Hip–Spine Syndrome: A Focus on the Pelvic Incidence in Hip Disorders
Abstract
1. Introduction
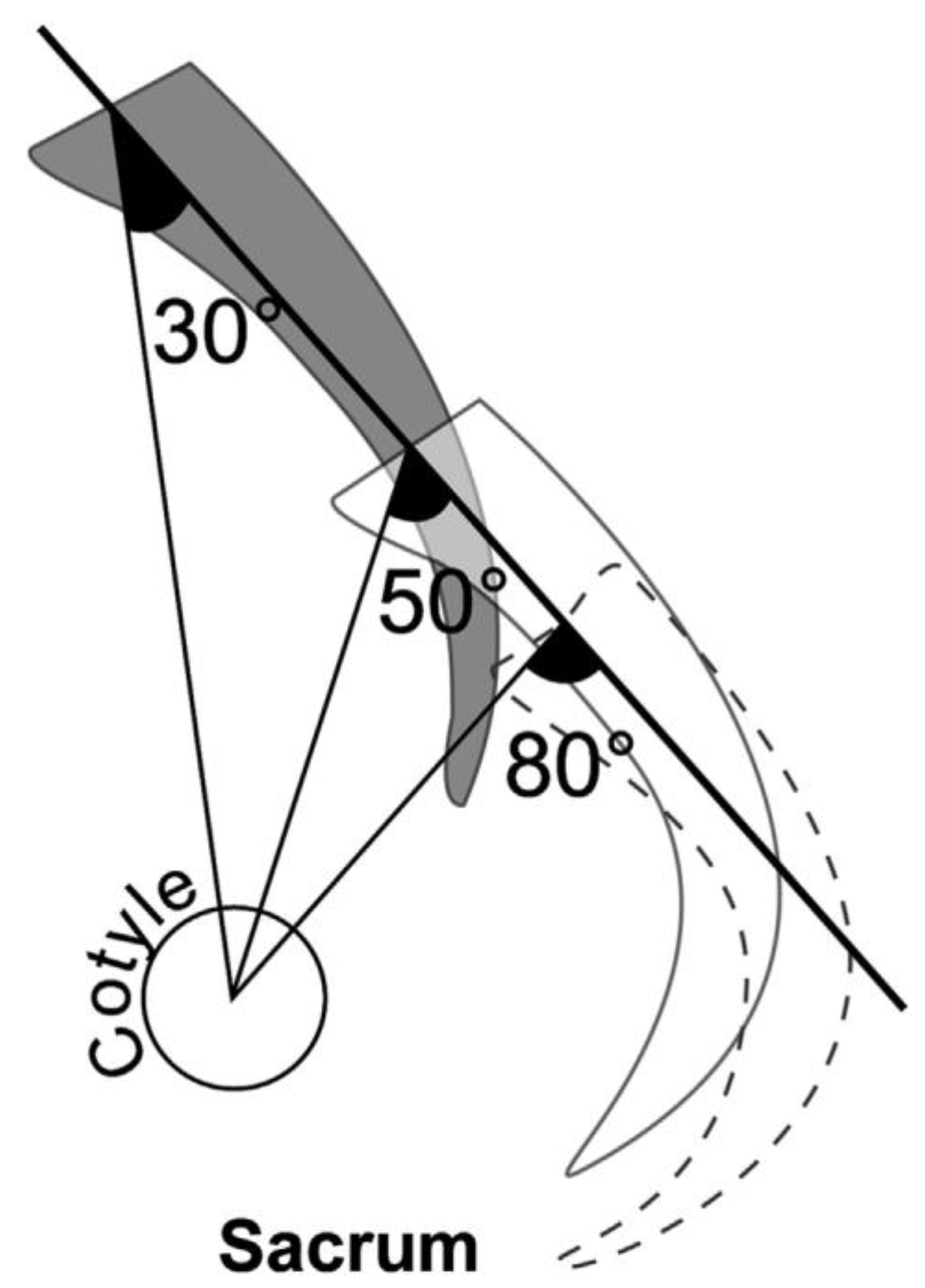
2. PI Changes in Phylogeny, Ontogeny, and Aging
3. Three Factors of the PI Increase
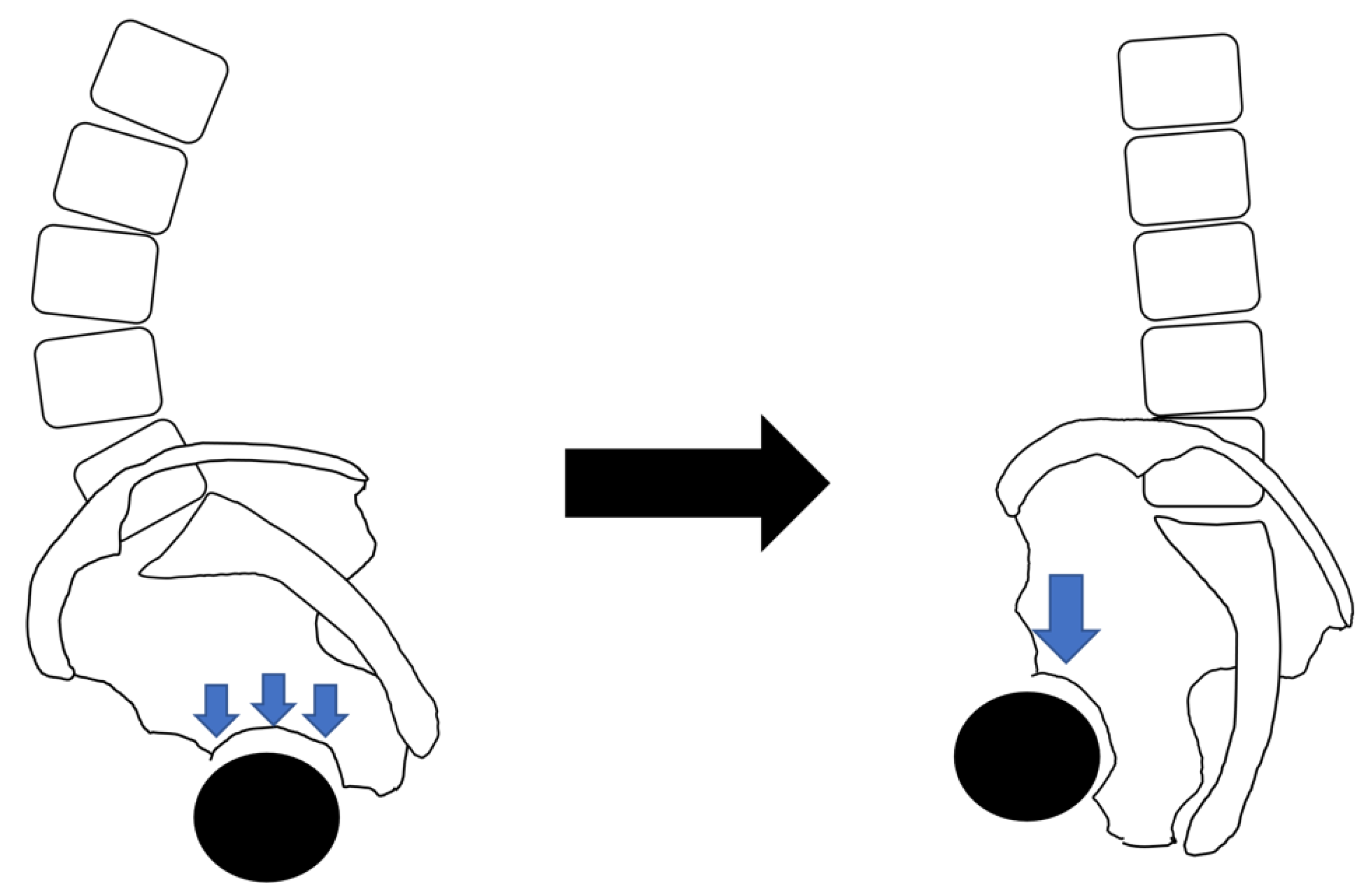
4. The Relationship between the PI, Lumbar Disorder, and Sacral Morphology
4.1. The Relationship between the PI and Lumbar Disorder
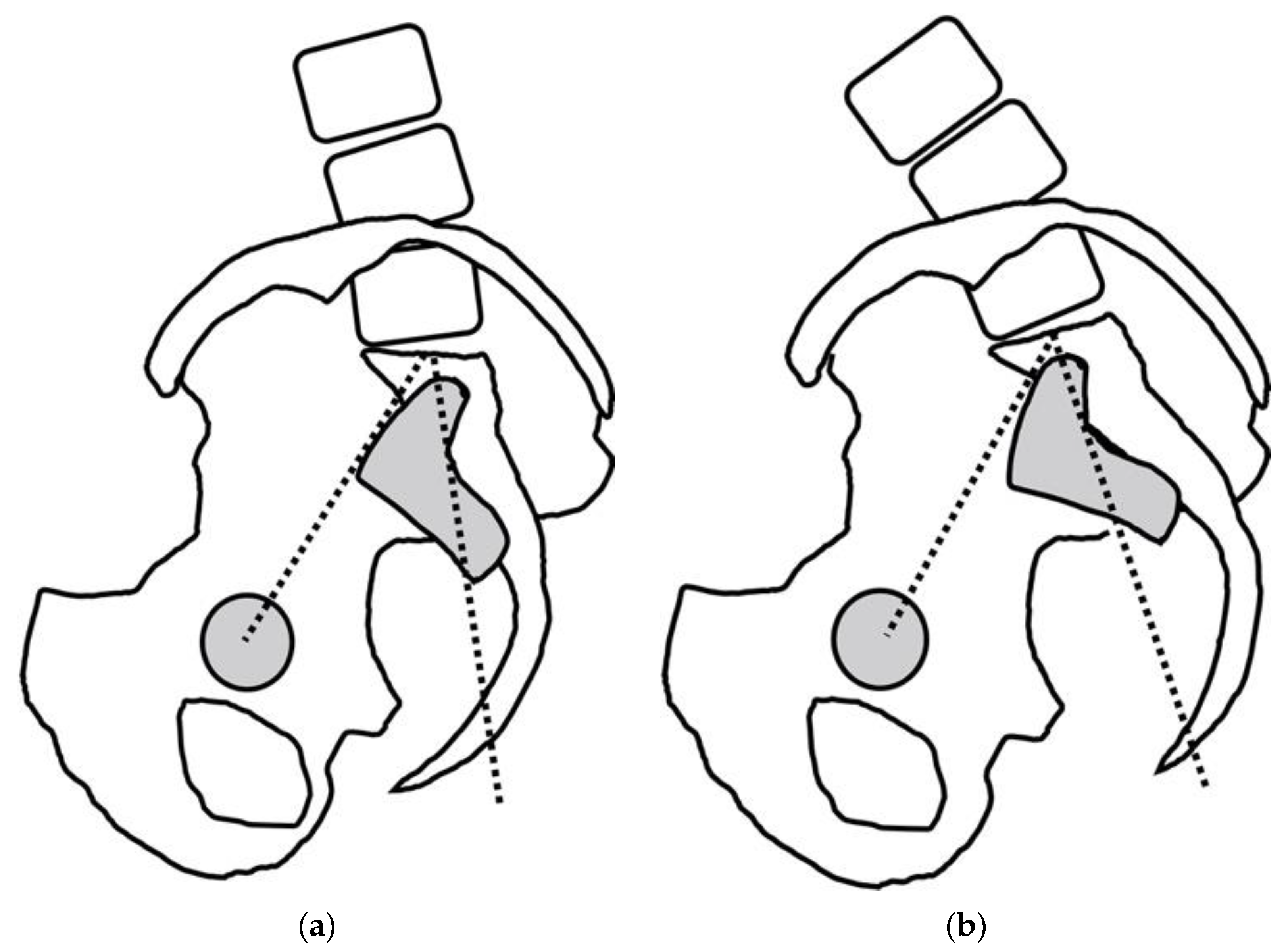
4.2. The Relationship between the PI and Sacral Morphology
5. PI–Hip Disorder Relationships
5.1. The Relationship between the PI and Hip Disorder
5.2. The Relationship between the PI and FAI
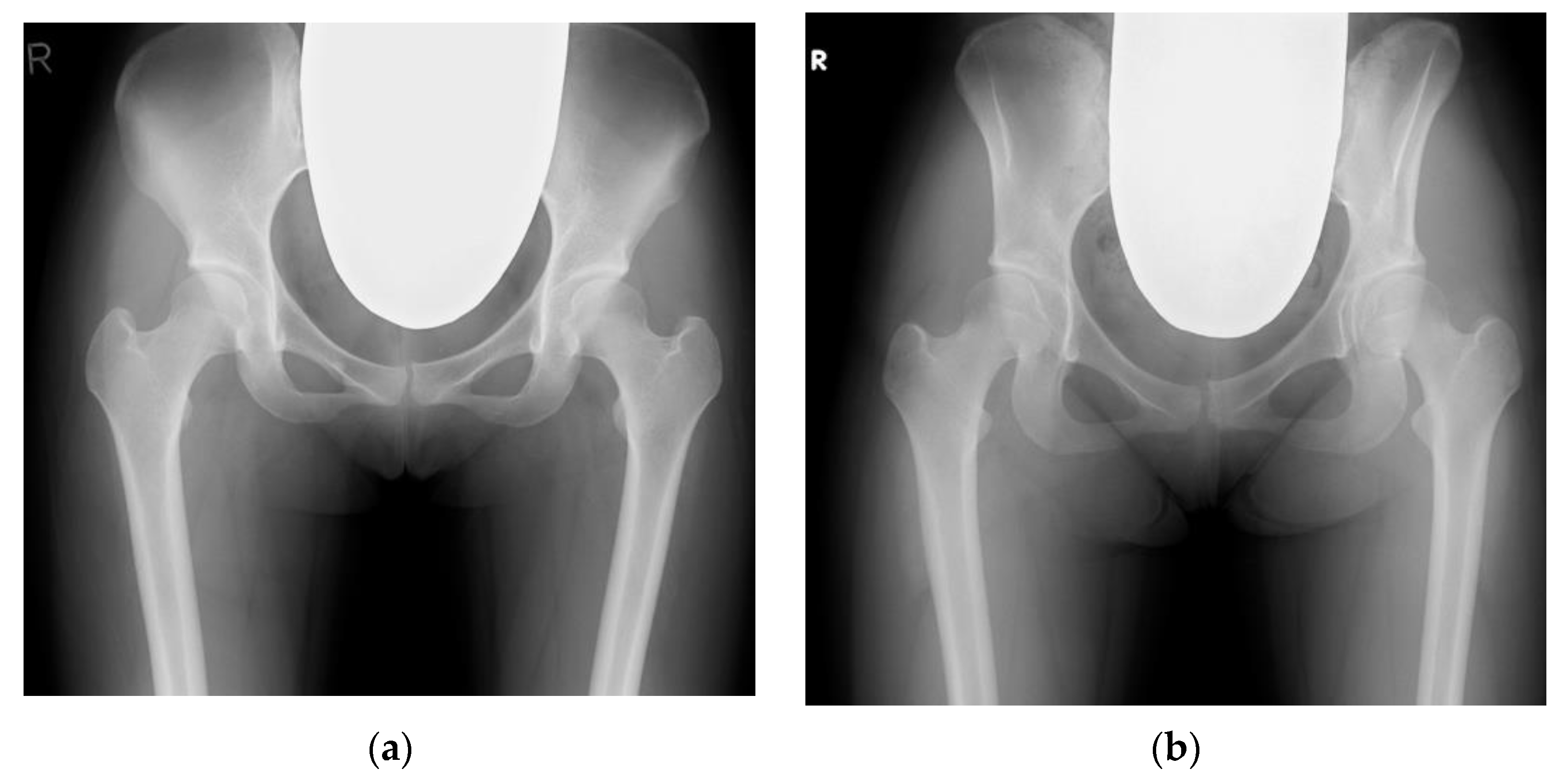
5.3. The Relationship between the PI and DDH
5.4. The Relationship between the PI and ONFH and RDC
5.5. What Is the Impact of HOA on the PI?
6. Limitations and Future Directions
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Offierski, C.M.; MacNab, I. Hip-spine syndrome. Spine 1983, 8, 316–321. [Google Scholar] [CrossRef]
- Rivière, C.; Lazennec, J.Y.; Van Der Straeten, C.; Auvinet, E.; Cobb, J.; Muirhead-Allwood, S. The influence of spine-hip relations on total hip replacement: A systematic review. Orthop. Traumatol. Surg. Res. 2017, 103, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Patel, A.; Ungar, B.; Farcy, J.P.; Lafage, V. Adult spinal deformity-postoperative standing imbalance: How much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine 2010, 35, 2224–2231. [Google Scholar] [CrossRef] [PubMed]
- Duval-Beaupère, G.; Schmidt, C.; Cosson, P. A Barycentremetric study of the sagittal shape of spine and pelvis: The conditions required for an economic standing position. Ann. Biomed. Eng. 1992, 20, 451–462. [Google Scholar] [CrossRef] [PubMed]
- Legaye, J.; Duval-Beaupere, G.; Barrau, A.; Boulay, C.; Hecquet, J.; Montigny, J.P.; Tardieu, C. Relationship between sacral pelvic incidence and acetabular orientation. Hip Int. 2011, 21, 87–97. [Google Scholar] [CrossRef]
- Mac-Thiong, J.M.; Roussouly, P.; Berthonnaud, E.; Guigui, P. Sagittal parameters of global spinal balance: Normative values from a prospective cohort of seven hundred nine Caucasian asymptomatic adults. Spine 2010, 35, E1193–E1198. [Google Scholar] [CrossRef]
- Mac-Thiong, J.M.; Roussouly, P.; Berthonnaud, E.; Guigui, P. Age- and sex-related variations in sagittal sacropelvic morphology and balance in asymptomatic adults. Eur. Spine J. 2011, 20 (Suppl. 5), 572–577. [Google Scholar] [CrossRef]
- Ramchandran, S. Pelvic incidence (PI) is more easily understood as the pelvic base angle (PBA). Spine Res. 2017, 3, 8. [Google Scholar] [CrossRef]
