Pediatric Diabetic Nephropathy: Novel Insights from microRNAs
Abstract
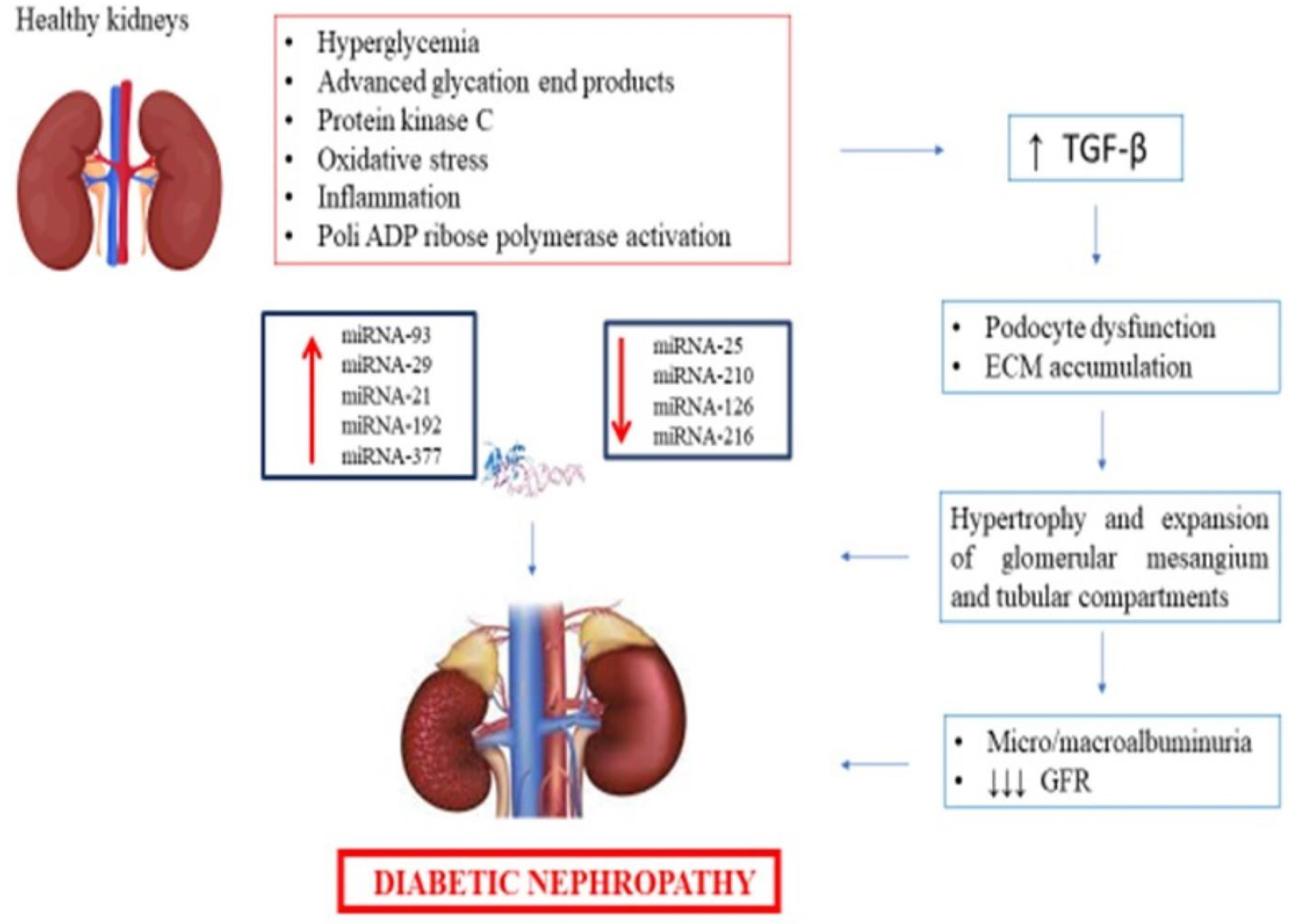
:1. Introduction
2. Evidence on the Role of miRNAs -21, -126, -216, and -377 in DN Pathogenesis
3. Evidence on the Role of mi-RNAs 25, -93, -210, -29, and -192 in DN Pathogenesis
4. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heinzel, A.; Muhlberger, I.; Stelzer, G.; Lancet, D.; Oberbauer, R.; Martin, M.; Perco, P. Molecular disease presentation in diabetic nephropathy. Nephrol. Dial. Transplant. 2015, 30 (Suppl. S4), iv17–iv25. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, E.; Lim, S.; Lamptey, R.; Webb, D.R.; Davies, M.J. Type 2 diabetes. Lancet 2022, 400, 1803–1820. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association Professional Practice Committee. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2022. Diabetes Care 2022, 45 (Suppl. S1), S17–S38. [Google Scholar] [CrossRef] [PubMed]
- Umanath, K.; Lewis, J.B. Diabetic Kidney Disease: The Tiger May Have New Stripes. Am. J. Kidney Dis. 2018, 72, 631–633. [Google Scholar] [CrossRef]
- Slomski, A. New Data on Retinopathy in Youth-Onset Type 2 Diabetes. JAMA. 2022, 327, 416. [Google Scholar] [CrossRef]
- Alicic, R.Z.; Rooney, M.T.; Tuttle, K.R. Diabetic Kidney Disease: Challenges, Progress, and Possibilities. Clin. J. Am. Soc. Nephrol. 2017, 12, 2032–2045. [Google Scholar] [CrossRef]
- Tuttle, K.R.; Jones, C.R.; Daratha, K.B.; Koyama, A.K.; Nicholas, S.B.; Alicic, R.Z.; Duru, O.K.; Neumiller, J.J.; Norris, K.C.; Burrows, N.; et al. Incidence of Chronic Kidney Disease among Adults with Diabetes, 2015–2020. N. Engl. J. Med. 2022, 387, 1430–1431. [Google Scholar] [CrossRef]
- Gilbert, R.E. Diabetic kidney disease 2.0: The treatment paradigm shifts. Lancet Diabetes Endocrinol. 2019, 7, 820–821. [Google Scholar] [CrossRef]
- Umanath, K.; Lewis, J.B. Update on Diabetic Nephropathy: Core Curriculum 2018. Am. J. Kidney Dis. 2018, 71, 884–895. [Google Scholar] [CrossRef]
- Lee, S.Y.; Choi, M.E. Urinary biomarkers for early diabetic nephropathy: Beyond albuminuria. Pediatr. Nephrol. 2015, 30, 1063–1075. [Google Scholar] [CrossRef] [Green Version]
- Sheetz, M.J.; King, G.L. Molecular understanding of hyperglycemia’s adverse effects for diabetic complications. JAMA 2002, 288, 2579–2588. [Google Scholar] [CrossRef]
- Tang, J.; Liu, F.; Cooper, M.E.; Chai, Z. Renal fibrosis as a hallmark of diabetic kidney disease: Potential role of targeting transforming growth factor-beta [TGF-beta] and related molecules. Expert Opin. Ther. Targets 2022, 26, 721–738. [Google Scholar] [CrossRef]
- Zhou, K.; Zi, X.; Song, J.; Zhao, Q.; Liu, J.; Bao, H.; Li, L. Molecular Mechanistic Pathways Targeted by Natural Compounds in the Prevention and Treatment of Diabetic Kidney Disease. Molecules 2022, 27, 6221. [Google Scholar] [CrossRef]
- Liu, H.; Feng, J.; Tang, L. Early renal structural changes and potential biomarkers in diabetic nephropathy. Front. Physiol. 2022, 13, 1020443. [Google Scholar] [CrossRef]
- Rico-Fontalvo, J.; Aroca, G.; Cabrales, J.; Daza-Arnedo, R.; Yanez-Rodriguez, T.; Martinez-Avila, M.C.; Uparella-Gulfo, I.; Raad-Sarabia, M. Molecular Mechanisms of Diabetic Kidney Disease. Int. J. Mol. Sci. 2022, 23, 8668. [Google Scholar] [CrossRef]
- Xie, Z.; Xiao, X. Novel biomarkers and therapeutic approaches for diabetic retinopathy and nephropathy: Recent progress and future perspectives. Front. Endocrinol. 2022, 13, 1065856. [Google Scholar] [CrossRef]
