Angiographic Outcomes for Arterial and Venous Conduits Used in CABG
Abstract
1. Introduction
2. Saphenous Vein
2.1. The Impact of the Harvesting Technique
2.2. The Impact of Pharmacotherapy
2.3. The Impact of External Stenting
2.4. The Impact of the Anastomotic Technique
3. Internal Thoracic Artery
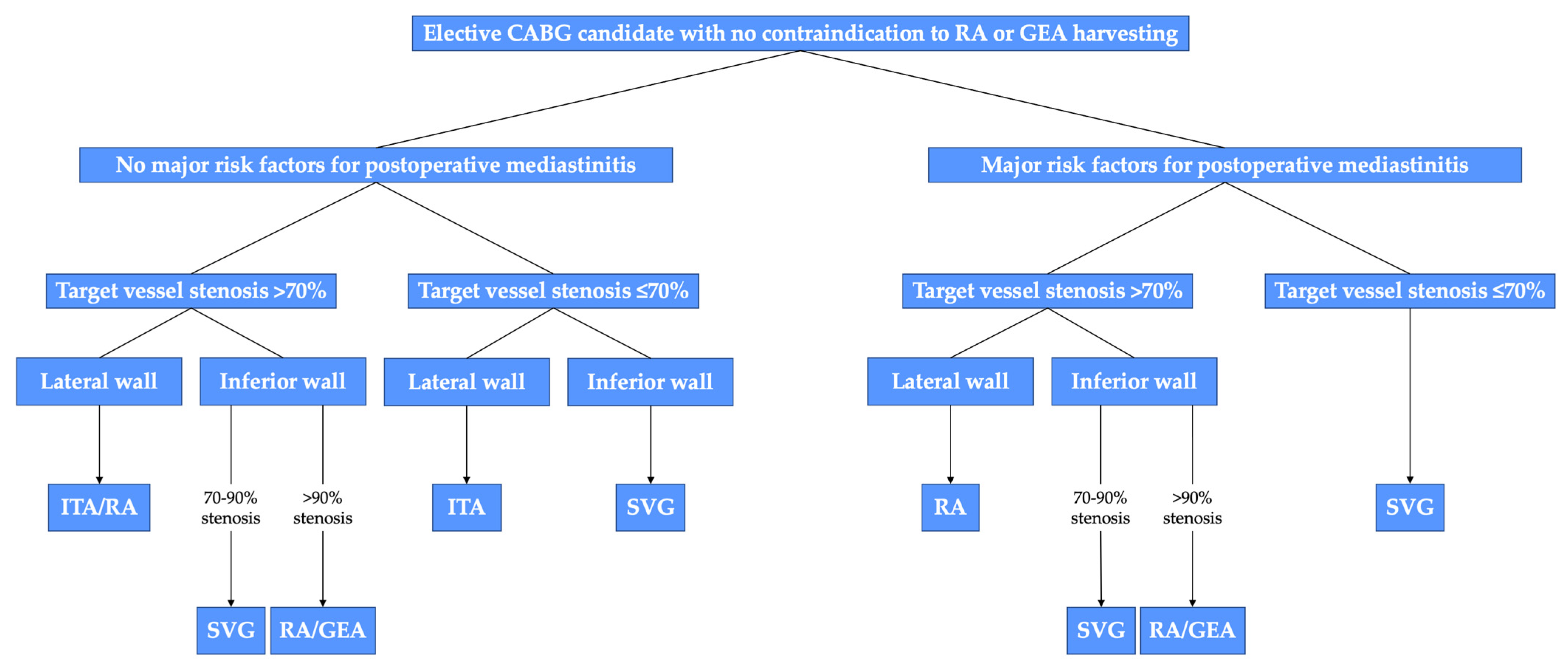
3.1. The Impact of the Harvesting Technique
3.2. The Impact of Graft Configuration and Target Coronary Vessel
3.3. The Impact of the Anastomotic Technique
4. Radial Artery
4.1. The Impact of Target Coronary Artery and Competitive Flow
4.2. The Impact of Sequential Grafting
4.3. The Impact of Graft Configuration
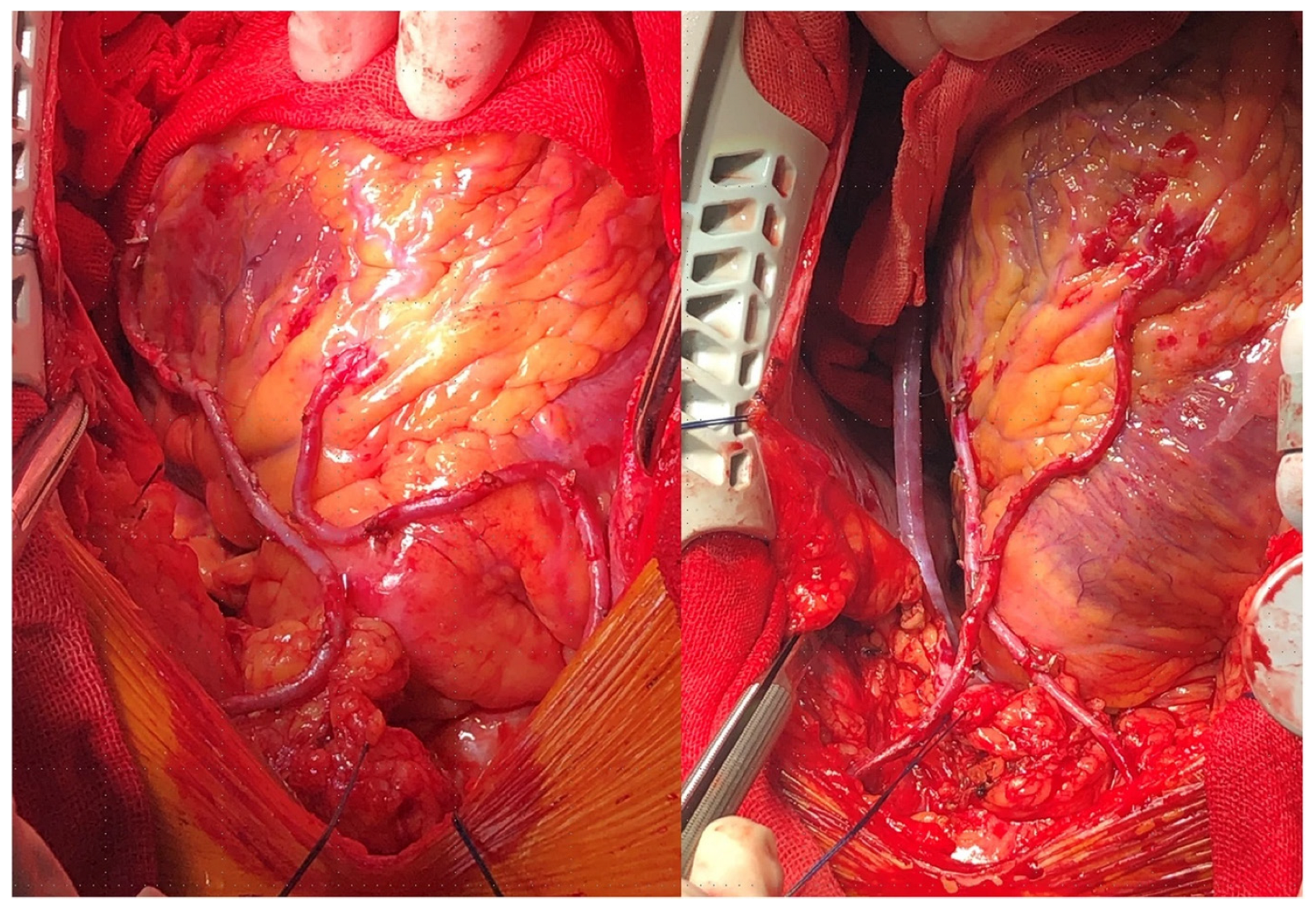
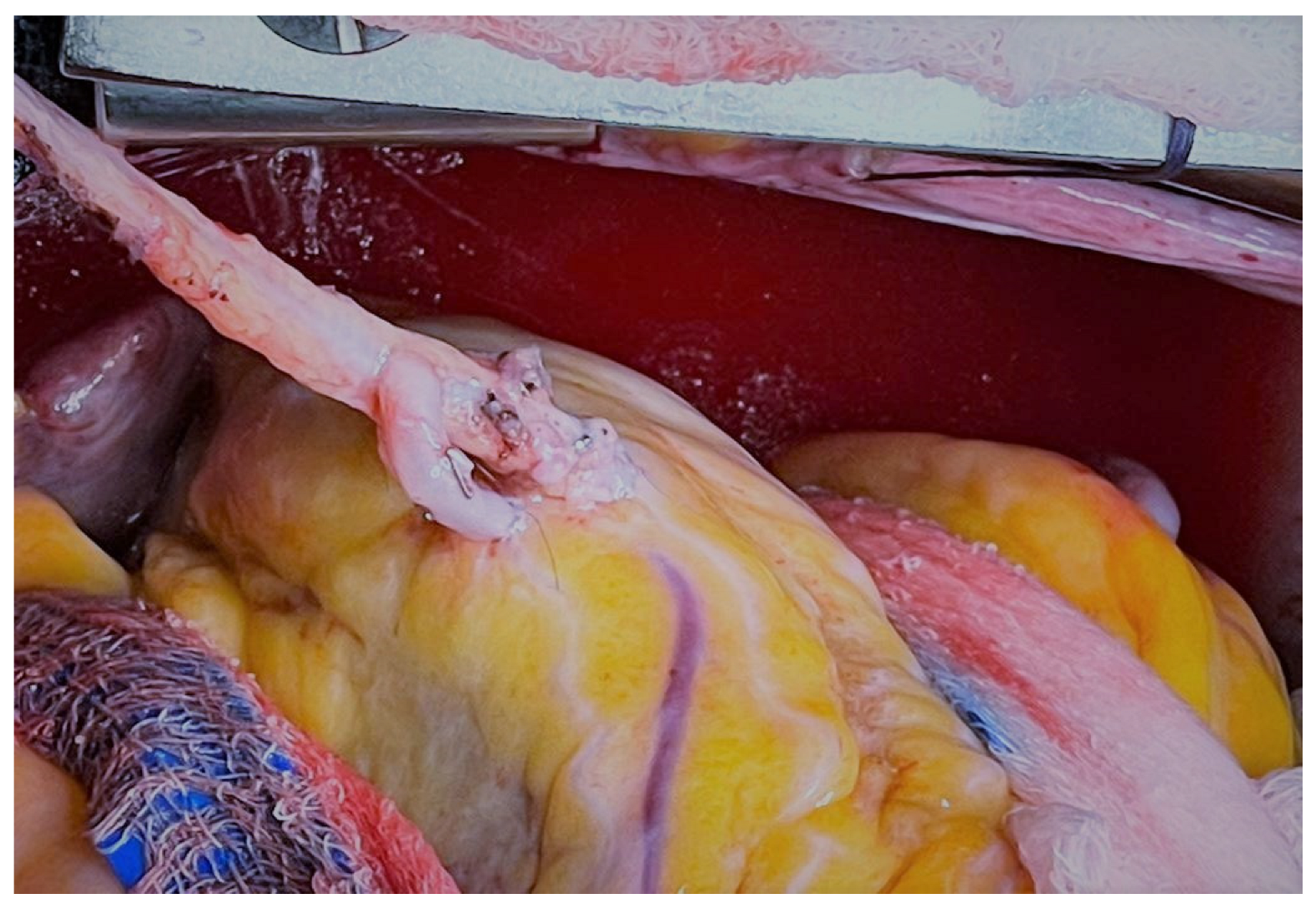
5. Gastroepiploic Artery
6. Comparisons of Conduit Patency
7. Surgical Revascularization Technique and Graft Patency
7.1. On- and Off-Pump CABG
7.2. Minimally Invasive and Robotic CABG
8. Angiographic and Clinical Outcomes
9. Tailoring Surgical Revascularization to Patients
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lawton, J.S.; Tamis-Holland, J.E.; Bangalore, S.; Bates, E.R.; Beckie, T.M.; Bischoff, J.M.; Bittl, J.A.; Cohen, M.G.; DiMaio, J.M.; Don, C.W.; et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022, 145, e18–e114. [Google Scholar] [CrossRef] [PubMed]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef]
- Gharibeh, L.; Ferrari, G.; Ouimet, M.; Grau, J.B. Conduits’ Biology Regulates the Outcomes of Coronary Artery Bypass Grafting. JACC Basic Transl. Sci. 2021, 6, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Schwann, T.A.; Habib, R.H.; Wallace, A.; Shahian, D.M.; O’Brien, S.; Jacobs, J.P.; Puskas, J.D.; Kurlansky, P.A.; Engoren, M.C.; Tranbaugh, R.F.; et al. Operative Outcomes of Multiple-Arterial Versus Single-Arterial Coronary Bypass Grafting. Ann. Thorac. Surg. 2018, 105, 1109–1119. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.; Dimagli, A.; Dong, T.; Fudulu, D.P.; Sinha, S.; Angelini, G.D. Trend and factors associated with multiple arterial revascularisation in coronary artery bypass grafting in the United Kingdom. Eur. J. Cardio-Thorac. Surg. 2022, 62, ezac284. [Google Scholar] [CrossRef]
- Schwann, T.A.; Tatoulis, J.; Puskas, J.; Bonnell, M.; Taggart, D.; Kurlansky, P.; Jacobs, J.P.; Thourani, V.H.; O’Brien, S.; Wallace, A.; et al. Worldwide Trends in Multi-arterial Coronary Artery Bypass Grafting Surgery 2004-2014: A Tale of 2 Continents. Semin. Thorac. Cardiovasc. Surg. 2017, 29, 273–280. [Google Scholar] [CrossRef]
- Favaloro, R.G. Saphenous vein autograft replacement of severe segmental coronary artery occlusion: Operative technique. Ann. Thorac. Surg. 1968, 5, 334–339. [Google Scholar] [CrossRef]
- Sabik, J.F. Understanding Saphenous Vein Graft Patency. Circulation 2011, 124, 273–275. [Google Scholar] [CrossRef]
- Bourassa, M.G.; Fisher, L.D.; Campeau, L.; Gillespie, M.J.; McConney, M.; Lespérance, J. Long-term fate of bypass grafts: The Coronary Artery Surgery Study (CASS) and Montreal Heart Institute experiences. Circulation 1985, 72, V71–V78. [Google Scholar]
- Alexander, J.H.; Hafley, G.; Harrington, R.A.; Peterson, E.D.; Ferguson, T.B.J.; Lorenz, T.J.; Goyal, A.; Gibson, M.; Mack, M.J.; Gennevois, D.; et al. Efficacy and safety of edifoligide, an E2F transcription factor decoy, for prevention of vein graft failure following coronary artery bypass graft surgery: PREVENT IV: A randomized controlled trial. JAMA 2005, 294, 2446–2454. [Google Scholar]
- Fitzgibbon, G.M.; Kafka, H.P.; Leach, A.J.; Keon, W.J.; Hooper, G.D.; Burton, J.R. Coronary bypass graft fate and patient outcome: Angiographic follow-up of 5065 grafts related to survival and reoperation in 1388 patients during 25 years. J. Am. Coll. Cardiol. 1996, 28, 616–626. [Google Scholar] [CrossRef]
- Souza, D. A new no-touch preparation technique. Technical notes. Scand. J. Thorac. Cardiovasc. Surg. 1996, 30, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Dreifaldt, M.; Souza, D.S.R.; Loesch, A.; Muddle, J.R.; Karlsson, M.G.; Filbey, D.; Bodin, L.; Norgren, L.; Dashwood, M.R. The “no-touch” harvesting technique for vein grafts in coronary artery bypass surgery preserves an intact vasa vasorum. J. Thorac. Cardiovasc. Surg. 2011, 141, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Dashwood, M.R.; Savage, K.; Tsui, J.C.S.; Dooley, A.; Shaw, S.G.; Fernández Alfonso, M.S.; Bodin, L.; Souza, D.S.R. Retaining perivascular tissue of human saphenous vein grafts protects against surgical and distension-induced damage and preserves endothelial nitric oxide synthase and nitric oxide synthase activity. J. Thorac. Cardiovasc. Surg. 2009, 138, 334–340. [Google Scholar] [CrossRef]
- Souza, D.S.R.; Dashwood, M.R.; Tsui, J.C.S.; Filbey, D.; Bodin, L.; Johansson, B.; Borowiec, J. Improved patency in vein grafts harvested with surrounding tissue: Results of a randomized study using three harvesting techniques. Ann. Thorac. Surg. 2002, 73, 1189–1195. [Google Scholar] [CrossRef] [PubMed]
