Symptomatic Characteristics of Hypozincemia Detected in Long COVID Patients
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Design and Patients’ Characteristics
2.2. Determination of Serum Zinc Deficiency
2.3. Statistical Analysis
2.4. Ethical Approval
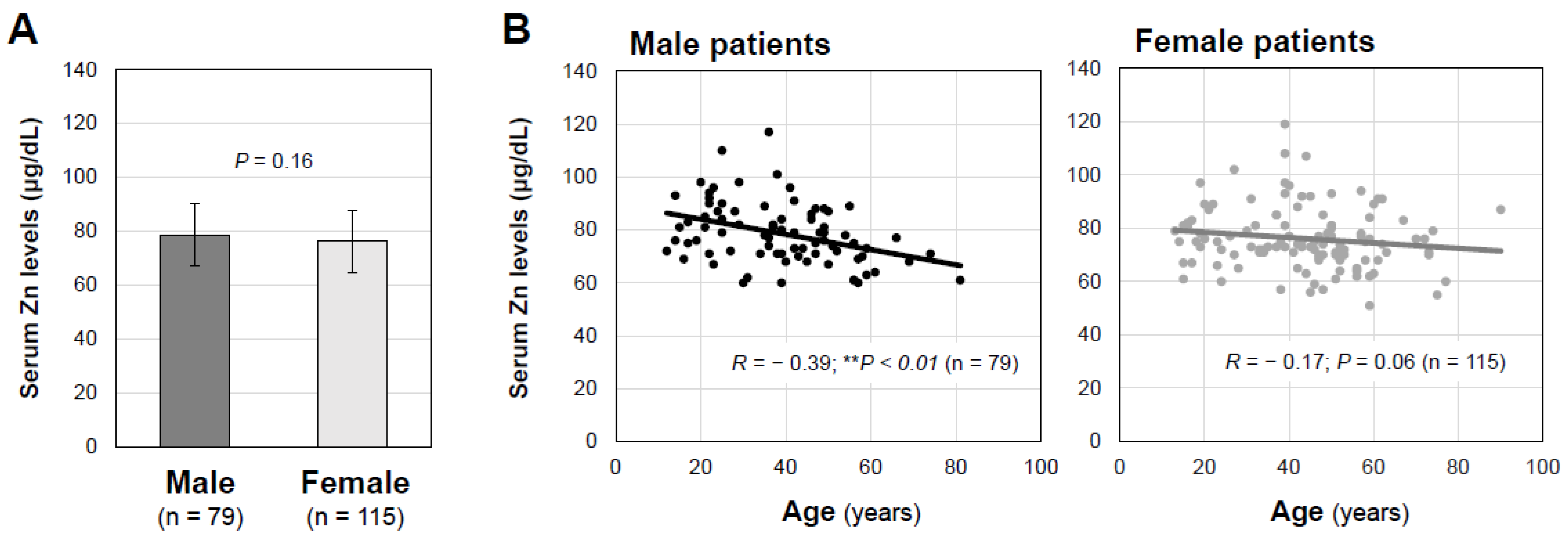
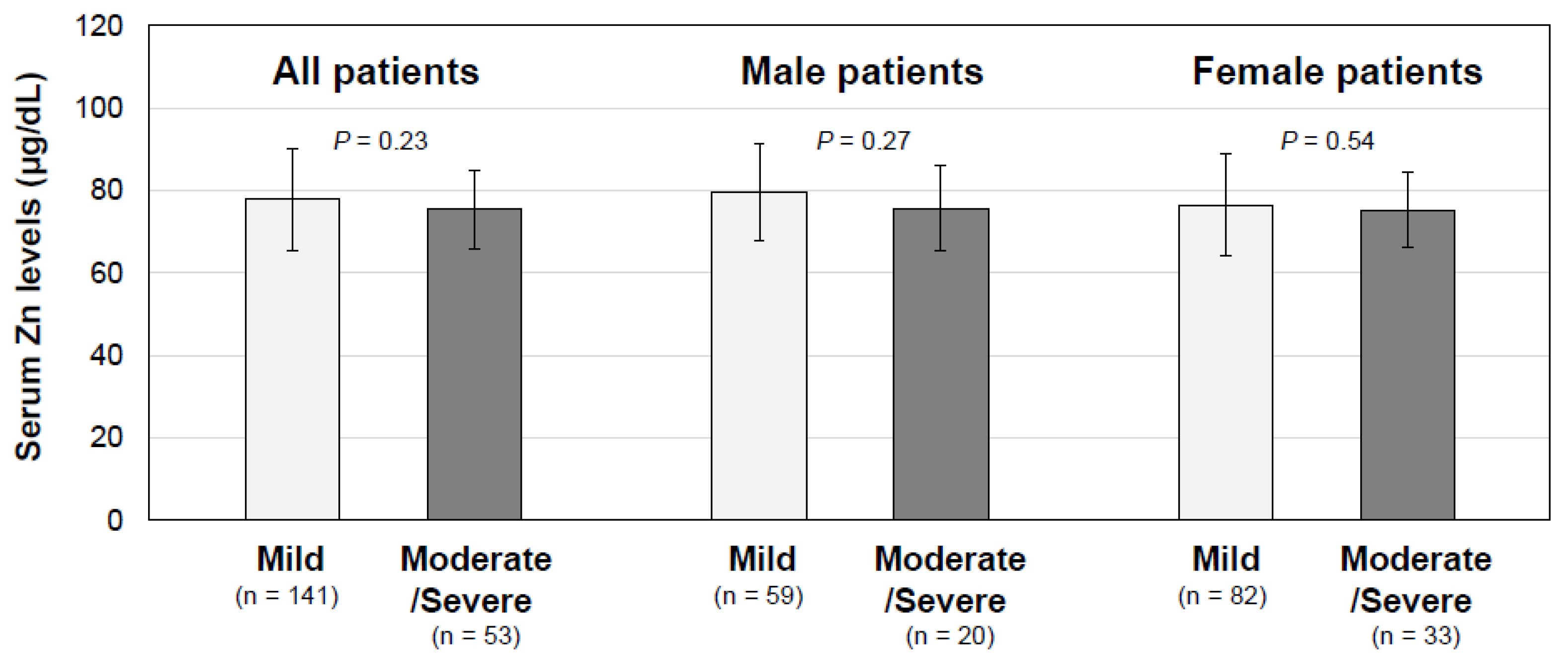
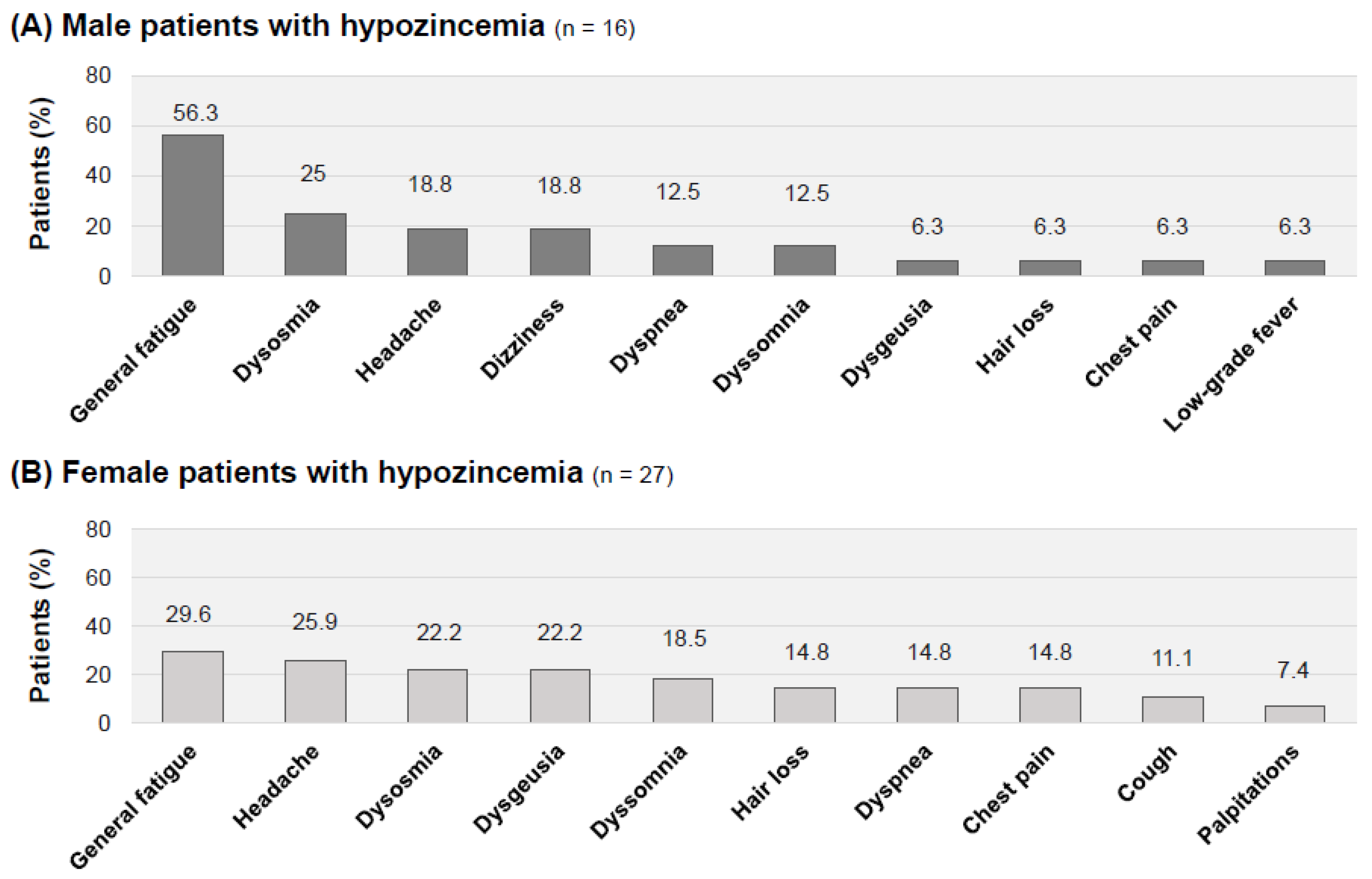
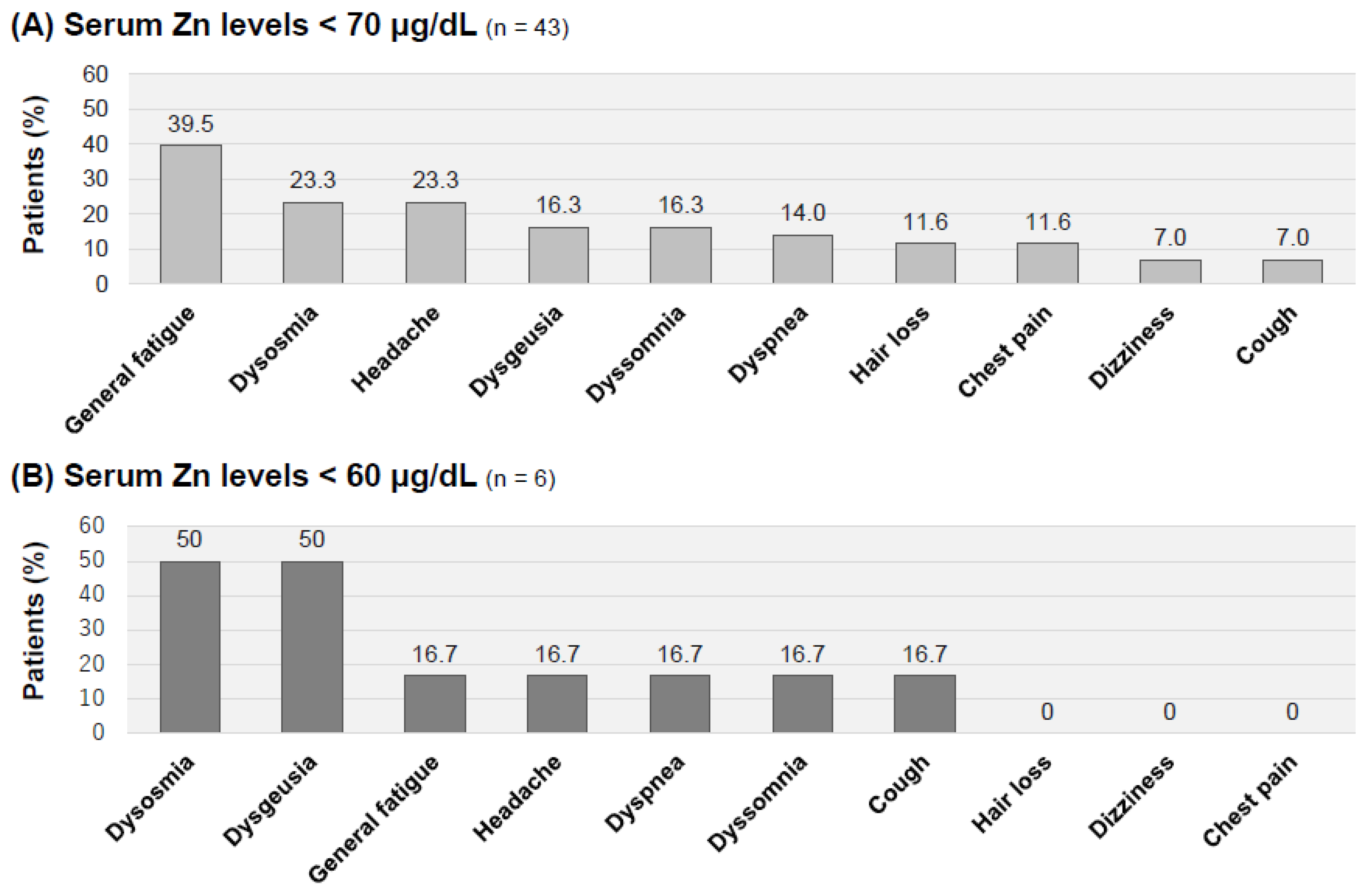
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Docea, A.O.; Tsatsakis, A.; Albulescu, D.; Cristea, O.; Zlatian, O.; Vinceti, M.; Moschos, S.A.; Tsoukalas, D.; Goumenou, M.; Drakoulis, N.; et al. A new threat from an old enemy: Re-emergence of coronavirus (Review). Int. J. Mol. Med. 2020, 45, 1631–1643. [Google Scholar] [CrossRef]
- Soriano, J.B.; Murthy, S.; Marshall, J.C.; Relan, P.; Diaz, J.V. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect. Dis. 2021, 22, e102–e107. [Google Scholar] [CrossRef]
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16144. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, Y.; Tokumasu, K.; Nakano, Y.; Honda, H.; Sakurada, Y.; Sunada, N.; Omura, D.; Hasegawa, K.; Hagiya, H.; Obika, M.; et al. Clinical Characteristics of Japanese Patients Who Visited a COVID-19 Aftercare Clinic for Post-Acute Sequelae of COVID-19/Long COVID. Cureus 2021, 13, e18568. [Google Scholar] [CrossRef] [PubMed]
- Miyazato, Y.; Morioka, S.; Tsuzuki, S.; Akashi, M.; Osanai, Y.; Tanaka, K.; Terada, M.; Suzuki, M.; Kutsuna, S.; Saito, S.; et al. Prolonged and Late-Onset Symptoms of Coronavirus Disease 2019. Open Forum Infect. Dis. 2020, 7, ofaa507. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, Y.; Nakano, Y.; Hagiya, H.; Tokumasu, K.; Otsuka, F. Recovery From Alopecia After COVID-19. Cureus 2022, 14, e21160. [Google Scholar] [CrossRef]
