Do Surgeons Anticipate Women’s Hopes and Fears Associated with Prolapse Repair? A Qualitative Analysis in the PROSPERE Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion
2.2. Questionnaires
2.3. Data Analysis
3. Results
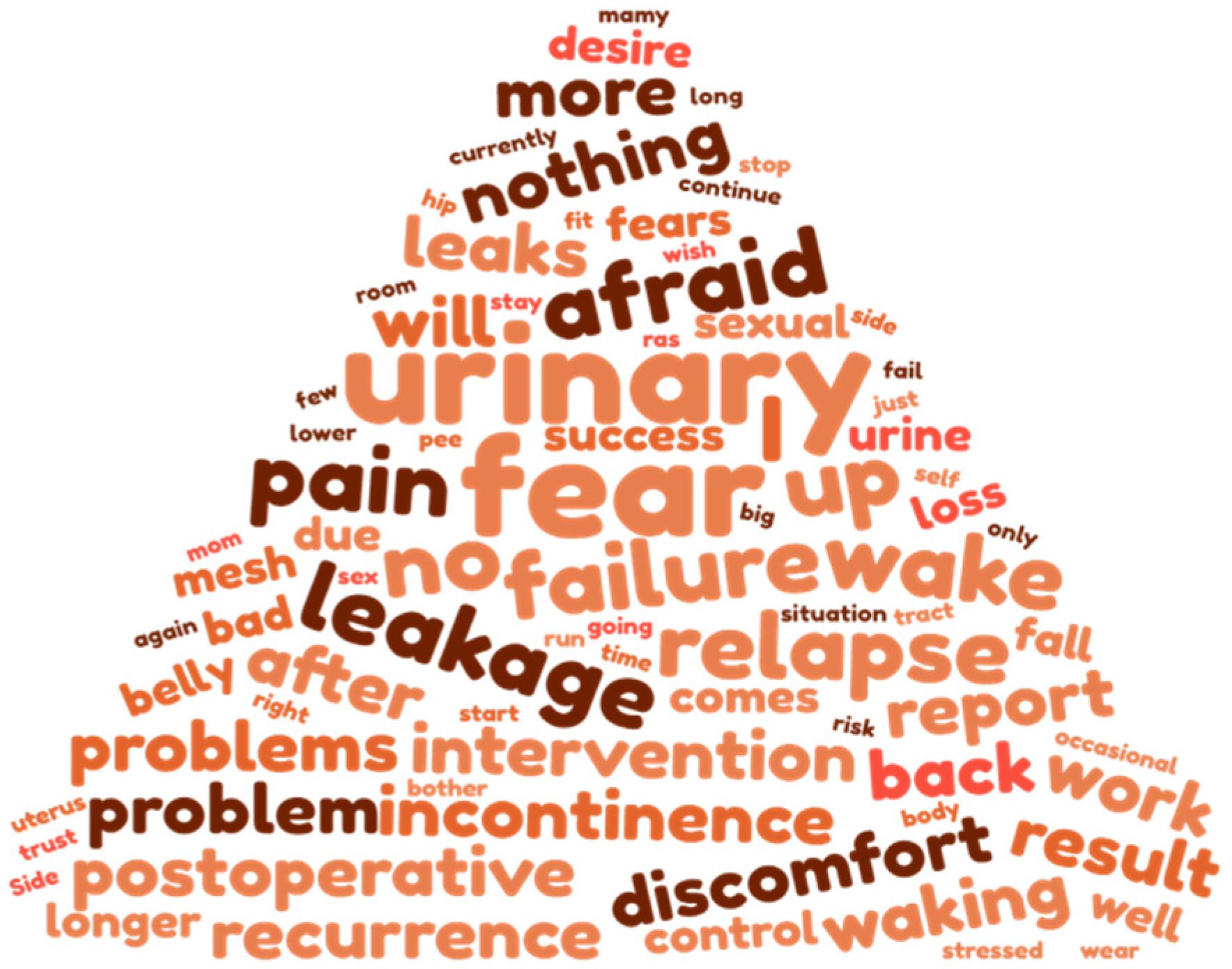
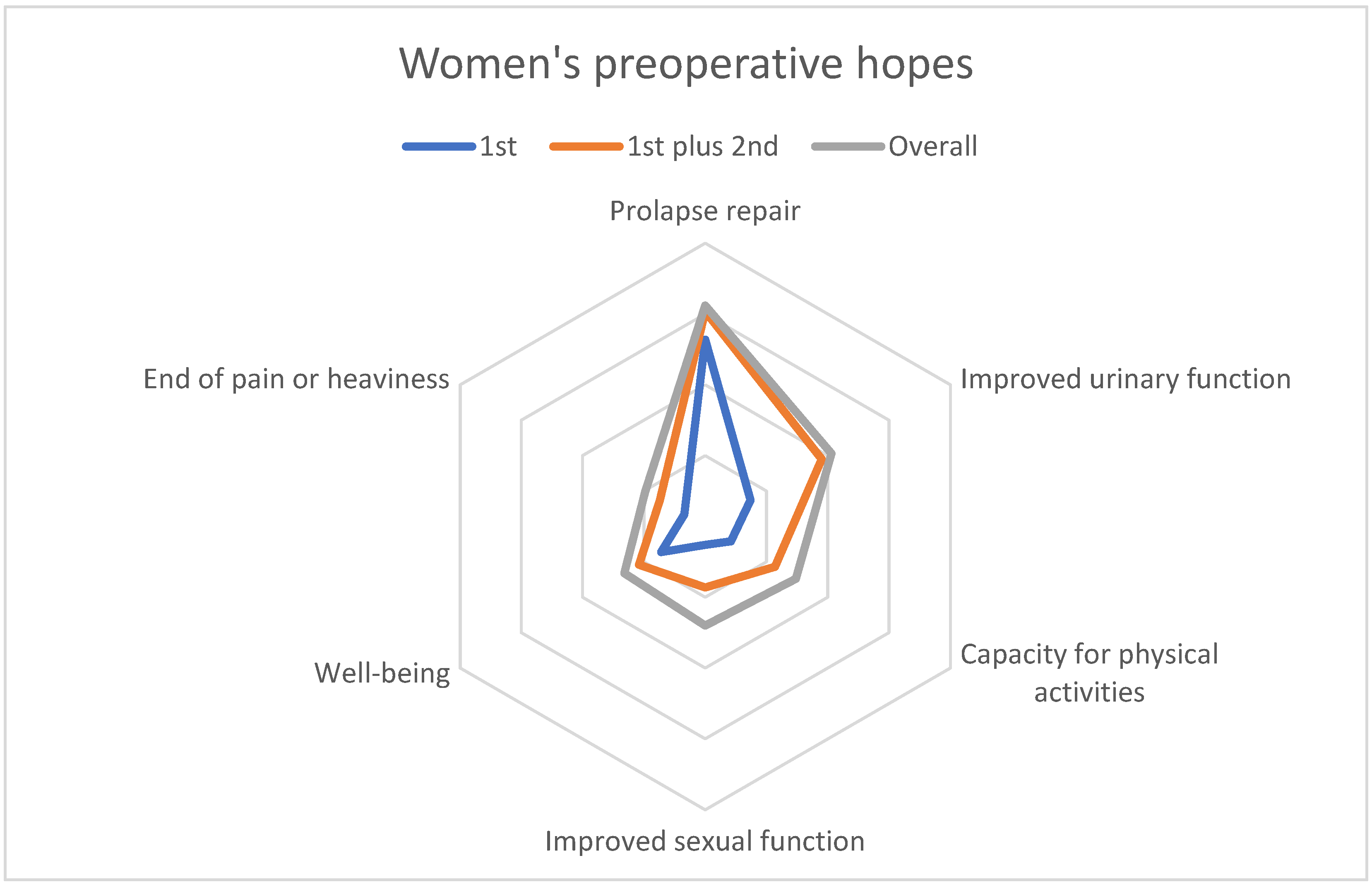
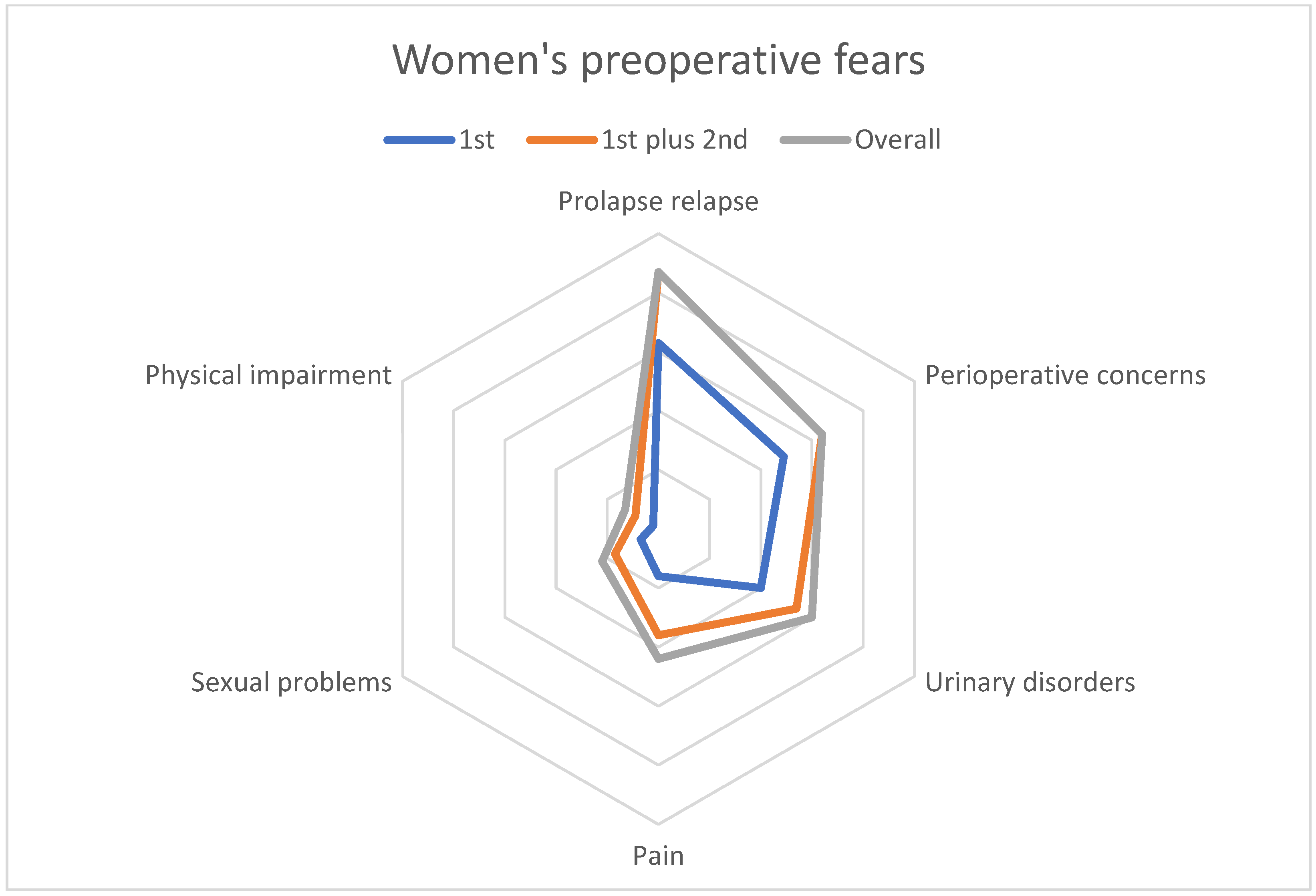
3.1. Qualitative Results for Women
3.2. Quantitative Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fritel, X.; Varnoux, N.; Zins, M.; Bréart, G.; Ringa, V. Symptomatic pelvic organ prolapse at midlife, quality of life, and risk factors. Obstet. Gynecol. 2009, 113, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Smith, F.J.; Holman, C.D.; Moorin, R.E.; Tsokos, N. Lifetime Risk of Undergoing Surgery for Pelvic Organ Prolapse. Obstet. Gynecol. 2010, 116, 1096–1100. [Google Scholar] [CrossRef] [PubMed]
- Fritel, X.; Panjo, H.; Varnoux, N.; Ringa, V. The individual determinants of care-seeking among middle-aged women reporting urinary incontinence: Analysis of a 2273-woman cohort. Neurourol. Urodyn. 2014, 33, 1116–1122. [Google Scholar] [CrossRef] [PubMed]
- Fauconnier, A.; Staraci, S.; Huchon, C.; Roman, H.; Panel, P.; Descamps, P. Comparison of patient- and physician-based descriptions of symptoms of endometriosis: A qualitative study. Hum. Reprod. 2013, 28, 2686–2694. [Google Scholar] [CrossRef] [PubMed]
