Delayed Surgical Treatment of Displaced Intra-Articular Calcaneal Fractures in Major Trauma Is Safe and Effective
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
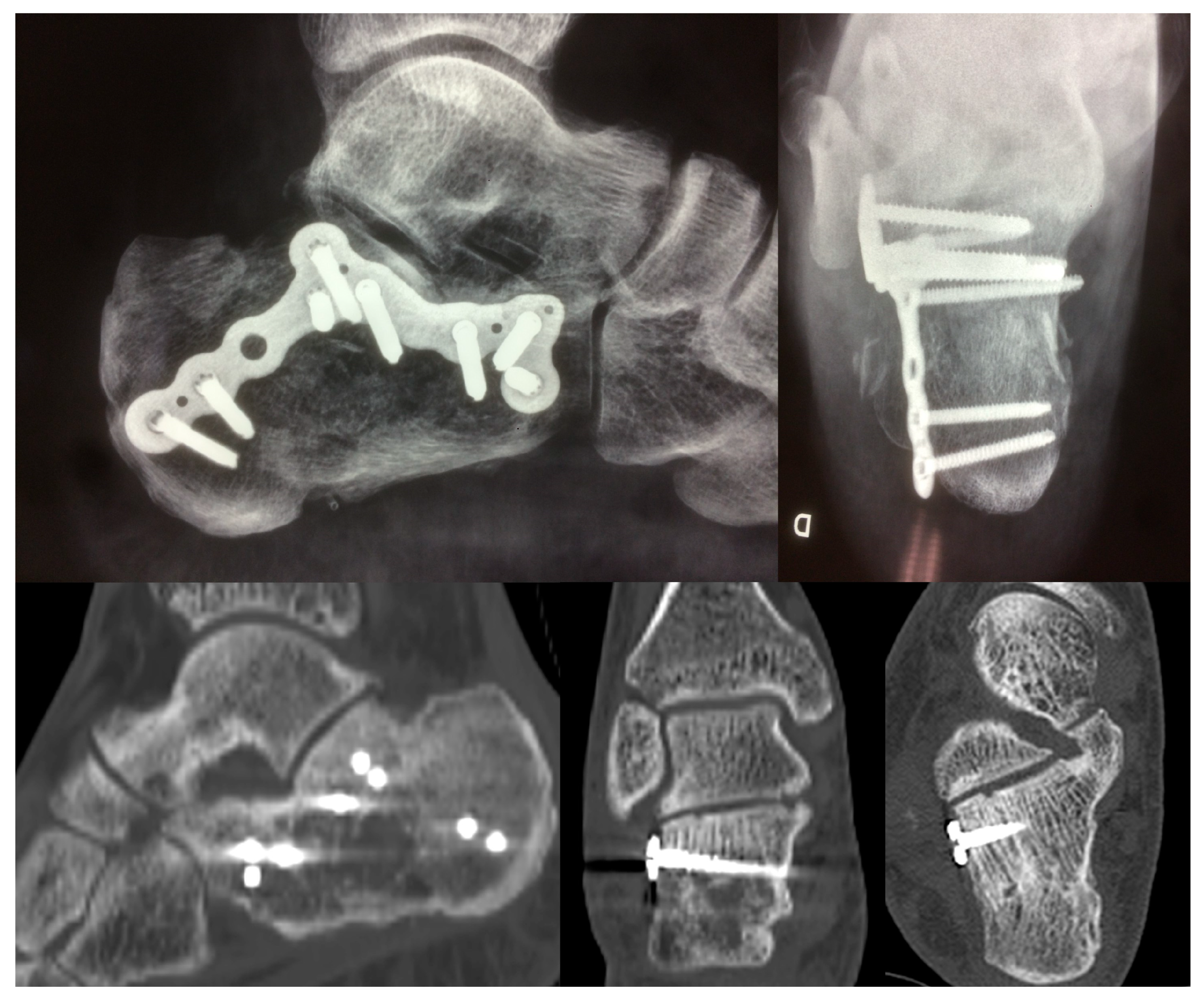
2.2. Surgical Procedure
2.3. Statistical Analysis
2.4. Sample Size
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ansari, E.; Ninama, D.; Panchal, H.; Damor, H. Calcaneum fractures: Overall operative outcomes. Paripex-Indian J. Res. 2020, 9, 39–41. [Google Scholar]
- Zwipp, H.; Rammelt, S.; Barthel, S. Fracture of the calcaneus. Der Unfallchirurg. 2005, 108, 737–747, quiz 48. [Google Scholar] [CrossRef]
- Potter, M.Q.; Nunley, J.A. Long-term functional outcomes after operative treatment for intra-articular fractures of the calcaneus. J. Bone Jt. Surg. 2009, 91, 1854–1860. [Google Scholar] [CrossRef] [PubMed]
- Volpin, G.; Cohen, Z.; Kirshner, G.; Shtarker, H. Displaced intra-articular calcaneal fractures: Current concepts and modern management. J. Foot Ankle Surg. 2014, 1, 24–31. [Google Scholar] [CrossRef]
- Buckley, R.; Tough, S.; McCormack, R. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures. Orthop. Trauma Dir. 2010, 8, 29–36. [Google Scholar] [CrossRef]
- Peng, C.; Yuan, B.; Guo, W.; Li, N.; Tian, H. Extensile lateral versus sinus tarsi approach for calcaneal fractures: A meta-analysis. Medicine 2021, 100, e26717. [Google Scholar] [CrossRef] [PubMed]
- Wallace, B.; Chhabra, A.; Narayanan, A.; O’Neill, D.; Xi, Y.; Van Pelt, M.; Wukich, D.K.; Liu, G.; Sanders, D.; Lalli, T.; et al. Low risk of wound complications with sinus tarsi approach for treatment of calcaneus fractures. J. Foot Ankle Surg. 2022, 61, 771–775. [Google Scholar] [CrossRef]
- Rammelt, S.; Amlang, M.; Barthel, S.; Gavlik, J.-M.; Zwipp, H. Percutaneous treatment of less severe intraarticular calcaneal fractures. Clin. Orthop. Relat. Res. 2010, 468, 983–990. [Google Scholar] [CrossRef]
- Cota, A.; Weber, T.G. Lateral Extensile Approach for ORIF. In Fractures and Dislocations of the Talus and Calcaneus; Springer: Cham, Switzerland, 2020; pp. 197–210. [Google Scholar]
- Schepers, T. The sinus tarsi approach in displaced intra-articular calcaneal fractures: A systematic review. Int. Orthop. 2011, 35, 697–703. [Google Scholar] [CrossRef]
- Poeze, M.; Verbruggen, J.P.; Brink, P.R. The relationship between the outcome of operatively treated calcaneal fractures and institutional fracture load: A systematic review of the literature. J. Bone Jt. Surg. 2008, 90, 1013–1021. [Google Scholar] [CrossRef]
