Initial Evidence for Positive Effects of a Psychological Preparation Program for MRI “iMReady” in Children with Neurofibromatosis Type I and Brain Tumors—How to Meet the Patients’ Needs Best
Abstract
1. Introduction
2. Materials and Methods
2.1. Development and Content of the Training “iMReady”
- (1)
- The primary goal of the first session is the psychological and medical preparation, while also discussing the pros and cons about having the MRI without anesthesia. Hence, in addition to basic information and procedural knowledge about the MRI, instructions regardin appropriate clothing, metal objects, lying still, and the sound of the MRI are discussed with the participants. Role play techniques are used to build and practice coping strategies and action control. To further explore the topic, the children receive instructions for exercises, which they are asked to complete at home together with their parents. The homework is composed of two exercises: building a shoebox-sized paper MRI model (e.g., suitable for LEGO figurines) and continuing the role-play techniques with the paper model (Figure 1).
- (2)
- In session two, the topics of the previous session are repeated before self-instruction and relaxation techniques for children are introduced and practiced. In general, it would be beneficial if MRI companies would build dummy machines for performing the training, in order not to occupy the scanning facilities. Considering available options, children and parents undergo a practice run in a 1.5 Tesla MRI (Siemens Aera) to build a relationship with MRI staff and to explore the MRI environment. During the practice run, children and parents can experience the MRI procedure and develop further helping strategies such as the use of additional blankets or pillows, a mirror on the head coil, or additional earplugs. The child has the opportunity to experience the room where the MRI takes