
2. Material and Methods
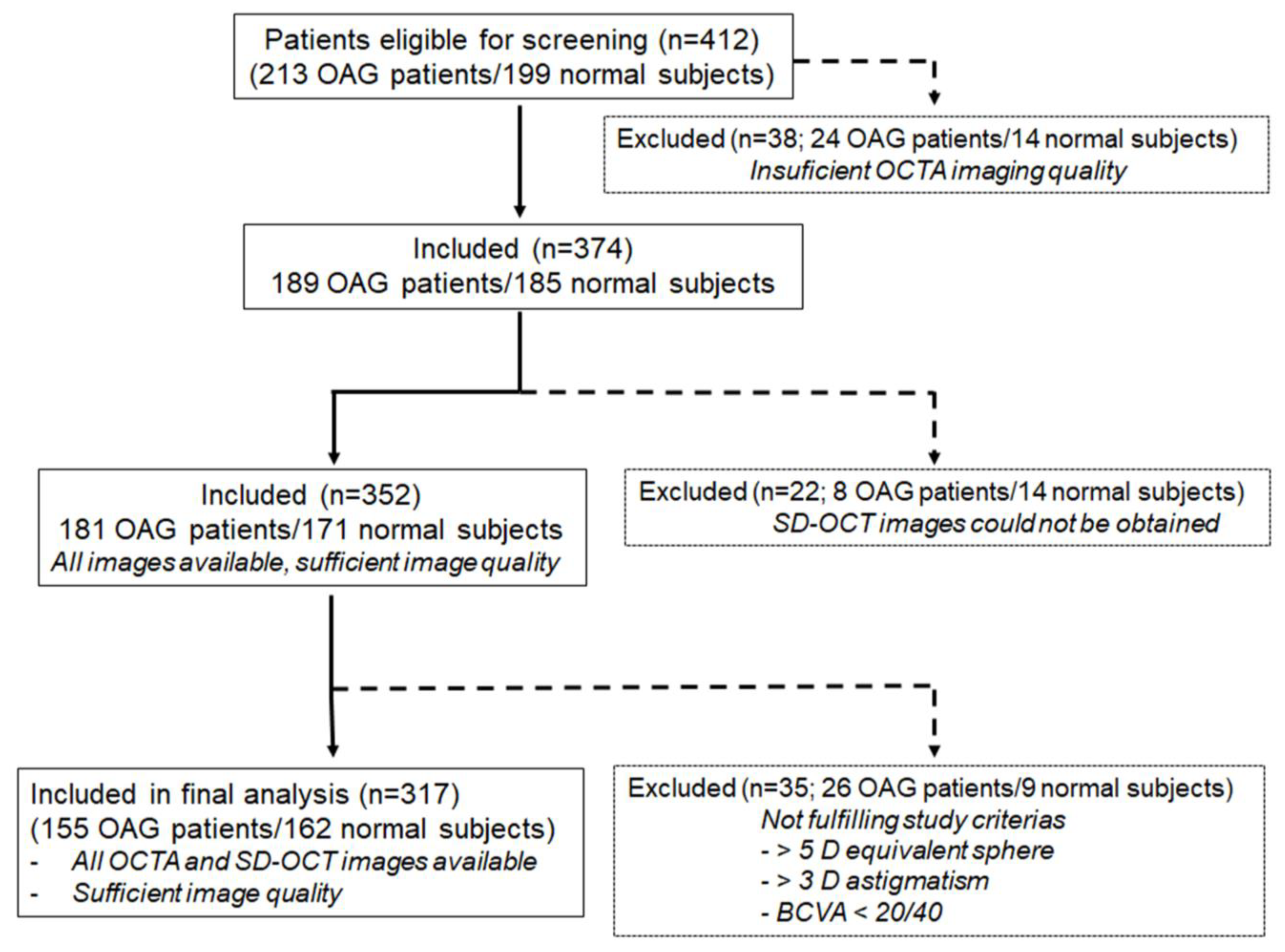
2.1. Study Design
2.2. Study Participants
2.3. Examination Protocol
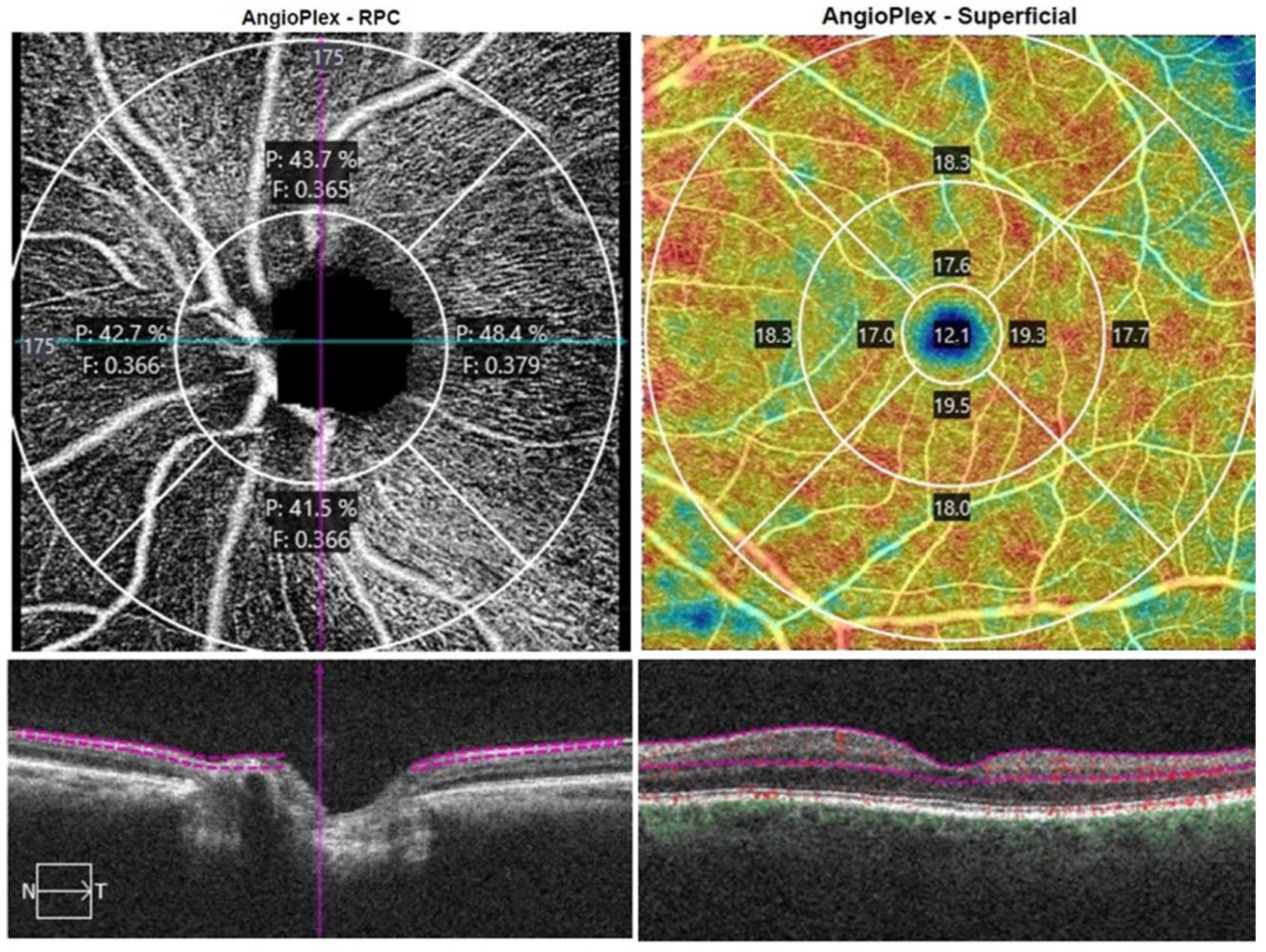
2.4. Optical Coherence Tomography Angiography
2.5. Statistical Analysis
3. Results
3.1. Analysis of Demographics
3.2. Qualitative Analysis
3.3. Quantitative Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AI | Acircularity index |
| AMD | Age-related macular degeneration |
| AUROCS | Areas under the ROC curves |
| BCVA | Best-corrected visual acuity |
| DM | Diabetes mellitus |
| FAZ | Foveal avascular zone |
| GCIPL | Ganglion cell layer and inner plexiform layer |
| GAT | Goldmann applanation tonometer |
| HC | Hypercholesterolemia |
| IOP | Intraocular pressure |
| sMVD | Macular vessel density on superficial vascular plexus |
| MD | Mean defect |
| ONH | Optic nerve head |
| OCT | Optical coherence tomography |
| OCTA | Optical coherence tomography angiography |
| sPVD | Peripapillary vessel density on superficial vascular plexus |
| POAG | Primary open-angle glaucoma |
| ROC | Receiver operating characteristics |
| RNFL | Retinal nerve fiber layer |
| SD | Standard deviation |
| SD-OCT | Spectral domain optical coherence tomography |
| SAH | Systemic arterial hypertension |
References
- Bourne, R.R.A.; Taylor, H.R.; Flaxman, S.R.; Keeffe, J.; Leasher, J.; Naidoo, K.; Pesudovs, K.; White, R.A.; Wong, T.Y.; Resnikoff, S.; et al. Number of People Blind or Visually Impaired by Glaucoma Worldwide and in World Regions 1990–2010: A Meta-Analysis. PLoS ONE 2016, 11, e0162229. [Google Scholar] [CrossRef]
- Ocular Hypertension Treatment Study Group; European Glaucoma Prevention Study Group. Validated Prediction Model for the Development of Primary Open-Angle Glaucoma in Individuals with Ocular Hypertension. Ophthalmology 2007, 114, 10–19.e2. [Google Scholar] [CrossRef]
- Gordon, M.O.; Beiser, J.A.; Brandt, J.D.; Heuer, D.K.; Higginbotham, E.J.; Johnson, C.A.; Keltner, J.L.; Miller, J.P.; Parrish, R.K.; Wilson, M.R.; et al. The Ocular Hypertension Treatment Study: Baseline Factors That Predict the Onset of Primary Open-Angle Glaucoma. Arch. Ophthalmol. 2002, 120, 714–720, discussion 829–830. [Google Scholar] [CrossRef]
- Dueker, D.K.; Singh, K.; Lin, S.C.; Fechtner, R.D.; Minckler, D.S.; Samples, J.R.; Schuman, J.S. Corneal Thickness Measurement in the Management of Primary Open-Angle Glaucoma. Ophthalmology 2007, 114, 1779–1787. [Google Scholar] [CrossRef]
- The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 12. Baseline Risk Factors for Sustained Loss of Visual Field and Visual Acuity in Patients with Advanced Glaucoma. Am. J. Ophthalmol. 2002, 134, 499–512. [Google Scholar] [CrossRef]
- Gillespie, B.W.; Niziol, L.M.; Ehrlich, J.R.; Johnson, C.A.; Caprioli, J.; VanVeldhuisen, P.C.; Lichter, P.R.; Musch, D.C. Demographic, Comorbid, and Clinical Variables Associated with Pointwise Visual Field Damage in Glaucoma: Data From the AGIS and CIGTS Clinical Trials. Transl. Vis. Sci. Technol. 2021, 10, 28. [Google Scholar] [CrossRef] [PubMed]