- Jung, C.Y.; Yoo, T.H. Pathophysiologic Mechanisms and Potential Biomarkers in Diabetic Kidney Disease. Diabetes Metab. J. 2022, 46, 181–197. [Google Scholar] [CrossRef]
- Jung, C.Y.; Yoo, T.H. Novel biomarkers for diabetic kidney disease. Kidney Res. Clin. Pract. 2022, 41 (Suppl. S2), S46–S62. [Google Scholar] [CrossRef]
- Persson, F.; Rossing, P. Diagnosis of diabetic kidney disease: State of the art and future perspective. Kidney Int. Suppl. 2018, 8, 2–7. [Google Scholar] [CrossRef]
- Limonte, C.P.; Kretzler, M.; Pennathur, S.; Pop-Busui, R.; de Boer, I.H. Present and future directions in diabetic kidney disease. J. Diabetes Complicat. 2022, 36, 108357. [Google Scholar] [CrossRef]
- Colhoun, H.M.; Marcovecchio, M.L. Biomarkers of diabetic kidney disease. Diabetologia 2018, 61, 996–1011. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, S.B. Use of urinary proteomics in diagnosis and monitoring of diabetic kidney disease. Lancet Diabetes Endocrinol. 2020, 8, 261–262. [Google Scholar] [CrossRef] [PubMed]
- Kushwaha, K.; Garg, S.S.; Gupta, J. Targeting epigenetic regulators for treating diabetic nephropathy. Biochimie 2022, 202, 146–158. [Google Scholar] [CrossRef] [PubMed]
- Tu, C.; Wang, L.; Wei, L.; Jiang, Z. The role of circular RNA in Diabetic Nephropathy. Int. J. Med. Sci. 2022, 19, 916–923. [Google Scholar] [CrossRef] [PubMed]
- Mafi, A.; Yadegar, N.; Salami, M.; Salami, R.; Vakili, O.; Aghadavod, E. Circular RNAs; powerful microRNA sponges to overcome diabetic nephropathy. Pathol. Res. Pract. 2021, 227, 153618. [Google Scholar] [CrossRef]
- Mahtal, N.; Lenoir, O.; Tinel, C.; Anglicheau, D.; Tharaux, P.L. MicroRNAs in kidney injury and disease. Nat. Rev. Nephrol. 2022, 18, 643–662. [Google Scholar] [CrossRef]
- Assmann, T.S.; Recamonde-Mendoza, M.; de Souza, B.M.; Bauer, A.C.; Crispim, D. MicroRNAs and diabetic kidney disease: Systematic review and bioinformatic analysis. Mol. Cell. Endocrinol. 2018, 477, 90–102. [Google Scholar] [CrossRef]
- Wu, H.; Kong, L.; Zhou, S.; Cui, W.; Xu, F.; Luo, M.; Li, X.; Tan, Y.; Miao, L. The role of microRNAs in diabetic nephropathy. J. Diabetes Res. 2014, 2014, 920134. [Google Scholar] [CrossRef]
- Lu, Y.; Liu, D.; Feng, Q.; Liu, Z. Diabetic Nephropathy: Perspective on Extracellular Vesicles. Front. Immunol. 2020, 11, 943. [Google Scholar] [CrossRef]
- Vishnoi, A.; Rani, S. miRNA Biogenesis and Regulation of Diseases: An Updated Overview. Methods Mol. Biol. 2023, 2595, 1–12. [Google Scholar]
- Abdel Halim, A.S.; Rudayni, H.A.; Chaudhary, A.A.; Ali, M.A.M. MicroRNAs: Small molecules with big impacts in liver injury. J. Cell. Physiol. 2022, 238, 32–69. [Google Scholar] [CrossRef]
- Ma, J.; Wang, Y.; Xu, H.T.; Ren, N.; Zhao, N.; Wang, B.M.; Du, L.K. MicroRNA: A novel biomarker and therapeutic target to combat autophagy in diabetic nephropathy. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 6257–6263. [Google Scholar]
- Liu, S.; Wu, W.; Tang, F.; Shen, M.; Xu, W.; Zhao, S. MicroRNA-21: A Critical Pathogenic Factor of Diabetic Nephropathy. Front. Endocrinol. 2022, 13, 895010. [Google Scholar] [CrossRef]
- Roy, D.; Modi, A.; Khokhar, M.; Sankanagoudar, S.; Yadav, D.; Sharma, S.; Purohit, P.; Sharma, P. MicroRNA 21 Emerging Role in Diabetic Complications: A Critical Update. Curr. Diabetes Rev. 2021, 17, 122–135. [Google Scholar]