place, the changing positions of the scanner bed, as well as the positions of parent, psychologist, and scanning administrator in a procedure that is convenient for them, involving age-appropriate communication methods. This includes methods for communication between the child and parent and/or team, which are developed individually (e.g., a hand signal from the child to the parent who is holding the hand or handset). One MRI sequence of approximately five minutes is performed, which gives children and parents the opportunity to experience the sound of the magnet and to make a first evaluation about picture quality. Finally, children, parents, and the psychologist reflect on the MRI training and together they decide whether the examination will be done with or without sedation. Children and parents are further instructed to regularly repeat and practice the acquired skills at home, while using relaxation, self-control, and operant techniques. More details on the proceedings can be found in Figure 1.
2.2. Ethical Approval
2.3. Participants
2.4. Design
2.4.1. Retrospective Analysis
2.4.2. Prospective Analysis
2.5. Statistical Analysis
3. Results
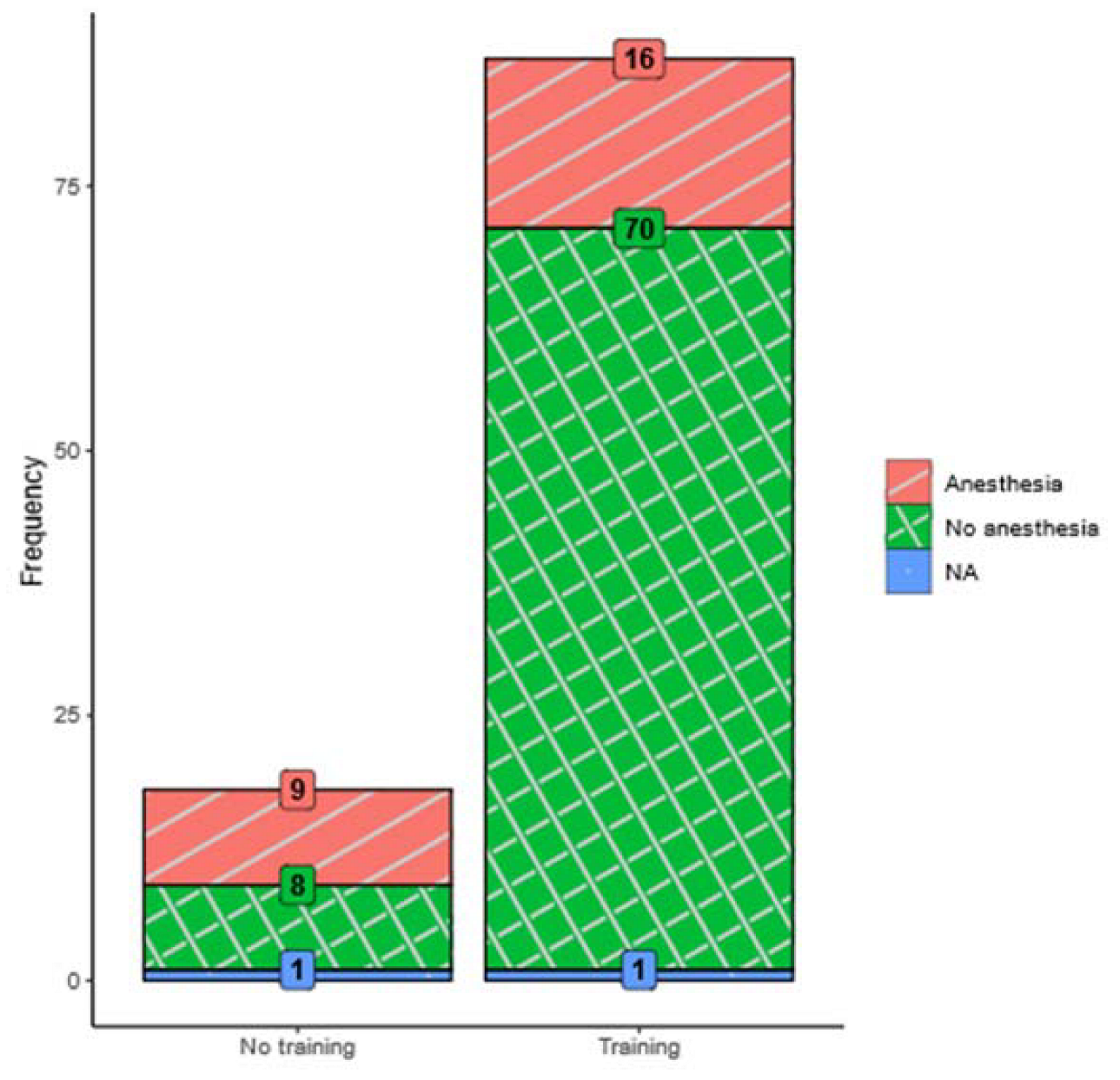
3.1. Effect of MRI Training (Retrospective Analysis)
3.2. Moderators of MRI Success (Retrospective Analysis)
3.2.1. Sociodemographic and Medical Associations
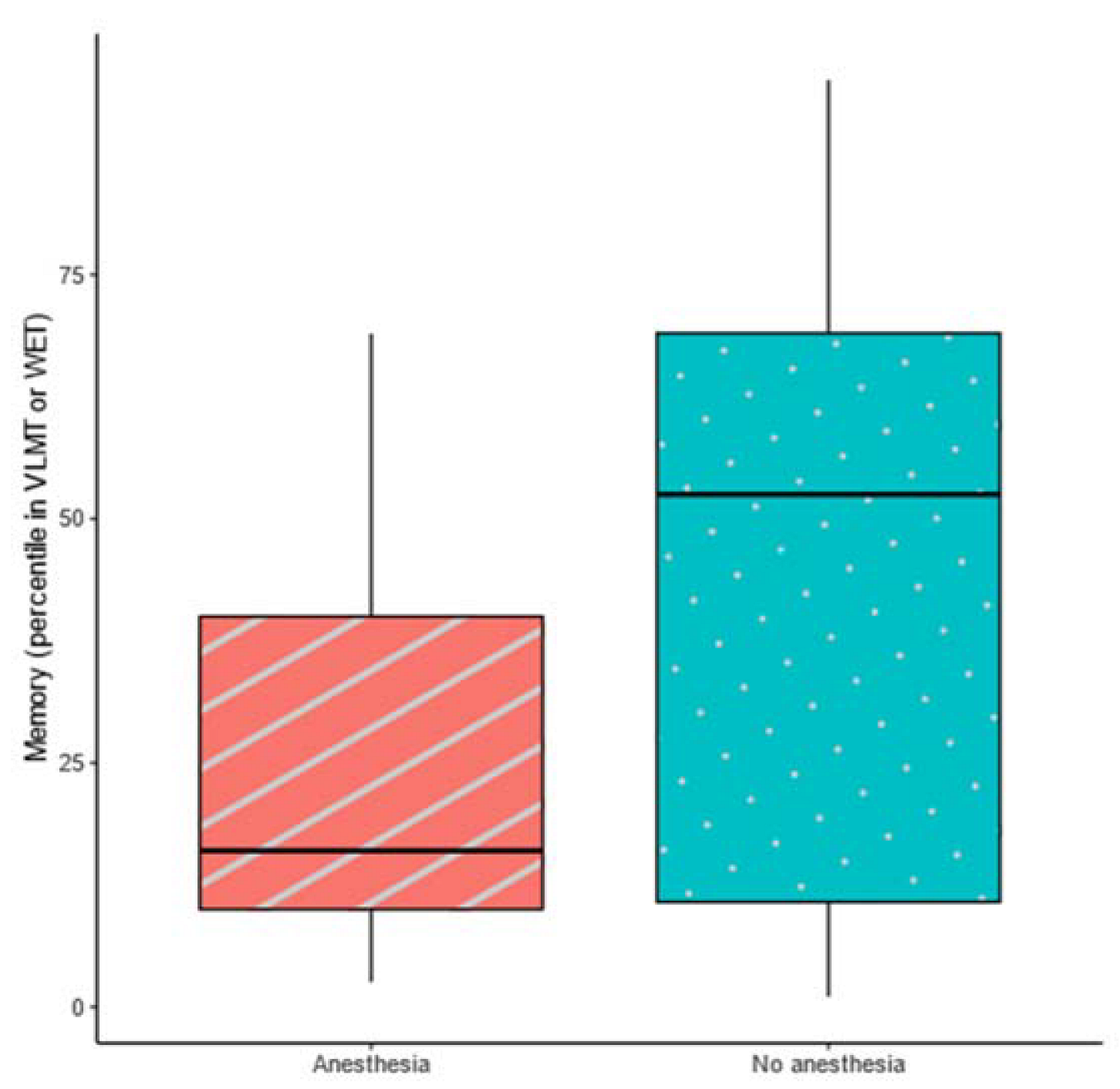
3.2.2. Neuropsychological and Behavioral Associations
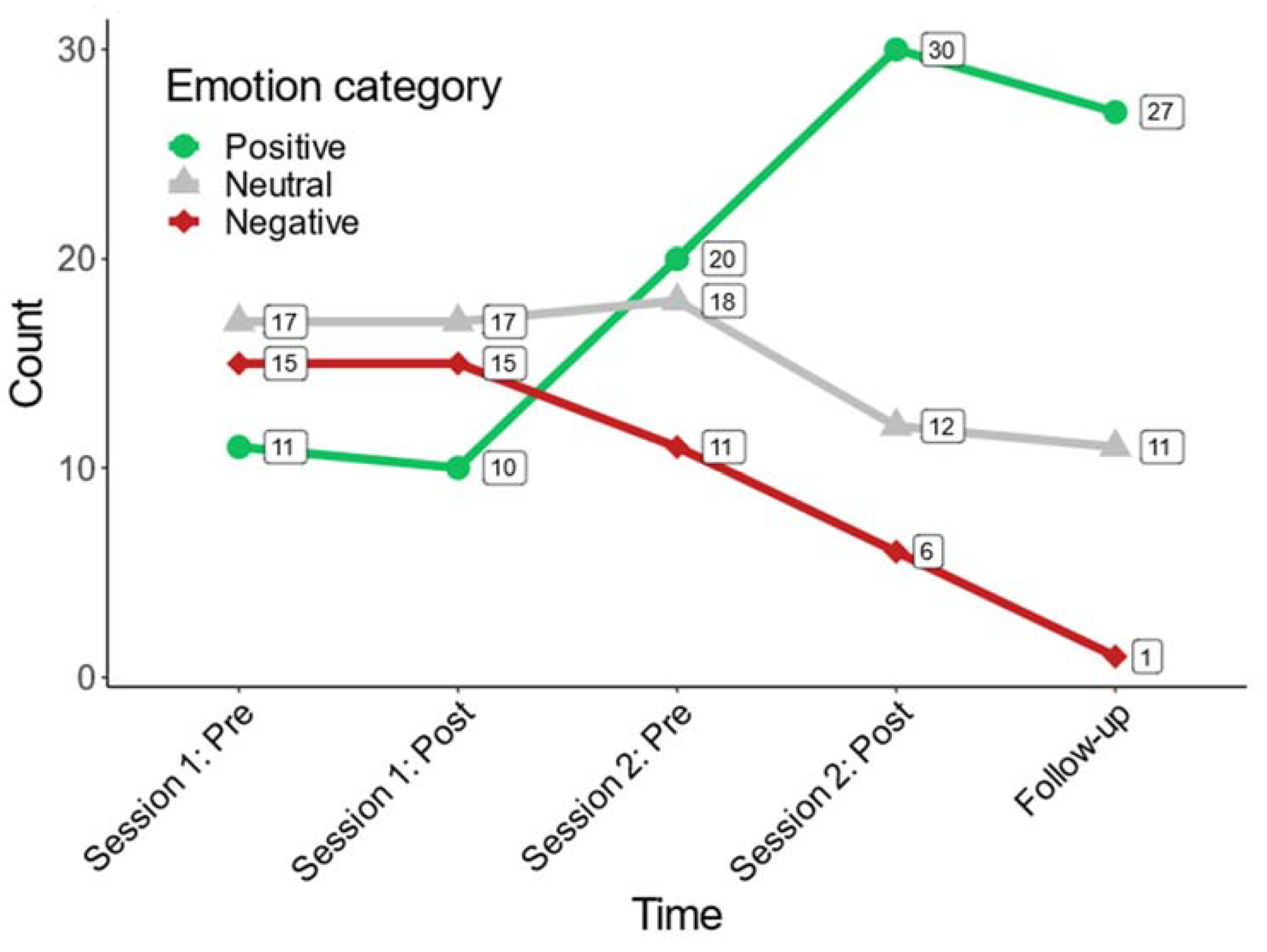
3.2.3. Evaluation of Patients’ Emotional Well-Being (Prospective Analysis)
3.2.4. Interdisciplinary Evaluation (Prospective Analysis)
4. Discussion
5. Limitations and Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chou, I.J.; Tench, C.R.; Gowland, P.; Jaspan, T.; Dineen, R.A.; Evangelou, N.; Abdel-Fahim, R.; Whitehouse, W.P.; Constantinescu, C.S. Subjective discomfort in children receiving 3 T MRI and experienced adults’ perspective on children’s tolerability of 7 T: A cross-sectional questionnaire survey. BMJ Open 2014, 4, e006094. [Google Scholar] [CrossRef]
