Stress Experience, Depression and Neck Disability in Patients with Temporomandibular Disorder—Myofascial Pain with Referral
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
- Inclusion criteria:
- Myofascial pain with referral with respect to I axis of DC/TMD;
- Self-reported pain of at least 8 points according to VAS (Visual Analogue Scale) within craniofacial and/or craniomandibular area;
- Complete natural dentition (Angle’s Molar Classification and Canine Position—Class I);
- Lack of orthodontic history or retention status over 3 years after the completion of treatment.
- Exclusion criteria:
- Any craniofacial and/or craniomandibular trauma (e.g., fractures, whiplash injury);
- Surgical treatment within the craniofacial and/or craniomandibular area (e.g., any orthognathic surgery, third molar extraction within the last year before examination, any previous cancer treatments, any botulinum toxin injection for masticatory muscles, any arthrocentesis of temporomandibular joint);
- Any occlusal splint therapy;
- Any prosthetic treatment;
- Any physiotherapy within the craniofacial and/or craniomandibular region;
- Any diseases which possible health concerns could affect the functioning of the masticatory muscles (e.g., hypothyroidism and hyperthyroidism, epilepsy, myopathy, muscular dystrophy, amyotrophic lateral sclerosis, multiple sclerosis);
- Any metabolic diseases (e.g., diabetes, osteopenia/osteoporosis, disorders of calcium and phosphorus metabolism);
- Chronic medication intake (in the past and at present).
2.2. Questionnaires
- Perceived Stress Scale (PSS−10);
- Beck Depression Inventory (BDI);
- Neck Disability Index (NDI).
2.3. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations of the Study
5. Conclusions
- Stress and depression, as well as neck disability coexist with temporomandibular disorder—myofascial pain with referral. Depression and neck disability appear to be significant predictors of perceived stress levels.
- The hypothesis that there are gender-related differences in prevalence of depression, neck disability, and the severity of stress has not been confirmed. Due to the small sample size, this cannot be excluded.
- In order to complete the biopsychosocial model of temporomandibular disorders, further studies on the detailed assessment of allostatic load as well as cervical spine disorders are necessary.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Réus, J.C.; Polmann, H.; Souza, B.D.M.; Flores-Mir, C.; Gonçalves, D.A.G.; de Queiroz, L.P.; Okeson, J.; Canto, G.D.L. Association between primary headaches and temporomandibular disorders: A systematic review and meta-analysis. J. Am. Dent. Assoc. 2022, 153, 120–131.e126. [Google Scholar] [CrossRef] [PubMed]
- Valesan, L.F.; Da-Cas, C.D.; Réus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Jin, L.; Lamster, I.; Greenspan, J.; Pitts, N.; Scully, C.; Warnakulasuriya, S. Global burden of oral diseases: Emerging concepts, management and interplay with systemic health. Oral Dis. 2016, 22, 609–619. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, F.R.; Barros, R.Q.; Gonçalves, A.S.; Freitas, P.M. Photobiomodulation therapy on the palliative care of temporomandibular disorder and orofacial/cervical skull pain: Study protocol for a randomized controlled clinical trial. Trials 2019, 20, 200. [Google Scholar] [CrossRef]
- Doetzer, A.D.; Herai, R.H.; Buzalaf, M.A.R.; Trevilatto, P.C. Proteomic expression profile in human temporomandibular joint dysfunction. Diagnostics 2021, 11, 601. [Google Scholar] [CrossRef]
- Shakouri, S.K.; Dolatkhah, N.; Omidbakhsh, S.; Pishgahi, A.; Hashemian, M. Serum inflammatory and oxidative stress biomarkers levels are associated with pain intensity, pressure pain threshold and quality of life in myofascial pain syndrome. BMC Res. Notes 2020, 13, 510. [Google Scholar] [CrossRef]
- Golanska, P.; Saczuk, K.; Domarecka, M.; Kuć, J.; Lukomska-Szymanska, M. Temporomandibular Myofascial Pain Syndrome—Aetiology and Biopsychosocial Modulation. A Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 7807. [Google Scholar] [CrossRef]
- Fernández-de-Las-Peñas, C.; Svensson, P. Myofascial temporomandibular disorder. Curr. Rheumatol. Rev. 2016, 12, 40–54. [Google Scholar] [CrossRef] [PubMed]
- Deregibus, A.; Ferrillo, M.; Piancino, M.G.; Domini, M.C.; de Sire, A.; Castroflorio, T. Are occlusal splints effective in reducing myofascial pain in patients with muscle-related temporomandibular disorders? A randomized-controlled trial. Turk. J. Phys. Med. Rehabil. 2021, 67, 32. [Google Scholar] [CrossRef]