- Almohanna, H.M.; Ahmed, A.A.; Tsatalis, J.P.; Tosti, A. The Role of Vitamins and Minerals in Hair Loss: A Review. Dermatol. Ther. 2019, 9, 51–70. [Google Scholar] [CrossRef]
- Henkin, R.I.; Patten, B.M.; Re, P.K.; Bronzert, D.A. A syndrome of acute zinc loss. Cerebellar dysfunction, mental changes, anorexia, and taste and smell dysfunction. Arch. Neurol. 1975, 32, 745–751. [Google Scholar] [CrossRef]
- Cereda, G.; Ciappolino, V.; Boscutti, A.; Cantu, F.; Enrico, P.; Oldani, L.; Delvecchio, G.; Brambilla, P. Zinc as a Neuroprotective Nutrient for COVID-19-Related Neuropsychiatric Manifestations: A Literature Review. Adv. Nutr. 2022, 13, 66–79. [Google Scholar] [CrossRef]
- Propper, R.E. Smell/Taste alteration in COVID-19 may reflect zinc deficiency. J. Clin. Biochem. Nutr. 2021, 68, 3. [Google Scholar] [CrossRef]
- Shah, W.; Hillman, T.; Playford, E.D.; Hishmeh, L. Managing the long term effects of COVID-19: Summary of NICE, SIGN, and RCGP rapid guideline. BMJ 2021, 372, n136. [Google Scholar] [CrossRef] [PubMed]
- Carfi, A.; Bernabei, R.; Landi, F.; Gemelli Against, C.-P.-A.C.S.G. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Kato, Y. Case Management of COVID-19 (Secondary Version). JMA J. 2021, 4, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Suter, P.M.; Russell, R.M. Vitamin and Trace Mineral Deficiency and Excess. In Harrison’s Principles of Internal Medicine, 20e; Jameson, J.L., Fauci, A.S., Kasper, D.L., Hauser, S.L., Longo, D.L., Loscalzo, J., Eds.; McGraw-Hill Education: New York, NY, USA, 2018. [Google Scholar]