- Souza, D.S.R.; Johansson, B.; Bojö, L.; Karlsson, R.; Geijer, H.; Filbey, D.; Bodin, L.; Arbeus, M.; Dashwood, M.R. Harvesting the saphenous vein with surrounding tissue for CABG provides long-term graft patency comparable to the left internal thoracic artery: Results of a randomized longitudinal trial. J. Thorac. Cardiovasc. Surg. 2006, 132, 373–378. [Google Scholar] [CrossRef]
- Samano, N.; Geijer, H.; Liden, M.; Fremes, S.; Bodin, L.; Souza, D. The no-touch saphenous vein for coronary artery bypass grafting maintains a patency, after 16 years, comparable to the left internal thoracic artery: A randomized trial. J. Thorac. Cardiovasc. Surg. 2015, 150, 880–888. [Google Scholar] [CrossRef] [PubMed]
- Pettersen, Ø.; Wiseth, R.; Hegbom, K.; Nordhaug, D.O. Pedicled Vein Grafts in Coronary Surgery Exhibit Reduced Intimal Hyperplasia at 6 Months. J. Am. Coll. Cardiol. 2016, 68, 427–429. [Google Scholar] [CrossRef] [PubMed]
- Deb, S.; Singh, S.K.; de Souza, D.; Chu, M.W.A.; Whitlock, R.; Meyer, S.R.; Verma, S.; Jeppsson, A.; Al-Saleh, A.; Brady, K.; et al. SUPERIOR SVG: No touch saphenous harvesting to improve patency following coronary bypass grafting (a multi-Centre randomized control trial, NCT01047449). J. Cardiothorac. Surg. 2019, 14, 85. [Google Scholar] [CrossRef]
- Tian, M.; Wang, X.; Sun, H.; Feng, W.; Song, Y.; Lu, F.; Wang, L.; Wang, Y.; Xu, B.; Wang, H.; et al. No-Touch Versus Conventional Vein Harvesting Techniques at 12 Months After Coronary Artery Bypass Grafting Surgery: Multicenter Randomized, Controlled Trial. Circulation 2021, 144, 1120–1129. [Google Scholar] [CrossRef]
- Ragnarsson, S.; Janiec, M.; Modrau, I.S.; Dreifaldt, M.; Ericsson, A.; Holmgren, A.; Hultkvist, H.; Jeppsson, A.; Sartipy, U.; Ternström, L.; et al. No-touch saphenous vein grafts in coronary artery surgery (SWEDEGRAFT): Rationale and design of a multicenter, prospective, registry-based randomized clinical trial. Am. Heart J. 2020, 224, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Zhang, Y.; Wu, Z.; Liu, Z.; Zheng, J. Mid-term and long-term outcomes of endoscopic versus open vein harvesting for coronary artery bypass: A systematic review and meta-analysis. Int. J. Surg. 2019, 72, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Chakos, A.; Jbara, D.; Singh, K.; Yan, T.D.; Tian, D.H. Network meta-analysis of antiplatelet therapy following coronary artery bypass grafting (CABG): None versus one versus two antiplatelet agents. Ann. Cardiothorac. Surg. 2018, 7, 577–585. [Google Scholar] [CrossRef] [PubMed]
- Saw, J.; Wong, G.C.; Mayo, J.; Bernstein, V.; Mancini, G.B.J.; Ye, J.; Skarsgard, P.; Starovoytov, A.; Cairns, J. Ticagrelor and aspirin for the prevention of cardiovascular events after coronary artery bypass graft surgery. Heart 2016, 102, 763–769. [Google Scholar] [CrossRef]
- Zhao, Q.; Zhu, Y.; Xu, Z.; Cheng, Z.; Mei, J.; Chen, X.; Wang, X. Effect of Ticagrelor Plus Aspirin, Ticagrelor Alone, or Aspirin Alone on Saphenous Vein Graft Patency 1 Year After Coronary Artery Bypass Grafting: A Randomized Clinical Trial. JAMA 2018, 319, 1677–1686. [Google Scholar] [CrossRef]
- Willemsen, L.M.; Janssen, P.W.A.; Peper, J.; Soliman-Hamad, M.A.; van Straten, A.H.M.; Klein, P.; Hackeng, C.M.; Sonker, U.; Bekker, M.W.A.; von Birgelen, C.; et al. Effect of Adding Ticagrelor to Standard Aspirin on Saphenous Vein Graft Patency in Patients Undergoing Coronary Artery Bypass Grafting (POPular CABG): A Randomized, Double-Blind, Placebo-Controlled Trial. Circulation 2020, 142, 1799–1807. [Google Scholar] [CrossRef]
- Kulik, A.; Abreu, A.M.; Boronat, V.; Kouchoukos, N.T.; Ruel, M. Ticagrelor versus aspirin 2 years after coronary bypass: Observational analysis from the TARGET trial. J. Card. Surg. 2022, 37, 1969–1977. [Google Scholar] [CrossRef]
- Sandner, S.; Redfors, B.; Angiolillo, D.J.; Audisio, K.; Fremes, S.E.; Janssen, P.W.A.; Kulik, A.; Mehran, R.; Peper, J.; Ruel, M.; et al. Association of Dual Antiplatelet Therapy With Ticagrelor With Vein Graft Failure After Coronary Artery Bypass Graft Surgery: A Systematic Review and Meta-analysis. JAMA 2022, 328, 554–562. [Google Scholar] [CrossRef]
- Post Coronary Artery Bypass Graft Trial Investigators. The effect of aggressive lowering of low-density lipoprotein cholesterol levels and low-dose anticoagulation on obstructive changes in saphenous-vein coronary-artery bypass grafts. N. Engl. J. Med. 1997, 336, 153–162. [Google Scholar] [CrossRef]
- Sacks, F.M.; Pfeffer, M.A.; Moye, L.A.; Rouleau, J.L.; Rutherford, J.D.; Cole, T.G.; Brown, L.; Warnica, J.W.; Arnold, J.M.; Wun, C.C.; et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N. Engl. J. Med. 1996, 335, 1001–1009. [Google Scholar] [CrossRef]
- Christenson, J.T. Preoperative lipid control with simvastatin reduces the risk for graft failure already 1 year after myocardial revascularization. Cardiovasc. Surg. 2001, 9, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Kulik, A.; Brookhart, M.A.; Levin, R.; Ruel, M.; Solomon, D.H.; Choudhry, N.K. Impact of statin use on outcomes after coronary artery bypass graft surgery. Circulation 2008, 118, 1785–1792. [Google Scholar] [CrossRef] [PubMed]