- Westra, A.E.; Zegers, M.P.A.; Sukhai, R.N.; Kaptein, A.A.; Holscher, H.C.; Ballieux, B.E.P.B.; van Zwet, E.W.; Wit, J.M. Discomfort in children undergoing unsedated MRI. Eur. J. Pediatr. 2011, 170, 771–777. [Google Scholar] [CrossRef]
- Janos, S.; Schooler, G.R.; Ngo, J.S.; Davis, J.T. Free-breathing unsedated MRI in children: Justification and techniques. J. Magn. Reson. Imaging 2019, 50, 365–376. [Google Scholar] [CrossRef]
- Edwards, A.D.; Arthurs, O.J. Paediatric MRI under sedation: Is it necessary? What is the evidence for the alternatives? Pediatr. Radiol. 2011, 41, 1353–1364. [Google Scholar] [CrossRef]
- Cravero, J.P.; Blike, G.T.; Beach, M.; Gallagher, S.M.; Hertzog, J.H.; Havidich, J.E.; Gelman, B. Incidence and nature of adverse events during pediatric sedation/anesthesia for procedures outside the operating room: Report from the pediatric sedation research consortium. Pediatrics 2006, 118, 1087–1096. [Google Scholar] [CrossRef]
- Schulte-Uentrop, L.; Goepfert, M.S. Anaesthesia or sedation for MRI in children. Curr. Opin. Anaesthesiol. 2010, 23, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Rothman, S.; Gonen, A.; Vodonos, A.; Novack, V.; Shelef, I. Does preparation of children before MRI reduce the need for anesthesia? Prospective randomized control trial. Pediatr. Radiol. 2016, 46, 1599–1605. [Google Scholar] [CrossRef] [PubMed]
- Durston, S.; Nederveen, H.; van Dijk, S.; van Belle, J.; de Zeeuw, P.; Langen, M.; van Dijk, A. Magnetic resonance simulation is effective in reducing anxiety related to magnetic resonance scanning in children. J. Am. Acad. Child Adolesc. Psychiatry 2009, 48, 206–207. [Google Scholar] [CrossRef] [PubMed]