- Cho, K.J.; Suk, S.I.; Park, S.R.; Kim, J.H.; Kang, S.B.; Kim, H.S.; Oh, S.J. Risk factors of sagittal decompensation after long posterior instrumentation and fusion for degenerative lumbar scoliosis. Spine 2010, 35, 1595–1601. [Google Scholar] [CrossRef]
- Schlösser, T.P.C.; Janssen, M.M.A.; Vrtovec, T.; Pernuš, F.; Öner, F.C.; Viergever, M.A.; Vincken, K.L.; Castelein, R.M. Evolution of the ischio-iliac lordosis during natural growth and its relation with the pelvic incidence. Eur. Spine J. 2014, 23, 1433–1441. [Google Scholar] [CrossRef]
- Tardieu, C.; Bonneau, N.; Hecquet, J.; Boulay, C.; Marty, C.; Legaye, J.; Duval-Beaupère, G. How is sagittal balance acquired during bipedal gait acquisition? Comparison of neonatal and adult pelves in three dimensions. Evolutionary implications. J. Hum. Evol. 2013, 65, 209–222. [Google Scholar] [CrossRef]
- Saltychev, M.; Pernaa, K.; Seppänen, M.; Mäkelä, K.; Laimi, K. Pelvic incidence and hip disorders. Acta Orthop. 2018, 89, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Hayama, S.; Nakatsukasa, M.; Kunimatsu, Y. Monkey performance: The development of bipedalism in trained Japanese monkeys. Kaibogaku Zasshi. J. Anat. 1992, 67, 169–185. [Google Scholar]
- Moon, J.W.; Shinn, J.K.; Ryu, D.; Oh, S.Y.; Shim, Y.S.; Yoon, S.H. Pelvic incidence can be changed not only by age and sex, but also by posture used during imaging. Korean J. Spine 2017, 14, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Nagamoto, Y.; Iwasaki, M.; Sakaura, H.; Sugiura, T.; Fujimori, T.; Matsuo, Y.; Kashii, M.; Murase, T.; Yoshikawa, H.; Sugamoto, K. Sacroiliac joint motion in patients with degenerative lumbar spine disorders. J. Neurosurg. Spine 2015, 23, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Oba, H.; Ebata, S.; Takahashi, J.; Ikegami, S.; Koyama, K.; Haro, H.; Kato, H.; Ohba, T. Loss of pelvic incidence correction after long fusion using iliac screws for adult spinal deformity: Cause and effect on clinical outcome. Spine 2019, 44, 195–202. [Google Scholar] [CrossRef]
- Cecchinato, R.; Redaelli, A.; Martini, C.; Morselli, C.; Villafañe, J.H.; Lamartina, C.; Berjano, P. Long fusions to S1 with or without pelvic fixation can induce relevant acute variations in pelvic incidence: A retrospective cohort study of adult spine deformity surgery. Eur. Spine J. 2017, 26, 436–441. [Google Scholar] [CrossRef] [PubMed]
- Chang, D.G.; Ha, K.Y.; Kim, Y.H.; Lee, E.W. Spinopelvic alignment by different surgical methods in the treatment of degenerative sagittal imbalance of the lumbar spine. Clin. Spine Surg. 2017, 30, E390–E397. [Google Scholar] [CrossRef]
