Mental Health and Health-Related Quality of Life in Austrian Adolescents with Chronic Physical Health Conditions: Results from the MHAT Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Recruitment
2.2. Measures
2.2.1. Sociodemographic Information and Chronic Physical Health Conditions (CPHC)
2.2.2. Mental Health Problems
2.2.3. Health-Related Quality of Life (HrQoL)
2.3. Data Analyses
3. Results
3.1. Prevalence of Chronic Physical Health Conditions
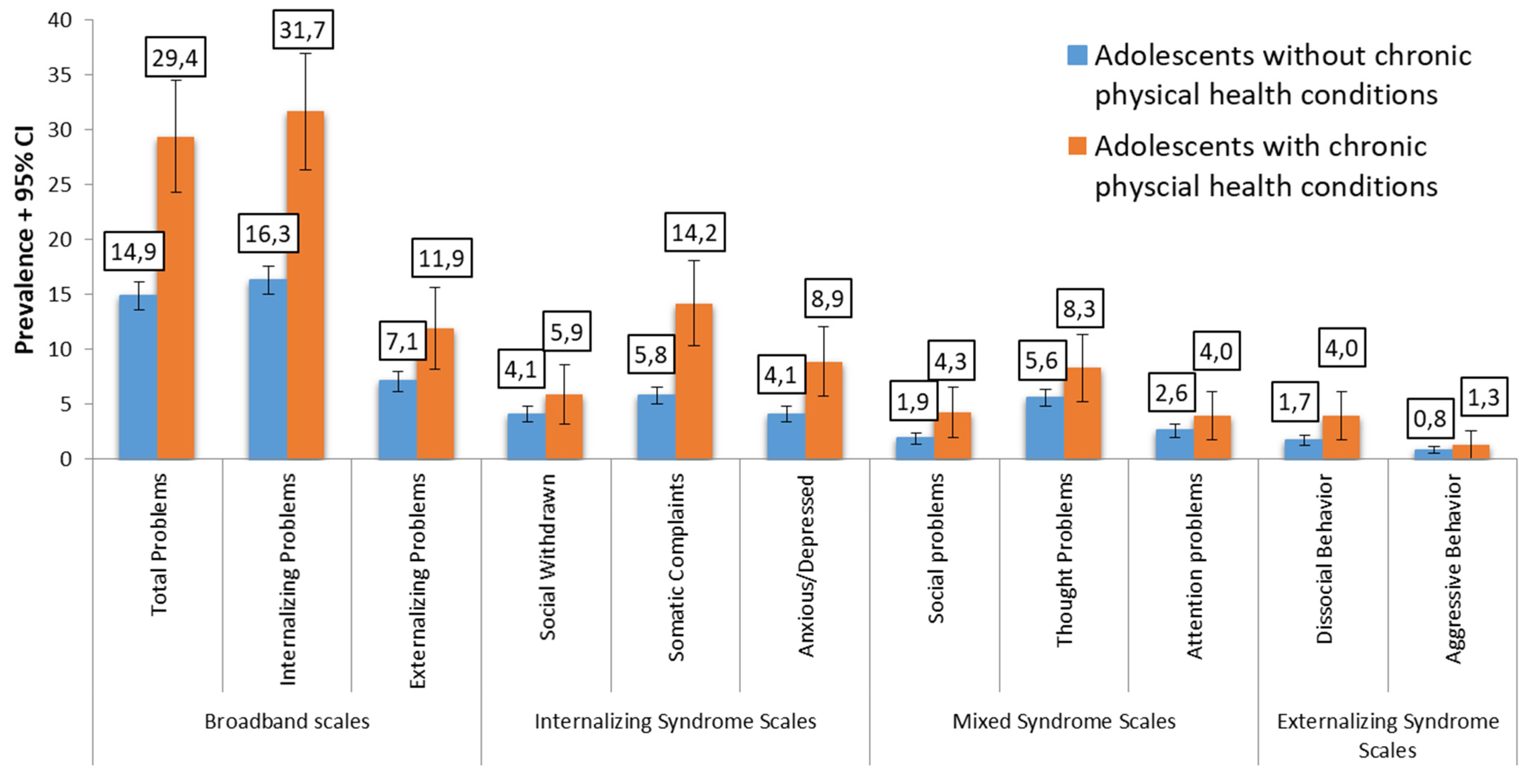
3.2. Prevalence of Mental Health Risk in Adolescents with and without Chronic Physical Health Conditions
3.3. Associated Variables with Mental Health Problems in Chronic Physical Health Conditions
3.4. Health Related Quality of Life in Adolescents with Chronic Physical Health Conditions and Mental Health Problems vs. without Mental Health Problems and Healthy Controls
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Michaud, P.A.; Suris, J.C.; Viner, R. The Adolescent with a Chronic Condition: Epidemiology, Developmental Issues and Health Care Provision; World Health Organization: Geneva, Switzerland, 2007; Available online: https://apps.who.int/iris/handle/10665/43775 (accessed on 31 August 2022).