- Barber, M.D.; Brubaker, L.; Nygaard, I.; Wheeler, T.L., 2nd; Schaffer, J.; Chen, Z.; Spino, C. Defining Success After Surgery for Pelvic Organ Prolapse. Obstet. Gynecol. 2009, 114, 600–609. [Google Scholar] [CrossRef] [PubMed]
- Digesu, A.; Chaliha, C.; Salvatore, S.; Hutchings, A.; Khullar, V. The relationship of vaginal prolapse severity to symptoms and quality of life. BJOG 2005, 112, 971–976. [Google Scholar] [CrossRef] [PubMed]
- Braddock, C.H., 3rd; Edwards, K.A.; Hasenberg, N.M.; Laidley, T.L.; Levinson, W. Informed decision making in outpatient practice: Time to get back to basics. JAMA 1999, 282, 2313–2320. [Google Scholar] [CrossRef] [PubMed]
- Lucot, J.P.; Cosson, M.; Bader, G.; Debodinance, P.; Akladios, C.; Salet-Lizée, D.; Delporte, P.; Savary, D.; Ferry, P.; Deffieux, X.; et al. Safety of Vaginal Mesh Surgery Versus Laparoscopic Mesh Sacropexy for Cystocele Repair: Results of the Prosthetic Pelvic Floor Repair Randomized Controlled Trial. Eur. Urol. 2018, 74, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Srikrishna, S.; Robinson, D.; Cardozo, L.; Cartwright, R. Experiences and expectations of women with urogenital prolapse: A quantitative and qualitative exploration. BJOG 2008, 115, 1362–1368. [Google Scholar] [CrossRef] [PubMed]