- Peck, C.C.; Goulet, J.P.; Lobbezoo, F.; Schiffman, E.L.; Alstergren, P.; Anderson, G.C.; de Leeuw, R.; Jensen, R.; Michelotti, A.; Ohrbach, R. Expanding the taxonomy of the diagnostic criteria for temporomandibular disorders. J. Oral Rehabil. 2014, 41, 2–23. [Google Scholar] [CrossRef] [PubMed]
- Dutra Dias, H.; Botelho, A.L.; Bortoloti, R.; Dos Reis, A.C. Neuroscience contributes to the understanding of the neurobiology of temporomandibular disorders associated with stress and anxiety. CRANIO® 2021, 1–6. [Google Scholar] [CrossRef]
- Noma, N.; Watanabe, Y.; Shimada, A.; Usuda, S.; Iida, T.; Shimada, A.; Tanaka, Y.; Oono, Y.; Sasaki, K. Effects of cognitive behavioral therapy on orofacial pain conditions. J. Oral Sci. 2021, 63, 4–7. [Google Scholar] [CrossRef] [PubMed]
- Penlington, C.; Bowes, C.; Taylor, G.; Otemade, A.A.; Waterhouse, P.; Durham, J.; Ohrbach, R. Psychological therapies for temporomandibular disorders (TMDs). Cochrane Database Syst. Rev. 2022, 8, CD013515. [Google Scholar] [CrossRef] [PubMed]
- Ferrillo, M.; Marotta, N.; Giudice, A.; Calafiore, D.; Curci, C.; Fortunato, L.; Ammendolia, A.; de Sire, A. Effects of occlusal splints on spinal posture in patients with temporomandibular disorders: A systematic review. Proc. Healthc. 2022, 10, 739. [Google Scholar] [CrossRef] [PubMed]
- Lövgren, A.; Visscher, C.; Lobbezo, F.; Yekkalam, N.; Vallin, S.; Wänman, A.; Häggman-Henrikson, B. The association between myofascial orofacial pain with and without referral and widespread pain. Acta Odontol. Scand. 2022, 80, 481–486. [Google Scholar] [CrossRef]
- Ohrbach, R.; Sharma, S.; Fillingim, R.B.; Greenspan, J.D.; Rosen, J.D.; Slade, G.D. Clinical characteristics of pain among five chronic overlapping pain conditions. J. Oral Facial Pain Headache 2020, 34, s29–s42. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Nikolaidis, P.T.; Knechtle, B.; Ruisoto, P. Psychophysiology of Stress. Front. Psychol. 2022, 13, 896773. [Google Scholar] [CrossRef]
- Ulrich-Lai, Y.M.; Herman, J.P. Neural regulation of endocrine and autonomic stress responses. Nat. Rev. Neurosci. 2009, 10, 397–409. [Google Scholar] [CrossRef]
- Benazzi, F. Various forms of depression. Dialogues Clin. Neurosci. 2006, 8, 151–161. [Google Scholar] [CrossRef]
- Paykel, E.S. Basic concepts of depression. Dialogues Clin. Neurosci. 2008, 10, 279–289. [Google Scholar] [CrossRef]
- Kazeminasab, S.; Nejadghaderi, S.A.; Amiri, P.; Pourfathi, H.; Araj-Khodaei, M.; Sullman, M.J.; Kolahi, A.-A.; Safiri, S. Neck pain: Global epidemiology, trends and risk factors. BMC Musculoskelet. Disord. 2022, 23, 26. [Google Scholar] [CrossRef]
- Xie, Y.; Jun, D.; Thomas, L.; Coombes, B.K.; Johnston, V. Comparing central pain processing in individuals with non-traumatic neck pain and healthy individuals: A systematic review and meta-analysis. J. Pain 2020, 21, 1101–1124. [Google Scholar] [CrossRef]
- Jennings, E.M.; Okine, B.N.; Roche, M.; Finn, D.P. Stress-induced hyperalgesia. Prog. Neurobiol. 2014, 121, 1–18. [Google Scholar] [CrossRef]
- Garrigós-Pedrón, M.; La Touche, R.; Navarro-Desentre, P.; Gracia-Naya, M.; Segura-Ortí, E. Widespread mechanical pain hypersensitivity in patients with chronic migraine and temporomandibular disorders: Relationship and correlation between psychological and sensorimotor variables. Acta Odontol. Scand. 2019, 77, 224–231. [Google Scholar] [CrossRef]
- Ferrillo, M.; Migliario, M.; Marotta, N.; Fortunato, F.; Bindi, M.; Pezzotti, F.; Ammendolia, A.; Giudice, A.; Foglio Bonda, P.L.; de Sire, A. Temporomandibular disorders and neck pain in primary headache patients: A retrospective machine learning study. Acta Odontol. Scand. 2022, 81, 151–157. [Google Scholar] [CrossRef]
- Kuć, J.; Szarejko, K.D.; Gołȩbiewska, M. Smiling, Yawning, Jaw Functional Limitations and Oral Behaviors With Respect to General Health Status in Patients With Temporomandibular Disorder—Myofascial Pain With Referral. Front. Neurol. 2021, 12, 646293. [Google Scholar] [CrossRef]
- Vale Braido, G.V.d.; Svensson, P.; dos Santos Proença, J.; Mercante, F.G.; Fernandes, G.; de Godoi Gonçalves, D.A. Are central sensitization symptoms and psychosocial alterations interfering in the association between painful TMD, migraine, and headache attributed to TMD? Clin. Oral Investig. 2022, 27, 681–690. [Google Scholar] [CrossRef]
- Ferrillo, M.; Giudice, A.; Marotta, N.; Fortunato, F.; Di Venere, D.; Ammendolia, A.; Fiore, P.; de Sire, A. Pain Management and Rehabilitation for Central Sensitization in Temporomandibular Disorders: A Comprehensive Review. Int. J. Mol. Sci. 2022, 23, 12164. [Google Scholar] [CrossRef]
- Ohrbach, R.; Gonzalez, Y.; List, T.; Michelotti, A.; Schiffman, E. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) Clinical Examination Protocol. 2013. Available online: www.rdc-tmdinternational.org (accessed on 2 June 2013).