- de Amorim e Silva, C.J.T.; Mackenzie, A.; Hallowell, L.M.; Stewart, S.E.; Ditchfield, M.R. Practice MRI: Reducing the need for sedation and general anaesthesia in children undergoing MRI. Australas. Radiol. 2006, 50, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Cahoon, G.D.; Davison, T.E. Prediction of compliance with MRI procedures among children of ages 3 years to 12 years. Pediatr. Radiol. 2014, 44, 1302–1309. [Google Scholar] [CrossRef]
- Gilboa, Y.; Rosenblum, S.; Fattal-Valevski, A.; Josman, N. Application of the International Classification of Functioning, Disability and Health in children with Neurofibromatosis Type 1: A review. Dev. Med. Child Neurol. 2010, 52, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Conklin, H.M.; Ashford, J.M.; Howarth, R.A.; Merchant, T.E.; Ogg, R.J.; Santana, V.M.; Reddick, W.E.; Wu, S.; Xiong, X. Working memory performance among childhood brain tumor survivors. J. Int. Neuropsychol. Soc. JINS 2012, 18, 996–1005. [Google Scholar] [CrossRef]
- Wegenschimmel, B.; Leiss, U.; Veigl, M.; Rosenmayr, V.; Formann, A.; Slavc, I.; Pletschko, T. Do we still need IQ-scores? Misleading interpretations of neurocognitive outcome in pediatric patients with medulloblastoma: A retrospective study. J. Neurooncol. 2017, 135, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Last, B.F.; Grootenhuis, M.A. Emotions, coping and the need for support in families of children with cancer. Patient Educ. Couns. 1998, 33, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Rutowski, S.; Trollmann, R.; Korinthenberg, R.; Warmuth-Metz, M.; Weckesser, M.; Krauss, J.; Pietsch, T. Leitsymptome und Diagnostik der ZNS-Tumoren im Kindes- und Jugendalter (Gemeinsame Leitlinie der Gesellschaft für Neuropädiatrie und der Gesellschaft für Pädiatrische Onkologie und Hämatologie). Available online: https://register.awmf.org/assets/guidelines/025-022l_S1_ZNS-Tumoren_Kinder_Jugendliche_2016-09-abgelaufen.pdf (accessed on 20 February 2023).