- Yarmohammadi, A.; Zangwill, L.M.; Diniz-Filho, A.; Suh, M.H.; Yousefi, S.; Saunders, L.J.; Belghith, A.; Manalastas, P.I.C.; Medeiros, F.A.; Weinreb, R.N. Relationship between Optical Coherence Tomography Angiography Vessel Density and Severity of Visual Field Loss in Glaucoma. Ophthalmology 2016, 123, 2498–2508. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.D.; Wolf, A.T.; Harris, A.; Verticchio Vercellin, A.; Siesky, B.; Rowe, L.W.; Packles, M.; Oddone, F. Vascular Biomarkers from Optical Coherence Tomography Angiography and Glaucoma: Where Do We Stand in 2021? Acta Ophthalmol. 2022, 100, e377–e385. [Google Scholar] [CrossRef] [PubMed]
- Burgoyne, C.F.; Crawford Downs, J.; Bellezza, A.J.; Francis Suh, J.-K.; Hart, R.T. The Optic Nerve Head as a Biomechanical Structure: A New Paradigm for Understanding the Role of IOP-Related Stress and Strain in the Pathophysiology of Glaucomatous Optic Nerve Head Damage. Prog. Retin. Eye Res. 2005, 24, 39–73. [Google Scholar] [CrossRef]
- Mursch-Edlmayr, A.-S.; Bolz, M.; Strohmaier, C. Vascular Aspects in Glaucoma: From Pathogenesis to Therapeutic Approaches. Int. J. Mol. Sci. 2021, 22, 4662. [Google Scholar] [CrossRef]
- Wang, S.; Bao, X. Hyperlipidemia, Blood Lipid Level, and the Risk of Glaucoma: A Meta-Analysis. Investig. Ophthalmol. Vis. Sci. 2019, 60, 1028. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.E.; Oh, S.; Baek, S.U.; Ahn, S.J.; Park, K.H.; Jeoung, J.W. Ocular Perfusion Pressure and the Risk of Open-Angle Glaucoma: Systematic Review and Meta-Analysis. Sci. Rep. 2020, 10, 10056. [Google Scholar] [CrossRef]
- Costa, L.; Cunha, J.P.; Amado, D.; Pinto, L.A.; Ferreira, J. Diabetes Mellitus as a Risk Factor in Glaucoma’s Physiopathology and Surgical Survival Time: A Literature Review. J. Curr. Glaucoma Pract. 2015, 9, 81–85. [Google Scholar]
- Salobrar-Garcia, E.; Méndez-Hernández, C.; de Hoz, R.; Ramírez, A.I.; López-Cuenca, I.; Fernández-Albarral, J.A.; Rojas, P.; Wang, S.; García-Feijoo, J.; Gil, P.; et al. Ocular Vascular Changes in Mild Alzheimer’s Disease Patients: Foveal Avascular Zone, Choroidal Thickness, and ONH Hemoglobin Analysis. J. Pers. Med. 2020, 10, 231. [Google Scholar] [CrossRef]
- Madala, S.; Adabifirouzjaei, F.; Lando, L.; Yarmohammadi, A.; Long, C.P.; Bakhoum, C.Y.; Goldbaum, M.H.; Sarraf, D.; DeMaria, A.N.; Bakhoum, M.F. Retinal Ischemic Perivascular Lesions, a Biomarker of Cardiovascular Disease. Ophthalmol. Retin. 2022, 6, 865–867. [Google Scholar] [CrossRef] [PubMed]
- Kasumovic, A.; Matoc, I.; Rebic, D.; Avdagic, N.; Halimic, T. Assessment of Retinal Microangiopathy in Chronic Kidney Disease Patients. Med. Arch. 2020, 74, 191. [Google Scholar] [CrossRef]
- Wagner, S.K.; Fu, D.J.; Faes, L.; Liu, X.; Huemer, J.; Khalid, H.; Ferraz, D.; Korot, E.; Kelly, C.; Balaskas, K.; et al. Insights into Systemic Disease through Retinal Imaging-Based Oculomics. Transl. Vis. Sci. Technol. 2020, 9, 6. [Google Scholar] [CrossRef]