- Kuć, J.; Szarejko, K.D.; Gołębiewska, M. Evaluation of Soft Tissue Mobilization in Patients with Temporomandibular Disorder-Myofascial Pain with Referral. Int. J. Environ. Res. Public Health 2020, 17, 9576. [Google Scholar] [CrossRef]
- Kuć, J.; Szarejko, K.D.; Gołębiewska, M. Comparative Evaluation of Occlusion before and after Soft Tissue Mobilization in Patients with Temporomandibular Disorder—Myofascial Pain with Referral. Int. J. Environ. Res. Public Health 2021, 18, 6568. [Google Scholar] [CrossRef]
- Kuć, J.; Szarejko, K.D.; Gołębiewska, M. The prevalence and overlaps of temporomandibular disorders in patients with myofascial pain with referral—A pilot study. Int. J. Environ. Res. Public Health 2021, 18, 9842. [Google Scholar] [CrossRef]
- Kuć, J.; Szarejko, K.D.; Sierpinska, T. Evaluation of Orofacial and General Pain Location in Patients With Temporomandibular Joint Disorder-Myofascial Pain With Referral. Front. Neurol. 2019, 10, 546. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef]
- Young, I.A.; Dunning, J.; Butts, R.; Cleland, J.A.; Fernández-de-Las-Peñas, C. Psychometric properties of the Numeric Pain Rating Scale and Neck Disability Index in patients with cervicogenic headache. Cephalalgia 2019, 39, 44–51. [Google Scholar] [CrossRef]
- Dawson, A.; Stensson, N.; Ghafouri, B.; Gerdle, B.; List, T.; Svensson, P.; Ernberg, M. Dopamine in plasma–a biomarker for myofascial TMD pain? J. Headache Pain 2016, 17, 65. [Google Scholar] [CrossRef]
- Salameh, E.; Alshaarani, F.; Abou Hamed, H.; Abou Nassar, J. Investigation of the relationship between psychosocial stress and temporomandibular disorder in adults by measuring salivary cortisol concentration: A case-control study. J. Indian Prosthodont. Soc. 2015, 15, 148. [Google Scholar] [CrossRef]
- Zieliński, G.; Ginszt, M.; Zawadka, M.; Rutkowska, K.; Podstawka, Z.; Szkutnik, J.; Majcher, P.; Gawda, P. The relationship between stress and masticatory muscle activity in female students. J. Clin. Med. 2021, 10, 3459. [Google Scholar] [CrossRef]
- Anna, S.; Joanna, K.; Teresa, S.; Maria, G.; Aneta, W. The influence of emotional state on the masticatory muscles function in the group of young healthy adults. BioMed Res. Int. 2015, 2015, 174013. [Google Scholar] [CrossRef]
- McEwen, B.S. Protective and damaging effects of stress mediators. N. Engl. J. Med. 1998, 338, 171–179. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S.; Stellar, E. Stress and the individual: Mechanisms leading to disease. Arch. Intern. Med. 1993, 153, 2093–2101. [Google Scholar] [CrossRef] [PubMed]
- Siew, R.V.K.; Bowe, S.J.; Turner, A.I.; Sarnyai, Z.; Nilsson, C.J.; Shaw, J.E.; Magliano, D.J.; Torres, S.J. The role of combined modifiable lifestyle behaviors in the longitudinal association between stressful life events and allostatic load in Australian adults. Psychoneuroendocrinology 2023, 149, 106021. [Google Scholar] [CrossRef] [PubMed]