- Sawyer, S.M.; Drew, S.; Yeo, M.S.; Britto, M.T. Adolescents with a chronic condition: Challenges living, challenges treating. Lancet 2007, 369, 1481–1489. [Google Scholar] [CrossRef] [PubMed]
- Silva, N.; Pereira, M.; Otto, C.; Ravens-Sieberer, U.; Canavarro, M.C.; Bullinger, M. Do 8- to 18-year-old children/adolescents with chronic physical health conditions have worse health-related quality of life than their healthy peers? a meta-analysis of studies using the KIDSCREEN questionnaires. Qual. Life Res. 2019, 28, 1725–1750. [Google Scholar] [CrossRef] [PubMed]
- Laurens, K.R.; Green, M.J.; Dean, K.; Tzoumakis, S.; Harris, F.; Islam, F.; Kariuki, M.; Essery, C.M.; Schofield, J.M.; Carr, V.J. Chronic Physical Health Conditions, Mental Health, and Sources of Support in a Longitudinal Australian Child Population Cohort. J. Pediatr. Psychol. 2019, 44, 1083–1096. [Google Scholar] [CrossRef] [PubMed]
- Felder-Puig, R.; Teutsch, F.; Ramelow, D.; Maier, G. Gesundheit Und Gesundheitsverhalten von Österreichischen Schülerinnen Und Schülern: Ergebnisse Des WHO-HBSC-Survey 2018. 2018. Available online: https://www.sozialministerium.at/dam/jcr:0f4973f8-dc8b-4227-9e64-c76cec64b343/2018%20HBSC-Bericht%20mit%20Alternativtexten_final.pdf (accessed on 31 August 2022).
- Ramelow, D.; Felder-Puig, R. HBSC Factsheet Nr. 07/2013: Die Psychische Gesundheit von Österreichischen Schülerinnen und Schülern: Ergebnisse 2010 und Trends. 2013. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwj50uCK4_D5AhVlXfEDHaMtBngQFnoECA-YQAQ&url=http%3A%2F%2Fwww.wiengs.at%2Ffileadmin%2Fuser_upload%2FFactsheets%2FLBIHPR__2013__Factsheet_Nr7_psychische_Gesundheit.pdf&usg=AOvVaw2Z4gvXv7R89xT8yyNxHnQC (accessed on 31 August 2022).
- Dür, W.; Griebler, R. Die Gesundheit Der Österreichischen SchülerInnen Im Lebenszusammenhang: Ergebnisse Des WHO-HBSC-Survey 2006. 2007. Available online: https://www.sozialministerium.at/dam/jcr:e5e56b2c-b7d5-4f74-99ba-2af4b4101991/bericht_hbsc_2007_gesamt_mit_anhang907.pdf (accessed on 31 August 2022).