- de Benoist, B.; Darnton-Hill, I.; Davidsson, L.; Fontaine, O.; Hotz, C. Conclusions of the Joint WHO/UNICEF/IAEA/IZiNCG Interagency Meeting on Zinc Status Indicators. Food Nutr. Bull. 2007, 28, S480–S484. [Google Scholar] [CrossRef] [PubMed]
- Hotz, C.; Peerson, J.M.; Brown, K.H. Suggested lower cutoffs of serum zinc concentrations for assessing zinc status: Reanalysis of the second National Health and Nutrition Examination Survey data (1976–1980). Am. J. Clin. Nutr. 2003, 78, 756–764. [Google Scholar] [CrossRef]
- Kodama, H.; Tanaka, M.; Naito, Y.; Katayama, K.; Moriyama, M. Japan’s Practical Guidelines for Zinc Deficiency with a Particular Focus on Taste Disorders, Inflammatory Bowel Disease, and Liver Cirrhosis. Int. J. Mol. Sci. 2020, 21, 2941. [Google Scholar] [CrossRef]
- Yasui, Y.; Yasui, H.; Suzuki, K.; Saitou, T.; Yamamoto, Y.; Ishizaka, T.; Nishida, K.; Yoshihara, S.; Gohma, I.; Ogawa, Y. Analysis of the predictive factors for a critical illness of COVID-19 during treatment—Relationship between serum zinc level and critical illness of COVID-19. Int. J. Infect. Dis. 2020, 100, 230–236. [Google Scholar] [CrossRef]
- Vogel-Gonzalez, M.; Tallo-Parra, M.; Herrera-Fernandez, V.; Perez-Vilaro, G.; Chillon, M.; Nogues, X.; Gomez-Zorrilla, S.; Lopez-Montesinos, I.; Arnau-Barres, I.; Sorli-Redo, M.L.; et al. Low Zinc Levels at Admission Associates with Poor Clinical Outcomes in SARS-CoV-2 Infection. Nutrients 2021, 13, 562. [Google Scholar] [CrossRef]