- Cianni, L.; Vitiello, R.; Greco, T.; Sirgiovanni, M.; Ragonesi, G.; Maccauro, G.; Perisano, C. Predictive Factors of Poor Outcome in Sanders Type III and IV Calcaneal Fractures Treated with an Open Reduction and Internal Fixation with Plate: A Medium-Term Follow-Up. J. Clin. Med. 2022, 11, 5660. [Google Scholar] [CrossRef] [PubMed]
- Court-Brown, C.M.; Schmidt, M.; Schutte, B.G. Factors affecting infection after calcaneal fracture fixation. Injury 2009, 40, 1313–1315. [Google Scholar] [CrossRef] [PubMed]
- Gitajn, I.L.; Abousayed, M.; Toussaint, R.J.; Vrahas, M.; Kwon, J.Y. Calcaneal avulsion fractures: A case series of 33 patients describing prognostic factors and outcomes. Foot Ankle Spec. 2015, 8, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Sanders, R. Current concepts review-displaced intra-articular fractures of the calcaneus. J. Bone Jt. Surg. 2000, 82, 225–250. [Google Scholar] [CrossRef]
- Fulkerson, E.W.; Egol, K.A. Timing Issues in Fracture Management. Bull. NYU Hosp. Jt. Dis. 2009, 67, 58–67. [Google Scholar] [PubMed]
- Kline, A.J.; Anderson, R.B.; Davis, W.H.; Jones, C.P.; Cohen, B.E. Minimally invasive technique versus an extensile lateral approach for intra-articular calcaneal fractures. Foot Ankle Int. 2013, 34, 773–780. [Google Scholar] [CrossRef]
- Mangram, A.J.; Horan, T.C.; Pearson, M.L.; Silver, L.C.; Jarvis, W.R. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am. J. Infect. Control. 1999, 27, 97–132. [Google Scholar] [CrossRef]
- Janzen, D.L.; Connell, D.G.; Munk, P.L.; Buckley, R.E.; Meek, R.N.; Schechter, M.T. Intraarticular fractures of the calcaneus: Value of CT findings in determining prognosis. AJR Am. J. Roentgenol. 1992, 158, 1271–1274. [Google Scholar] [CrossRef]
- Holecek, T.; Dedek, T. Open versus closed method of operative treatment of calcaneal fractures. Eur. J. Trauma 2002, 28 (Suppl. S1), 84. [Google Scholar]
- O’Farrell, D.A.; O’Byrne, J.M.; McCabe, J.P.; Stephens, M.M. Fractures of the os calcis: Improved results with internal fixation. Injury 1993, 24, 263–265. [Google Scholar] [CrossRef] [PubMed]
- Kakwani, R.; Siddique, M. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: A prospective, randomized, controlled multicenter trial. In Classic Papers in Orthopaedics; Springer: London, UK, 2014; pp. 229–231. [Google Scholar]
- Biz, C.; Barison, E.; Ruggieri, P.; Iacobellis, C. Radiographic and functional outcomes after displaced intra-articular calcaneal fractures: A comparative cohort study among the traditional open technique (ORIF) and percutaneous surgical procedures (PS). J. Orthop. Surg. Res. 2016, 11, 92. [Google Scholar] [CrossRef] [PubMed]
