Outcomes of Intraductal Placement of Covered Metal Stents for Unresectable Distal Malignant Biliary Obstruction
Abstract
1. Introduction
2. Materials and Methods
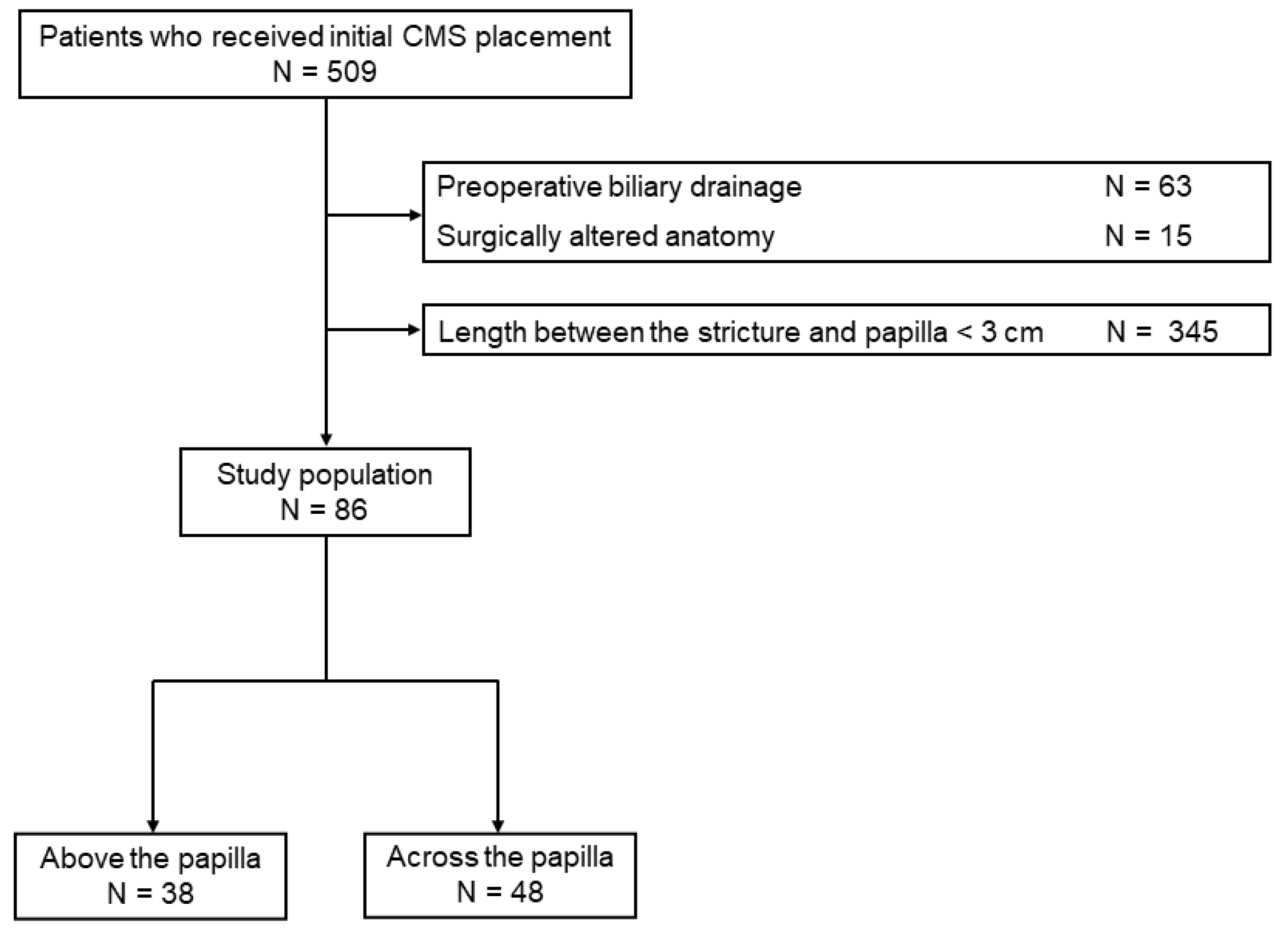
2.1. Patients
2.2. Endoscopic Interventions
2.3. Outcomes and Definitions
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
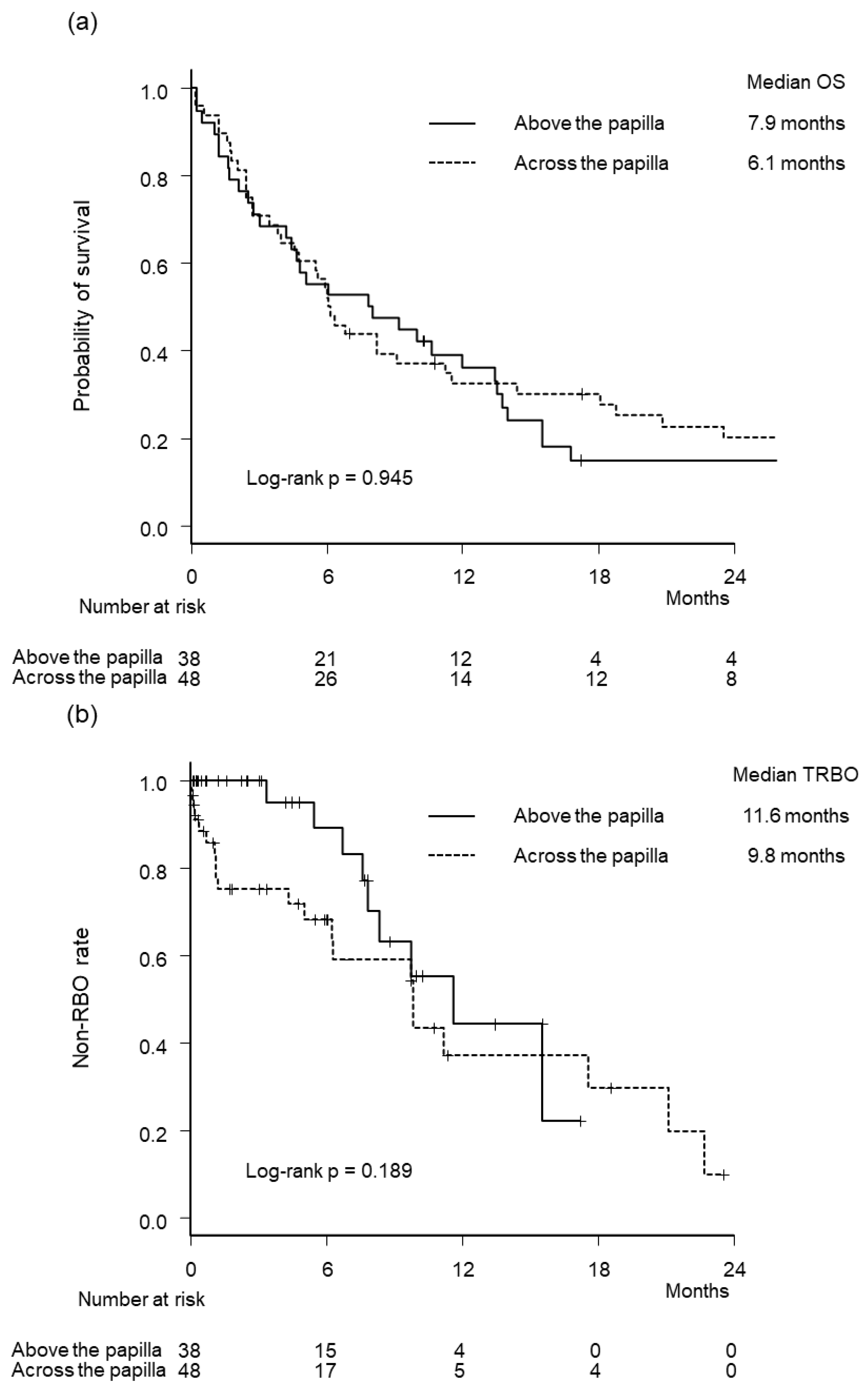
3.2. Outcome Measures
3.3. Reinterventions
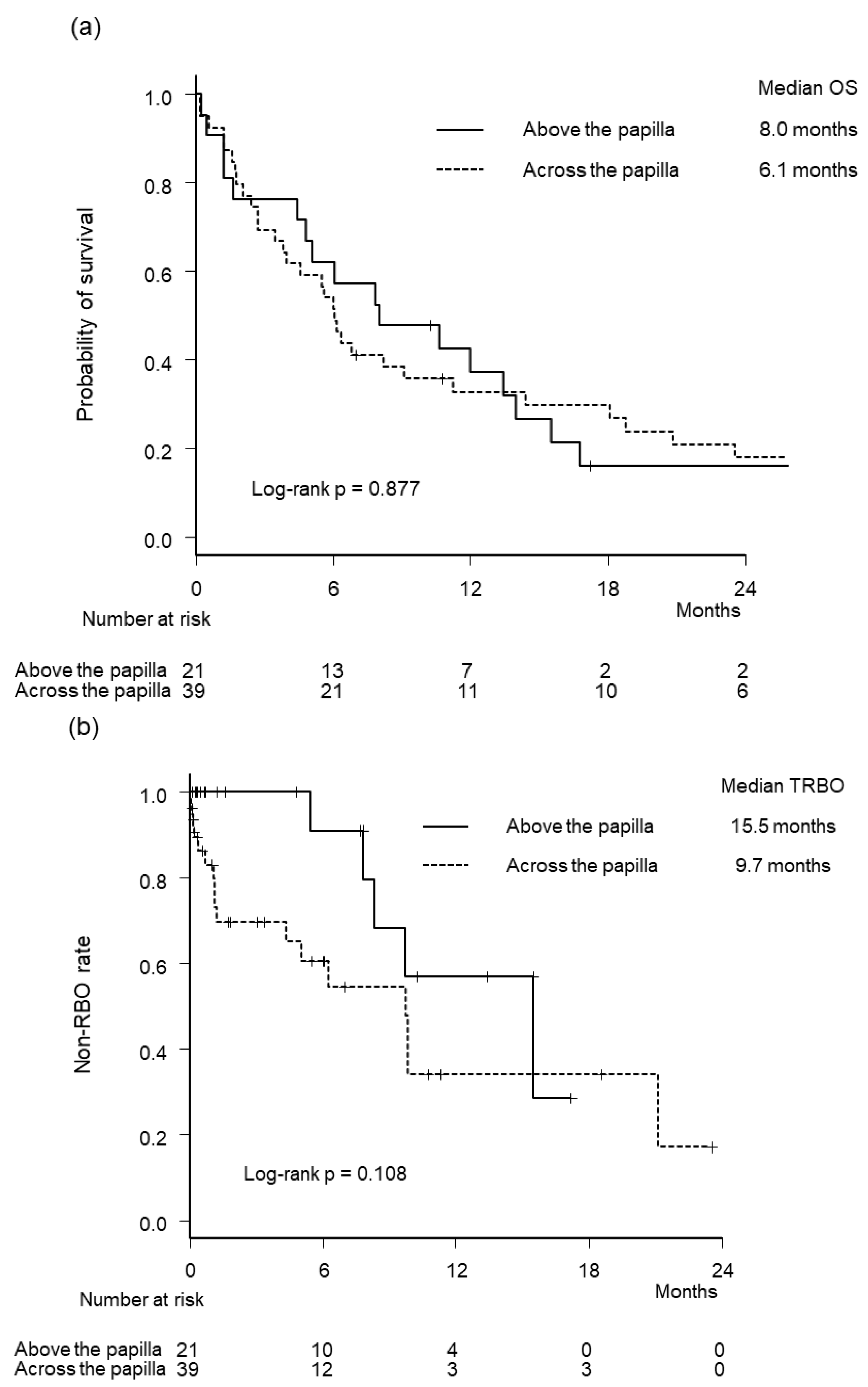
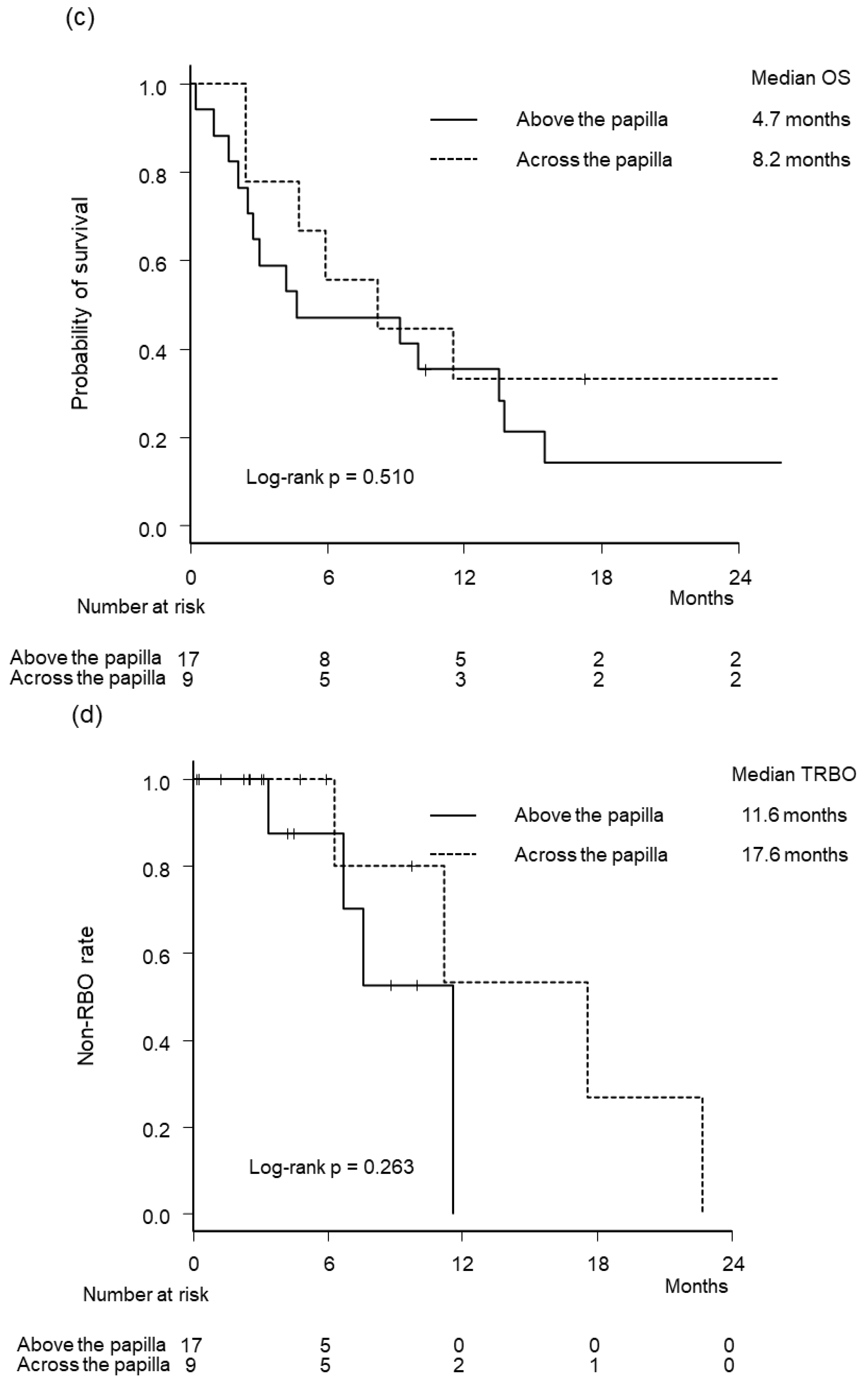
3.4. Subgroup Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Isayama, H.; Yasuda, I.; Ryozawa, S.; Maguchi, H.; Igarashi, Y.; Matsuyama, Y.; Katanuma, A.; Hasebe, O.; Irisawa, A.; Itoi, T.; et al. Results of a Japanese multicenter, randomized trial of endoscopic stenting for non-resectable pancreatic head cancer (JM-test): Covered Wallstent versus DoubleLayer stent. Dig. Endosc. 2011, 23, 310–315. [Google Scholar] [CrossRef]
- Nakai, Y.; Isayama, H.; Wang, H.P.; Rerknimitr, R.; Khor, C.; Yasuda, I.; Kogure, H.; Moon, J.H.; Lau, J.; Lakhtakia, S.; et al. International consensus statements for endoscopic management of distal biliary stricture. J. Gastroenterol. Hepatol. 2020, 35, 967–979. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, Y.; Tachikawa, A.; Shimokawa, T.; Yamazaki, H.; Itonaga, M.; Sakai, Y.; Sugiyama, H.; Nakai, Y.; Tanaka, K.; Isayama, H.; et al. Covered versus uncovered metal stent for endoscopic drainage of a malignant distal biliary obstruction: Meta-analysis. Dig. Endosc. 2022, 34, 938–951. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, T.; Fujioka, S.; Yanagisawa, S.; Yanaga, K.; Kakutani, H.; Tajiri, H.; Urashima, M. Placement of a metallic stent across the main duodenal papilla may predispose to cholangitis. Gastrointest. Endosc. 2006, 63, 792–796. [Google Scholar] [CrossRef] [PubMed]
- Misra, S.P.; Dwivedi, M. Reflux of duodenal contents and cholangitis in patients undergoing self-expanding metal stent placement. Gastrointest. Endosc. 2009, 70, 317–321. [Google Scholar] [CrossRef] [PubMed]
- Uchida, N.; Tsutsui, K.; Ezaki, T.; Fukuma, H.; Kamata, H.; Kobara, H.; Matsuoka, H.; Kinekawa, F.; Aritomo, Y.; Yokoyama, F.; et al. Estimation of the stent placement above the intact sphincter of Oddi against malignant bile duct obstruction. J. Gastroenterol. 2005, 40, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.J.; Moon, J.H.; Lee, Y.N.; Kim, H.S.; Choi, M.H.; Lee, T.H.; Cha, S.W.; Cho, Y.D.; Park, S.H.; Kim, S.J. Evaluation of a newly modified nonflared fully covered metal stent, 12 mm in diameter, for intraductal placement in patients with malignant biliary strictures: A feasibility study. Endoscopy 2016, 48, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Inoue, T.; Suzuki, Y.; Okumura, F.; Naitoh, I.; Sano, H.; Ibusuki, M.; Kitano, R.; Kobayashi, Y.; Ito, K.; Yoneda, M. Intraductal placement of a fully covered metal stent with a long string for distal malignant biliary obstruction without endoscopic sphincterotomy: Prospective multi-center feasibility study. Dig. Endosc. 2020, 32, 949–956. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.N.; Han, J.; Kim, H.G.; Shin, I.H.; Park, S.H.; Moon, J.H.; Kim, J.H.; Lee, D.H.; Maetani, I.; Maguchi, H.; et al. Prospective randomized trial comparing covered metal stent placed above and across the sphincter of oddi in malignant biliary obstruction. Gastrointest. Endosc. 2013, 77, AB139–AB140. [Google Scholar] [CrossRef]
- Takada, R.; Ikezawa, K.; Kiyota, R.; Imai, T.; Abe, Y.; Fukutake, N.; Ashida, R.; Nawa, T.; Tabuchi, T.; Katayama, K.; et al. Self-expandable metallic stent placement above the papilla without endoscopic sphincterotomy in patients with distal malignant biliary obstruction. Endosc. Int. Open 2020, 8, E753–E760. [Google Scholar] [CrossRef] [PubMed]
- Mangiavillano, B.; Montale, A.; Frazzoni, L.; Bianchetti, M.; Sethi, A.; Repici, A.; Fuccio, L. Endoscopic biliary self-expandable metallic stent in malignant biliary obstruction with or without sphincterotomy: Systematic review and meta-analysis. Endosc. Int. Open 2019, 7, E26–E35. [Google Scholar] [CrossRef] [PubMed]
- Isayama, H.; Hamada, T.; Yasuda, I.; Itoi, T.; Ryozawa, S.; Nakai, Y.; Kogure, H.; Koike, K. TOKYO criteria 2014 for transpapillary biliary stenting. Dig. Endosc. 2015, 27, 259–264. [Google Scholar] [CrossRef]
- Cotton, P.B.; Eisen, G.M.; Aabakken, L.; Baron, T.H.; Hutter, M.M.; Jacobson, B.C.; Mergener, K.; Nemcek, A., Jr.; Petersen, B.T.; Petrini, J.L.; et al. A lexicon for endoscopic adverse events: Report of an ASGE workshop. Gastrointest. Endosc. 2010, 71, 446–454. [Google Scholar] [CrossRef]