- Arrieta, F.; Martinez-Vaello, V.; Bengoa, N.; Jimenez-Mendiguchia, L.; Rosillo, M.; de Pablo, A.; Voguel, C.; Martinez-Barros, H.; Pintor, R.; Belanger-Quintana, A.; et al. Serum zinc and copper in people with COVID-19 and zinc supplementation in parenteral nutrition. Nutrition 2021, 91–92, 111467. [Google Scholar] [CrossRef]
- Gammoh, N.Z.; Rink, L. Zinc in Infection and Inflammation. Nutrients 2017, 9, 624. [Google Scholar] [CrossRef]
- Duncan, A.; Talwar, D.; McMillan, D.C.; Stefanowicz, F.; O’Reilly, D.S. Quantitative data on the magnitude of the systemic inflammatory response and its effect on micronutrient status based on plasma measurements. Am. J. Clin. Nutr. 2012, 95, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, T.; Sato, Y.; Kudo, A.; Oikawa, M.; Iijima, H. A study on SARS-CoV-2 infected patients with measured serum zinc levels during home care. Met. Res. 2022, 2, reg-1–reg-10. [Google Scholar] [CrossRef]
- Prasad, A.S. Clinical manifestations of zinc deficiency. Annu. Rev. Nutr. 1985, 5, 341–363. [Google Scholar] [CrossRef]
- Fromonot, J.; Gette, M.; Ben Lassoued, A.; Gueant, J.L.; Gueant-Rodriguez, R.M.; Guieu, R. Hypozincemia in the early stage of COVID-19 is associated with an increased risk of severe COVID-19. Clin. Nutr. 2021, 41, 3115–3119. [Google Scholar] [CrossRef] [PubMed]
- Kodama, H.; Itakura, H.; Omori, H.; Sasaki, M.; Sando, K.; Takamura, T.; Fuse, Y.; Hosoi, T.; Yoshida, H. Practice guideline for zinc deficiency. J. Jpn. Soc. Clin. Nutr. 2018, 40, 120–167. (in Japanese). [Google Scholar]
- Tomita, H. [Zinc-deficient disorders of sense organs--dark adaptation, taste and smell disorders]. Nihon Rinsho 1996, 54, 141–147. [Google Scholar]