- Kaur, P.; Kotru, S.; Singh, S.; Munshi, A. miRNA signatures in diabetic retinopathy and nephropathy: Delineating underlying mechanisms. J. Physiol. Biochem. 2022, 78, 19–37. [Google Scholar] [CrossRef]
- Fawzy, M.S.; Al Ageeli, E.; Al-Qahtani, S.A.; Abu Alsel, B.T.; Kattan, S.W.; Alelwani, W.; Toraih, E.A. MicroRNA-499a [rs3746444A/G] gene variant and susceptibility to type 2 diabetes-associated end-stage renal disease. Exp. Ther. Med. 2022, 23, 63. [Google Scholar] [CrossRef]
- Cai, Q.; Wang, C.; Huang, L.; Wu, C.; Yan, B.; Chen, T.; Li, Q.; Wang, L. Long Non-Coding RNA Small Nucleolar RNA Host Gene 5 [SNHG5] Regulates Renal Tubular Damage in Diabetic Nephropathy via Targeting MiR-26a-5p. Horm. Metab. Res. 2021, 53, 818–824. [Google Scholar] [CrossRef]
- Han, Q.; Zhang, Y.; Jiao, T.; Li, Q.; Ding, X.; Zhang, D.; Cai, G.; Zhu, H. Urinary sediment microRNAs can be used as potential noninvasive biomarkers for diagnosis, reflecting the severity and prognosis of diabetic nephropathy. Nutr. Diabetes 2021, 11, 24. [Google Scholar] [CrossRef]
- Ishii, H.; Kaneko, S.; Yanai, K.; Aomatsu, A.; Hirai, K.; Ookawara, S.; Morishita, Y. MicroRNA Expression Profiling in Diabetic Kidney Disease. Transl. Res. 2021, 237, 31–52. [Google Scholar] [CrossRef]
- Argyropoulos, C.; Wang, K.; Bernardo, J.; Ellis, D.; Orchard, T.; Galas, D.; Johnson, J.P. Urinary MicroRNA Profiling Predicts the Development of Microalbuminuria in Patients with Type 1 Diabetes. J. Clin. Med. 2015, 4, 1498–1517. [Google Scholar] [CrossRef]
- Ishii, H.; Kaneko, S.; Yanai, K.; Aomatsu, A.; Hirai, K.; Ookawara, S.; Morishita, Y. MicroRNAs in Podocyte Injury in Diabetic Nephropathy. Front. Genet. 2020, 11, 993. [Google Scholar] [CrossRef] [PubMed]
- Ren, H.; Wang, Q. Non-Coding RNA and Diabetic Kidney Disease. DNA Cell Biol. 2021, 40, 553–567. [Google Scholar] [CrossRef] [PubMed]
- Abdelghaffar, S.; Shora, H.; Abdelatty, S.; Elmougy, F.; El Sayed, R.; Abdelrahman, H.; Soliman, H.; Algebaly, H.; Ahmed, S.; Alfy, P.; et al. MicroRNAs and Risk Factors for Diabetic Nephropathy in Egyptian Children and Adolescents with Type 1 Diabetes. Diabetes Metab. Syndr. Obes. 2020, 13, 2485–2494. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Cai, D.; Wang, Y.; Zou, Y.; Zhao, T. SNHG15 knockdown inhibits diabetic nephropathy progression in pediatric patients by regulating the miR-141/ICAM-1 axis in vitro. Biosci. Rep. 2021, 41, BSR20204099. [Google Scholar] [CrossRef]
- Osipova, J.; Fischer, D.C.; Dangwal, S.; Volkmann, I.; Widera, C.; Schwarz, K.; Lorenzen, J.M.; Schreiver, C.; Jacoby, U.; Heimhalt, M.; et al. Diabetes-associated microRNAs in pediatric patients with type 1 diabetes mellitus: A cross-sectional cohort study. J. Clin. Endocrinol. Metab. 2014, 99, E1661–E1665. [Google Scholar] [CrossRef]
- El-Samahy, M.H.; Adly, A.A.; Elhenawy, Y.I.; Ismail, E.A.; Pessar, S.A.; Mowafy, M.E.; Saad, M.S.; Mohammed, H.H. Urinary miRNA-377 and miRNA-216a as biomarkers of nephropathy and subclinical atherosclerotic risk in pediatric patients with type 1 diabetes. J Diabetes Complicat. 2018, 32, 185–192. [Google Scholar] [CrossRef]
- Gong, Z.; Banchs, P.A.P.; Liu, Y.; Fu, H.; Arena, V.C.; Forno, E.; Libman, I.; Ho, J.; Muzumdar, R. Serum alpha-KL, a potential early marker of diabetes complications in youth with T1D, is regulated by miRNA 192. Front. Endocrinol. 2022, 13, 937093. [Google Scholar] [CrossRef]