- Ebata, S.; Oba, H.; Ohba, T.; Takahashi, J.; Ikegami, S.; Koyama, K.; Kato, H.; Haro, H. Surgical outcomes of long fusion using dual iliac screws bilaterally for adult spinal deformities: The effect on the loosening rate and sacroiliac joint correction. Spine Surg. Relat. Res. 2019, 3, 236–243. [Google Scholar] [CrossRef]
- Lee, J.H.; Na, K.H.; Kim, J.H.; Jeong, H.Y.; Chang, D.G. Is pelvic incidence a constant, as everyone knows? Changes of pelvic incidence in surgically corrected adult sagittal deformity. Eur. Spine J. 2016, 25, 3707–3714. [Google Scholar] [CrossRef]
- Schroeder, N.; Noschenko, A.; Burger, E.; Patel, V.; Cain, C.; Ou-Yang, D.; Kleck, C. Pelvic incidence changes between flexion and extension. Spine Deform. 2018, 6, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, K.; Okamoto, M.; Hatsushikano, S.; Caseiro, G.; Watanabe, K. Difference in whole spinal alignment between supine and standing positions in patients with adult spinal deformity using a new comparison method with slot-scanning three-dimensional X-ray imager and computed tomography through digital reconstructed radiography. BMC Musculoskelet. Disord. 2018, 19, 437. [Google Scholar] [CrossRef]
- Sturesson, B.; Uden, A.; Vleeming, A. A radiostereometric analysis of movements of the sacroiliac joints during the standing hip flexion test. Spine 2000, 25, 364–368. [Google Scholar] [CrossRef]
- Ohya, J.; Kawamura, N.; Takasawa, E.; Onishi, Y.; Ohtomo, N.; Miyahara, J.; Hayakawa, C.; Kunogi, J. Pelvic incidence change on the operating table. Eur. Spine J. 2021, 30, 2473–2479. [Google Scholar] [CrossRef] [PubMed]
- Boulay, C.; Tardieu, C.; Hecquet, J.; Benaim, C.; Mitulescu, A.; Marty, C.; Prat-Pradal, D.; Legaye, J.; Duval-Beaupère, G.; Pélissier, J. Anatomical reliability of two fundamental radiological and clinical pelvic parameters: Incidence and thickness. Eur. J. Orthop. Surg. Traumatol. 2005, 15, 197–204. [Google Scholar] [CrossRef]
- Ino, M.; Fueki, K.; Toda, N.; Tanouchi, T.; Manabe, N.; Itoh, K.; Ono, M.; Shimizu, T. Change of pelvic incidence due to rotatory subluxation of sacroiliac joint in severe adult spinal deformity. J. Spine Res. 2018, 9, 1649–1651. [Google Scholar]
- Toy, J.O.; Tinley, J.C.; Eubanks, J.D.; Qureshi, S.A.; Ahn, N.U. Correlation of sacropelvic geometry with disc degeneration in spondylolytic cadaver specimens. Spine 2012, 37, E10–E15. [Google Scholar] [CrossRef]
- Vrtovec, T.; Janssen, M.M.; Likar, B.; Castelein, R.M.; Viergever, M.A.; Pernuš, F. A review of methods for evaluating the quantitative parameters of sagittal pelvic alignment. Spine J. 2012, 12, 433–446. [Google Scholar] [CrossRef]