- Siew, R.V.K.; Nabe-Nielsen, K.; Turner, A.I.; Bujtor, M.; Torres, S.J. The role of combined modifiable lifestyle behaviors in the association between exposure to stressors and allostatic load: A systematic review of observational studies. Psychoneuroendocrinology 2022, 138, 105668. [Google Scholar] [CrossRef]
- Obeng-Gyasi, E.; Ferguson, A.C.; Stamatakis, K.A.; Province, M.A. Combined effect of lead exposure and allostatic load on cardiovascular disease mortality—A preliminary study. Int. J. Environ. Res. Public Health 2021, 18, 6879. [Google Scholar] [CrossRef]
- Christensen, D.S.; Zachariae, R.; Amidi, A.; Wu, L.M. Sleep and allostatic load: A systematic review and meta-analysis. Sleep Med. Rev. 2022, 64, 101650. [Google Scholar] [CrossRef]
- Parker, H.W.; Abreu, A.M.; Sullivan, M.C.; Vadiveloo, M.K. Allostatic Load and Mortality: A Systematic Review and Meta-Analysis. Am. J. Prev. Med. 2022, 63, 131–140. [Google Scholar] [CrossRef]
- De Felice, F.G.; Gonçalves, R.A.; Ferreira, S.T. Impaired insulin signalling and allostatic load in Alzheimer disease. Nat. Rev. Neurosci. 2022, 23, 215–230. [Google Scholar] [CrossRef]
- Honkalampi, K.; Virtanen, M.; Hintsa, T.; Ruusunen, A.; Mäntyselkä, P.; Ali-Sisto, T.; Kärkkäinen, O.; Koivumaa-Honkanen, H.; Valkonen-Korhonen, M.; Panayiotou, G. Comparison of the level of allostatic load between patients with major depression and the general population. J. Psychosom. Res. 2021, 143, 110389. [Google Scholar] [CrossRef]
- De Miguel, Z.; Khoury, N.; Betley, M.J.; Lehallier, B.; Willoughby, D.; Olsson, N.; Yang, A.C.; Hahn, O.; Lu, N.; Vest, R.T. Exercise plasma boosts memory and dampens brain inflammation via clusterin. Nature 2021, 600, 494–499. [Google Scholar] [CrossRef]
- Kandola, A.; Ashdown-Franks, G.; Hendrikse, J.; Sabiston, C.M.; Stubbs, B. Physical activity and depression: Towards understanding the antidepressant mechanisms of physical activity. Neurosci. Biobehav. Rev. 2019, 107, 525–539. [Google Scholar] [CrossRef] [PubMed]
- Schultchen, D.; Reichenberger, J.; Mittl, T.; Weh, T.R.; Smyth, J.M.; Blechert, J.; Pollatos, O. Bidirectional relationship of stress and affect with physical activity and healthy eating. Br. J. Health Psychol. 2019, 24, 315–333. [Google Scholar] [CrossRef] [PubMed]
- Wallden, M.; Nijs, J. Before & beyond the pain–Allostatic load, central sensitivity and their role in health and function. J. Bodyw. Mov. Ther. 2021, 27, 388–392. [Google Scholar] [CrossRef] [PubMed]