- Martino, F.; Lorenzen, J.; Schmidt, J.; Schmidt, M.; Broll, M.; Görzig, Y.; Kielstein, J.T.; Thum, T. Circulating microRNAs are not eliminated by hemodialysis. PLoS ONE 2012, 7, e38269. [Google Scholar] [CrossRef]
- Barutta, F.; Bruno, G.; Matullo, G.; Chaturvedi, N.; Grimaldi, S.; Schalkwijk, C.; Stehouwer, C.D.; Fuller, J.H.; Gruden, G. MicroRNA-126 and micro-/macrovascular complications of type 1 diabetes in the EURODIAB Prospective Complications Study. Acta Diabetol. 2017, 54, 133–139. [Google Scholar] [CrossRef]
- Milas, O.; Gadalean, F.; Vlad, A.; Dumitrascu, V.; Gluhovschi, C.; Gluhovschi, G.; Velciov, S.; Popescu, R.; Bob, F.; Matusz, P.; et al. Deregulated profiles of urinary microRNAs may explain podocyte injury and proximal tubule dysfunction in normoalbuminuric patients with type 2 diabetes mellitus. J. Investig. Med. 2018, 66, 747–754. [Google Scholar] [CrossRef]
- Olivieri, F.; Spazzafumo, L.; Bonafè, M.; Recchioni, R.; Prattichizzo, F.; Marcheselli, F.; Micolucci, L.; Mensà, E.; Giuliani, A.; Santini, G.; et al. MiR-21-5p and miR-126a-3p levels in plasma and circulating angiogenic cells: Relationship with type 2 diabetes complications. Oncotarget 2015, 6, 35372–35382. [Google Scholar] [CrossRef]
- Thum, T.; Gross, C.; Fiedler, J.; Fischer, T.; Kissler, S.; Bussen, M.; Galuppo, P.; Just, S.; Rottbauer, W.; Frantz, S.; et al. MicroRNA-21 contributes to myocardial disease by stimulating MAP kinase signalling in fibroblasts. Nature 2008, 456, 980–984. [Google Scholar] [CrossRef]
- Chau, B.N.; Xin, C.; Hartner, J.; Ren, S.; Castano, A.P.; Linn, G.; Li, J.; Tran, P.T.; Kaimal, V.; Huang, X.; et al. MicroRNA-21 promotes fibrosis of the kidney by silencing metabolic pathways. Sci. Transl. Med. 2012, 4, 121ra18. [Google Scholar] [CrossRef] [Green Version]
- Zarjou, A.; Yang, S.; Abraham, E.; Agarwal, A.; Liu, G. Identification of a microRNA signature in renal fibrosis: Role of miR-21. Am. J. Physiol. Renal. Physiol. 2011, 301, F793–F801. [Google Scholar] [CrossRef]
- Kumarswamy, R.; Volkmann, I.; Jazbutyte, V.; Dangwal, S.; Park, D.H.; Thum, T. Transforming growth factor-β-induced endothelial-to-mesenchymal transition is partly mediated by microRNA-21. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 361–369. [Google Scholar] [CrossRef]
- Nigi, L.; Grieco, G.E.; Ventriglia, G.; Brusco, N.; Mancarella, F.; Formichi, C.; Dotta, F.; Sebastiani, G. MicroRNAs as Regulators of Insulin Signaling: Research Updates and Potential Therapeutic Perspectives in Type 2 Diabetes. Int. J. Mol. Sci. 2018, 19, 3705. [Google Scholar] [CrossRef]
- Dey, N.; Das, F.; Mariappan, M.M.; Mandal, C.C.; Ghosh-Choudhury, N.; Kasinath, B.S.; Choudhury, G.G. MicroRNA-21 orchestrates high glucose-induced signals to TOR complex 1, resulting in renal cell pathology in diabetes. J. Biol. Chem. 2011, 286, 25586–25603. [Google Scholar] [CrossRef]
- Wang, J.; Gao, Y.; Ma, M.; Li, M.; Zou, D.; Yang, J.; Zhu, Z.; Zhao, X. Effect of miR-21 on renal fibrosis by regulating MMP-9 and TIMP1 in kk-ay diabetic nephropathy mice. Cell Biochem. Biophys. 2013, 67, 537–546. [Google Scholar] [CrossRef]
- Zhong, X.; Chung, A.C.; Chen, H.Y.; Dong, Y.; Meng, X.M.; Li, R.; Yang, W.; Hou, F.F.; Lan, H.Y. miR-21 is a key therapeutic target for renal injury in a mouse model of type 2 diabetes. Diabetologia 2013, 56, 663–674. [Google Scholar] [CrossRef]