- Stöss, C.; Steffani, M.; Pergolini, I.; Hartmann, D.; Radenkovic, D.; Novotny, A.; Friess, H.; Müller, M.W. Impact of the COVID-19 Pandemic on Surgical Oncology in Europe: Results of a European Survey. Dig. Surg. 2021, 38, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Jacquetin, B.; Hinoul, P.; Gauld, J.; Fatton, B.; Rosenthal, C.; Clave, H.; Garbin, O.; Berrocal, J.; Villet, R.; Salet-Lizée, D.; et al. Total transvaginal mesh (TVM) technique for treatment of pelvic organ prolapse: A 5-year prospective follow-up study. Int. Urogynecol. J. 2013, 24, 1679–1686. [Google Scholar] [CrossRef] [PubMed]
- Olsen, A.; Smith, V.J.; Berstrom, J.O.; Colling, J.C.; Clark, A.L. Epidemilogy of surgically managed pelvic organ prolapse and incontinence. Obstet. Gynecol. 1997, 89, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Verbeek, M.; Hayward, L. Pelvic floor dysfunction and its effect on quality of sexual life. Sex. Med. Rev. 2019, 7, 559–564. [Google Scholar] [CrossRef] [PubMed]
- Jha, S.; Gray, T. A systematic review and meta-analysis of the impact of native tissue repair for pelvic organ prolapse on sexual function. Int. Urogynecol. J. 2015, 26, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Srikrishna, S.; Robinson, D.; Cardozo, L.; Thiagamoorthy, G. Patient and surgeon goal achievement 10 years following surgery for pelvic organ prolapse and urinary incontinence. Int. Urogynecol. J. 2015, 26, 1679–1686. [Google Scholar] [CrossRef] [PubMed]