- Pan, E.; Nielsen, S.J.; Mennander, A.; Björklund, E.; Martinsson, A.; Lindgren, M.; Hansson, E.C.; Pivodic, A.; Jeppsson, A. Statins for secondary prevention and major adverse events after coronary artery bypass grafting. J. Thorac. Cardiovasc. Surg. 2022, 164, 1875–1886.e4. [Google Scholar] [CrossRef] [PubMed]
- Kulik, A.; Abreu, A.M.; Boronat, V.; Ruel, M. Intensive versus moderate statin therapy and early graft occlusion after coronary bypass surgery: The Aggressive Cholesterol Therapy to Inhibit Vein Graft Events randomized clinical trial. J. Thorac. Cardiovasc. Surg. 2019, 157, 151–161.e1. [Google Scholar] [CrossRef]
- Angelini, G.D.; Lloyd, C.; Bush, R.; Johnson, J.; Newby, A.C. An external, oversized, porous polyester stent reduces vein graft neointima formation, cholesterol concentration, and vascular cell adhesion molecule 1 expression in cholesterol-fed pigs. J. Thorac. Cardiovasc. Surg. 2002, 124, 950–956. [Google Scholar] [CrossRef]
- Ben-Gal, Y.; Taggart, D.P.; Williams, M.R.; Orion, E.; Uretzky, G.; Shofti, R.; Banai, S.; Yosef, L.; Bolotin, G. Expandable external support device to improve Saphenous Vein Graft Patency after CABG. J. Cardiothorac. Surg. 2013, 8, 122. [Google Scholar] [CrossRef] [PubMed]
- Murphy, G.J.; Newby, A.C.; Jeremy, J.Y.; Baumbach, A.; Angelini, G.D. A randomized trial of an external Dacron sheath for the prevention of vein graft disease: The Extent study. J. Thorac. Cardiovasc. Surg. 2007, 134, 504–505. [Google Scholar] [CrossRef] [PubMed]
- Schoettler, J.; Jussli-Melchers, J.; Grothusen, C.; Stracke, L.; Schoeneich, F.; Stohn, S.; Hoffmann, G.; Cremer, J. Highly flexible nitinol mesh to encase aortocoronary saphenous vein grafts: First clinical experiences and angiographic results nine months postoperatively. Interact Cardiovasc. Thorac. Surg. 2011, 13, 396–400. [Google Scholar] [CrossRef]
- Rescigno, G.; Aratari, C.; Matteucci, S.M.; Parisi, R.; Gironi, G.; Schicchi, N.; D’Alfonso, A.; Cola, V.; Torracca, L. Saphenous Vein Graft Wrapping by Nitinol Mesh: A Word of Caution. Thorac. Cardiovasc. Surg. 2015, 63, 292–297. [Google Scholar]
- Wan, S.; Arifi, A.A.; Chan, M.C.W.; Yip, J.H.Y.; Ng, C.S.H.; Chow, L.T.C.; Yim, A.P.C.; Jeremy, J.Y. Differential, time-dependent effects of perivenous application of fibrin glue on medial thickening in porcine saphenous vein grafts. Eur. J. Cardiothorac. Surg. 2006, 29, 742–746; discussion 747. [Google Scholar] [CrossRef] [PubMed]
- Taggart, D.P.; Ben Gal, Y.; Lees, B.; Patel, N.; Webb, C.; Rehman, S.M.; Desouza, A.; Yadav, R.; De Robertis, F.; Dalby, M.; et al. A Randomized Trial of External Stenting for Saphenous Vein Grafts in Coronary Artery Bypass Grafting. Ann. Thorac. Surg. 2015, 99, 2039–2045. [Google Scholar] [CrossRef]
- Taggart, D.P.; Webb, C.M.; Desouza, A.; Yadav, R.; Channon, K.M.; De Robertis, F.; Di Mario, C. Long-term performance of an external stent for saphenous vein grafts: The VEST IV trial. J. Cardiothorac. Surg. 2018, 13, 117. [Google Scholar] [CrossRef]
- Taggart, D.P.; Amin, S.; Djordjevic, J.; Oikonomou, E.K.; Thomas, S.; Kampoli, A.-M.; Sabharwal, N.; Antoniades, C.; Krasopoulos, G. A prospective study of external stenting of saphenous vein grafts to the right coronary artery: The VEST II study. Eur. J. Cardio-Thorac. Surg. 2017, 51, 952–958. [Google Scholar] [CrossRef] [PubMed]
- Taggart, D.P.; Gavrilov, Y.; Krasopoulos, G.; Rajakaruna, C.; Zacharias, J.; De Silva, R.; Channon, K.M.; Gehrig, T.; Donovan, T.J.; Friedrich, I.; et al. External stenting and disease progression in saphenous vein grafts two years after coronary artery bypass grafting: A multicenter randomized trial. J. Thorac. Cardiovasc. Surg. 2022, 164, 1532–1541.e2. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Kim, H.J.; Kim, J.B.; Jung, S.-H.; Choo, S.J.; Lee, J.W.; Chung, C.H. Sequential Versus Individual Saphenous Vein Grafting During Coronary Arterial Bypass Surgery. Ann. Thorac. Surg. 2020, 109, 1165–1173. [Google Scholar] [CrossRef]
- Mehta, R.H.; Ferguson, T.B.; Lopes, R.D.; Hafley, G.E.; Mack, M.J.; Kouchoukos, N.T.; Gibson, C.M.; Harrington, R.A.; Califf, R.M.; Peterson, E.D.; et al. Saphenous vein grafts with multiple versus single distal targets in patients undergoing coronary artery bypass surgery: One-year graft failure and five-year outcomes from the Project of Ex-Vivo Vein Graft Engineering via Transfection (PREVENT) IV trial. Circulation 2011, 124, 280–288. [Google Scholar] [CrossRef]
- Li, Y.; Liu, B.; Li, C.; Yu, Y.; Liu, X.; Li, L.; Li, Z.; Duan, C.; Luo, S.; Hou, W. The patency of graft and anastomoses in sequential and individual coronary artery bypass grafting: A meta-analysis. Anatol. J. Cardiol. 2020, 24, 235. [Google Scholar]