- Zampetaki, A.; Kiechl, S.; Drozdov, I.; Willeit, P.; Mayr, U.; Prokopi, M.; Mayr, A.; Weger, S.; Oberhollenzer, F.; Bonora, E.; et al. Plasma microRNA profiling reveals loss of endothelial miR-126 and other microRNAs in type 2 diabetes. Circ. Res. 2010, 107, 810–817. [Google Scholar] [CrossRef]
- La Marca, V.; Fierabracci, A. Insights into the Diagnostic Potential of Extracellular Vesicles and Their miRNA Signature from Liquid Biopsy as Early Biomarkers of Diabetic Micro/Macrovascular Complications. Int. J. Mol. Sci. 2017, 18, 1974. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Aurora, A.B.; Johnson, B.A.; Qi, X.; McAnally, J.; Hill, J.A.; Richardson, J.A.; Bassel-Duby, R.; Olson, E.N. The endothelial-specific microRNA miR-126 governs vascular integrity and angiogenesis. Dev. Cell 2008, 15, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Fish, J.E.; Santoro, M.M.; Morton, S.U.; Yu, S.; Yeh, R.F.; Wythe, J.D.; Ivey, K.N.; Bruneau, B.G.; Stainier, D.Y.; Srivastava, D. miR-126 regulates angiogenic signaling and vascular integrity. Dev. Cell 2008, 15, 272–284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, F.; Long, G.; Zhao, C.; Li, H.; Chaugai, S.; Wang, Y.; Chen, C.; Wang, D.W. Atherosclerosis-related circulating miRNAs as novel and sensitive predictors for acute myocardial infarction. PLoS ONE 2014, 9, e105734. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandra, Y.; Carena, M.C.; Spazzafumo, L.; Martinelli, F.; Bassetti, B.; Devanna, P.; Rubino, M.; Marenzi, G.; Colombo, G.I.; Achilli, F.; et al. Diagnostic potential of plasmatic MicroRNA signatures in stable and unstable angina. PLoS ONE 2013, 8, e80345. [Google Scholar] [CrossRef]
- Joladarashi, D.; Garikipati, V.N.S.; Thandavarayan, R.A.; Verma, S.K.; Mackie, A.R.; Khan, M.; Gumpert, A.M.; Bhimaraj, A.; Youker, K.A.; Uribe, C.; et al. Enhanced Cardiac Regenerative Ability of Stem Cells After Ischemia-Reperfusion Injury: Role of Human CD34+ Cells Deficient in MicroRNA-377. J. Am. Coll. Cardiol. 2015, 66, 2214–2226. [Google Scholar] [CrossRef]
- Wen, Z.; Huang, W.; Feng, Y.; Cai, W.; Wang, Y.; Wang, X.; Liang, J.; Wani, M.; Chen, J.; Zhu, P.; et al. MicroRNA-377 regulates mesenchymal stem cell-induced angiogenesis in ischemic hearts by targeting VEGF. PLoS ONE 2014, 9, e104666. [Google Scholar] [CrossRef]
- Wang, Q.; Wang, Y.; Minto, A.W.; Wang, J.; Shi, Q.; Li, X.; Quigg, R.J. MicroRNA-377 is up-regulated and can lead to increased fibronectin production in diabetic nephropathy. FASEB J. 2008, 22, 4126–4135. [Google Scholar] [CrossRef]
- Oh, H.J.; Kato, M.; Deshpande, S.; Zhang, E.; Das, S.; Lanting, L.; Wang, M.; Natarajan, R. Inhibition of the processing of miR-25 by HIPK2-Phosphorylated-MeCP2 induces NOX4 in early diabetic nephropathy. Sci. Rep. 2016, 6, 38789. [Google Scholar] [CrossRef]
- Fu, Y.; Zhang, Y.; Wang, Z.; Wang, L.; Wei, X.; Zhang, B.; Wen, Z.; Fang, H.; Pang, Q.; Yi, F. Regulation of NADPH oxidase activity is associated with miRNA-25-mediated NOX4 expression in experimental diabetic nephropathy. Am. J. Nephrol. 2010, 32, 581–589. [Google Scholar] [CrossRef]
- Ma, J.; Zhang, L.; Hao, J.; Li, N.; Tang, J.; Hao, L. Up-regulation of microRNA-93 inhibits TGF-β1-induced EMT and renal fibrogenesis by down-regulation of Orai1. J. Pharmacol. Sci. 2018, 136, 218–227. [Google Scholar] [CrossRef]
- Long, J.; Wang, Y.; Wang, W.; Chang, B.H.; Danesh, F.R. Identification of microRNA-93 as a novel regulator of vascular endothelial growth factor in hyperglycemic conditions. J. Biol. Chem. 2010, 285, 23457–23465. [Google Scholar] [CrossRef]