- Gray, R.J. A Class of K-Sample Tests for Comparing the Cumulative Incidence of a Competing Risk. Ann. Stat. 1988, 16, 1141–1154. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed]

| Above the Papilla n = 38 | Across the Papilla n = 48 | p Value | ||
|---|---|---|---|---|
| Age, years | 71 (46–96) | 70 (47–88) | 0.537 | |
| Sex | 0.823 | |||
| Male | 13 (34%) | 18 (38%) | ||
| Female | 25 (66%) | 30 (63%) | ||
| Eastern Cooperative Oncology Group Performance status | 0.126 | |||
| 0 | 27 (71%) | 35 (73%) | ||
| 1 | 10 (26%) | 7 (15%) | ||
| ≥2 | 1 (3%) | 6 (13%) | ||
| Stricture length, mm | 21 (8–41) | 22 (12–40) | 0.770 | |
| Length between the distal end of the stricture and the papilla, mm | 34 (30–77) | 34 (30–45) | 0.786 | |
| Primary disease | 0.017 | |||
| Pancreatic cancer | 21 (55%) | 39 (81%) | ||
| Others | 17 (45%) | 9 (19%) | ||
| Tumor status | 0.813 | |||
| Locally advanced | 10 (26%) | 14 (29%) | ||
| Metastatic/recurrent | 28 (74%) | 34 (71%) | ||
| Duodenal invasion | 5 (13%) | 5 (10%) | 0.744 | |
| Co-existing duodenal stent | 3 (8%) | 0 | 0.082 | |
| Moderate to severe ascites | 0 | 2 (4%) | 0.501 | |
| Peritoneal dissemination | 9 (24%) | 9 (19%) | 0.603 | |
| Tumor invasion of the main pancreatic duct | 7 (18%) | 34 (71%) | <0.001 | |
| Post-cholecystectomy | 5 (13%) | 1 (2%) | 0.083 | |
| Tumor invasion of the cystic duct orifice * | 7 (18%) | 8 (17%) | >0.999 | |
| History of endoscopic biliary drainage before SEMS placement | 34 (89%) | 38 (79%) | 0.248 | |