- Roussouly, P.; Gollogly, S.; Berthonnaud, E.; Labelle, H.; Weidenbaum, M. Sagittal alignment of the spine and pelvis in the presence of L5-s1 isthmic lysis and low-grade spondylolisthesis. Spine 2006, 31, 2484–2490. [Google Scholar] [CrossRef]
- Oh, S.K.; Chung, S.S.; Lee, C.S. Correlation of pelvic parameters with isthmic spondylolisthesis. Asian Spine J. 2009, 3, 21–26. [Google Scholar] [CrossRef]
- Labelle, H.; Roussouly, P.; Berthonnaud, E.; Transfeldt, E.; O’Brien, M.; Chopin, D.; Hresko, T.; Dimnet, J. Spondylolisthesis, pelvic incidence, and spinopelvic balance: A correlation study. Spine 2004, 29, 2049–2054. [Google Scholar] [CrossRef] [PubMed]
- Mac-Thiong, J.M.; Labelle, H.; Charlebois, M.; Huot, M.P.; de Guise, J.A. Sagittal plane analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine 2003, 28, 1404–1409. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Cao, L.; Bian, C.; Wang, H.R.; Lin, H.; Li, X.L.; Jiang, Y.Q.; Dong, J. Degenerative spondylolisthesis in the fifth lumbar vertebra and radiographic parameters: A correlation analysis. Clin. Spine Surg. 2017, 30, E1233–E1238. [Google Scholar] [CrossRef] [PubMed]
- Schuller, S.; Charles, Y.P.; Steib, J.P. Sagittal spinopelvic alignment and body mass index in patients with degenerative spondylolisthesis. Eur. Spine J. 2011, 20, 713–719. [Google Scholar] [CrossRef] [PubMed]
- Sahin, M.S.; Ergün, A.; Aslan, A. The relationship between osteoarthritis of the lumbar facet joints and lumbosacropelvic morphology. Spine 2015, 40, E1058–E1062. [Google Scholar] [CrossRef]
- Strube, P.; Pumberger, M.; Sonnow, L.; Zippelius, T.; Nowack, D.; Zahn, R.K.; Putzier, M. Association between lumbar spinal degeneration and anatomic pelvic parameters. Clin. Spine Surg. 2018, 31, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Abola, M.V.; Teplensky, J.R.; Cooperman, D.R.; Bauer, J.M.; Liu, R.W. Pelvic incidence is associated with sacral curvature, sacroiliac joint angulation, and sacral Ala width. Spine 2018, 43, 1529–1535. [Google Scholar] [CrossRef]
- Blondel, B.; Parratte, S.; Tropiano, P.; Pauly, V.; Aubaniac, J.M.; Argenson, J.N. Pelvic tilt measurement before and after total hip arthroplasty. Orthop. Traumatol. Surg. Res. 2009, 95, 568–572. [Google Scholar] [CrossRef]
- Weng, W.J.; Wang, W.J.; Wu, M.D.; Xu, Z.H.; Xu, L.L.; Qiu, Y. Characteristics of sagittal spine–pelvis–leg alignment in patients with severe hip osteoarthritis. Eur. Spine J. 2015, 24, 1228–1236. [Google Scholar] [CrossRef]