- Lawndy, S.S.; Withagen, M.I.; Kluivers, K.B.; Vierhout, M.E. Between hope and fear: Patient’s expectations prior to pelvic organ prolapse surgery. Int. Urogynecol. J. 2011, 22, 1159–1163. [Google Scholar] [CrossRef] [PubMed]
- Baskayne, K.; Willars, J.; Pitchforth, E.; Tincello, D.G. Women’s Expectations of Prolapse Surgery: A Retrospective Qualitative Study. Neurourol. Urodyn. 2014, 33, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Hullfish, K.L.; Bovbjerg, V.E.; Gibson, J.; Steers, W.D. Patient-centered goals for pelvic floor dysfunction surgery: What is success, and is it achieved? Am. J. Obstet. Gynecol. 2002, 187, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Chattot, C.; Deffieux, X.; Lucot, J.P.; Fritel, X.; Fauconnier, A. Preoperative predictors and a prediction score for perception of improvement after mesh prolapse surgery. Int. Urogynecol. J. 2020, 31, 1393–1400. [Google Scholar] [CrossRef] [PubMed]

| Women Characteristics | N = 265 | |
|---|---|---|
| Age | median (range) | 64 (45–75) |
| Number of deliveries | median (range) | 2 (0–16) |
| POP-Q Stage—no. of patients (%) | 2 | 58 (21.9%) |
| 3 | 185 (69.8%) | |
| 4 | 21 (7.9%) | |
| PFDI 20 | means (±SD) | 94.32 (±50.67) |
| POPDI-6 | 43.81 (±22.24) | |
| DDI-8 | 16.25 (±16.18) | |