- Loop, F.D.; Lytle, B.W.; Cosgrove, D.M.; Stewart, R.W.; Goormastic, M.; Williams, G.W.; Golding, L.A.; Gill, C.C.; Taylor, P.C.; Sheldon, W.C. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N. Engl. J. Med. 1986, 314, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Voutilainen, S.M.; Järvinen, A.A.; Verkkala, K.A.; Keto, P.E.; Heikkinen, L.O.; Voutilainen, P.E.; Harjola, P.T. Angiographic 20-year follow-up of 61 consecutive patients with internal thoracic artery grafts. Ann. Surg. 1999, 229, 154–158. [Google Scholar] [CrossRef]
- Barner, H.B.; Barnett, M.G. Fifteen- to twenty-one-year angiographic assessment of internal thoracic artery as a bypass conduit. Ann. Thorac. Surg. 1994, 57, 1526–1528. [Google Scholar] [CrossRef]
- Goldman, S.; Zadina, K.; Moritz, T.; Ovitt, T.; Sethi, G.; Copeland, J.G.; Thottapurathu, L.; Krasnicka, B.; Ellis, N.; Anderson, R.J.; et al. Long-term patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery: Results from a Department of Veterans Affairs Cooperative Study. J. Am. Coll. Cardiol. 2004, 44, 2149–2156. [Google Scholar] [CrossRef] [PubMed]
- Tatoulis, J.; Buxton, B.F.; Fuller, J.A. Patencies of 2127 arterial to coronary conduits over 15 years. Ann. Thorac. Surg. 2004, 77, 93–101. [Google Scholar] [CrossRef]
- Gaudino, M.; Bakaeen, F.G.; Benedetto, U.; Di Franco, A.; Fremes, S.; Glineur, D.; Girardi, L.N.; Grau, J.; Puskas, J.D.; Ruel, M.; et al. Arterial Grafts for Coronary Bypass. Circulation 2019, 140, 1273–1284. [Google Scholar] [CrossRef] [PubMed]
- Buxton, B.F.; Hayward, P.A.; Raman, J.; Moten, S.C.; Rosalion, A.; Gordon, I.; Seevanayagam, S.; Matalanis, G.; Benedetto, U.; Gaudino, M.; et al. Long-Term Results of the RAPCO Trials. Circulation 2020, 142, 1330–1338. [Google Scholar] [CrossRef]
- Gaudino, M.; Di Franco, A.; Rahouma, M.; Tam, D.Y.; Iannaccone, M.; Deb, S.; D’Ascenzo, F.; Abouarab, A.A.; Girardi, L.N.; Taggart, D.P.; et al. Unmeasured Confounders in Observational Studies Comparing Bilateral Versus Single Internal Thoracic Artery for Coronary Artery Bypass Grafting: A Meta-Analysis. J. Am. Heart Assoc. 2018, 7, e008010. [Google Scholar] [CrossRef]
- Tatoulis, J.; Wynne, R.; Skillington, P.D.; Buxton, B.F. Total Arterial Revascularization: Achievable and Prognostically Effective-A Multicenter Analysis. Ann. Thorac. Surg. 2015, 100, 1268–1275; discussion 1275. [Google Scholar] [CrossRef]
- Gaudino, M.; Bakaeen, F.; Benedetto, U.; Rahouma, M.; Di Franco, A.; Tam, D.Y.; Iannaccone, M.; Schwann, T.A.; Habib, R.; Ruel, M.; et al. Use Rate and Outcome in Bilateral Internal Thoracic Artery Grafting: Insights From a Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2018, 7, e009361. [Google Scholar] [CrossRef] [PubMed]
- Kappetein, A.P.; Dawkins, K.D.; Mohr, F.W.; Morice, M.C.; Mack, M.J.; Russell, M.E.; Pomar, J.; Serruys, P.W.J.C. Current percutaneous coronary intervention and coronary artery bypass grafting practices for three-vessel and left main coronary artery disease. Insights from the SYNTAX run-in phase. Eur. J. Cardiothorac. Surg. 2006, 29, 486–491. [Google Scholar] [CrossRef]
- Behranwala, A.A.; Raja, S.G.; Dunning, J. Is skeletonised internal mammary harvest better than pedicled internal mammary harvest for patients undergoing coronary artery bypass grafting? Interact. CardioVascular Thorac. Surg. 2005, 4, 577–582. [Google Scholar] [CrossRef][Green Version]
- Kieser, T.M.; Aluthman, U.; Narine, K.; Rose, M.S. Quicker yet safe: Skeletonization of 1640 internal mammary arteries with harmonic technology in 965 patients. Eur. J. Cardio-Thorac. Surg. 2014, 45, e142–e150. [Google Scholar] [CrossRef]
- Eikelboom, J.W.; Connolly, S.J.; Bosch, J.; Dagenais, G.R.; Hart, R.G.; Shestakovska, O.; Diaz, R.; Alings, M.; Lonn, E.M.; Anand, S.S.; et al. Rivaroxaban with or without Aspirin in Stable Cardiovascular Disease. N. Engl. J. Med. 2017, 377, 1319–1330. [Google Scholar] [CrossRef]
- Lamy, A.; Browne, A.; Sheth, T.; Zheng, Z.; Dagenais, F.; Noiseux, N.; Chen, X.; Bakeen, F.G.; Brtko, M.; Stevens, L.-M.; et al. Skeletonized vs Pedicled Internal Mammary Artery Graft Harvesting in Coronary Artery Bypass Surgery: A Post Hoc Analysis From the COMPASS Trial. JAMA Cardiol. 2021, 6, 1042–1049. [Google Scholar] [CrossRef]
- Taggart, D.P.; Benedetto, U.; Gerry, S.; Altman, D.G.; Gray, A.M.; Lees, B.; Gaudino, M.; Zamvar, V.; Bochenek, A.; Buxton, B.; et al. Bilateral versus Single Internal-Thoracic-Artery Grafts at 10 Years. N. Engl. J. Med. 2019, 380, 437–446. [Google Scholar] [CrossRef]
- Gaudino, M.; Audisio, K.; Rahouma, M.; Chadow, D.; Cancelli, G.; Soletti, G.J.; Gray, A.; Lees, B.; Gerry, S.; Benedetto, U.; et al. Comparison of Long-term Clinical Outcomes of Skeletonized vs Pedicled Internal Thoracic Artery Harvesting Techniques in the Arterial Revascularization Trial. JAMA Cardiol. 2021, 6, 1380–1386. [Google Scholar] [CrossRef]
- Gaudino, M.; Toesca, A.; Nori, S.L.; Glieca, F.; Possati, G. Effect of skeletonization of the internal thoracic artery on vessel wall integrity. Ann. Thorac. Surg. 1999, 68, 1623–1627. [Google Scholar] [CrossRef]