- Greco, S.; Fasanaro, P.; Castelvecchio, S.; D’Alessandra, Y.; Arcelli, D.; Di Donato, M.; Malavazos, A.; Capogrossi, M.C.; Menicanti, L.; Martelli, F. MicroRNA dysregulation in diabetic ischemic heart failure patients. Diabetes 2012, 61, 1633–1641. [Google Scholar] [CrossRef] [Green Version]
- Kong, L.; Zhu, J.; Han, W.; Jiang, X.; Xu, M.; Zhao, Y.; Dong, Q.; Pang, Z.; Guan, Q.; Gao, L.; et al. Significance of serum microRNAs in pre-diabetes and newly diagnosed type 2 diabetes: A clinical study. Acta Diabetol. 2011, 48, 61–69. [Google Scholar] [CrossRef]
- Wang, B.; Komers, R.; Carew, R.; Winbanks, C.E.; Xu, B.; Herman-Edelstein, M.; Koh, P.; Thomas, M.; Jandeleit-Dahm, K.; Gregorevic, P.; et al. Suppression of microRNA-29 expression by TGF-β1 promotes collagen expression and renal fibrosis. J. Am. Soc. Nephrol. 2012, 23, 252–265. [Google Scholar] [CrossRef]
- Long, J.; Wang, Y.; Wang, W.; Chang, B.H.; Danesh, F.R. MicroRNA-29c is a signature microRNA under high glucose conditions that targets Sprouty homolog 1, and its in vivo knockdown prevents progression of diabetic nephropathy. J. Biol. Chem. 2011, 286, 11837–11848. [Google Scholar] [CrossRef]
- Kanasaki, K.; Shi, S.; Kanasaki, M.; He, J.; Nagai, T.; Nakamura, Y.; Ishigaki, Y.; Kitada, M.; Srivastava, S.P.; Koya, D. Linagliptin-mediated DPP-4 inhibition ameliorates kidney fibrosis in streptozotocin-induced diabetic mice by inhibiting endothelial-to-mesenchymal transition in a therapeutic regimen. Diabetes 2014, 63, 2120–2131. [Google Scholar] [CrossRef]
- Srivastava, S.P.; Goodwin, J.E.; Kanasaki, K.; Koya, D. Inhibition of Angiotensin-Converting Enzyme Ameliorates Renal Fibrosis by Mitigating DPP-4 Level and Restoring Antifibrotic MicroRNAs. Genes 2020, 11, 211. [Google Scholar] [CrossRef]
- Lee, H.W.; Khan, S.Q.; Khaliqdina, S.; Altintas, M.M.; Grahammer, F.; Zhao, J.L.; Koh, K.H.; Tardi, N.J.; Faridi, M.H.; Geraghty, T.; et al. Absence of miR-146a in Podocytes Increases Risk of Diabetic Glomerulopathy via Up-regulation of ErbB4 and Notch-1. J. Biol. Chem. 2017, 292, 732–747. [Google Scholar] [CrossRef]
- Li, X.; Venkatesh, I.; Villanueva, V.; Wei, H.; Geraghty, T.; Rajagopalan, A.; Helmuth, R.W.; Altintas, M.M.; Faridi, H.M.; Gupta, V. Podocyte-specific deletion of miR-146a increases podocyte injury and diabetic kidney disease. Front. Med. 2022, 9, 897188. [Google Scholar] [CrossRef]
- Motawi, T.K.; Shehata, N.I.; ElNokeety, M.M.; El-Emady, Y.F. Potential serum biomarkers for early detection of diabetic nephropathy. Diabetes Res. Clin. Pract. 2018, 136, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Yan, Y.; Xu, N.; Hui, Y.; Yin, D. Upregulation of microRNA-424 relieved diabetic nephropathy by targeting Rictor through mTOR Complex2/Protein Kinase B signaling. J. Cell. Physiol. 2019, 234, 11646–11653. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Arce, L.; Wang, M.; Putta, S.; Lanting, L.; Natarajan, R. A microRNA circuit mediates transforming growth factor-β1 autoregulation in renal glomerular mesangial cells. Kidney Int. 2011, 80, 358–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kato, M.; Zhang, J.; Wang, M.; Lanting, L.; Yuan, H.; Rossi, J.J.; Natarajan, R. MicroRNA-192 in diabetic kidney glomeruli and its function in TGF-beta-induced collagen expression via inhibition of E-box repressors. Proc. Natl. Acad. Sci. USA 2007, 104, 3432–3437. [Google Scholar] [CrossRef]