- Newacheck, P.W.; Taylor, W.R. Childhood chronic illness: Prevalence, severity, and impact. Am. J. Public Health 1992, 82, 364–371. [Google Scholar] [CrossRef]
- Nibras, S.; Kentor, R.; Masood, Y.; Price, K.; Schneider, N.M.; Tenenbaum, R.B.; Calarge, C. Psychological and Psychiatric Comorbidities in Youth with Serious Physical Illness. Children 2022, 9, 1051. [Google Scholar] [CrossRef]
- Vessey, J.A. Psychological comorbidity in children with chronic conditions. Pediatr. Nurs. 1999, 25, 211–214. [Google Scholar]
- Committee on Children with Disabilities and Committee on Psychosocial Aspects of Child and Family Health Psychosocial risks of chronic health conditions in childhood and adolescence. Pediatrics 1993, 92, 876–878. [CrossRef]
- Delamater, A.M.; Guzman, A.; Aparicio, K. Mental health issues in children and adolescents with chronic illness. Int. J. Hum. Rights Healthc. 2017, 10, 163–173. [Google Scholar] [CrossRef]
- Jones, L.C.; Mrug, S.; Elliott, M.N.; Toomey, S.L.; Tortolero, S.; Schuster, M.A. Chronic Physical Health Conditions and Emotional Problems From Early Adolescence Through Midadolescence. Acad. Pediatr. 2017, 17, 649–655. [Google Scholar] [CrossRef]
- Brady, A.M.; Deighton, J.; Stansfeld, S. Psychiatric outcomes associated with chronic illness in adolescence: A systematic review. J. Adolesc. 2017, 59, 112–123. [Google Scholar] [CrossRef]
- Brady, A.M.; Deighton, J.; Stansfeld, S. Chronic illness in childhood and early adolescence: A longitudinal exploration of co-occurring mental illness. Dev. Psychopathol. 2021, 33, 885–898. [Google Scholar] [CrossRef] [PubMed]
- Määttä, H.; Honkanen, M.; Hurtig, T.; Taanila, A.; Ebeling, H.; Koivumaa-Honkanen, H. Childhood chronic condition and subsequent self-reported internalizing and externalizing problems in adolescence: A birth cohort study. Eur. J. Pediatr. 2022, 181, 3377–3387. [Google Scholar] [CrossRef]
- Pinquart, M.; Shen, Y. Behavior Problems in Children and Adolescents With Chronic Physical Illness: A Meta-Analysis. J. Pediatr. Psychol. 2011, 36, 1003–1016. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, S.; Petersen, C.; Bullinger, M. Coping with chronic disease from the perspective of children and adolescents–A conceptual framework and its implications for participation: Coping with chronic disease. Child Care Health Dev. 2003, 29, 63–75. [Google Scholar] [CrossRef] [PubMed]
- Stein, R.E.; Jessop, D.J. A noncategorical approach to chronic childhood illness. Public Health Rep. 1982, 97, 354–362. [Google Scholar]
- Stam, H.; Hartman, E.E.; Deurloo, J.A.; Groothoff, J.; Grootenhuis, M.A. Young Adult Patients with a History of Pediatric Disease: Impact on Course of Life and Transition into Adulthood. J. Adolesc. Health 2006, 39, 4–13. [Google Scholar] [CrossRef]
- Taylor, R.M.; Gibson, F.; Franck, L.S. The experience of living with a chronic illness during adolescence: A critical review of the literature. J. Clin. Nurs. 2008, 17, 3083–3091. [Google Scholar] [CrossRef]
- Sentenac, M.; Arnaud, C.; Gavin, A.; Molcho, M.; Gabhainn, S.N.; Godeau, E. Peer Victimization Among School-aged Children With Chronic Conditions. Epidemiol. Rev. 2012, 34, 120–128. [Google Scholar] [CrossRef]
- COACH Consortium; Reinauer, C.; Viermann, R.; Förtsch, K.; Linderskamp, H.; Warschburger, P.; Holl, R.W.; Staab, D.; Minden, K.; Muche, R.; et al. Motivational Interviewing as a tool to enhance access to mental health treatment in adolescents with chronic medical conditions and need for psychological support (COACH-MI): Study protocol for a clusterrandomised controlled trial. Trials 2018, 19, 629. [Google Scholar] [CrossRef]