- Puslecki, M.; Buczkowski, P.; Nowicki, M.; Sujka-Kordowska, P.; Ligowski, M.; Misterski, M.; Stefaniak, S.; Dąbrowski, M.; Dabrowska, A.; Bocianski, M.; et al. An innovative panel to assess endothelial integrity of pedicled and skeletonized internal thoracic artery used as aortocoronary bypass graft: A randomized comparative histologic and immunohistochemical study. J. Thorac. Dis. 2018, 10, 4865–4873. [Google Scholar] [CrossRef]
- Dreifaldt, M.; Samano, N.; Geijer, H.; Lidén, M.; Bodin, L.; Souza, D. Pedicled versus skeletonized internal thoracic artery grafts: A randomized trial. Asian Cardiovasc. Thorac. Ann. 2021, 29, 490–497. [Google Scholar] [CrossRef]
- Glineur, D.; Hanet, C.; Poncelet, A.; D’hoore, W.; Funken, J.-C.; Rubay, J.; Kefer, J.; Astarci, P.; Lacroix, V.; Verhelst, R.; et al. Comparison of bilateral internal thoracic artery revascularization using in situ or Y graft configurations: A prospective randomized clinical, functional, and angiographic midterm evaluation. Circulation 2008, 118, S216–S221. [Google Scholar] [CrossRef]
- Glineur, D.; Boodhwani, M.; Hanet, C.; de Kerchove, L.; Navarra, E.; Astarci, P.; Noirhomme, P.; El Khoury, G. Bilateral Internal Thoracic Artery Configuration for Coronary Artery Bypass Surgery. Circ. Cardiovasc. Interv. 2016, 9, e003518. [Google Scholar] [CrossRef]
- Calafiore, A.M.; Contini, M.; Vitolla, G.; Di Mauro, M.; Mazzei, V.; Teodori, G.; Di Giammarco, G. Bilateral internal thoracic artery grafting: Long-term clinical and angiographic results of in situ versus Y grafts. J. Thorac. Cardiovasc. Surg. 2000, 120, 990–996. [Google Scholar] [CrossRef]
- Bakaeen, F.G.; Ghandour, H.; Ravichandren, K.; Zhen-Yu Tong, M.; Soltesz, E.G.; Johnston, D.R.; Roselli, E.E.; Houghtaling, P.L.; Pettersson, G.B.; Smedira, N.G.; et al. Right Internal Thoracic Artery Patency Is Affected More by Target Choice Than Conduit Configuration. Ann. Thorac. Surg. 2022, 114, 458–466. [Google Scholar] [CrossRef]
- Tatoulis, J.; Buxton, B.F.; Fuller, J.A. The right internal thoracic artery: The forgotten conduit--5,766 patients and 991 angiograms. Ann. Thorac. Surg. 2011, 92, 9–15; discussion 15–17. [Google Scholar] [CrossRef]
- Robinson, B.M.; Paterson, H.S.; Naidoo, R.; Dhurandhar, V.; Denniss, A.R. Bilateral Internal Thoracic Artery Composite Y Grafts: Analysis of 464 Angiograms in 296 Patients. Ann. Thorac. Surg. 2016, 101, 974–980. [Google Scholar] [CrossRef]
- Bakay, C.; Onan, B.; Korkmaz, A.A.; Onan, I.S.; Özkara, A. Sequential in situ left internal thoracic artery grafting to the circumflex and right coronary artery areas. Ann. Thorac. Surg. 2013, 95, 63–70. [Google Scholar] [CrossRef]
- Ohira, S.; Doi, K.; Okawa, K.; Dohi, M.; Yamamoto, T.; Kawajiri, H.; Yaku, H. Safety and Efficacy of Sequential Left Internal Thoracic Artery Grafting to Left Circumflex Area. Ann. Thorac. Surg. 2016, 102, 766–773. [Google Scholar] [CrossRef]
- Ji, Q.; Shi, Y.; Xia, L.; Ma, R.; Shen, J.; Lai, H.; Ding, W.; Wang, C. Revascularization of Left Coronary System Using a Skeletonized Left Internal Mammary Artery—Sequential vs. Separate Grafting. Circ. J. 2017, 82, 102–109. [Google Scholar] [CrossRef]
- Nakajima, H.; Kobayashi, J.; Toda, K.; Fujita, T.; Shimahara, Y.; Kasahara, Y.; Kitamura, S. A 10-year angiographic follow-up of competitive flow in sequential and composite arterial grafts. Eur. J. Cardiothorac. Surg. 2011, 40, 399–404. [Google Scholar] [CrossRef]
- Glineur, D.; Grau, J.B.; Etienne, P.-Y.; Benedetto, U.; Fortier, J.H.; Papadatos, S.; Laruelle, C.; Pieters, D.; El Khoury, E.; Blouard, P.; et al. Impact of preoperative fractional flow reserve on arterial bypass graft anastomotic function: The IMPAG trial. Eur. Heart J. 2019, 40, 2421–2428. [Google Scholar] [CrossRef]
- Glineur, D.; Rahouma, M.; Grau, J.B.; Etienne, P.-Y.; Fortier, J.H.; Papadatos, S.; Laruelle, C.; Pieters, D.; El, K.E.; Gaudino, M. FFR Cutoff by Arterial Graft Configuration and Location. JACC Cardiovasc. Interv. 2020, 13, 143–144. [Google Scholar] [CrossRef]
- Carpentier, A.; Guermonprez, J.L.; Deloche, A.; Frechette, C.; DuBost, C. The aorta-to-coronary radial artery bypass graft. A technique avoiding pathological changes in grafts. Ann. Thorac. Surg. 1973, 16, 111–121. [Google Scholar] [CrossRef]
- Geha, A.S.; Krone, R.J.; McCormick, J.R.; Baue, A.E. Selection of coronary bypass: Anatomic, physiological, and angiographic considerations of vein and mammary artery grafts. J. Thorac. Cardiovasc. Surg. 1975, 70, 414–431. [Google Scholar] [CrossRef]
- Acar, C.; Ramsheyi, A.; Pagny, J.Y.; Jebara, V.; Barrier, P.; Fabiani, N.; Deloche, A.; Guermonprez, J.L.; Carpentier, A.; Barner, H.B.; et al. The radial artery for coronary artery bypass grafting: Clinical and angiographic results at five years. J. Thorac. Cardiovasc. Surg. 1998, 116, 981–989. [Google Scholar] [CrossRef]
- Aldea, G.S.; Bakaeen, F.G.; Pal, J.; Fremes, S.; Head, S.J.; Sabik, J.; Rosengart, T.; Kappetein, A.P.; Thourani, V.H.; Firestone, S.; et al. The Society of Thoracic Surgeons Clinical Practice Guidelines on Arterial Conduits for Coronary Artery Bypass Grafting. Ann. Thorac. Surg. 2016, 101, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Tatoulis, J. The radial artery: An important component of multiarterial coronary surgery and considerations for its optimal harvest. JTCVS Tech. 2021, 5, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Tatoulis, J.; Buxton, B.F.; Fuller, J.A.; Meswani, M.; Theodore, S.; Powar, N.; Wynne, R. Long-term patency of 1108 radial arterial-coronary angiograms over 10 years. Ann. Thorac. Surg. 2009, 88, 23–30. [Google Scholar] [CrossRef]