- Kato, M.; Dang, V.; Wang, M.; Park, J.T.; Deshpande, S.; Kadam, S.; Mardiros, A.; Zhan, Y.; Oettgen, P.; Putta, S.; et al. TGF-β induces acetylation of chromatin and of Ets-1 to alleviate repression of miR-192 in diabetic nephropathy. Sci. Signal. 2013, 6, ra43. [Google Scholar] [CrossRef]
- Al-Kafaji, G.; Al-Muhtaresh, H.A. Expression of microRNA-377 and microRNA-192 and their potential as blood-based biomarkers for early detection of type 2 diabetic nephropathy. Mol. Med. Rep. 2018, 18, 1171–1180. [Google Scholar] [CrossRef]
- Olejnik, A.; Franczak, A.; Krzywonos-Zawadzka, A.; Kałużna-Oleksy, M.; Bil-Lula, I. The Biological Role of Klotho Protein in the Development of Cardiovascular Diseases. Biomed. Res. Int. 2018, 2018, 5171945. [Google Scholar] [CrossRef]
- Kuro-o, M.; Matsumura, Y.; Aizawa, H.; Kawaguchi, H.; Suga, T.; Utsugi, T.; Ohyama, Y.; Kurabayashi, M.; Kaname, T.; Kume, E.; et al. Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature 1997, 390, 45–51. [Google Scholar] [CrossRef]
- Chen, H.Y.; Zhong, X.; Huang, X.R.; Meng, X.M.; You, Y.; Chung, A.C.; Lan, H.Y. MicroRNA-29b inhibits diabetic nephropathy in db/db mice. Mol. Ther. 2014, 22, 842–853. [Google Scholar] [CrossRef] [Green Version]
| miRNA | References | Study Design | Population | Main Findings |
|---|---|---|---|---|
| miRNA 377 | [43] | Cross-sectional study | 70 children and adolescent with T1D from Diabetes, Endocrine and Metabolism Pediatric Unit (DEMPU) Children Hospital, Cairo University. Mean age 13.21 ± 3.66 years. -25 without DN -45 with DN | Serum miRNA377 was significantly higher in patients with DN than in those without DN and it was positively correlated with LDL cholesterol. |
| [46] | Cross-sectional study | 50 patients with T1D compared to 50 healthy controls from Pediatric Diabetes Clinic, of Pediatric Hospital, Ain Shams University. Mean age 13.7 ± 3.3 years. T1D patients were divided in two groups: -group A: 26 normoalbuminuric diabetic patients without nephropathy. -group B: 24 diabetic patients with nephropathy. | Compared to healthy controls, both patients with and without DN had significantly higher urinary miRNA-377 levels (p ≤ 0.05). In the analyzed diabetic cohort, urinary miR-377 expression was considerably higher in the group B (p ≤ 0.001). | |
| miRNA-126 | [48] | Cross-sectional nested case-control study | 455 patients with T1D. Case subjects (n = 312): patients with ≥1 complications of diabetes; control subjects (n = 143): individuals with no evidence of any complication. | miRNA-126 was negatively linked to each micro-/macrovascular complication that was independently analyzed and with all complications (OR = 0.85, 95% CI 0.75–0.96). |
| [45] | Cross-sectional observational cohort study | -68 young patients with T1D (age 6–18 years) and 79 age- and gender-matched healthy subjects. | Patients with T1D had considerably lower urinary miRNA-126 levels than age- and gender-matched controls. There was a negative correlation between HbA1c mean and miRNA-126 levels. | |
| miRNA-21 | [45] | Cross-sectional observational cohort study | 68 patients with T1D Age 6–18 years, duration of disease >1 year, C-peptide < 0.3 nmol/L, and intensive insulin treatment with either multiple daily insulin injections or continuous subcutaneous insulin infusion for at least 6 months. | A significant increase in miRNA-21 in plasma (p = 0.008) and urine (p ≤ 0.0001) of patients with T1D was found. A positive correlation between urinary miRNA-21 and CRP (r = 0.298, p = 0.029) was showed. |