- Bendaya, S.; Lazennec, J.Y.; Anglin, C.; Allena, R.; Sellam, N.; Thoumie, P.; Skalli, W. Healthy vs. osteoarthritic hips: A comparison of hip, pelvis and femoral parameters and relationships using the EOS® system. Clin. Biomech. 2015, 30, 195–204. [Google Scholar] [CrossRef]
- Eyvazov, K.; Eyvazov, B.; Basar, S.; Nasto, L.A.; Kanatli, U. Effects of total hip arthroplasty on spinal sagittal alignment and static balance: A prospective study on 28 patients. Eur. Spine J. 2016, 25, 3615–3621. [Google Scholar] [CrossRef]
- Raphael, I.J.; Rasouli, M.R.; Kepler, C.K.; Restrepo, S.; Albert, T.J.; Radcliff, K.E. Pelvic incidence in patients with hip osteoarthritis. Arch. Bone Jt. Surg. 2016, 4, 132–136. [Google Scholar] [PubMed]
- Buckland, A.J.; Ayres, E.W.; Shimmin, A.J.; Bare, J.V.; McMahon, S.J.; Vigdorchik, J.M. Prevalence of sagittal spinal deformity among patients undergoing total hip arthroplasty. J. Arthroplast. 2020, 35, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Czubak-Wrzosek, M.; Nitek, Z.; Sztwiertnia, P.; Czubak, J.; Grzelecki, D.; Kowalczewski, J.; Tyrakowski, M. Pelvic incidence and pelvic tilt can be calculated using either the femoral heads or acetabular domes in patients with hip osteoarthritis. Bone Jt. J. 2021, 103, 1345–1350. [Google Scholar] [CrossRef] [PubMed]
- Sculco, P.K.; Windsor, E.N.; Jerabek, S.A.; Mayman, D.J.; Elbuluk, A.; Buckland, A.J.; Vigdorchik, J.M. Preoperative spinopelvic hypermobility resolves following total hip arthroplasty. Bone Jt. J. 2021, 103, 1766–1773. [Google Scholar] [CrossRef]
- Innmann, M.M.; Merle, C.; Phan, P.; Beaulé, P.E.; Grammatopoulos, G. Differences in spinopelvic characteristics between hip osteoarthritis patients and controls. J. Arthroplast. 2021, 36, 2808–2816. [Google Scholar] [CrossRef]
- Yoshimoto, H.; Sato, S.; Masuda, T.; Kanno, T.; Shundo, M.; Hyakumachi, T.; Yanagibashi, Y. Spinopelvic alignment in patients with osteoarthrosis of the hip: A radiographic comparison to patients with low back pain. Spine 2005, 30, 1650–1657. [Google Scholar] [CrossRef]
- Ochi, H.; Baba, T.; Homma, Y.; Matsumoto, M.; Nojiri, H.; Kaneko, K. Importance of the spinopelvic factors on the pelvic inclination from standing to sitting before total hip arthroplasty. Eur. Spine J. 2016, 25, 3699–3706. [Google Scholar] [CrossRef]
- Morimoto, T.; Kitajima, M.; Tsukamoto, M.; Yoshihara, T.; Sonohata, M.; Mawatari, M. Sagittal spino-pelvic alignment in rapidly destructive coxarthrosis. Eur. Spine J. 2018, 27, 475–481. [Google Scholar] [CrossRef]
- Hagiwara, S.; Orita, S.; Nakamura, J.; Inage, K.; Kawasaki, Y.; Shiko, Y.; Eguchi, Y.; Ohtori, S. Impact of spinal alignment and stiffness on impingement after total hip arthroplasty: A radiographic study of pre- and post-operative spinopelvic alignment. Eur. Spine J. 2021, 30, 2443–2449. [Google Scholar] [CrossRef]