- Ptito, M.; Bleau, M.; Bouskila, J. The Retina: A Window into the Brain. Cells 2021, 10, 3269. [Google Scholar] [CrossRef]
- Kashani, A.H.; Chen, C.-L.; Gahm, J.K.; Zheng, F.; Richter, G.M.; Rosenfeld, P.J.; Shi, Y.; Wang, R.K. Optical Coherence Tomography Angiography: A Comprehensive Review of Current Methods and Clinical Applications. Prog. Retin. Eye Res. 2017, 60, 66–100. [Google Scholar] [CrossRef]
- Rao, H.L.; Pradhan, Z.S.; Suh, M.H.; Moghimi, S.; Mansouri, K.; Weinreb, R.N. Optical Coherence Tomography Angiography in Glaucoma. J. Glaucoma 2020, 29, 312–321. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the Areas under Two or More Correlated Receiver Operating Characteristic Curves: A Nonparametric Approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef]
- Weinreb, R.N.; Aung, T.; Medeiros, F.A. The Pathophysiology and Treatment of Glaucoma. JAMA 2014, 311, 1901. [Google Scholar] [CrossRef]
- Boned-Murillo, A.; Albertos-Arranz, H.; Diaz-Barreda, M.D.; Orduna-Hospital, E.; Sánchez-Cano, A.; Ferreras, A.; Cuenca, N.; Pinilla, I. Optical Coherence Tomography Angiography in Diabetic Patients: A Systematic Review. Biomedicines 2021, 10, 88. [Google Scholar] [CrossRef] [PubMed]
- Anjos, R.; Ferreira, A.; Barkoudah, E.; Claggett, B.; Abegão Pinto, L.; Miguel, A. Application of Optical Coherence Tomography Angiography Macular Analysis for Systemic Hypertension. A Systematic Review and Meta-Analysis. Am. J. Hypertens. 2022, 35, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Eid, P.; Arnould, L.; Gabrielle, P.-H.; Aho, L.S.; Farnier, M.; Creuzot-Garcher, C.; Cottin, Y. Retinal Microvascular Changes in Familial Hypercholesterolemia: Analysis with Swept-Source Optical Coherence Tomography Angiography. J. Pers. Med. 2022, 12, 871. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.; Frueh, B.E.; Steinmair, D.; Ebneter, A.; Wolf, S.; Zinkernagel, M.S.; Munk, M.R. Cataract Significantly Influences Quantitative Measurements on Swept-Source Optical Coherence Tomography Angiography Imaging. PLoS ONE 2018, 13, e0204501. [Google Scholar] [CrossRef] [PubMed]
- Abay, R.N.; Akdeniz, G.Ş.; Katipoğlu, Z.; Kerimoğlu, H. Normative Data Assessment of Age-Related Changes in Macular and Optic Nerve Head Vessel Density Using Optical Coherence Tomography Angiography. Photodiagnosis Photodyn. Ther. 2022, 37, 102624. [Google Scholar] [CrossRef] [PubMed]
- Gadde, S.G.K.; Anegondi, N.; Bhanushali, D.; Chidambara, L.; Yadav, N.K.; Khurana, A.; Sinha Roy, A. Quantification of Vessel Density in Retinal Optical Coherence Tomography Angiography Images Using Local Fractal Dimension. Investig. Ophthalmol. Vis. Sci. 2016, 57, 246. [Google Scholar] [CrossRef] [PubMed]
- Rao, H.L.; Pradhan, Z.S.; Weinreb, R.N.; Reddy, H.B.; Riyazuddin, M.; Sachdeva, S.; Puttaiah, N.K.; Jayadev, C.; Webers, C.A.B. Determinants of Peripapillary and Macular Vessel Densities Measured by Optical Coherence Tomography Angiography in Normal Eyes. J. Glaucoma 2017, 26, 491–497. [Google Scholar] [CrossRef]