- Cejda, K.R.; Smeltzer, M.P.; Hansbury, E.N.; McCarville, M.E.; Helton, K.J.; Hankins, J.S. The impact of preparation and support procedures for children with sickle cell disease undergoing MRI. Pediatr. Radiol. 2012, 42, 1223–1228. [Google Scholar] [CrossRef]
- Hallowell, L.M.; Stewart, S.E.; de Amorim e Silva, C.T.; Ditchfield, M.R. Reviewing the process of preparing children for MRI. Pediatr. Radiol. 2007, 38, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Wiener, L.; Kazak, A.E.; Noll, R.B.; Patenaude, A.F.; Kupst, M.J. Standards for the psychosocial care of children with cancer and their families: An introduction to the special issue. Pediatr. Blood Cancer 2015, 62 (Suppl. S5), S419–S424. [Google Scholar] [CrossRef]
- Flowers, S.R.; Birnie, K.A. Procedural preparation and support as a standard of care in pediatric oncology. Pediatr. Blood Cancer 2015, 62, S694–S723. [Google Scholar] [CrossRef]
- Thompson, A.L.; Young-Saleme, T.K. Anticipatory guidance and psychoeducation as a standard of care in pediatric oncology. Pediatr. Blood Cancer 2015, 62, S684–S693. [Google Scholar] [CrossRef]
- Theys, C.; Wouters, J.; Ghesquière, P. Diffusion tensor imaging and resting-state functional MRI-scanning in 5- and 6-year-old children: Training protocol and motion assessment. PLoS ONE 2014, 9, e94019. [Google Scholar] [CrossRef]
- Thieba, C.; Frayne, A.; Walton, M.; Mah, A.; Benischek, A.; Dewey, D.; Lebel, C. Factors associated with successful MRI scanning in unsedated young children. Front. Pediatr. 2018, 6, 146. [Google Scholar] [CrossRef]
- Viggiano, M.P.; Giganti, F.; Rossi, A.; Di Feo, D.; Vagnoli, L.; Calcagno, G.; Defilippi, C. Impact of psychological interventions on reducing anxiety, fear and the need for sedation in children undergoing magnetic resonance imaging. Pediatr. Rep. 2015, 7, 5682. [Google Scholar] [CrossRef]
- Törnqvist, E.; Månsson, Å.; Hallström, I. Children having magnetic resonance imaging. J. Child Health Care 2014, 19, 359–369. [Google Scholar] [CrossRef]
- Szeszak, S.; Man, R.; Love, A.; Langmack, G.; Wharrad, H.; Dineen, R.A. Animated educational video to prepare children for MRI without sedation: Evaluation of the appeal and value. Pediatr. Radiol. 2016, 46, 1744–1750. [Google Scholar] [CrossRef]
- Rudder, B.S.; Easley, S.J.; Robinson, A.L.; Noel-MacDonnell, J.R.; Nielsen, D.B. Effects of an MRI Try without Program on patient access. Pediatr. Radiol. 2019, 49, 1712–1717. [Google Scholar] [CrossRef]
- Bharti, B.; Malhi, P.; Khandelwal, N. MRI customized play therapy in children reduces the need for sedation: A randomized controlled trial. Am. J. Transplant. 2015, 83, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Perez, M.; Cuscaden, C.; Somers, J.F.; Simms, N.; Shaheed, S.; Kehoe, L.A.; Holowka, S.A.; Aziza, A.A.; Shroff, M.M.; Greer, M.-L.C. Easing anxiety in preparation for pediatric magnetic resonance imaging: A pilot study using animal-assisted therapy. Pediatr. Radiol. 2019, 49, 1000–1009. [Google Scholar] [CrossRef] [PubMed]
- Carter, A.J.; Greer, M.-L.C.; Gray, S.E.; Ware, R.S. Mock MRI: Reducing the need for anaesthesia in children. Pediatr. Radiol. 2010, 40, 1368–1374. [Google Scholar] [CrossRef] [PubMed]
- Morel, B.; Andersson, F.; Samalbide, M.; Binninger, G.; Carpentier, E.; Sirinelli, D.; Cottier, J.-P. Impact on child and parent anxiety level of a teddy bear-scale mock magnetic resonance scanner. Pediatr. Radiol. 2019, 50, 116–120. [Google Scholar] [CrossRef]
- Schröder, H.M.; Lilienthal, S.; Schreiber-Gollwitzer, B.M.; Grießmeier, B.; Hesselbarth, B.; Lein-Köhler, I.; Nest, A.; Weiler-Wichtl, L.J.; Leiss, U. Psychosoziale Versorgung in der Pädiatrischen Onkologie und Hämatologie. Available online: https://www.gpoh.de/sites/gpoh/kinderkrebsinfo/content/e1676/e176475/e176588/e176593/PSAPOHS3-Leitlinie_025_002_Langfassung2019_ger.pdf (accessed on 2 April 2022).