- Tokumasu, K.; Honda, H.; Sunada, N.; Sakurada, Y.; Matsuda, Y.; Yamamoto, K.; Nakano, Y.; Hasegawa, T.; Yamamoto, Y.; Otsuka, Y.; et al. Clinical Characteristics of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) Diagnosed in Patients with Long COVID. Medicina 2022, 58, 850. [Google Scholar] [CrossRef]
- Fukuda, K.; Straus, S.E.; Hickie, I.; Sharpe, M.C.; Dobbins, J.G.; Komaroff, A. The chronic fatigue syndrome: A comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann. Intern. Med. 1994, 121, 953–959. [Google Scholar] [CrossRef]
- Carruthers, B.M.; van de Sande, M.I.; De Meirleir, K.L.; Klimas, N.G.; Broderick, G.; Mitchell, T.; Staines, D.; Powles, A.C.; Speight, N.; Vallings, R.; et al. Myalgic encephalomyelitis: International Consensus Criteria. J. Intern. Med. 2011, 270, 327–338. [Google Scholar] [CrossRef]
- Carruthers, B.M.; Jain, A.K.; De Meirleir, K.L.; Peterson, D.L.; Klimas, N.G.; Lerner, A.M.; Bested, A.C.; Flor-Henry, P.; Joshi, P.; Powles, A.C.P.; et al. Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. J. Chronic Fatigue Syndr. 2003, 11, 7–115. [Google Scholar] [CrossRef]
- Clayton, E.W. Beyond myalgic encephalomyelitis/chronic fatigue syndrome: An IOM report on redefining an illness. JAMA 2015, 313, 1101–1102. [Google Scholar] [CrossRef]
- Lim, E.J.; Ahn, Y.C.; Jang, E.S.; Lee, S.W.; Lee, S.H.; Son, C.G. Systematic review and meta-analysis of the prevalence of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). J. Transl. Med. 2020, 18, 100. [Google Scholar] [CrossRef] [PubMed]