- Wang, S.; Mendez-Hernandez, C.; Arribas-Pardo, P.; Salazar Quiñones, L.; Fernandez-Perez, C.; Garcia-Feijoo, J. Gender-Related Influences on Superficial Papillary Microcirculation Measured with Optical Coherence Tomography Angiography in Patients with Glaucoma. Curr. Eye Res. 2020, 45, 1534–1542. [Google Scholar] [CrossRef]
- Yip, V.C.H.; Wong, H.T.; Yong, V.K.Y.; Lim, B.A.; Hee, O.K.; Cheng, J.; Fu, H.; Lim, C.; Tay, E.L.T.; Loo-Valdez, R.G.; et al. Optical Coherence Tomography Angiography of Optic Disc and Macula Vessel Density in Glaucoma and Healthy Eyes. J. Glaucoma 2019, 28, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Triolo, G.; Rabiolo, A.; Shemonski, N.D.; Fard, A.; di Matteo, F.; Sacconi, R.; Bettin, P.; Magazzeni, S.; Querques, G.; Vazquez, L.E.; et al. Optical Coherence Tomography Angiography Macular and Peripapillary Vessel Perfusion Density in Healthy Subjects, Glaucoma Suspects, and Glaucoma Patients. Investig. Ophthalmol. Vis. Sci. 2017, 58, 5713. [Google Scholar] [CrossRef] [PubMed]
- Oddone, F.; Lucenteforte, E.; Michelessi, M.; Rizzo, S.; Donati, S.; Parravano, M.; Virgili, G. Macular versus Retinal Nerve Fiber Layer Parameters for Diagnosing Manifest Glaucoma. Ophthalmology 2016, 123, 939–949. [Google Scholar] [CrossRef] [PubMed]
- Rezkallah, A.; Douma, I.; Bonjour, M.; Mathis, T.; Kodjikian, L.; Denis, P. Evaluation of the Correlation between Regional Retinal Ganglion Cell Damage and Visual Field Sensitivity in Patients with Advanced Glaucoma. J. Clin. Med. 2022, 11, 4880. [Google Scholar] [CrossRef] [PubMed]
| Normal + Glaucoma Subjects (n = 317) | Normal (n = 162) | Glaucoma (n = 155) | p Value | |
|---|---|---|---|---|
| Gender (M/F) | 118/199 | 59/140 | 94/119 | 0.002 & |
| Age (yr) | 58.27 ± 20.55 | 50.37 ± 21.17 | 66.53 ± 16.24 | <0.0001 # |
| Patients taking glaucoma medications | 52 (32.2%) | - | 52 (32.2%) | - |
| Number of glaucoma medications | 0.56 [0; 1] | - | 1 [0; 2] | - |
| Glaucoma surgery | 18 (11.6%) | - | 18 (11.6%) | - |
| Mean Defect (dB) | 2 [−0.25; 3.5] | 0.7 [−2.05; 3.1] | 2.5 [0.4; 5.2] | 0.038 * |
| Arterial hypertension | 123/194 | 34 (21%) | 89 (57.4%) | <0.0001 & |
| Diabetes mellitus | 44/273 | 14 (8.6%) | 30 (19.3%) | 0.005 & |
| Hypercholesterolaemia | 90/127 | 20 (12.3%) | 70 (45.2%) | <0.0001 & |
| Pseudophakia | 88/229 | 34 (21%) | 54 (34.8%) | 0.004 & |
| Visual Acuity | 0.79 ± 0.24 | 0.79 ± 0.27 | 0.74 ± 0.26 | 0.068 # |
| Sphere | 0.34 ± 1.94 | 0.1 ± 1.96 | 0.60 ± 1.89 | 0.021 # |
| Astigmatism | −0.75 [−1.25; −0.5] | −0.75 [−1.25; −0.5] | −1 [−1.5; −0.5] | 0.001 * |
| IOP GAT (mmHg) | 16.62 ± 3.82 | 15.52 ± 2.79 | 17.77 ± 4.38 | <0.0001 # |
| IOP iCare (mmHg) | 16.79 ± 4.06 | 15.88 ± 3.05 | 17.73 ± 4.73 | <0.0001 # |
| CCT (µ) | 529.23 ± 65.79 | 532.33 ± 56.75 | 526.00 ± 74.13 | 0.393 # |
| SD-OCT parameters | ||||
| Disc area (mm2) | 1.84 ± 0.30 | 1.85 ± 0.37 | 1.84 ± 0.38 | 0.937 # |