- Reinauer, C.; Platzbecker, A.L.; Viermann, R.; Domhardt, M.; Baumeister, H.; Foertsch, K.; Linderskamp, H.; Krassuski, L.; Staab, D.; Minden, K.; et al. Efficacy of Motivational Interviewing to Improve Utilization of Mental Health Services Among Youths With Chronic Medical Conditions. JAMA Netw. Open 2021, 4, e2127622. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Gosch, A.; Abel, T.; Auquier, P.; Bellach, B.-M.; Bruil, J.; Dür, W.; Power, M.; Rajmil, L. The European KIDSCREEN Group Quality of life in children and adolescents: A European public health perspective. Soz.-Präventivmedizin 2001, 46, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Gaspar, T.; Ribeiro, J.P.; de Matos, M.G.; Leal, I.; Ferreira, A. Health-Related Quality of Life in Children and Adolescents: Subjective Well Being. Span. J. Psychol. 2012, 15, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Berkelbach van der Sprenkel, E.E.; Nijhof, S.L.; Dalmeijer, G.W.; Onland-Moret, N.C.; de Roos, S.A.; Lesscher, H.M.B.; van de Putte, E.M.; van der Ent, C.K.; Finkenauer, C.; Stevens, G.W.J.M. Psychosocial functioning in adolescents growing up with chronic disease: The Dutch HBSC study. Eur. J. Pediatr. 2022, 181, 763–773. [Google Scholar] [CrossRef]
- Wagner, G.; Berger, G.; Sinnreich, U.; Grylli, V.; Schober, E.; Huber, W.-D.; Karwautz, A. Quality of Life in Adolescents With Treated Coeliac Disease: Influence of Compliance and Age at Diagnosis. J. Pediatr. Gastroenterol. Nutr. 2008, 47, 7. [Google Scholar] [CrossRef]
- Zeiler, M.; Peer, S.; Philipp, J.; Truttmann, S.; Wagner, G.; Karwautz, A.; Waldherr, K. Web-Based Versus Paper-Pencil Assessment of Behavioral Problems Using the Youth Self-Report. Eur. J. Psychol. Assess. 2021, 37, 95–103. [Google Scholar] [CrossRef]
- Philipp, J.; Zeiler, M.; Waldherr, K.; Nitsch, M.; Dür, W.; Karwautz, A.; Wagner, G. The Mental Health in Austrian Teenagers (MHAT)-Study: Preliminary results from a pilot study. Neuropsychiatrie 2014, 28, 198–207. [Google Scholar] [CrossRef]
- Zeiler, M.; Wagner, G.; Philipp, J.; Nitsch, M.; Truttmann, S.; Dür, W.; Karwautz, A.; Waldherr, K. The Mental Health in Austrian Teenagers (MHAT) Study: Design, methodology, description of study population. Neuropsychiatrie 2018, 32, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Wagner, G.; Zeiler, M.; Waldherr, K.; Philipp, J.; Truttmann, S.; Dür, W.; Treasure, J.L.; Karwautz, A.F.K. Mental health problems in Austrian adolescents: A nationwide, two-stage epidemiological study applying DSM-5 criteria. Eur. Child Adolesc. Psychiatry 2017, 26, 1483–1499. [Google Scholar] [CrossRef]
- Boyce, W.; Torsheim, T.; Currie, C.; Zambon, A. The Family Affluence Scale as a Measure of National Wealth: Validation of an Adolescent Self-Report Measure. Soc. Indic. Res. 2006, 78, 473–487. [Google Scholar] [CrossRef]
- Achenbach, T.M. Manual for the Youth Self-Report and 1991 Profile; Department of Psychiatry, University of Vermont: Burlington, VT, USA, 1991. [Google Scholar]
- von M. Döpfner, B.; Plück, J.; Bölte, S.; Lenz, K.; Melchers, P. (Eds.) Arbeitsgruppe Deutsche Child Behavior Checklist Fragebogen für Jugendliche. In Deutsche Bearbeitung der Youth Self-Report Form der Child Behavior Checklist (YSR). Einführung und Anleitung zur Handauswertung mit deutschen Normen; (2. Aufl.); Arbeitsgruppe Kinder-, Jugend- und Familiendiagnostik (KJFD): Köln, Germany, 1991. [Google Scholar]