- Iwasa, M.; Ando, W.; Uemura, K.; Hamada, H.; Takao, M.; Sugano, N. Pelvic incidence is not associated with the development of hip osteoarthritis. Bone Jt. J. 2021, 103, 1656–1661. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Morimoto, T.; Yoshihara, T.; Sonohata, M.; Rivière, C.; Mawatari, M. The significant relationship among the factors of pelvic incidence, standing lumbar lordosis, and lumbar flexibility in Japanese patients with hip osteoarthritis: A descriptive radiographic study. Orthop. Traumatol. Surg Res. 2022, 108, 103123. [Google Scholar] [CrossRef]
- Okuzu, Y.; Miyahara, T.; Goto, K.; Kuroda, Y.; Kawai, T.; Matsuda, S. Investigating sagittal spinal alignment, low back pain, and clinical outcomes after total hip arthroplasty for lumbar hyperlordosis: A retrospective study. Arch. Orthop. Trauma. Surg. 2022, 142, 4007–4013. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, Y.; Wakama, H.; Okayoshi, T.; Matsuyama, J.; Otsuki, S.; Neo, M. Spinopelvic mismatch is associated with patient-reported outcome measures after total knee arthroplasty at a mean follow-up of 15 years. Knee 2022, 34, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Onishi, E.; Ota, S.; Fujita, S.; Tsukamoto, Y.; Yamashita, S.; Hashimura, T.; Matsunaga, K.; Yasuda, T. Association between sagittal spinopelvic alignment and femoral head destruction in the early stage of rapidly destructive coxopathy. Bone Jt. Open 2022, 3, 77–84. [Google Scholar] [CrossRef]
- Jingushi, S.; Ohfuji, S.; Sofue, M.; Hirota, Y.; Itoman, M.; Matsumoto, T.; Hamada, Y.; Shindo, H.; Takatori, Y.; Yamada, H.; et al. Multiinstitutional epidemiological study regarding osteoarthritis of the hip in Japan. J. Orthop. Sci. 2010, 15, 626–631. [Google Scholar] [CrossRef]
- Vaz, G.; Roussouly, P.; Berthonnaud, E.; Dimnet, J. Sagittal morphology and equilibrium of pelvis and spine. Eur. Spine J. 2002, 11, 80–87. [Google Scholar] [CrossRef]
- Gebhart, J.J.; Weinberg, D.S.; Bohl, M.S.; Liu, R.W. Relationship between pelvic incidence and osteoarthritis of the hip. Bone Jt. Res. 2016, 5, 66–72. [Google Scholar] [CrossRef]
- Dandachli, W.; Ul Islam, S.; Richards, R.; Hall-Craggs, M.; Witt, J. The influence of pelvic tilt on acetabular orientation and cover: A three-dimensional computerised tomography analysis. Hip Int. 2013, 23, 87–92. [Google Scholar] [CrossRef]
- Hellman, M.D.; Haughom, B.D.; Brown, N.M.; Fillingham, Y.A.; Philippon, M.J.; Nho, S.J. Femoroacetabular impingement and pelvic incidence: Radiographic comparison to an asymptomatic control. Arthroscopy 2017, 33, 545–550. [Google Scholar] [CrossRef]