| Rim area (mm2) | 1.21 ± 0.30 | 1.34 ± 0.24 | 1.08 ± 0.30 | <0.0001 # |
| C/D | 0.54 ± 0.19 | 0.47 ± 0.20 | 0.60 ± 0.17 | <0.0001 # |
| Vertical C/D | 0.51 ± 0.189 | 0.44 ± 0.17 | 0.58 ± 0.18 | <0.0001 # |
| Cup Volume | 0.21 ± 0.19 | 0.14 ± 0.14 | 0.27 ± 0.22 | <0.0001 # |
| RNFL (µ) | 89.57 ± 13.04 | 94.431 ± 9.30 | 84.48 ± 14.42 | <0.0001 # |
| GCIPL (µ) | 261.49 ± 30.17 | 258.25 ± 30.49 | 264.88 ± 29.55 | 0.050 # |
| Normal (n = 162) | Glaucoma (n = 155) | p Value | |
|---|---|---|---|
| Peripapillary OCTA Vessel Density | |||
| Whole Peripapillary Perfusion Density (%) | 44.92 ± 1.65 | 43.22 ± 2.64 | <0.0001 |
| Whole Peripapillary Blood Flux Index | 0.44 ± 0.03 | 0.41 ± 0.04 | <0.0001 |
| Peripapillary Perfusion Density in the superior quadrant (%) | 43.22 ± 2.33 | 41.12 ± 3.64 | <0.0001 |
| Peripapillary Blood Flux Index in the superior quadrant | 0.43 ± 0.03 | 0.40 ± 0.04 | <0.0001 |
| Peripapillary Perfusion Density in the inferior quadrant (%) | 45.25 ± 2.28 | 41.90 ± 4.07 | <0.0001 |
| Peripapillary Blood Flux Index in the inferior quadrant | 0.44 ± 0.03 | 0.40 ± 0.04 | <0.0001 |
| Peripapillary Perfusion Density in the temporal quadrant (%) | 47.33 ± 2.82 | 46.61 ± 2.72 | 0.021 |
| Peripapillary Blood Flux Index in the temporal quadrant | 0.46 ± 0.42 | 0.42 ± 0.05 | <0.0001 |
| Peripapillary Perfusion Density in the nasal quadrant (%) | 43.82 ± 2.33 | 42.85 ± 2.85 | 0.001 |
| Peripapillary Blood Flux Index in the nasal quadrant | 0.45 ± 0.04 | 0.41 ± 0.04 | <0.0001 |
| Macular OCTA Vessel Density | |||
| Whole Macular Perfusion Density (%) | 43.72 ± 4.55 | 40.88 ± 5.75 | <0.0001 |
| Macular Perfusion Density in the outer circle (%) | 45.04 ± 4.71 | 41.94 ± 5.74 | <0.0001 |
| Macular Perfusion Density in the inner circle (%) | 42.28 ± 4.81 | 39.96 ± 6.74 | <0.0001 |
| Macular Perfusion Density in the central circle (%) | 21.38 ± 7.44 | 20.18 ± 8.35 | 0.177 |
| Foveal Avascular Zone Area (mm2) | 0.23 ± 0.11 | 0.21 ± 0.13 | 0.191 |
| Foveal Avascular Perimeter (mm) | 1.96 ± 0.50 | 1.96 ± 0.75 | 0.929 |
| Acircularity Index | 0.71 ± 0.09 | 0.68 ± 0.11 | 0.005 |
| Whole Peripapillary Perfusion Density (%) | Peripapillary Perfusion Density in the Superior Quadrant (%) | Peripapillary Perfusion Density in the Inferior Quadrant (%) | Peripapillary Perfusion Density in the Temporal Quadrant (%) | Peripapillary Perfusion Density in the Nasal Quadrant (%) | Whole Macular Perfusion Density (%) | Macular Perfusion Density in the Outer Circle (%) | Macular Perfusion Density in the Inner Circle (%) | Macular Perfusion Density in the Central Circle (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Age (yr) | −0.397 (<0.0001) § | −0.305 (<0.0001) § | −0.397 (<0.0001) § | −0.221 (<0.0001) § | −0.171 (0.002) § | −0.478 (<0.0001) § | −0.484 (<0.0001) § | −0.388 (<0.0001) § | −0.254 (<0.0001) § |
| Glaucoma medications | −0.363 (<0.0001) * | −0.320 (<0.0001) * | −0.443 (<0.0001) * | −0.127 (0.024) * | −0.183 (0.001) * | −0.267 (<0.0001) * | −0.319 (<0.0001) * | ||