- Lohr, J.B.; Chang, H.; Sexton, M.; Palmer, B.W. Allostatic load and the cannabinoid system: Implications for the treatment of physiological abnormalities in post-traumatic stress disorder (PTSD). CNS Spectr. 2020, 25, 743–749. [Google Scholar] [CrossRef]
- Knibbe, W.; Lobbezoo, F.; Voorendonk, E.M.; Visscher, C.M.; de Jongh, A. Prevalence of painful temporomandibular disorders, awake bruxism and sleep bruxism among patients with severe post-traumatic stress disorder. J. Oral Rehabil. 2022, 49, 1031–1040. [Google Scholar] [CrossRef]
- Perlman, G.; Cogo-Moreira, H.; Wu, C.-Y.; Herrmann, N.; Swardfager, W. Depression interacts with allostatic load to predict cognitive decline in middle age. Psychoneuroendocrinology 2022, 146, 105922. [Google Scholar] [CrossRef]
- Perini, G.; Cotta Ramusino, M.; Sinforiani, E.; Bernini, S.; Petrachi, R.; Costa, A. Cognitive impairment in depression: Recent advances and novel treatments. Neuropsychiatr. Dis. Treat. 2019, 15, 1249–1258. [Google Scholar] [CrossRef]
- Formánek, T.; Csajbók, Z.; Wolfová, K.; Kučera, M.; Tom, S.; Aarsland, D.; Cermakova, P. Trajectories of depressive symptoms and associated patterns of cognitive decline. Sci. Rep. 2020, 10, 20888. [Google Scholar] [CrossRef]
- Verdelho, A.; Madureira, S.; Moleiro, C.; Ferro, J.M.; O’Brien, J.T.; Poggesi, A.; Pantoni, L.; Fazekas, F.; Scheltens, P.; Waldemar, G. Depressive symptoms predict cognitive decline and dementia in older people independently of cerebral white matter changes: The LADIS study. J. Neurol. Neurosurg. Psychiatry 2013, 84, 1250–1254. [Google Scholar] [CrossRef]
- Gębska, M.; Dalewski, B.; Pałka, Ł.; Kołodziej, Ł.; Sobolewska, E. The importance of type d personality in the development of temporomandibular disorders (TMDs) and depression in students during the COVID-19 pandemic. Brain Sci. 2022, 12, 28. [Google Scholar] [CrossRef]
- Uher, J. Personality psychology: Lexical approaches, assessment methods, and trait concepts reveal only half of the story—Why it is time for a paradigm shift. Integr. Psychol. Behav. Sci. 2013, 47, 1–55. [Google Scholar] [CrossRef] [PubMed]
- Kindler, S.; Samietz, S.; Houshmand, M.; Grabe, H.J.; Bernhardt, O.; Biffar, R.; Kocher, T.; Meyer, G.; Völzke, H.; Metelmann, H.-R. Depressive and anxiety symptoms as risk factors for temporomandibular joint pain: A prospective cohort study in the general population. J. Pain 2012, 13, 1188–1197. [Google Scholar] [CrossRef] [PubMed]
- Stocka, A.; Sierpinska, T.; Kuc, J.; Golebiewska, M. Relationship between depression and masticatory muscles function in a group of adolescents. CRANIO® 2018, 36, 390–395. [Google Scholar] [CrossRef]
- Zieliński, G.; Byś, A.; Ginszt, M.; Baszczowski, M.; Szkutnik, J.; Majcher, P.; Gawda, P. Depression and Resting Masticatory Muscle Activity. J. Clin. Med. 2020, 9, 1097. [Google Scholar] [CrossRef]