- Schurmann, J.V.; Gayes, L.A.; Slosky, L.; Hunter, M.E.; Pino, F.A. Publishing quality improvement work in Clinical Practice in Pediatric Psychology: The “why” and “how to”. Clin. Pract. Pediatr. Psychol. 2015, 3, 80–91. [Google Scholar] [CrossRef]
- Weiler-Wichtl, L.J. Quality Improvement Project—“My Logbook—I Know My Way around!” (German: “Mein Logbuch—Ich Kenne Mich Aus!”). Available online: https://clinicaltrials.gov/ct2/show/NCT04474678 (accessed on 2 April 2022).
- Petermann, F.; Petermann, U. Wechsler Intelligence Scale for Children, 4th ed.; Deutschsprachige Adaption Nach D. Wechsler; Pearson: Frankfurt, Germany, 2011. [Google Scholar] [CrossRef]
- Petermann, F.; Lipsus, M. Wechsler Intelligence Scale for Children, 3rd ed.; Deutschsprachige Adaption Nach D. Wechsler; Pearson: Frankfurt, Germany, 2011. [Google Scholar]
- Kubinger, K.D.; Holocher-Ertl, S. AID 3: Adaptives Intelligenz Diagnostikum 3. Z. Entwicklungspsychol. Padagog. Psychol. 2014, 47, 173–176. [Google Scholar] [CrossRef]
- Macha, T.; Petermann, F. Bayley Scales of Infant and Toddler Development, Third Edition—Deutsche Fassung. Z. Psychiatr. Psychol. Psychother. 2015, 63, 139–143. [Google Scholar] [CrossRef]
- Zimmermann, P.; Gondan, M.; Fimm, B. Kinderversion der Testbatterie zur Aufmerksamkeitsprüfung (KITAP); Psytest: Herzogenrath, Germany, 2002. [Google Scholar]
- Ettrich, K.U.; Ettrich, C. Konzentrations-Handlungsverfahren für Vorschulkinder; Hogrefe: Göttingen, Germany, 2006. [Google Scholar]
- Helmstaedter, C.; Lendt, M.; Lux, S. Verbaler Lern- und Merkfähigkeitstest (VLMT); Beltz Test: Göttingen, Germany, 2001. [Google Scholar]
- Kastner-Koller, U.; Deimann, P. Der Wiener Entwicklungstest. Ein Verfahren zur Erfassung des Allgemeinen Entwicklungsstandes bei Kindern von 3 bis 6 Jahren; Hogrefe: Göttingen, Germany, 2012. [Google Scholar]
- Bernstein, J.H.; Waber, D.P. Developmental Scoring System for the Rey-Osterrieth Complex Figure (DSS ROCF); Psychological Assessment Resources Inc.: Lutz, FL, USA, 1996. [Google Scholar]
- Goodman, R. Strengths and Difficulties Questionnaire (SDQ); APA PsycTests: Washington, DC, USA, 1997. [Google Scholar]
- Weiler-Wichtl, L.J.; Fries, J.; Schwarzinger, A.; Fohn-Erhold, V.; Pletschko, T.; Leiss, U. How do you feel? A simple tool visual tool for assessing emotional well-being. Health Educ. Public Health 2021, 4, 436–440. [Google Scholar] [CrossRef]
- Derrick, B.; White, P. Why Welch’s test is Type I error robust. Quant. Methods Psychol. 2016, 12, 30–38. [Google Scholar] [CrossRef]
- Faraway, J.J. Extending the Linear Model with R: Generalized Linear, Mixed Effects, and Nonparametric Regression Models; CRC Press: New York, NY, USA, 2004. [Google Scholar]
- Nakagawa, S. A farewell to Bonferroni: The problems of low statistical power and publication bias. Behav. Ecol. 2004, 15, 1044–1045. [Google Scholar] [CrossRef]
- Barnea-Goraly, N.; Weinzimer, S.A.; Ruedy, K.J.; Mauras, N.; Beck, R.W.; Marzelli, M.J.; Mazaika, P.K.; Aye, T.; White, N.H.; Tsalikian, E.; et al. High success rates of sedation-free brain MRI scanning in young children using simple subject preparation protocols with and without a commercial mock scanner: The Diabetes Research in Children Network (DirecNet) experience. Pediatr. Radiol. 2014, 44, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Tazegul, G.; Etcioglu, E.; Yildiz, F.; Yildiz, R.; Tuney, D. Can MRI related patient anxiety be prevented? Magn. Reson. Imaging 2015, 33, 180–183. [Google Scholar] [CrossRef] [PubMed]