| Mean Defect (dB) | −0.630 (0.002) * | −0.686 (<0.0001) * | |||||||
| Visual Acuity | 0.136 (0.016) § | 0.171 (0.002) § | 0.270 (<0.0001) § | 0.277 (<0.0001) § | 0.202 (<0.0001) § | 0.196 (0.001) § | |||
| Sphere | −0.145 (0.010) § | −0.218 (<0.0001) § | |||||||
| Astigmatism | 0.159 (0.009) * | 0.195 (0.032) * | 0.191 (0.002) * | −0.120 (0.048) * | 0.336 (<0.0001) * | 0.338 (<0.0001) * | 0.218 (<0.0001) * | 0.131 (0.020) * | |
| IOP GAT (mmHg) | −0.142 (0.011) § | −0.142 (0.011) § | |||||||
| IOP iCare (mmHg) | |||||||||
| CCT (µ) | 0.267 (<0.0001) § | 0.269 (<0.0001) § | 0.161 (0.004) § | 0.134 (0.017) § | 0.232 (<0.0001) § | ||||
| SD-OCT parameters | |||||||||
| Disc area (mm2) | |||||||||
| Rim area (mm2) | 0.471 (<0.0001) § | 0.351 (<0.0001) § | 0.502 (<0.0001) § | 0.259 (<0.0001) § | 0.294 (<0.0001) § | 0.204 (<0.0001) § | 0.253 (<0.0001) § | −0.145 (0.010) § | |
| C/D | −0.248 (<0.0001) § | −0.212 (<0.0001) § | −0.290 (<0.0001) § | −0.143 (0.011) § | −0.124 (0.028) § | −0.146 (0.009) § | |||
| Vertical C/D | −0.327 (<0.0001) § | −0.249 (<0.0001) § | −0.371 (<0.0001) § | −0.181 (0.001) § | −0.174 (0.002) § | −0.165 (0.003) § | −0.202 (<0.0001) § | ||
| Cup Volume | −0.276 (<0.0001) § | −0.220 (<0.0001) § | −0.361 (<0.0001) § | −0.129 (0.022) § | −0.133 (0.018) § | ||||
| RNFL (µ) | 0.356 (<0.0001) § | 0.429 (<0.0001) § | 0.313 (<0.0001) § | 0.253 (<0.0001) § | 0.172 (0.002) § | 0.204 (<0.0001) § | |||
| GCIPL (µ) | −0.196 (<0.0001) § | −0.153 (0.006) § | −0.223 (<0.0001) § | 0.136 (0.016) § | −0.157 (0.005) § | −0.115 (0.041) § | −0.137 (0.014) § | 0.282 (<0.0001) § |
| β | 95%CI | p | |
|---|---|---|---|
| Whole Peripapillary Perfusion Density (%) | |||
| Diabetes mellitus | 0.925 | (0.293; 1.558) | 0.004 |
| Gender | 1.190 | (0.750; 1.631) | <0.0001 |
| Pseudophakia | 1.795 | (1.311; 2.280) | <0.0001 |
| Glaucoma | 1.228 | (0.798; 1.659) | <0.0001 |
| Peripapillary Perfusion Density in the superior quadrant (%) | |||
| Pseudophakia | 2.082 | (1.379; 2.784) | <0.0001 |
| Gender | 1.497 | (0.857; 2.136) | <0.0001 |
| Diabetes mellitus | 1.153 | (0.235; 2.070) | 0.014 |
| Glaucoma | 1.542 | (0.917; 2.166) | <0.0001 |
| Peripapillary Perfusion Density in the inferior quadrant (%) | |||
| Gender | 1.886 | (1.215; 2.558) | <0.0001 |
| Pseudophakia | 2.225 | (1.376; 3.074) | <0.001 |
| Glaucoma | 2.530 | (1.823; 3.238) | <0.0001 |
| Peripapillary Perfusion Density in the temporal quadrant (%) | |||
| Pseudophakia | 0.942 | (0.156; 1.727) | 0.019 |
| Age | −0.019 | (−0.036; −0.002) | 0.029 |
| Peripapillary Perfusion Density in the nasal quadrant (%) | |||
| Diabetes mellitus | 1.205 | (0.389; 2.020) | 0.004 |
| Gender | 1.006 | (0.438; 1.574) | 0.001 |
| Pseudophakia | 1.151 | (0.527; 1.776) | <0.0001 |
| Glaucoma | 0.576 | (0.438; 1.574) | 0.042 |
| Whole Macular Perfusion Density (%) | |||
| Age | −0.081 | (−0.115; −0.047) | <0.0001 |
| Hypercholesterolaemia | 1.324 | (0.015; 2.634) | 0.047 |