- Miyata, S. [Zinc deficiency in the elderly]. Nihon Ronen Igakkai Zasshi 2007, 44, 677–689. [Google Scholar]
- Harada, K.; Hanayama, Y.; Yasuda, M.; Hasegawa, K.; Obika, M.; Kataoka, H.; Itoshima, K.; Okada, K.; Otsuka, F. Clinical relevance of low androgen to gastroesophageal reflux symptoms. Endocr. J. 2018, 65, 1039–1047. [Google Scholar] [CrossRef] [PubMed]
- Prasad, A.S.; Mantzoros, C.S.; Beck, F.W.; Hess, J.W.; Brewer, G.J. Zinc status and serum testosterone levels of healthy adults. Nutrition 1996, 12, 344–348. [Google Scholar] [CrossRef] [PubMed]

| Total | Hypozincemia (Zn < 70 μg/dL) | Normozincemia (Zn ≥ 70 μg/dL) | p Value | |
|---|---|---|---|---|
| Number of patients | 194 | 43 (22.2%) | 151 (77.8%) | |
| Serum zinc concentration (μg/dL), median (IQR) | 75 (70–84) | 63 (60.5–67) | 79 (73–87) | <0.01 (b) ** |
| Age, median (IQR) | 42 (28–52) | 50 (38.5–57.5) | 39 (26.5–50) | <0.01 (a) ** |
| Sex | ||||
| Male | 79 (40.7%) | 16 (37.2%) | 63 (41.7%) | 0.595 (c) |
| Female | 115 (59.3%) | 27 (62.8%) | 88 (58.3%) | |
| BMI, median (IQR) | 23.5 (20.6–26.7) | 23.7 (20.9–27.2) | 23.1 (20.6–26.1) | 0.588 (b) |
| Smoking habit | 79 (40.7%) | 16 (37.2%) | 63 (41.7%) | 0.595 (c) |
| Alcohol drinking habit | 86 (44.3%) | 22 (51.2%) | 64 (42.4%) | 0.307 (c) |
| Admission | 60 (30.9%) | 16 (37.2%) | 44 (29.1%) | 0.312 (c) |
| O2 therapy | 28 (14.4%) | 9 (20.9%) | 19 (12.6%) | 0.169 (c) |
| Severity of COVID-19 in acute phase | ||||
| Mild | 141 (72.7%) | 30 (69.8%) | 111 (73.5%) | 0.173 (c) |
| Moderate | 50 (25.8%) | 11 (25.6%) | 39 (25.8%) | |
| Severe | 3 (1.5%) | 2 (4.6%) | 1 (0.7%) | |