| Stent diameter, mm | 6–8/10 | 2 (5%)/36 (95%) | 0/48 (100%) | 0.192 |
| Stent length, cm | 3–5/6–8 | 34 (89%)/4 (11%) | 1 (2%)/47 (98%) | <0.001 |
| Stent type | ||||
| HANAROSTENT Biliary | 10 (26%) | 35 (73%) | <0.001 | |
| Evolution biliary Controlled release Stent—fully covered | 2 (5%) | 7 (15%) | 0.288 | |
| Niti-S SUPREMO stent | 5 (13%) | 4 (8%) | 0.500 | |
| EGIS biliary stent | 0 | 1 (2%) | >0.999 | |
| BONASTENT M-Intraductal | 21 (55%) | 1 (2%) | <0.001 | |
| Endoscopic sphincterotomy | 25 (66%) | 47 (98%) | <0.001 | |
| Chemotherapy after SEMS | 32 (84%) | 40 (83%) | >0.999 | |
| Above the Papilla n = 38 | Across the Papilla n = 48 | p Value | |
|---|---|---|---|
| Technical success | 38 (100%) | 48 (100%) | >0.999 |
| Clinical success | 36 (95%) | 48 (100%) | 0.501 |
| Adverse events | 4 (11%) | 11 (23%) | 0.161 |
| Pancreatitis | 1 (3%) | 6 (13%) | 0.127 |
| Mild/moderate/severe | 0/0/1 | 1/3/2 | |
| Cholecystitis | 3 (8%) | 3 (6%) | >0.999 |
| Mild/moderate/severe | 2/1/0 | 2/1/0 | |
| Non-occlusion cholangitis | 0 | 2 (4%) | 0.501 |
| Mild/moderate/severe | 0/0/0 | 1/0/1 | |
| Recurrent biliary obstruction | 9 (24%) | 21 (44%) | 0.069 |
| Causes of recurrent biliary obstruction | |||
| Occlusion | 7 (18%) | 14 (29%) | 0.316 |
| Sludge | 5 (13%) | 12 (25%) | 0.275 |
| Tumor ingrowth | 0 | 0 | >0.999 |
| Tumor overgrowth | 2 (5%) | 2 (4%) | >0.999 |
| Migration | 1 (3%) | 5 (10%) | 0.222 |
| Inward migration | 1 (3%) | 1 (2%) | >0.999 |
| Outward migration | 0 | 4 (8%) | 0.126 |