| [43] | Cross-sectional study | 70 children and adolescents with T1D. | miRNA-21 was positively correlated with urinary levels of cystatin c (r = 0.6, p = 0.01) and negatively correlated with eGFR using cystatin c (r = −0.6, p = 0.01). |
| miRNA | Reference | Study Design | Population | Main Findings |
|---|---|---|---|---|
| miRNA-25 | [43] | Hospital-based cohort cross-sectional study | 70 patients with T1D with a 5 years’ duration of diabetes or more -25 patients (16 males and 9 females) without DN (normal ACR) -45 patients (19 males and 26 females) with DN (increased ACR). | miRNA-25 may have a reno-protective role. Negative correlation between miRNA-25 and ACR was found. miRNAs-25 levels were upregulated in the group without DN and downregulated in the group with DN. |
| miRNA-93 | [43] | Hospital-based cohort | 70 T1D patients with a 5 years’ duration of diabetes or more -25 patients (16 males and 9 females) without DN (normal ACR) -45 patients (19 males and 26 females) with DN (increased ACR). | A positive correlation between miR-93 and HbA1c and ACR was reported. Up-regulation of miRNA-93 in the group with DN compared to the group without DN was found. |
| miRNA-210 | [45] | Cross-sectional observational cohort study | 68 patients with T1D Age 6–18 years, duration of disease > 1 year, C-peptide < 0.3 nmol/L, and intensive insulin treatment with either multiple daily insulin injections or continuous subcutaneous insulin infusion for at least 6 months. | Both plasma and urinary miRNA-210 levels of patients with T1D were higher than controls. |
| miRNA-126 | [45] | Cross-sectional observational cohort study | 68 patients with T1D Age 6–18 years, duration of disease > 1 year, C-peptide < 0.3 nmol/L, and intensive insulin treatment with either multiple daily insulin injections or continuous subcutaneous insulin infusion for at least 6 months. | No differences emerged in plasmatic T1D sample, while lower miRNA-126 levels were confirmed in urine T1D samples compared to controls (p = 0.016). A negative association between urinary miRNA-126 levels and HbA1c was found. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lanzaro, F.; Barlabà, A.; De Nigris, A.; Di Domenico, F.; Verde, V.; Miraglia del Giudice, E.; Di Sessa, A. Pediatric Diabetic Nephropathy: Novel Insights from microRNAs. J. Clin. Med. 2023, 12, 1447. https://doi.org/10.3390/jcm12041447
Lanzaro F, Barlabà A, De Nigris A, Di Domenico F, Verde V, Miraglia del Giudice E, Di Sessa A. Pediatric Diabetic Nephropathy: Novel Insights from microRNAs. Journal of Clinical Medicine. 2023; 12(4):1447. https://doi.org/10.3390/jcm12041447
Chicago/Turabian StyleLanzaro, Francesca, Annalisa Barlabà, Angelica De Nigris, Federica Di Domenico, Valentina Verde, Emanuele Miraglia del Giudice, and Anna Di Sessa. 2023. "Pediatric Diabetic Nephropathy: Novel Insights from microRNAs" Journal of Clinical Medicine 12, no. 4: 1447. https://doi.org/10.3390/jcm12041447
APA StyleLanzaro, F., Barlabà, A., De Nigris, A., Di Domenico, F., Verde, V., Miraglia del Giudice, E., & Di Sessa, A. (2023). Pediatric Diabetic Nephropathy: Novel Insights from microRNAs. Journal of Clinical Medicine, 12(4), 1447. https://doi.org/10.3390/jcm12041447