- de Bie, H.M.A.; Boersma, M.; Wattjes, M.P.; Adriaanse, S.; Vermeulen, R.J.; Oostrom, K.J.; Huisman, J.; Veltman, D.J.; Delemarre-Van de Waal, H.A. Preparing children with a mock scanner training protocol results in high quality structural and functional MRI scans. Eur. J. Pediatr. 2010, 169, 1079–1085. [Google Scholar] [CrossRef]
- Stavinoha, P.L.; Askins, M.A.; Powell, S.K.; Pillay Smiley, N.; Robert, R.S. Neurocognitive and psychosocial outcomes in pediatric brain tumor survivors. Bioengineering 2018, 5, 73. [Google Scholar] [CrossRef]
- Chevignard, M.; Câmara-Costa, H.; Doz, F.; Dellatolas, G. Core deficits and quality of survival after childhood medulloblastoma: A review. Neuro-Oncol. Pract. 2017, 4, 82–97. [Google Scholar] [CrossRef]
- Wefel, J.S.; Noll, K.R.; Scheurer, M.E. Neurocognitive functioning and genetic variation in patients with primary brain tumours. Lancet Oncol. 2016, 17, e97–e108. [Google Scholar] [CrossRef] [PubMed]
- Sbicigo, J.B.; Toazza, R.; Becker, N.; Ecker, K.; Manfro, G.G.; Salles, J.F.d. Memory and language impairments are associated with anxiety disorder severity in childhood. Trends Psychiatry Psychother. 2020, 42, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Tziraki, M.; Garg, S.; Harrison, E.; Wright, N.B.; Hawkes, R.; Akhtar, K.; Green, J.; Stivaros, S. A neuroimaging preparation protocol tailored for autism. Autism Res. 2020, 14, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Sury, M.R.J.; Harker, H.; Begent, J.; Chong, W.K. The management of infants and children for painless imaging. Clin. Radiol. 2005, 60, 731–741. [Google Scholar] [CrossRef] [PubMed]
- Baxter, S.; Johnson, M.; Chambers, D.; Sutton, A.; Goyder, E.; Booth, A. The effects of integrated care: A systematic review of UK and international evidence. BMC Health Serv. Res. 2018, 18, 350. [Google Scholar] [CrossRef]

| Variable | Frequency (%) |
|---|---|
| Sex | |
| Female | 53 (50.5%) |
| Male | 52 (49.5%) |
| First language | |
| German | 60 (66%) |
| Turkish | 5 (6%) |
| Serbian | 3 (4%) |
| Bosnian | 1 (1%) |
| Polish | 1 (1%) |
| Other | 9 (10%) |
| Bilingual | 12 (13%) |
| Education | |
| Kindergarten/pre-school | 38 (36%) |
| Primary school | 44 (41%) |
| High school | 8 (8%) |
| Not available | 16 (15%) |
| Special education needs | |
| Regular school | 34 (32%) |
| Special education | 12 (12%) |
| Not available | 59 (56%) |
| Diagnosis | |
| NF1 | 33 (31%) |
| NF1 with low grade glioma | 21 (20%) |
| Low grade glioma | 32 (31%) |
| Other brain tumors | 15 (14%) |
| Other | 4 (4%) |
| Progression of brain tumor | |
| No | 98 (93%) |
| Yes | 7 (7%) |
| Medication | |
| None | 71 (68%) |
| Yes | 34 (32%) |
| Medical Therapy | |
| Observance only | 52 (50%) |
| Surgery only | 22 (21%) |
| Surgery + chemotherapy | 6 (6%) |
| Surgery + chemotherapy + radiation therapy | 10 (9%) |
| Surgery + radiation therapy + chemotherapy + antiangiogenic therapy | 2 (2%) |
| chemotherapy only | 10 (9%) |
| chemotherapy + radiation therapy | 2 (2%) |
| none | 1 (1%) |
| Neuropsychological Construct | Name of Test | Publication Year |
|---|---|---|
| Intelligence | Wechsler Intelligence Scale for Children—Fourth Edition [34] | 2011 |
| Wechsler Preschool and Primary Scale of Intelligence—Third Edition[35] | 2014 | |
| Adaptives Intelligenzdiagnostikum III [36] | 2014 | |