| Non-occlusion cholangitis | 0 | 1 (2%) | >0.999 |
| Kinking | 1 (3%) | 1 (2%) | >0.999 |
| Pancreatic Cancer | Non-Pancreatic Cancer | |||||
|---|---|---|---|---|---|---|
| Above the Papilla n = 21 | Across the Papilla n = 39 | p Value | Above the Papilla n = 17 | Across the Papilla n = 9 | p Value | |
| Technical success | 21 (100%) | 39 (100%) | >0.999 | 17 (100%) | 9 (100%) | >0.999 |
| Clinical success | 19 (90%) | 39 (100%) | 0.537 | 17 (100%) | 9 (100%) | >0.999 |
| Adverse events | 3 (14%) | 7 (18%) | >0.999 | 1 (6%) | 4 (44%) | 0.035 |
| Pancreatitis | 1 (5%) | 4 (10%) | 0.649 | 0 | 2 (22%) | 0.111 |
| Mild/moderate/severe | 0/0/1 | 1/1/2 | 0/0/0 | 0/2/0 | ||
| Cholecystitis | 2 (10%) | 2 (5%) | 0.606 | 1 (6%) | 1 (11%) | >0.999 |
| Mild/moderate/severe | 1/1/0 | 1/1/0 | 1/0/0 | 1/0/0 | ||
| Non-occlusion cholangitis | 0 | 1 (3%) | >0.999 | 0 | 1 (11%) | 0.346 |
| Mild/moderate/severe | 0/0/0 | 0/0/1 | 0/0/0 | 1/0/0 | ||
| RBO | 5 (24%) | 17 (44%) | 0.166 | 4 (24%) | 4 (44%) | 0.382 |
| Causes of RBO | ||||||
| Occlusion | 3 (14%) | 10 (26%) | 0.512 | 4 (24%) | 4 (44%) | 0.382 |
| Sludge | 3 (14%) | 8 (21%) | 0.731 | 2 (12%) | 4 (44%) | 0.138 |
| Tumor ingrowth | 0 | 0 | >0.999 | 0 | 0 | >0.999 |
| Tumor overgrowth | 0 | 2 (5%) | 0.537 | 2 (12%) | 0 | 0.529 |
| Migration | 1 (5%) | 5 (13%) | 0.412 | 0 | 0 | >0.999 |
| Inward migration | 1 (5%) | 1 (3%) | >0.999 | 0 | 0 | >0.999 |
| Outward migration | 0 | 4 (10%) | 0.287 | 0 | 0 | >0.999 |
| Non-occlusion cholangitis | 0 | 1 (3%) | >0.999 | 0 | 0 | >0.999 |