- Rescorla, L.; Ivanova, M.Y.; Achenbach, T.M.; Begovac, I.; Chahed, M.; Drugli, M.B.; Emerich, D.R.; Fung, D.S.S.; Haider, M.; Hansson, K.; et al. International Epidemiology of Child and Adolescent Psychopathology II: Integration and Applications of Dimensional Findings From 44 Societies. J. Am. Acad. Child Adolesc. Psychiatry 2012, 51, 1273–1283.e8. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Gosch, A.; Rajmil, L.; Erhart, M.; Bruil, J.; Power, M.; Duer, W.; Auquier, P.; Cloetta, B.; Czemy, L.; et al. The KIDSCREEN-52 quality of life measure for children and adolescents: Psychometric results from a cross-cultural survey in 13 European countries. Value Health 2008, 11, 645–658. [Google Scholar] [CrossRef] [PubMed]
- Cobham, V.E.; Hickling, A.; Kimball, H.; Thomas, H.J.; Scott, J.G.; Middeldorp, C.M. Systematic Review: Anxiety in Children and Adolescents With Chronic Medical Conditions. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 595–618. [Google Scholar] [CrossRef]
- Tegethoff, M.; Belardi, A.; Stalujanis, E.; Meinlschmidt, G. Association between mental disorders and physical diseases in adolescents from a nationally representative cohort. Psychosom. Med. 2015, 77, 319–332. [Google Scholar] [CrossRef]
- Berger, G.; Waldhoer, T.; Barrientos, I.; Kunkel, D.; Rami-Merhar, B.M.; Schober, E.; Karwautz, A.; Wagner, G. Association of insulin-manipulation and psychiatric disorders: A systematic epidemiological evaluation of adolescents with type 1 diabetes in Austria. Pediatr. Diabetes 2019, 20, 127–136. [Google Scholar] [CrossRef]
- Kline-Simon, A.H.; Weisner, C.; Sterling, S. Point Prevalence of Co-Occurring Behavioral Health Conditions and Associated Chronic Disease Burden Among Adolescents. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 408–414. [Google Scholar] [CrossRef]
- Zheng, K.; Abraham, C.; Bruzzese, J.-M.; Smaldone, A. Longitudinal Relationships Between Depression and Chronic Illness in Adolescents: An Integrative Review. J. Pediatr. Health Care 2020, 34, 333–345. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.B.; Cox, B.J.; Afifi, T.O.; Belik, S.-L.; Sareen, J. Does co-morbid depressive illness magnify the impact of chronic physical illness? A population-based perspective. Psychol. Med. 2006, 36, 587. [Google Scholar] [CrossRef]
- Scott, K.M.; Von Korff, M.; Alonso, J.; Angermeyer, M.C.; Bromet, E.; Fayyad, J.; de Girolamo, G.; Demyttenaere, K.; Gasquet, I.; Gureje, O.; et al. Mental–physical co-morbidity and its relationship with disability: Results from the World Mental Health Surveys. Psychol. Med. 2009, 39, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.; Hiscock, H.; Wurzel, D.; Kao, K.-T.; Freeman, J.L.; Ride, J. Mental healthcare for children with chronic conditions: A qualitative study. Arch. Dis. Child. 2022, 107, 134–140. [Google Scholar] [CrossRef]
- Lunkenheimer, F.; Domhardt, M.; Geirhos, A.; Kilian, R.; Mueller-Stierlin, A.S.; Holl, R.W.; Meissner, T.; Minden, K.; Moshagen, M.; Ranz, R.; et al. Effectiveness and cost-effectiveness of guided Internet- and mobile-based CBT for adolescents and young adults with chronic somatic conditions and comorbid depression and anxiety symptoms (youthCOACHCD): Study protocol for a multicentre randomized controlled trial. Trials 2020, 21, 253. [Google Scholar] [CrossRef]
- Zeiler, M.; Wittek, T.; Graf, T.; Bozic, I.; Nitsch, M.; Waldherr, K.; Karwautz, A.; Wagner, G.; Berger, G. Psychosocial impact of the COVID-19 pandemic for adolescents with type-1-diabetes: A qualitative interview study involving adolescents and parents. Behav. Med. 2022, 48, 101695. [Google Scholar] [CrossRef]
- Jones, B.; Woolfenden, S.; Pengilly, S.; Breen, C.; Cohn, R.; Biviano, L.; Johns, A.; Worth, A.; Lamb, R.; Lingam, R.; et al. COVID-19 pandemic: The impact on vulnerable children and young people in Australia. J. Paediatr. Child Health 2020, 56, 1851–1855. [Google Scholar] [CrossRef]