- Chen, H.F.; Zhao, C.Q. Pelvic incidence variation among individuals: Functional influence versus genetic determinism. J. Orthop. Surg. Res. 2018, 13, 59. [Google Scholar] [CrossRef]
- Vaswani, R.; White, A.E.; Feingold, J.; Ranawat, A.S. Hip-spine syndrome in the nonarthritic patient. Arthroscopy 2022, 38, 2930–2938. [Google Scholar] [CrossRef]
- Boughton, O.R.; Uemura, K.; Tamura, K.; Takao, M.; Hamada, H.; Cobb, J.P.; Sugano, N. Gender and disease severity determine proximal femoral morphology in developmental dysplasia of the hip. J. Orthop. Res. 2019, 37, 1123–1132. [Google Scholar] [CrossRef] [PubMed]
- Imai, N.; Miyasaka, D.; Tsuchiya, K.; Suzuki, H.; Ito, T.; Minato, I.; Endo, N. Evaluation of pelvic morphology in female patients with developmental dysplasia of the hip using three-dimensional computed tomography: A cross-sectional study. J. Orthop. Sci. 2018, 23, 788–792. [Google Scholar] [CrossRef] [PubMed]
- Cheng, R.; Huang, M.; Kernkamp, W.A.; Li, H.; Zhu, Z.; Wang, L.; Tsai, T.-Y. The severity of developmental dysplasia of the hip does not correlate with the abnormality in pelvic incidence. BMC Musculoskelet. Disord. 2020, 21, 623. [Google Scholar] [CrossRef]
- Sako, N.; Kaku, N.; Tagomori, H.; Tsumura, H. Is the iliac wing curved inward in patients with developmental dysplasia of the hip? Clin. Orthop. Surg. 2021, 13, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.M.; Yang, I.H.; Park, K.K.; Cho, B.W.; Kam, J.H.; Kong, Y.; Yang, J.H.; Lee, W.S. High pelvic incidence is associated with disease progression in nontraumatic osteonecrosis of the femoral head. Clin. Orthop. Relat. Res. 2020, 478, 1870–1876. [Google Scholar] [CrossRef] [PubMed]
- Mont, M.A. CORR Insights®: High pelvic incidence is associated with disease progression in nontraumatic osteonecrosis of the femoral head. Clin. Orthop. Relat. Res. 2020, 478, 1877–1879. [Google Scholar] [CrossRef] [PubMed]
- Okuzu, Y.; Goto, K.; Shimizu, Y.; Kawai, T.; Kuroda, Y.; Matsuda, S. Sacroiliac joint degeneration is common in patients with end-stage hip osteoarthritis secondary to unilateral developmental dysplasia of the hip: Factors associated with its severity and laterality. J. Orthop. Sci. 2021, 26, 135–140. [Google Scholar] [CrossRef] [PubMed]
| Reference | Nationality | Inclusion | Number | Age; Mean ± SD (Range) | Sex; Men, Women | PI; Mean ± SD | PI; Range |
|---|---|---|---|---|---|---|---|
| [38] | France | HOA | 50 | 64 (47–81) | 26, 24 | 56.04 | 40–87 |