| Kinking | 1 (5%) | 1 (3%) | >0.999 | 0 | 0 | >0.999 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamada, M.; Takeda, T.; Sasaki, T.; Okamoto, T.; Hamada, T.; Ishitsuka, T.; Nakagawa, H.; Mie, T.; Furukawa, T.; Kasuga, A.; et al. Outcomes of Intraductal Placement of Covered Metal Stents for Unresectable Distal Malignant Biliary Obstruction. J. Clin. Med. 2023, 12, 2001. https://doi.org/10.3390/jcm12052001
Yamada M, Takeda T, Sasaki T, Okamoto T, Hamada T, Ishitsuka T, Nakagawa H, Mie T, Furukawa T, Kasuga A, et al. Outcomes of Intraductal Placement of Covered Metal Stents for Unresectable Distal Malignant Biliary Obstruction. Journal of Clinical Medicine. 2023; 12(5):2001. https://doi.org/10.3390/jcm12052001
Chicago/Turabian StyleYamada, Manabu, Tsuyoshi Takeda, Takashi Sasaki, Takeshi Okamoto, Tsuyoshi Hamada, Takahiro Ishitsuka, Hiroki Nakagawa, Takafumi Mie, Takaaki Furukawa, Akiyoshi Kasuga, and et al. 2023. "Outcomes of Intraductal Placement of Covered Metal Stents for Unresectable Distal Malignant Biliary Obstruction" Journal of Clinical Medicine 12, no. 5: 2001. https://doi.org/10.3390/jcm12052001
APA StyleYamada, M., Takeda, T., Sasaki, T., Okamoto, T., Hamada, T., Ishitsuka, T., Nakagawa, H., Mie, T., Furukawa, T., Kasuga, A., Matsuyama, M., Ozaka, M., Kobara, H., Masaki, T., & Sasahira, N. (2023). Outcomes of Intraductal Placement of Covered Metal Stents for Unresectable Distal Malignant Biliary Obstruction. Journal of Clinical Medicine, 12(5), 2001. https://doi.org/10.3390/jcm12052001