- Cay, M.; Gonzalez-Heydrich, J.; Teicher, M.H.; van der Heijden, H.; Ongur, D.; Shinn, A.K.; Upadhyay, J. Childhood maltreatment and its role in the development of pain and psychopathology. Lancet Child Adolesc. Health 2022, 6, 195–206. [Google Scholar] [CrossRef]
- Overstreet, C.; Berenz, E.C.; Kendler, K.S.; Dick, D.M.; Amstadter, A.B. Predictors and mental health outcomes of potentially traumatic event exposure. Psychiatry Res. 2017, 247, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Avenevoli, S.; Costello, E.J.; Georgiades, K.; Green, J.G.; Gruber, M.J.; He, J.; Koretz, D.; McLaughlin, K.A.; Petukhova, M.; et al. Prevalence, Persistence, and Sociodemographic Correlates of DSM-IV Disorders in the National Comorbidity Survey Replication Adolescent Supplement. Arch. Gen. Psychiatry 2012, 69, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Yung, A.R. Youth services: The need to integrate mental health, physical health and social care: Commentary on Malla et al.: From early intervention in psychosis to youth mental health reform: A review of the evolution and transformation of mental health services for young people. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 327–329. [Google Scholar] [CrossRef] [PubMed]
- Barlow, J.H.; Ellard, D.R. The psychosocial well-being of children with chronic disease, their parents and siblings: An overview of the research evidence base. Child Care Health Dev. 2006, 32, 19–31. [Google Scholar] [CrossRef]
- Pinquart, M. Self-esteem of children and adolescents with chronic illness: A meta-analysis: Self-esteem and chronic illness. Child Care Health Dev. 2013, 39, 153–161. [Google Scholar] [CrossRef]
- Pinquart, M. Do the Parent–Child Relationship and Parenting Behaviors Differ Between Families With a Child With and Without Chronic Illness? A Meta-Analysis. J. Pediatr. Psychol. 2013, 38, 708–721. [Google Scholar] [CrossRef]
- Philipp, J.; Truttmann, S.; Zeiler, M.; Franta, C.; Wittek, T.; Schöfbeck, G.; Mitterer, M.; Mairhofer, D.; Zanko, A.; Imgart, H.; et al. Reduction of High Expressed Emotion and Treatment Outcomes in Anorexia Nervosa-Caregivers’ and Adolescents’ Perspective. J. Clin. Med. 2020, 9, 2021. [Google Scholar] [CrossRef]
- Delamater, A.M.; de Wit, M.; McDarby, V.; Malik, J.A.; Hilliard, M.E.; Northam, E.; Acerini, C.L. ISPAD Clinical Practice Consensus Guidelines 2018: Psychological care of children and adolescents with type 1 diabetes. Pediatr. Diabetes 2018, 19 (Suppl. S27), 237–249. [Google Scholar] [CrossRef]
- Coburn, S.; Rose, M.; Streisand, R.; Sady, M.; Parker, M.; Suslovic, W.; Weisbrod, V.; Kerzner, B.; Kahn, I. Psychological Needs and Services in a Pediatric Multidisciplinary Celiac Disease Clinic. J. Clin. Psychol. Med. Settings 2020, 27, 433–443. [Google Scholar] [CrossRef] [PubMed]
- James, C.; Corman, H.; Noonan, K.; Reichman, N.E.; Jimenez, M.E. Adolescent Chronic Health Conditions and School Disconnectedness. J. Dev. Behav. Pediatr. JDBP 2022, 43, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Bai, G.; Herten, M.H.; Landgraf, J.M.; Korfage, I.J.; Raat, H. Childhood chronic conditions and health-related quality of life: Findings from a large population-based study. PLoS ONE 2017, 12, e0178539. [Google Scholar] [CrossRef] [PubMed]
- Hölling, H.; Schlack, R.; Dippelhofer, A.; Kurth, B.-M. Personale, familiäre und soziale Schutzfaktoren und gesundheitsbezogene Lebensqualität chronisch kranker Kinder und Jugendlicher. Bundesgesundheitsblatt-Gesundh.-Gesundh. 2008, 51, 606–620. [Google Scholar] [CrossRef]