| Macular Perfusion Density in the outer circle (%) | |||
| Age | −0.072 | (−0.106; −0.039) | <0.001 |
| Pseudophakia | 1.921 | (0.568; 3.274) | 0.006 |
| Arterial Hypertension | 1.513 | (0.216; 2.810) | 0.022 |
| Hypercholesterolaemia | 1.549 | (0.240; 2.858) | 0.021 |
| Macular Perfusion Density in the inner circle (%) | |||
| Age | −0.112 | (−0.142; −0.083) | <0.0001 |
| Macular Perfusion Density in the central circle (%) | |||
| Age | −0.125 | (−0.173; −0.077) | <0.001 |
| Pseudophakia | −2.384 | (−4.595; −0.174) | 0.035 |
| Foveal Avascular Zone Area (mm2) | |||
| Gender | 0.044 | (0.018; 0.070) | 0.001 |
| Arterial hypertension | 0.048 | (0.022; 0.074) | <0.001 |
| Foveal Avascular Perimeter (mm) | |||
| Arterial hypertension | 0.192 | (0.049; 0.336) | 0.009 |
| Gender | 0.151 | (0.007; 0.296) | 0.040 |
| Acircularity Index | |||
| Age | −0.002 | (−0.002; −0.001) | <0.0001 |
| Sensitivity at 95% Specificity | Sensitivity at 80% Specificity | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AUROC | 95%CI | p-Valor | Cut-Off | Sensitivity | 95%CI | LR+ | LR− | Cut-Off | Sensitivity | 95%CI | LR+ | LR− | ||||
| RNFL (µ) | 0.692 | 0.62 | 0.76 | <0.001 | 80.0 | 0.43 | 0.33 | 0.53 | 8.7 | 0.59 | 86.0 | 0.53 | 0.43 | 0.63 | 2.66 | 0.58 |
| Symmetry | 0.738 | 0.67 | 0.8 | <0.001 | 58.5 | 0.28 | 0.18 | 0.43 | 5.63 | 0.76 | 76.5 | 0.61 | 0.47 | 0.7 | 3.06 | 0.49 |
| Rim area (mm2) | 0.746 | 0.68 | 0.81 | <0.001 | 0.98 | 0.44 | 0.33 | 0.59 | 8.81 | 0.59 | 1.14 | 0.61 | 0.5 | 0.72 | 3.03 | 0.49 |
| Cup Volume | 0.687 | 0.62 | 0.76 | <0.001 | 0.5 | 0.16 | 0.08 | 0.39 | 3.12 | 0.89 | 0.27 | 0.44 | 0.32 | 0.61 | 2.21 | 0.7 |
| Vertical C/D | 0.716 | 0.65 | 0.78 | <0.001 | 0.65 | 0.31 | 0.15 | 0.47 | 6.25 | 0.72 | 0.59 | 0.55 | 0.41 | 0.67 | 2.74 | 0.56 |
| C/D | 0.716 | 0.65 | 0.78 | <0.001 | 0.48 | 0.27 | 0.13 | 0.47 | 5.32 | 0.77 | 0.41 | 0.54 | 0.43 | 0.65 | 2.73 | 0.57 |
| Whole Peripapillary Perfusion Density (%) | 0.708 | 0.64 | 0.78 | <0.001 | 42.05 | 0.25 | 0.1 | 0.38 | 4.95 | 0.79 | 43.6 | 0.53 | 0.34 | 0.65 | 2.65 | 0.59 |
| Whole Peripapillary Blood Flux Index | 0.789 | 0.73 | 0.85 | <0.001 | 0.39 | 0.29 | 0.18 | 0.41 | 5.85 | 0.74 | 0.42 | 0.65 | 0.46 | 0.77 | 3.26 | 0.43 |
| Peripapillary Perfusion Density in the superior quadrant (%) | 0.709 | 0.64 | 0.78 | <0.001 | 38.95 | 0.19 | 0.09 | 0.39 | 3.89 | 0.85 | 41.6 | 0.46 | 0.32 | 0.63 | 2.32 | 0.67 |
| Peripapillary Blood Flux Index in the superior quadrant | 0.772 | 0.71 | 0.84 | <0.001 | 0.38 | 0.31 | 0.15 | 0.48 | 6.27 | 0.72 | 0.41 | 0.64 | 0.48 | 0.78 | 3.19 | 0.45 |
| Peripapillary Perfusion Density in the inferior quadrant (%) | 0.788 | 0.73 | 0.85 | <0.001 | 41.45 | 0.37 | 0.24 | 0.51 | 7.34 | 0.67 | 43.35 | 0.6 | 0.49 | 0.72 | 3.01 | 0.5 |
| Peripapillary Blood Flux Index in the inferior quadrant | 0.763 | 0.70 | 0.83 | <0.001 | 0.39 | 0.27 | 0.17 | 0.4 | 5.36 | 0.77 | 0.42 | 0.56 | 0.39 | 0.69 | 2.8 | 0.55 |