- van Son, J.A.; Smedts, F.; Vincent, J.G.; van Lier, H.J.; Kubat, K. Comparative anatomic studies of various arterial conduits for myocardial revascularization. J. Thorac. Cardiovasc. Surg. 1990, 99, 703–707. [Google Scholar] [CrossRef]
- Yie, K.; Na, C.-Y.; Oh, S.S.; Kim, J.-H.; Shinn, S.-H.; Seo, H.-J. Angiographic results of the radial artery graft patency according to the degree of native coronary stenosis. Eur. J. Cardiothorac. Surg. 2008, 33, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Gaudino, M.; Tondi, P.; Benedetto, U.; Milazzo, V.; Flore, R.; Glieca, F.; Ponziani, F.R.; Luciani, N.; Girardi, L.N.; Crea, F.; et al. Radial Artery as a Coronary Artery Bypass Conduit: 20-Year Results. J. Am. Coll. Cardiol. 2016, 68, 603–610. [Google Scholar] [CrossRef]
- Hosono, M.; Murakami, T.; Hirai, H.; Sasaki, Y.; Suehiro, S.; Shibata, T. The Risk Factor Analysis for the Late Graft Failure of Radial Artery Graft in Coronary Artery Bypass Grafting. Ann. Thorac. Cardiovasc. Surg. 2019, 25, 32–38. [Google Scholar] [CrossRef]
- Kasahara, H.; Shin, H.; Takahashi, T.; Murata, S.; Mori, M. Comparison of patency of single and sequential radial artery grafting in coronary artery bypass. Interact. CardioVascular Thorac. Surg. 2022, 34, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, H.; Kobayashi, J.; Toda, K.; Fujita, T.; Shimahara, Y.; Kasahara, Y.; Kitamura, S. Determinants for successful sequential radial artery grafting to the left circumflex and right coronary arteries. Interact. CardioVascular Thorac. Surg. 2011, 12, 125–129. [Google Scholar] [CrossRef]
- Gaudino, M.; Alessandrini, F.; Pragliola, C.; Cellini, C.; Glieca, F.; Luciani, N.; Girola, F.; Possati, G. Effect of target artery location and severity of stenosis on mid-term patency of aorta-anastomosed vs. internal thoracic artery-anastomosed radial artery grafts. Eur. J. Cardiothorac. Surg. 2004, 25, 424–428. [Google Scholar] [CrossRef]
- Kamiya, H.; Ushijima, T.; Kanamori, T.; Ikeda, C.; Nakagaki, C.; Ueyama, K.; Watanabe, G. Use of the radial artery graft after transradial catheterization: Is it suitable as a bypass conduit? Ann. Thorac. Surg. 2003, 76, 1505–1509. [Google Scholar] [CrossRef]
- Antonopoulos, A.S.; Odutayo, A.; Oikonomou, E.K.; Trivella, M.; Petrou, M.; Collins, G.S.; Antoniades, C.; SAFINOUS-CABG (Saphenous Vein Graft Failure—An Outcomes Study in Coronary Artery Bypass Grafting) Group. Development of a risk score for early saphenous vein graft failure: An individual patient data meta-analysis. J. Thorac. Cardiovasc. Surg. 2020, 160, 116–127.e4. [Google Scholar] [CrossRef]
- Staniloae, C.S.; Mody, K.P.; Sanghvi, K.; Mindrescu, C.; Coppola, J.T.; Antonescu, C.R.; Shah, S.; Patel, T. Histopathologic changes of the radial artery wall secondary to transradial catheterization. Vasc. Health Risk Manag. 2009, 5, 527–532. [Google Scholar]
- Chadow, D.; Soletti, G.J.; Gaudino, M. Never Again. Once Used for Cardiac Catherization the Radial Artery Cannot be Used for CABG. J. Card. Surg. 2021, 36, 4799–4800. Available online: https://onlinelibrary.wiley.com/doi/10.1111/jocs.16045 (accessed on 11 January 2023). [CrossRef]
- Bailey, C.P.; Hirose, T.; Aventura, A.; Yamamoto, N.; Brancato, R.; Vera, C.; O’Connor, R. Revascularization of the ischemic posterior myocardium. Dis. Chest 1967, 52, 273–285. [Google Scholar] [CrossRef]
- Suma, H.; Tanabe, H.; Takahashi, A.; Horii, T.; Isomura, T.; Hirose, H.; Amano, A. Twenty Years Experience With the Gastroepiploic Artery Graft for CABG. Circulation 2007, 116 (Suppl. 11), I–188. [Google Scholar] [CrossRef]
- Suzuki, T.; Asai, T.; Nota, H.; Kuroyanagi, S.; Kinoshita, T.; Takashima, N.; Hayakawa, M. Early and long-term patency of in situ skeletonized gastroepiploic artery after off-pump coronary artery bypass graft surgery. Ann. Thorac. Surg. 2013, 96, 90–95. [Google Scholar] [CrossRef]
- Akita, S.; Tajima, K.; Kato, W.; Tanaka, K.; Goto, Y.; Yamamoto, R.; Yazawa, T.; Kozakai, M.; Usui, A. The long-term patency of a gastroepiploic artery bypass graft deployed in a semiskeletonized fashion: Predictors of patency. Interact Cardiovasc. Thorac. Surg. 2019, 28, 868–875. [Google Scholar] [CrossRef]
- Gaudino, M.; Benedetto, U.; Fremes, S.; Biondi-Zoccai, G.; Sedrakyan, A.; Puskas, J.D.; Angelini, G.D.; Buxton, B.; Frati, G.; Hare, D.L.; et al. Radial-Artery or Saphenous-Vein Grafts in Coronary-Artery Bypass Surgery. N. Engl. J. Med. 2018, 378, 2069–2077. [Google Scholar] [CrossRef]
- Deng, M.X.; Lia, H.; Lee, G.; Rahouma, M.; Franco, A.D.; Demetres, M.; Angelini, G.D.; Gaudino, M.; Fremes, S.E. Angiographic Patency of Coronary Artery Bypass Conduits: An Updated Network Meta-Analysis of Randomized Trials. Braz. J. Cardiovasc. Surg. 2022, 37, 7–31. [Google Scholar] [CrossRef]