- Varni, J.W.; Limbers, C.A.; Burwinkle, T.M. Impaired health-related quality of life in children and adolescents with chronic conditions: A comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQLTM 4.0 Generic Core Scales. Health Qual. Life Outcomes 2007, 5, 43. [Google Scholar] [CrossRef]
- The BELLA Study Group; Ravens-Sieberer, U.; Erhart, M.; Wille, N.; Bullinger, M. Health-related quality of life in children and adolescents in Germany: Results of the BELLA study. Eur. Child Adolesc. Psychiatry 2008, 17, 148–156. [Google Scholar] [CrossRef]
- Ferro, M.A.; Lipman, E.L.; Van Lieshout, R.J.; Gorter, J.W.; Shanahan, L.; Boyle, M.; Georgiades, K.; Timmons, B. Multimorbidity in Children and Youth Across the Life-course (MY LIFE): Protocol of a Canadian prospective study. BMJ Open 2019, 9, e034544. [Google Scholar] [CrossRef]
- Danne, T.; Limbert, C. COVID-19, type 1 diabetes, and technology: Why paediatric patients are leading the way. Lancet Diabetes Endocrinol. 2020, 8, 465–467. [Google Scholar] [CrossRef]
| Weighted Prevalence 1 | |||
|---|---|---|---|
| Total (n = 3469) | Boys (n = 1544) | Girls (n = 1925) | |
| Any chronic physical health conditions | 287 (8.3%) | 110 (7.1%) | 182 (9.4%) |
| Diabetes/metabolic disease | 10 (0.3%) | 5 (0.3%) | 5 (0.3%) |
| Hypertension | 2 (0.1%) | 2 (0.1%) | 0 (0.0%) |
| Arthritis/rheumatism | 11 (0.3%) | 2 (0.1%) | 9 (0.5%) |
| Paralysis | 1 (<0.1%) | 1 (0.1%) | 0 (0.0%) |
| Asthma/bronchitis | 65 (1.9%) | 32 (2.1%) | 32 (1.7%) |
| Epilepsy | 5 (0.1%) | 2 (0.2%) | 2 (0.1%) |
| Migraine/headache | 49 (1.4%) | 14 (0.9%) | 37 (1.9%) |
| Orthopedic disease | 65 (1.9%) | 21 (1.3%) | 46 (2.4%) |
| Thyroid disease | 21 (0.6%) | 8 (0.5%) | 12 (0.6%) |
| Cancer/tumor disease | 3 (0.1%) | 1 (0.1%) | 3 (0.1%) |
| Heart disease | 18 (0.5%) | 7 (0.4%) | 12 (0.6%) |
| Enteropathy | 4 (0.1%) | 0 (0.0%) | 4 (0.2%) |
| Allergy 2 | 63 (1.8%) | 27 (1.8%) | 36 (1.9%) |
| Disability | 18 (0.5%) | 8 (0.5%) | 10 (0.5%) |
| Other | 33 (0.9%) | 15 (1.0%) | 18 (0.9%) |
| Adolescent without Chronic Physical Health Conditions (n = 3.170) | Adolescent with Chronic Physical Health Conditions (n = 311) | chi2 (df) | p | |
|---|---|---|---|---|
| Gender | 9.983 (1) | 0.002 | ||
| boys | 1432 (45.3%) | 112 (36.0%) | ||
| girls | 1726 (54.7%) | 199 (64.0%) | ||
| missing | 12 | 0 | ||
| Age group | 18.529 (3) | <0.001 | ||
| 5th grade | 503 (15.9%) | 28 (9.0%) | ||
| 7th grade | 822 (25.9%) | 66 (21.2%) | ||
| 9th grade | 994 (31.4%) | 110 (35.4%) | ||
| 11th grade | 851 (26.8%) | 107 (34.4%) | ||
| Socioeconomic status (SES) | 0.569 (2) | 0.753 | ||
| low SES | 62 (2.0%) | 6 (2.0%) | ||
| medium SES | 772 (25.0%) | 71 (23.1%) | ||
| high SES | 2248 (72.9%) | 230 (74.9%) | ||
| missing | 88 | 4 | ||
| Migration background 1 | 0.237 (1) | 0.626 | ||
| no | 2307 (74.1%) | 230 (75.4%) | ||
| yes | 805 (25.9%) | 75 (24.6%) | ||
| missing | 58 | 6 | ||
| Residency 2 | 2.760 (1) | 0.097 | ||
| urban | 1819 (58.2%) | 193 (63.1%) | ||
| rural | 1308 (41.8%) | 113 (36.9%) | ||
| missing | 43 | 5 | ||
| Family status | 2.137 (2) | 0.343 | ||
| living with both parents | 2293 (74.5%) | 212 (70.9%) | ||
| living with single parent | 506 (16.4%) | 54 (18.1%) | ||
| living in patchwork family | 277 (9.0%) | 33 (11.0%) | ||
| missing | 94 | 12 | ||
| Parental employment | 0.055 (2) | 0.973 | ||
| both parents | 2442 (78.1%) | 239 (78.1%) | ||
| one parent | 598 (19.1%) | 58 (19.0%) | ||
| no parent | 85 (2.7%) | 9 (2.9%) | ||
| missing | 45 | 5 | ||
| Chronic physical health conditions in a parent or sibling | 224.665 (2) | <0.001 | ||
| no | 2397 (76.9%) | 126 (41.4%) | ||