| Peripapillary Perfusion Density in the temporal quadrant (%) | 0.558 | 0.48 | 0.64 | 0.146 | 42.15 | 0.05 | 0.01 | 0.14 | 1.1 | 0.99 | 45.05 | 0.29 | 0.14 | 0.39 | 1.47 | 0.88 |
| Peripapillary Blood Flux Index in the temporal quadrant | 0.769 | 0.7 | 0.83 | <0.001 | 0.39 | 0.22 | 0.13 | 0.41 | 4.45 | 0.82 | 0.43 | 0.56 | 0.41 | 0.77 | 2.79 | 0.55 |
| Peripapillary Perfusion Density in the nasal quadrant (%) | 0.549 | 0.47 | 0.63 | 0.214 | 39.9 | 0.12 | 0.05 | 0.19 | 2.39 | 0.93 | 41.5 | 0.28 | 0.17 | 0.39 | 1.38 | 0.91 |
| Peripapillary Blood Flux Index in the nasal quadrant | 0.792 | 0.73 | 0.85 | <0.001 | 0.39 | 0.27 | 0.14 | 0.5 | 5.47 | 0.76 | 0.42 | 0.59 | 0.46 | 0.73 | 2.95 | 0.51 |
| Whole Macular Perfusion Density (%) | 0.738 | 0.67 | 0.81 | <0.001 | 35.6 | 0.12 | 0.06 | 0.3 | 2.39 | 0.93 | 33.6 | 0.52 | 0.32 | 0.69 | 2.61 | 0.6 |
| Macular Perfusion Density in the outer circle (%) | 0.751 | 0.69 | 0.82 | <0.001 | 36.4 | 0.13 | 0.06 | 0.3 | 2.57 | 0.92 | 44.4 | 0.56 | 0.36 | 0.75 | 2.78 | 0.55 |
| Macular Perfusion Density in the inner circle (%) | 0.573 | 0.5 | 0.65 | 0.065 | 10.95 | 0.13 | 0.03 | 0.24 | 2.57 | 0.92 | 17.15 | 0.32 | 0.21 | 0.43 | 1.61 | 0.85 |
| Macular Perfusion Density in the central circle (%) | 0.629 | 0.55 | 0.71 | 0.001 | 32.7 | 0.13 | 0.06 | 0.36 | 2.57 | 0.92 | 41.25 | 0.47 | 0.33 | 0.59 | 2.33 | 0.67 |
| Acircularity Index | 0.552 | 0.47 | 0.63 | 0.192 | 0.54 | 0.10 | 0.03 | 0.26 | 2.02 | 0.95 | 0.65 | 0.29 | 0.2 | 0.4 | 1.43 | 0.89 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gomez, M.S.; Zeng, N.; Catagna Catagna, G.E.; Arribas-Pardo, P.; Garcia-Feijoo, J.; Mendez-Hernandez, C. Effect of Hypercholesterolemia, Systemic Arterial Hypertension and Diabetes Mellitus on Peripapillary and Macular Vessel Density on Superficial Vascular Plexus in Glaucoma. J. Clin. Med. 2023, 12, 2071. https://doi.org/10.3390/jcm12052071
Gomez MS, Zeng N, Catagna Catagna GE, Arribas-Pardo P, Garcia-Feijoo J, Mendez-Hernandez C. Effect of Hypercholesterolemia, Systemic Arterial Hypertension and Diabetes Mellitus on Peripapillary and Macular Vessel Density on Superficial Vascular Plexus in Glaucoma. Journal of Clinical Medicine. 2023; 12(5):2071. https://doi.org/10.3390/jcm12052071
Chicago/Turabian StyleGomez, María Sanz, Ni Zeng, Gloria Estefania Catagna Catagna, Paula Arribas-Pardo, Julian Garcia-Feijoo, and Carmen Mendez-Hernandez. 2023. "Effect of Hypercholesterolemia, Systemic Arterial Hypertension and Diabetes Mellitus on Peripapillary and Macular Vessel Density on Superficial Vascular Plexus in Glaucoma" Journal of Clinical Medicine 12, no. 5: 2071. https://doi.org/10.3390/jcm12052071
APA StyleGomez, M. S., Zeng, N., Catagna Catagna, G. E., Arribas-Pardo, P., Garcia-Feijoo, J., & Mendez-Hernandez, C. (2023). Effect of Hypercholesterolemia, Systemic Arterial Hypertension and Diabetes Mellitus on Peripapillary and Macular Vessel Density on Superficial Vascular Plexus in Glaucoma. Journal of Clinical Medicine, 12(5), 2071. https://doi.org/10.3390/jcm12052071