- Parel, N.S.; Krishna, P.V.; Gupta, A.; Uthayaseelan, K.; Uthayaseelan, K.; Kadari, M.; Subhan, M.; Kasire, S.P. Depression and Vitamin D: A Peculiar Relationship. Cureus 2022, 14, e24363. [Google Scholar] [CrossRef]
- Ferrillo, M.; Lippi, L.; Giudice, A.; Calafiore, D.; Paolucci, T.; Renò, F.; Migliario, M.; Fortunato, L.; Invernizzi, M.; de Sire, A. Temporomandibular Disorders and Vitamin D Deficiency: What Is the Linkage between These Conditions? A Systematic Review. J. Clin. Med. 2022, 11, 6231. [Google Scholar] [CrossRef]
- Gupta, A.K.; Gupta, R.; Gill, S. Effectiveness of Vitamin D along with Splint therapy in the Vit D deficient patients with Temporomandibular disorder-A Randomized, double-blind, placebo-controlled clinical trial. J. Indian Prosthodont. Soc. 2022, 22, 65–73. [Google Scholar] [CrossRef]
- Palacios, C.; Gonzalez, L. Is vitamin D deficiency a major global public health problem? J. Steroid Biochem. Mol. Biol. 2014, 144, 138–145. [Google Scholar] [CrossRef]
- Marques, A.; Gomez-Baya, D.; Peralta, M.; Frasquilho, D.; Santos, T.; Martins, J.; Ferrari, G.; Gaspar de Matos, M. The effect of muscular strength on depression symptoms in adults: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 5674. [Google Scholar] [CrossRef]
- von Piekartz, H.; Rösner, C.; Batz, A.; Hall, T.; Ballenberger, N. Bruxism, temporomandibular dysfunction and cervical impairments in females–Results from an observational study. Musculoskelet. Sci. Pract. 2020, 45, 102073. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Magee, D. Cervical musculoskeletal impairments and temporomandibular disorders. J. Oral Maxillofac. Res. 2012, 3, e4. [Google Scholar] [CrossRef] [PubMed]
- Bogduk, N. Cervicogenic headache: Anatomic basis and pathophysiologic mechanisms. Curr. Pain Headache Rep. 2001, 5, 382–386. [Google Scholar] [CrossRef] [PubMed]
- Giannakopoulos, N.N.; Hellmann, D.; Schmitter, M.; Krüger, B.; Hauser, T.; Schindler, H.J. Neuromuscular interaction of jaw and neck muscles during jaw clenching. J. Orofac. Pain 2013, 27, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Giannakopoulos, N.; Schindler, H.; Rammelsberg, P.; Eberhard, L.; Schmitter, M.; Hellmann, D. Co-activation of jaw and neck muscles during submaximum clenching in the supine position. Arch. Oral Biol. 2013, 58, 1751–1760. [Google Scholar] [CrossRef] [PubMed]
- von Piekartz, H.; Pudelko, A.; Danzeisen, M.; Hall, T.; Ballenberger, N. Do subjects with acute/subacute temporomandibular disorder have associated cervical impairments: A cross-sectional study. Man. Ther. 2016, 26, 208–215. [Google Scholar] [CrossRef]
- Olivo, S.A.; Fuentes, J.; Major, P.; Warren, S.; Thie, N.; Magee, D. The association between neck disability and jaw disability. J. Oral Rehabil. 2010, 37, 670–679. [Google Scholar] [CrossRef]