- Houlind, K.; Fenger-Grøn, M.; Holme, S.J.; Kjeldsen, B.J.; Madsen, S.N.; Rasmussen, B.S.; Jepsen, M.H.; Ravkilde, J.; Aaroe, J.; Hansen, P.R.; et al. Graft patency after off-pump coronary artery bypass surgery is inferior even with identical heparinization protocols: Results from the Danish On-pump Versus Off-pump Randomization Study (DOORS). J. Thorac. Cardiovasc. Surg. 2014, 148, 1812–1819.e2. [Google Scholar] [CrossRef]
- Hattler, B.; Messenger, J.C.; Shroyer, A.L.; Collins, J.F.; Haugen, S.J.; Garcia, J.A.; Baltz, J.H.; Cleveland, J.C.; Novitzky, D.; Grover, F.L.; et al. Off-Pump coronary artery bypass surgery is associated with worse arterial and saphenous vein graft patency and less effective revascularization: Results from the Veterans Affairs Randomized On/Off Bypass (ROOBY) trial. Circulation 2012, 125, 2827–2835. [Google Scholar] [CrossRef]
- Noiseux, N.; Stevens, L.-M.; Chartrand-Lefebvre, C.; Soulez, G.; Prieto, I.; Basile, F.; Mansour, S.; Dyub, A.M.; Kieser, T.M.; Lamy, A.; et al. Off-pump Versus On-pump Coronary Artery Bypass Surgery: Graft Patency Assessment With Coronary Computed Tomographic Angiography: A Prospective Multicenter Randomized Controlled Pilot Study. J. Thorac. Imaging 2017, 32, 370–377. [Google Scholar] [CrossRef]
- Zhou, Z.; Fu, G.; Feng, K.; Huang, S.; Chen, G.; Liang, M.; Wu, Z. Randomized evidence on graft patency after off-pump versus on-pump coronary artery bypass grafting: An updated meta-analysis. Int. J. Surg. 2022, 98, 106212. [Google Scholar] [CrossRef]
- Dimagli, A.; Weiss, A.J.; Bakaeen, F.G. Off-Pump Coronary Artery Bypass Grafting—Not for Every Patient, Not for Every Surgeon. JAMA Surg. 2022, 157, 310–311. [Google Scholar] [CrossRef] [PubMed]
- Detter, C.; Reichenspurner, H.; Boehm, D.H.; Thalhammer, M.; Raptis, P.; Schütz, A.; Reichart, B. Minimally invasive direct coronary artery bypass grafting (MIDCAB) and off-pump coronary artery bypass grafting (OPCAB): Two techniques for beating heart surgery. Heart Surg. Forum 2002, 5, 157–162. [Google Scholar]
- Diegeler, A.; Matin, M.; Kayser, S.; Binner, C.; Autschbach, R.; Battellini, R.; Krankenberg, H.; Mohr, F.W. Angiographic results after minimally invasive coronary bypass grafting using the minimally invasive direct coronary bypass grafting (MIDCAB) approach. Eur. J. Cardiothorac. Surg. 1999, 15, 680–684. [Google Scholar] [CrossRef]
- Mack, M.J.; Magovern, J.A.; Acuff, T.A.; Landreneau, R.J.; Tennison, D.M.; Tinnerman, E.J.; Osborne, J.A. Results of graft patency by immediate angiography in minimally invasive coronary artery surgery. Ann. Thorac. Surg. 1999, 68, 383–389; discussion 389–390. [Google Scholar] [CrossRef]
- Ruel, M.; Shariff, M.A.; Lapierre, H.; Goyal, N.; Dennie, C.; Sadel, S.M.; Sohmer, B.; McGinn, J.T. Results of the minimally invasive coronary artery bypass grafting angiographic patency study. J. Thorac. Cardiovasc. Surg. 2014, 147, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Repossini, A.; Bacco, L.D.; Nicoli, F.; Passaretti, B.; Stara, A.; Jonida, B.; Muneretto, C. Minimally invasive coronary artery bypass: Twenty-year experience. J. Thorac. Cardiovasc. Surg. 2019, 158, 127–138.e1. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Yang, M.; Wu, Y.; Wang, G.; Wang, J.; Yan, J.; Gao, C. A 7-year, single-center research and long term follow-up of graft patency of robotic total arterial off-pump coronary artery bypass grafting. Med. J. Chin. People’s Lib. Army 2016, 41, 512–517. [Google Scholar]
- Kitahara, H.; Nisivaco, S.; Balkhy, H.H. Graft Patency after Robotically Assisted Coronary Artery Bypass Surgery. Innovations 2019, 14, 117–123. [Google Scholar] [CrossRef]
- Doenst, T.; Haverich, A.; Serruys, P.; Bonow, R.O.; Kappetein, P.; Falk, V.; Velazquez, E.; Diegeler, A.; Sigusch, H. PCI and CABG for Treating Stable Coronary Artery Disease: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2019, 73, 964–976. [Google Scholar] [CrossRef]
- Lytle, B.W.; Loop, F.D.; Taylor, P.C.; Simpfendorfer, C.; Kramer, J.R.; Ratliff, N.B.; Goormastic, M.; Cosgrove, D.M. Vein graft disease: The clinical impact of stenoses in saphenous vein bypass grafts to coronary arteries. J. Thorac. Cardiovasc. Surg. 1992, 103, 831–840. [Google Scholar] [CrossRef]
- Lopes, R.D.; Mehta, R.H.; Hafley, G.E.; Williams, J.B.; Mack, M.J.; Peterson, E.D.; Allen, K.B.; Harrington, R.A.; Gibson, C.M.; Califf, R.M.; et al. Relationship between vein graft failure and subsequent clinical outcomes after coronary artery bypass surgery. Circulation 2012, 125, 749–756. [Google Scholar] [CrossRef]
- Shavadia, J.; Norris, C.M.; Graham, M.M.; Verma, S.; Ali, I.; Bainey, K.R. Symptomatic graft failure and impact on clinical outcome after coronary artery bypass grafting surgery: Results from the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease registry. Am. Heart J. 2015, 169, 833–840. [Google Scholar] [CrossRef] [PubMed]