| [39] | China | HOA | 58 | 59.0 ± 11.9 | N/A | 49.0 ± 10.8 | N/A |
| [40] | France | HOA | 30 | 59.5 ± 15.6 (25–81) | 12, 18 | 56.3 ± 11.5 | 35.1–81.4 |
| [41] | Turkey | HOA | 28 | 60.9 ± 7.3 (50–76) | 11, 17 | 50 | (35, 60) # |
| [42] | Iran | HOA | 95 | 68 (43–93) | 50, 45 | 56.0 ± 12.8 | 33–96 |
| [43] | USA | HOA | 1088 | 64.1 ± 10.4 | 557, 531 | 56.0 ± 11.5 | N/A |
| [44] | Poland | HOA | 50 | N/A | N/A | 50.9 | 19.7–78.4 |
| [45] | USA | HOA | 136 | 56.8 ± 10.8 (16–86) | 77, 59 | 60.6 ± 12.0 | N/A |
| [46] | Canada | HOA | 52 | 63 ± 11 (38–82) | 20, 32 | 57 ± 12 | 31–89 |
| [47] | Japan | HOA | 4 | 61.0 ± 11.1 | 30, 120 | 58.5 ± 14.0 | 29–90 |
| DDH | 146 | ||||||
| [48] | Japan | HOA | 64 | 65.5 ± 13.4 (27–86) | 14, 60 | 54.7 ± 13.6 | 18–92 |
| ONFH | 13 | ||||||
| [49] | Japan | HOA | 70 | 75 ± 4 | 0, 70 | 55 ± 14 | N/A |
| RDC | 44 | 79 ± 5 | 0, 44 | 58 ± 16 | |||
| [50] | Japan | HOA | 77 | 62.2 ± 12.8 (21–84) | 73 | 48.3 ± 15.8 | 18–70 |
| [51] | Japan | DDH | 100 | 65.5 ± 10.3 | 14, 86 | 53.7 ± 10.0 | N/A |
| HOA | 100 | 61.0 ± 9.3 | 9, 91 | 52.3 ± 10.4 | |||
| [52] | Japan | HOA | 945 | 64.4 ± 9.9 (34–89) | 141, 804 | 53.3 ± 11.0 | 27–84 |
| [53] | Japan | DDH | 78 | 53.6 ± 12.9 | 21, 102 | 48.0 ± 8.9 | N/A |
| HOA | 8 | ||||||
| ONFH | 10 | ||||||
| Others (RDC, trauma) | 6 | ||||||
| [54] | Japan | DDH | 213 | 74.5 ± 7.0 | 30, 243 | 57.0 ± 13.9 | N/A |
| HOA | 60 | ||||||
| [55] | Japan | HOA | 25 | 71.9 ± 6.4 | 4, 21 | 45.8 ± 10.0 | 41.6–49.9 |
| RDC | 34 | 74.6 ± 8.1 | 1, 33 | 49.6 ± 11.6 | 45.6–53.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morimoto, T.; Kobayashi, T.; Tsukamoto, M.; Hirata, H.; Yoshihara, T.; Toda, Y.; Mawatari, M. Hip–Spine Syndrome: A Focus on the Pelvic Incidence in Hip Disorders. J. Clin. Med. 2023, 12, 2034. https://doi.org/10.3390/jcm12052034
Morimoto T, Kobayashi T, Tsukamoto M, Hirata H, Yoshihara T, Toda Y, Mawatari M. Hip–Spine Syndrome: A Focus on the Pelvic Incidence in Hip Disorders. Journal of Clinical Medicine. 2023; 12(5):2034. https://doi.org/10.3390/jcm12052034
Chicago/Turabian StyleMorimoto, Tadatsugu, Takaomi Kobayashi, Masatsugu Tsukamoto, Hirohito Hirata, Tomohito Yoshihara, Yu Toda, and Masaaki Mawatari. 2023. "Hip–Spine Syndrome: A Focus on the Pelvic Incidence in Hip Disorders" Journal of Clinical Medicine 12, no. 5: 2034. https://doi.org/10.3390/jcm12052034
APA StyleMorimoto, T., Kobayashi, T., Tsukamoto, M., Hirata, H., Yoshihara, T., Toda, Y., & Mawatari, M. (2023). Hip–Spine Syndrome: A Focus on the Pelvic Incidence in Hip Disorders. Journal of Clinical Medicine, 12(5), 2034. https://doi.org/10.3390/jcm12052034