- Winocur, E.; Messer, T.; Eli, I.; Emodi-Perlman, A.; Kedem, R.; Reiter, S.; Friedman-Rubin, P. Awake and sleep bruxism among Israeli adolescents. Front. Neurol. 2019, 10, 443. [Google Scholar] [CrossRef]
- Gil-Martinez, A.; Navarro-Fernández, G.; Mangas-Guijarro, M.Á.; Lara-Lara, M.; Lopez-Lopez, A.; Fernandez-Carnero, J.; La Touche, R. Comparison between chronic migraine and temporomandibular disorders in pain-related disability and fear-avoidance behaviors. Pain Med. 2017, 18, 2214–2223. [Google Scholar] [CrossRef]
| Comparison with Respect to Gender | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PSS−10 | Reference Values | Entire Group | Female Group | Male Group | Chi-Squared Test with Yates Correction | Fisher’s Exact Unilateral Test | Sample Size for 80% Test Power | |||
| n = 50 | n = 37 | n = 13 | Chi2 | df | p-Value | p-Value | 1 − β | n | ||
| Low Stress vs. All Others | ||||||||||
| Low stress | 0–13 | 11 (22%) | 8 (22%) | 3 (23%) | 0.079 | 1 | 0.779 | 0.596 | 0.029 | 56410 |
| Moderate stress | 14–26 | 33 (66%) | 24 (65%) | 9 (69%) | ||||||
| High stress | 27–40 | 6 (12%) | 5 (14%) | 1 (8%) | ||||||
| Reference Value | Entire Group n = 50 | Female Group n = 37 | Male Group n = 13 | Mann–Whitney U Test | Sample Size for 80% Test Power | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | ±SD | Me | Mean | ±SD | Me | Mean | ±SD | Me | p-Value | 1 − β | n | ||
| PSS−10 | 0–40 | 18.00 | 6.31 | 17.00 | 18.24 | 6.19 | 17.00 | 17.31 | 6.87 | 19.00 | 0.748 | 0.111 | 1665 |
| Comparison with Respect to Gender | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BDI | Reference Values | Entire Group | Female Group | Male Group | Chi-Squared Test with Yates Correction | Fisher’s Exact Unilateral Test | Sample Size for 80% Test Power | |||
| n = 50 | n = 37 | n = 13 | Chi2 | df | p-Value | p-Value | 1 − β | n | ||
| Normal vs. All Others | ||||||||||
| Normal | 1–10 | 35 (70%) | 27 (73%) | 8 (62%) | 0.178 | 1 | 0.673 | 0.330 | 0.950 | 480 |
| Mild mood disturbance | 11–16 | 9 (18%) | 5 (14%) | 4 (31%) | ||||||
| Borderline clinical depression | 17–20 | 3 (6%) | 3 (8%) | 0 (0%) | ||||||
| Moderate depression | 21–30 | 3 (6%) | 2 (5%) | 1 (8%) | ||||||
| Severe depression | 31–40 | 0 (0%) | 0 (0%) | 0 (0%) | ||||||
| Extreme depression | >40 | 0 (0%) | 0 (0%) | 0 (0%) | ||||||
| Reference Value | Entire Group n = 50 | Female Group n = 37 | Male Group n = 13 | Mann–Whitney U Test | Sample Size for 80% Test Power | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | ±SD | Me | Mean | ±SD | Me | Mean | ±SD | Me | p-Value | 1 − β | n | ||
| BDI | 0–63 | 8.94 | 6.37 | 8.00 | 8.68 | 6.26 | 8.00 | 9.69 | 6.86 | 8.00 | 0.579 | 0.118 | 1430 |