- Polichetti, C.; Greco, T.; Inverso, M.; Maccauro, G.; Forconi, F.; Perisano, C. Retro-Malleolar Z-Plasty of Flexor Hallucis Longus Tendon in Post-Traumatic Checkrein Deformity: A Case Series and Literature Review. Medicina 2022, 58, 1072. [Google Scholar] [CrossRef] [PubMed]
- Dickenson, E.J.; Parsons, N.; Griffin, D.R. Open reduction and internal fixation versus nonoperative treatment for closed, displaced, intra-articular fractures of the calcaneus: Long-term follow-up from the HeFT randomized controlled trial. Bone Jt. J. 2021, 103–B, 1040–1046. [Google Scholar] [CrossRef]
- Buckley, R.; Tough, S.; McCormack, R.; Pate, G.; Leighton, R.; Petrie, D.; Galpin, R. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: A prospective randomized controlled multicenter trial. J. Bone Jt. Surg. Am. 2002, 84–A, 1733–1744. [Google Scholar] [CrossRef] [PubMed]
- Basile, A. Subjective results after surgical treatment for displaced intra-articular calcaneal fractures. J. Foot Ankle Surg. 2012, 51, 182–186. [Google Scholar] [CrossRef]
- Basile, A.; Albo, F.; Via, A.G. Comparison between sinus tarsi approach and extensile lateral approach for treatment of closed displaced intra-articular calcaneal fractures: A multicenter prospective study. J. Foot Ankle Surg. 2016, 55, 513–521. [Google Scholar] [CrossRef]
- Holmes, G.B., Jr. Treatment of displaced calcaneal fractures using a small sinus tarsi approach. Tech. Foot Ankle Surg. 2005, 4, 35–41. [Google Scholar] [CrossRef]
- Nosewicz, T.; Knupp, M.; Barg, A.; Maas, M.; Bolliger, L.; Goslings, J.C.; Hintermann, B. Mini-open sinus tarsi approach with percutaneous screw fixation of displaced calcaneal fractures: A prospective computed tomography–based study. Foot Ankle Int. 2012, 33, 925–933. [Google Scholar] [CrossRef]
- Kwon, J.Y.; Guss, D.; Lin, D.E.; Abousayed, M.; Jeng, C.; Kang, S.; Ellington, J.K. Effect tof delay to definitive surgical fixation on wound complications in the treatment of closed, intra-articular calcaneus fractures. Foot Ankle Int. 2015, 36, 508–517. [Google Scholar] [CrossRef]
- Li, S. Wound and sural nerve complications of the sinus tarsi approach for calcaneus fractures. Foot Ankle Int. 2018, 39, 1106–1112. [Google Scholar] [CrossRef]



| Sanders Type | Patterns of fracture | ||
|---|---|---|---|
| Type I | Not displaced or minimally displaced | ||
| Type II A | A—Lateral third | ||
| Type II | Two-part fracture | Type II B | B—Central third |
| Type II C | C—Medial Third | ||
| Type II AB | AB—Involvement of the lateral and central aspects of the posterior facet of the calcaneus | ||