| COVID-19 vaccination | ||||
| None | 117 (60.3%) | 27 (62.8%) | 90 (59.6%) | 0.927 (c) |
| 1 dose | 21 (10.8%) | 4 (9.3%) | 17 (11.3%) | |
| 2 doses | 55 (28.4%) | 12 (27.9%) | 43 (28.5%) | |
| 3 doses | 1 (0.5%) | 0 (0%) | 1 (0.6%) | |
| Duration after the onset of COVID-19 to the 1st visit, median (IQR) | 86 (55.3–128) | 80 (58.5–129.5) | 88 (55.5–128) | 0.528 (b) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsuda, Y.; Tokumasu, K.; Otsuka, Y.; Sunada, N.; Honda, H.; Sakurada, Y.; Nakano, Y.; Hasegawa, T.; Obika, M.; Ueda, K.; et al. Symptomatic Characteristics of Hypozincemia Detected in Long COVID Patients. J. Clin. Med. 2023, 12, 2062. https://doi.org/10.3390/jcm12052062
Matsuda Y, Tokumasu K, Otsuka Y, Sunada N, Honda H, Sakurada Y, Nakano Y, Hasegawa T, Obika M, Ueda K, et al. Symptomatic Characteristics of Hypozincemia Detected in Long COVID Patients. Journal of Clinical Medicine. 2023; 12(5):2062. https://doi.org/10.3390/jcm12052062
Chicago/Turabian StyleMatsuda, Yui, Kazuki Tokumasu, Yuki Otsuka, Naruhiko Sunada, Hiroyuki Honda, Yasue Sakurada, Yasuhiro Nakano, Toru Hasegawa, Mikako Obika, Keigo Ueda, and et al. 2023. "Symptomatic Characteristics of Hypozincemia Detected in Long COVID Patients" Journal of Clinical Medicine 12, no. 5: 2062. https://doi.org/10.3390/jcm12052062
APA StyleMatsuda, Y., Tokumasu, K., Otsuka, Y., Sunada, N., Honda, H., Sakurada, Y., Nakano, Y., Hasegawa, T., Obika, M., Ueda, K., & Otsuka, F. (2023). Symptomatic Characteristics of Hypozincemia Detected in Long COVID Patients. Journal of Clinical Medicine, 12(5), 2062. https://doi.org/10.3390/jcm12052062