| Comparison with Respect to Gender | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NDI | Reference Values | Entire Group | Female Group | Male Group | Chi-Squared Test with Yates Correction | Fisher’s Exact Unilateral Test | Sample Size for 80% Test Power | |||
| n = 50 | n = 37 | n = 13 | Chi2 | df | p-Value | p-Value | 1 − β | n | ||
| No Disability vs. All Others | ||||||||||
| No disability | 0–4 | 9 (18%) | 7 (19%) | 2 (15%) | 0.018 | 1 | 0.893 | 0.571 | 0.033 | 2970 |
| Mild | 5–14 | 30 (60%) | 22 (59%) | 8 (62%) | ||||||
| Moderate | 15–24 | 10 (20%) | 8 (22%) | 2 (15%) | ||||||
| Severe | 25–34 | 1 (2%) | 0 (0%) | 1 (8%) | ||||||
| Complete | >34 | 0 (0%) | 0 (0%) | 0 (0%) | ||||||
| Reference Value | Entire Group n = 50 | Female Group n = 37 | Male Group n = 13 | Mann–Whitney U test | Sample Size for 80% Test Power | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | ±SD | Me | Mean | ±SD | Me | Mean | ±SD | Me | p-Value | 1 − β | n | ||
| NDI | 0–50 | 10.16 | 6.27 | 9.00 | 9.57 | 5.95 | 9.00 | 11.85 | 7.10 | 12.00 | 0.308 | 0.272 | 280 |
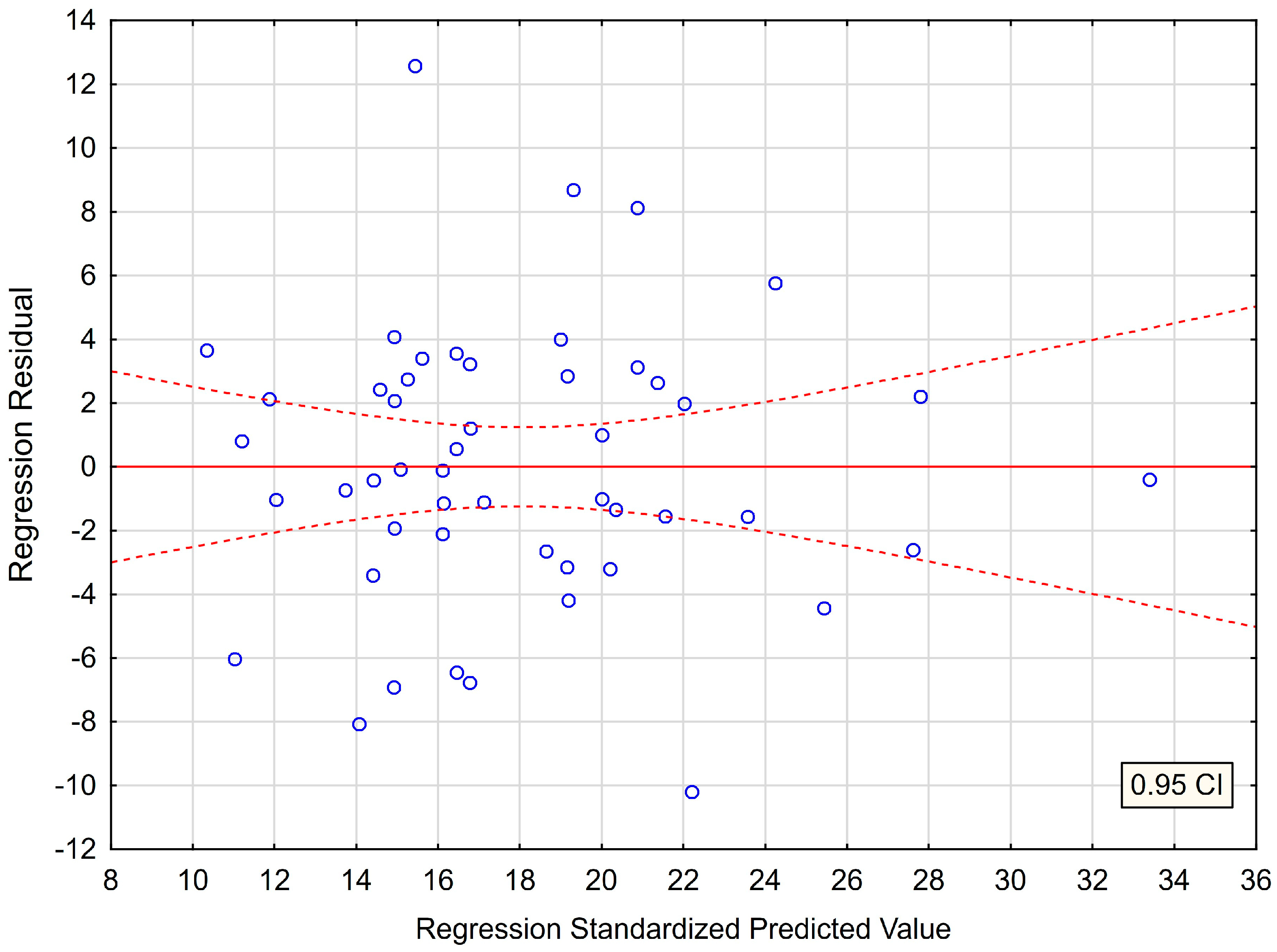
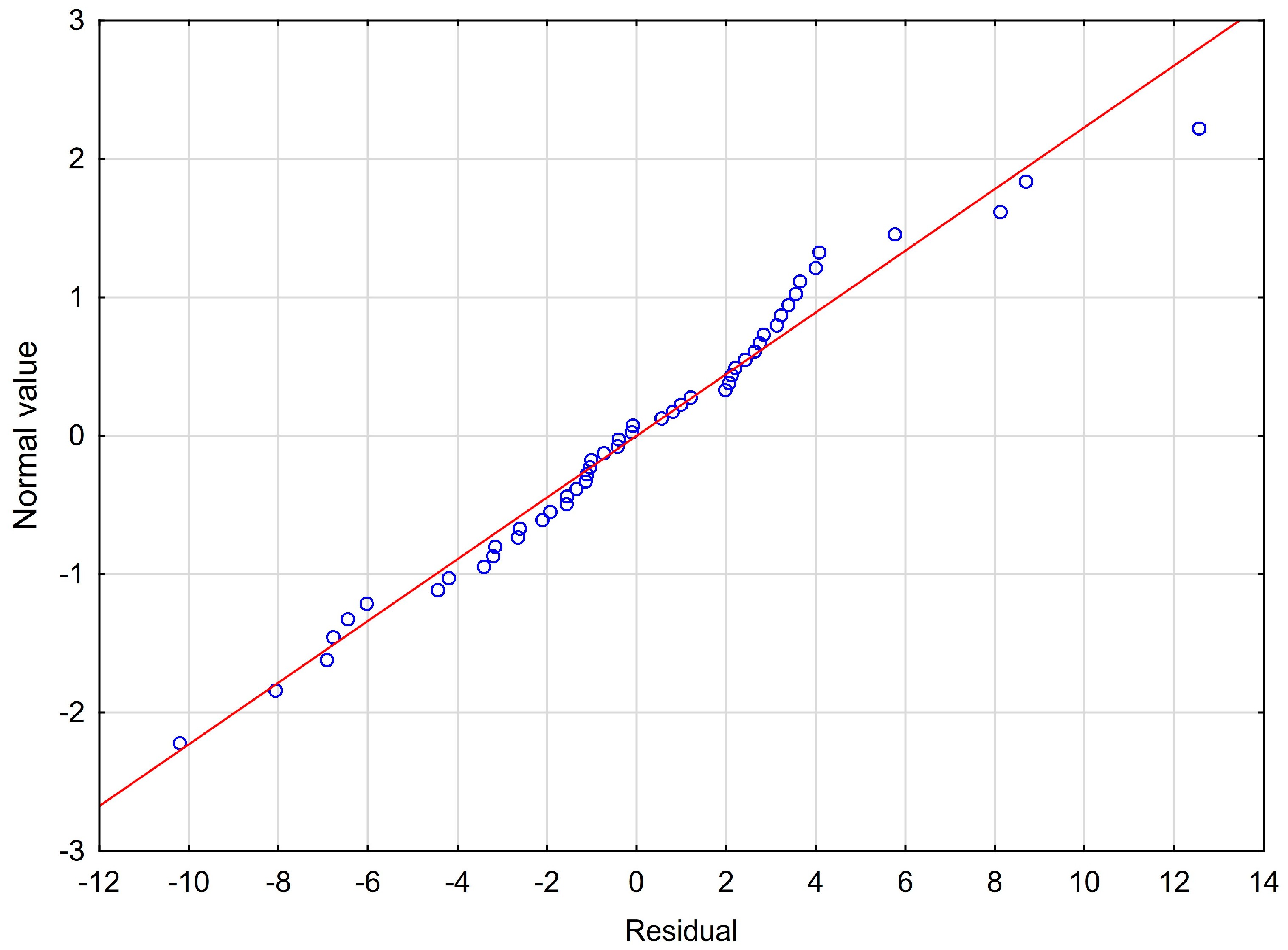
| Regression Coefficient (b) | SE | Standardized Coefficient (β) | t-Value | p-Value | Tolerance Score | R2 Value | Semipartial Correlations (r) | Durbin-Watson Statistic | |
|---|---|---|---|---|---|---|---|---|---|
| Intercept | 10.007 | 1.289 | - | 7.760 | 0.000 * | - | - | - | |
| BDI | 0.507 | 0.111 | 0.511 | 4.573 | 0.000 * | 0.799 | 0.201 | 0.457 | 2.010 |
| NDI | 0.341 | 0.112 | 0.339 | 3.030 | 0.004 * | 0.799 | 0.201 | 0.303 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szarejko, K.D.; Gołębiewska, M.; Lukomska-Szymanska, M.; Kuć, J. Stress Experience, Depression and Neck Disability in Patients with Temporomandibular Disorder—Myofascial Pain with Referral. J. Clin. Med. 2023, 12, 1988. https://doi.org/10.3390/jcm12051988
Szarejko KD, Gołębiewska M, Lukomska-Szymanska M, Kuć J. Stress Experience, Depression and Neck Disability in Patients with Temporomandibular Disorder—Myofascial Pain with Referral. Journal of Clinical Medicine. 2023; 12(5):1988. https://doi.org/10.3390/jcm12051988
Chicago/Turabian StyleSzarejko, Krzysztof Dariusz, Maria Gołębiewska, Monika Lukomska-Szymanska, and Joanna Kuć. 2023. "Stress Experience, Depression and Neck Disability in Patients with Temporomandibular Disorder—Myofascial Pain with Referral" Journal of Clinical Medicine 12, no. 5: 1988. https://doi.org/10.3390/jcm12051988
APA StyleSzarejko, K. D., Gołębiewska, M., Lukomska-Szymanska, M., & Kuć, J. (2023). Stress Experience, Depression and Neck Disability in Patients with Temporomandibular Disorder—Myofascial Pain with Referral. Journal of Clinical Medicine, 12(5), 1988. https://doi.org/10.3390/jcm12051988