| Type III | Three-part fracture | Type II BC | BC—Involvement of the central and medial aspects of the posterior facet of the calcaneus |
| Type II AC | AC—Involvement of the lateral and medial aspects of the posterior facet of the calcaneus. | ||
| Type IV | Four or more fragments |
| Patient Position | Lateral Decubitus |
| Intra-operatory aids | C-arm fluoroscopy |
| Anatomical markers | Tip of the lateral malleolus Base of the 4th metatarsal bone |
| Fragments exposure | Release of the inferior peroneal retinaculum Release of the CFL and subtalar ligaments SJ exposure |
| Steps for fragments reduction | Reduction of the PT fragment to the sustentacular constant fragment Reduction of articular fragments from posterior to anterior |
| Osteosynthesis | Temporary fixation with K-wires IF with plate and screws |
| Wound closure |
Gender
| |
Mean Age sample, years
| |
Body Mass Index
| p = 0.34 |
Sanders Classification
| |
| N = Number, SD = Standard Deviation |
| Wound Complications | |||
|---|---|---|---|
| Group A | N. 4 (34 fractures; 12%) | 3 superficial; 1 deep | p = 0.60 |
| Group B | N.2 (20 fractures; 10%) | 1 superficial; 1 deep | |
| Duration of surgery (Min) | |||
| Group A | 95.67 ± 22.93 | p < 0.001 | |
| Group B | 167.35 ± 30.93 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Basile, A.; Lanzetti, R.M.; Giai Via, A.; Venditto, T.; Spoliti, M.; Sessa, P.; Tortora, M.; Maffulli, N. Delayed Surgical Treatment of Displaced Intra-Articular Calcaneal Fractures in Major Trauma Is Safe and Effective. J. Clin. Med. 2023, 12, 2039. https://doi.org/10.3390/jcm12052039
Basile A, Lanzetti RM, Giai Via A, Venditto T, Spoliti M, Sessa P, Tortora M, Maffulli N. Delayed Surgical Treatment of Displaced Intra-Articular Calcaneal Fractures in Major Trauma Is Safe and Effective. Journal of Clinical Medicine. 2023; 12(5):2039. https://doi.org/10.3390/jcm12052039
Chicago/Turabian StyleBasile, Attilio, Riccardo Maria Lanzetti, Alessio Giai Via, Teresa Venditto, Marco Spoliti, Pasquale Sessa, Mauro Tortora, and Nicola Maffulli. 2023. "Delayed Surgical Treatment of Displaced Intra-Articular Calcaneal Fractures in Major Trauma Is Safe and Effective" Journal of Clinical Medicine 12, no. 5: 2039. https://doi.org/10.3390/jcm12052039
APA StyleBasile, A., Lanzetti, R. M., Giai Via, A., Venditto, T., Spoliti, M., Sessa, P., Tortora, M., & Maffulli, N. (2023). Delayed Surgical Treatment of Displaced Intra-Articular Calcaneal Fractures in Major Trauma Is Safe and Effective. Journal of Clinical Medicine, 12(5), 2039. https://doi.org/10.3390/jcm12052039