- Gaudino, M.; Di Franco, A.; Bhatt, D.L.; Alexander, J.H.; Abbate, A.; Azzalini, L.; Sandner, S.; Sharma, G.; Rao, S.V.; Crea, F.; et al. The association between coronary graft patency and clinical status in patients with coronary artery disease. Eur. Heart J. 2021, 42, 1433–1441. [Google Scholar] [CrossRef]
- Morice, M.-C.; Feldman, T.E.E.; Mack, M.J.; Ståhle, E.; Holmes, D.R.; Colombo, A.; Morel, M.-A.; van den Brand, M.; Serruys, P.W.; Mohr, F.; et al. Angiographic outcomes following stenting or coronary artery bypass surgery of the left main coronary artery: Fifteen-month outcomes from the synergy between PCI with TAXUS express and cardiac surgery left main angiographic substudy (SYNTAX-LE MANS). EuroIntervention 2011, 7, 670–679. [Google Scholar] [CrossRef]
- Benedetto, U.; Raja, S.G.; Albanese, A.; Amrani, M.; Biondi-Zoccai, G.; Frati, G. Searching for the second best graft for coronary artery bypass surgery: A network meta-analysis of randomized controlled trials†. Eur. J. Cardiothorac. Surg. 2015, 47, 59–65; discussion 65. [Google Scholar] [CrossRef] [PubMed]
- Gaudino, M.; Di Franco, A.; Flather, M.; Gerry, S.; Bagiella, E.; Gray, A.; Pearcey, L.; Saw, T.-H.; Lees, B.; Benedetto, U.; et al. Association of Age With 10-Year Outcomes After Coronary Surgery in the Arterial Revascularization Trial. J. Am. Coll. Cardiol. 2021, 77, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Chikwe, J.; Sun, E.; Hannan, E.L.; Itagaki, S.; Lee, T.; Adams, D.H.; Egorova, N.N. Outcomes of Second Arterial Conduits in Patients Undergoing Multivessel Coronary Artery Bypass Graft Surgery. J. Am. Coll. Cardiol. 2019, 74, 2238–2248. [Google Scholar] [CrossRef] [PubMed]
- Perezgrovas-Olaria, R.; Audisio, K.; Cancelli, G.; Rahouma, M.; Ibrahim, M.; Soletti, G.J.; Chadow, D.; Demetres, M.; Girardi, L.N.; Gaudino, M. Deep Sternal Wound Infection and Mortality in Cardiac Surgery: A Meta-analysis. Ann. Thorac. Surg. 2023, 115, 272–280. [Google Scholar] [CrossRef]
- Naito, S.; Demal, T.J.; Sill, B.; Reichenspurner, H.; Onorati, F.; Gatti, G.; Mariscalco, G.; Faggian, G.; Salsano, A.; Santini, F.; et al. Impact of Surgeon Experience and Centre Volume on Outcome After Off-Pump Coronary Artery Bypass Surgery: Results from the European Multicenter Study on Coronary Artery Bypass Grafting (E-CABG) Registry. Heart Lung Circ. 2022. [Google Scholar] [CrossRef]
- Ueki, C.; Yamamoto, H.; Motomura, N.; Miyata, H.; Sakata, R.; Tsuneyoshi, H. Effect of Hospital and Surgeon Procedure Volumes on the Incidence of Intraoperative Conversion During Off-Pump Coronary Artery Bypass Grafting. Semin. Thorac. Cardiovasc. Surg. 2021, 33, 49–58. [Google Scholar] [CrossRef]
- Taggart, D.P.; Gaudino, M.F.; Gerry, S.; Gray, A.; Lees, B.; Sajja, L.R.; Zamvar, V.; Flather, M.; Benedetto, U. Arterial Revascularization Trial Investigators Ten-year outcomes after off-pump versus on-pump coronary artery bypass grafting: Insights from the Arterial Revascularization Trial. J. Thorac. Cardiovasc. Surg. 2021, 162, 591–599.e8. [Google Scholar] [CrossRef]
- Gaudino, M.; Alexander, J.H.; Bakaeen, F.G.; Ballman, K.; Barili, F.; Calafiore, A.M.; Davierwala, P.; Goldman, S.; Kappetein, P.; Lorusso, R.; et al. Randomized comparison of the clinical outcome of single versus multiple arterial grafts: The ROMA trial-rationale and study protocol. Eur. J. Cardiothorac. Surg. 2017, 52, 1031–1040. [Google Scholar] [CrossRef]
- Gaudino, M.; Taggart, D.; Suma, H.; Puskas, J.D.; Crea, F.; Massetti, M. The Choice of Conduits in Coronary Artery Bypass Surgery. J. Am. Coll. Cardiol. 2015, 66, 1729–1737. [Google Scholar] [CrossRef]


| Conduit | Patency Rate |
|---|---|
| RA | 94.1% (95% CI 90.0–97.6) |
| No touch-SVG | 91.4% (95% CI 87.3–94.3) |
| RITA | 89.2% (95% CI 71.2–96.5) |
| Conventionally harvested SVG | 86.3% (95% CI 81.2–90.2) |
| GEA | 61.2% (95% CI 52.2–69.4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dimagli, A.; Soletti, G., Jr.; Harik, L.; Perezgrovas Olaria, R.; Cancelli, G.; An, K.R.; Alzghari, T.; Mack, C.; Gaudino, M. Angiographic Outcomes for Arterial and Venous Conduits Used in CABG. J. Clin. Med. 2023, 12, 2022. https://doi.org/10.3390/jcm12052022
Dimagli A, Soletti G Jr., Harik L, Perezgrovas Olaria R, Cancelli G, An KR, Alzghari T, Mack C, Gaudino M. Angiographic Outcomes for Arterial and Venous Conduits Used in CABG. Journal of Clinical Medicine. 2023; 12(5):2022. https://doi.org/10.3390/jcm12052022
Chicago/Turabian StyleDimagli, Arnaldo, Giovanni Soletti, Jr., Lamia Harik, Roberto Perezgrovas Olaria, Gianmarco Cancelli, Kevin R. An, Talal Alzghari, Charles Mack, and Mario Gaudino. 2023. "Angiographic Outcomes for Arterial and Venous Conduits Used in CABG" Journal of Clinical Medicine 12, no. 5: 2022. https://doi.org/10.3390/jcm12052022
APA StyleDimagli, A., Soletti, G., Jr., Harik, L., Perezgrovas Olaria, R., Cancelli, G., An, K. R., Alzghari, T., Mack, C., & Gaudino, M. (2023). Angiographic Outcomes for Arterial and Venous Conduits Used in CABG. Journal of Clinical Medicine, 12(5), 2022. https://doi.org/10.3390/jcm12052022