| Bayley Scales of Infant and Toddler Development-Third Edition [37] | 2015 | |
| Attention | Kinderversion der Testbatterie zur Aufmerksamkeitsprüfung (KITAP) [38] | |
| Konzentrations-Handlungsverfahren für Vorschulkinder [39] | 2006 | |
| Memory | Verbaler Lern- und Merkfähigkeits Test [40] | 2001 |
| Wiener Entwicklungstest [41] | 2012 | |
| Developmental Scoring System for the Rey Osterrith Complex Figure [42] | ||
| Behavior | Strengths and Difficulties Questionnaire [43] | 1999 |
| Psychometric Assessment | t (df) | p | Cohen’s d | |
| IQ (Wechsler test) | 0.06 (28.67) | 0.95 | 0.02 | |
| IQ (AID-3) | −1.38 (13.67) | 0.19 | −0.57 | |
| Range of intelligence (AID-3) | 0.18 (10.36) | 0.86 | 0.08 | |
| Memory (VLMT/WET) | −3.03 (38.28) | 0.00 * | −0.72 | |
| KHV-VK: time | 0.27 (23.12) | 0.79 | 0.09 | |
| KHV-VK: errors | −0.71 (23.34) | 0.48 | −0.25 | |
| KiTAP: time in distractibility condition | 0.37 (21.18) | 0.72 | 0.11 | |
| KiTAP: correctness (distractibility condition) | −0.10 (13.08) | 0.92 | −0.04 | |
| KiTAP: completeness (distractibility condition) | −0.94 (21.06) | 0.36 | −0.29 | |
| SDQ Category (Normal vs. Critical Range) | χ2 (df) | p | OR | Cramér’s V |
| Overall stress | 2.57 (1) | 0.11 | 2.37 | 0.19 |
| Emotional distress | 0.42 (1) | 0.52 | 1.44 | 0.08 |
| Behavioral difficulties | 0.74 (1) | 0.39 | 1.59 | 0.10 |
| Hyperactivity and attentional difficulties | 8.31 (1) | 0.00 * | 4.73 * | 0.34 |
| Difficulties getting along with others | 0.00 (1) | 0.97 | 1.02 | 0.00 |
| Kind and helpful behavior | 1.52 (1) | 0.22 | 2.11 | 0.14 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weiler-Wichtl, L.J.; Fries, J.; Fohn-Erhold, V.; Schwarzinger, A.; Holzer, A.E.; Pletschko, T.; Furtner-Srajer, J.; Prayer, D.; Bär, P.; Slavc, I.; et al. Initial Evidence for Positive Effects of a Psychological Preparation Program for MRI “iMReady” in Children with Neurofibromatosis Type I and Brain Tumors—How to Meet the Patients’ Needs Best. J. Clin. Med. 2023, 12, 1902. https://doi.org/10.3390/jcm12051902
Weiler-Wichtl LJ, Fries J, Fohn-Erhold V, Schwarzinger A, Holzer AE, Pletschko T, Furtner-Srajer J, Prayer D, Bär P, Slavc I, et al. Initial Evidence for Positive Effects of a Psychological Preparation Program for MRI “iMReady” in Children with Neurofibromatosis Type I and Brain Tumors—How to Meet the Patients’ Needs Best. Journal of Clinical Medicine. 2023; 12(5):1902. https://doi.org/10.3390/jcm12051902
Chicago/Turabian StyleWeiler-Wichtl, Liesa Josephine, Jonathan Fries, Verena Fohn-Erhold, Agathe Schwarzinger, Angelika Elisabeth Holzer, Thomas Pletschko, Julia Furtner-Srajer, Daniela Prayer, Paul Bär, Irene Slavc, and et al. 2023. "Initial Evidence for Positive Effects of a Psychological Preparation Program for MRI “iMReady” in Children with Neurofibromatosis Type I and Brain Tumors—How to Meet the Patients’ Needs Best" Journal of Clinical Medicine 12, no. 5: 1902. https://doi.org/10.3390/jcm12051902
APA StyleWeiler-Wichtl, L. J., Fries, J., Fohn-Erhold, V., Schwarzinger, A., Holzer, A. E., Pletschko, T., Furtner-Srajer, J., Prayer, D., Bär, P., Slavc, I., Peyrl, A., Azizi, A., Hansl, R., & Leiss, U. (2023). Initial Evidence for Positive Effects of a Psychological Preparation Program for MRI “iMReady” in Children with Neurofibromatosis Type I and Brain Tumors—How to Meet the Patients’ Needs Best. Journal of Clinical Medicine, 12(5), 1902. https://doi.org/10.3390/jcm12051902