| yes | 392 (12.6%) | 132 (43.4%) | ||
| do not know | 327 (10.5%) | 46 (15.1%) | ||
| missing | 54 | 7 | ||
| Psychiatric disorder in a parent or sibling | 22.470 (2) | <0.001 | ||
| no | 2753 (87.8%) | 237 (78.2%) | ||
| yes | 125 (4.0%) | 22 (7.3%) | ||
| do not know | 257 (8.2%) | 44 (14.5%) | ||
| missing | 35 | 8 | ||
| Self-reported school performance | 8.645 (3) | 0.034 | ||
| very good | 682 (21.9%) | 49 (16.1%) | ||
| good | 1300 (41.7%) | 129 (42.3%) | ||
| mediocre | 1031 (33.1%) | 120 (39.3%) | ||
| below average | 105 (3.4%) | 7 (2.3%) | ||
| missing | 52 | 6 |
| Predictor | b (SE) | Wald | p | Odds Ratio (OR) | OR 95% CI |
|---|---|---|---|---|---|
| Constant | 5.718 | 0.057 | |||
| Psychiatric disorder of parent or sibling (Ref. no) | |||||
| do not know | 0.587 (0.36) | 2.735 | 0.098 | 1.80 | [0.90; 3.61] |
| yes | 0.995 (0.52) | 3.677 | 0.055 | 2.71 | [0.98; 7.48] |
| Any potentially traumatizing life event (Ref. no) | 1.212 (0.39) | 9.914 | 0.002 | 3.36 | [1.58; 7.15] |
| More than one chronic physical health condition (Ref. Single chronic physical health condition) | 0.018 (0.39) | 0.003 | 0.956 | 1.02 | [0.54; 1.92] |
| Needs regular medication intake due to chronic disease (Ref. no) | 0.926 (0.29) | 10.570 | 0.001 | 2.52 | [1.44; 1.41] |
| Mean (SD) | Test Statistic | |||||
|---|---|---|---|---|---|---|
| Healthy Adolescents 1 A | Adolescents with a Chronic Physical Health Condition without Comorbid Mental Health Problems 2 B | Adolescents a Chronic Physical Health Condition and Comorbid Mental Health Problems 3 C | F | p | Tukey Post-Hoc-Tests | |
| KIDSCREEN-10 | 54.34 (8.93) | 51.44 (8.82) | 39.23 (10.85) | 156.495 | <0.001 | A,B > C; A > B |
| Self-Perception | 51.51 (8.55) | 49.88 (9.16) | 40.70 (9.80) | 88.947 | <0.001 | A,B > C; A > B |
| Parent Relation and Home Life | 54.76 (7.94) | 53.35 (8.00) | 44.22 (11.68) | 94.615 | <0.001 | A,B > C |
| Social Support and Peers | 53.66 (8.11) | 52.38 (9.27) | 47.52 (10.63) | 31.798 | <0.001 | A,B > C |
| School Environment | 53.58 (8.66) | 51.61 (8.24) | 44.39 (9.53) | 64.395 | <0.001 | A,B > C; A > B |
| Bullying (Social Acceptance) | 52.74 (7.71) | 53.05 (7.12) | 45.13 (14.06) | 50.143 | <0.001 | A,B > C |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wagner, G.; Karwautz, A.; Philipp, J.; Truttmann, S.; Dür, W.; Waldherr, K.; Berger, G.; Zeiler, M. Mental Health and Health-Related Quality of Life in Austrian Adolescents with Chronic Physical Health Conditions: Results from the MHAT Study. J. Clin. Med. 2023, 12, 1927. https://doi.org/10.3390/jcm12051927
Wagner G, Karwautz A, Philipp J, Truttmann S, Dür W, Waldherr K, Berger G, Zeiler M. Mental Health and Health-Related Quality of Life in Austrian Adolescents with Chronic Physical Health Conditions: Results from the MHAT Study. Journal of Clinical Medicine. 2023; 12(5):1927. https://doi.org/10.3390/jcm12051927
Chicago/Turabian StyleWagner, Gudrun, Andreas Karwautz, Julia Philipp, Stefanie Truttmann, Wolfgang Dür, Karin Waldherr, Gabriele Berger, and Michael Zeiler. 2023. "Mental Health and Health-Related Quality of Life in Austrian Adolescents with Chronic Physical Health Conditions: Results from the MHAT Study" Journal of Clinical Medicine 12, no. 5: 1927. https://doi.org/10.3390/jcm12051927
APA StyleWagner, G., Karwautz, A., Philipp, J., Truttmann, S., Dür, W., Waldherr, K., Berger, G., & Zeiler, M. (2023). Mental Health and Health-Related Quality of Life in Austrian Adolescents with Chronic Physical Health Conditions: Results from the MHAT Study. Journal of Clinical Medicine, 12(5), 1927. https://doi.org/10.3390/jcm12051927