| UDI-6 | 34.25 (±25.98) | |
| EQ5D | means (±SD) | 0.78 (±0.20) |
| Hope Themes | Women | Surgeons |
|---|---|---|
| Prolapse repair | “no longer bulge out of my vagina”, “do not see this ball anymore”, “that my bladder is put back in place”, “stop having to push up my uterus”, “avoid this organ descent sensation”, “do not push back the ball in the vagina” | “no more vaginal ball” |
| Improved urinary function | “no more leakage”, “not have to go urinate every 5 min”, “fewer runs to the bathroom”, “urinate normally” | “reduction of urgency-pollakiuria”, “urinate easily” |
| Capacity for physical activities | “to return to normal physical activity”, “to walk and move normally”, “to regain my mobility” | “recovery of physical activity” |
| Improved sexual function | “resume my sex life”, “regain my femininity” | “more harmonious sexuality” |
| Well-being or comfort | “feel better”, “have a normal life”, “not have this embarrassment anymore” | “feel better” |
| End of pain or heaviness | “no more feeling of heaviness”, “no more pain in the lower abdomen” | “no longer feeling of heaviness” |
| Improved bowel function | “move my bowels correctly”, “no longer sitting on the toilet waiting for a bowel movement” | “move my bowels easily” |
| No more pads or other expectation | “not wearing pads anymore”, “no more irritation or burn”, “that the operation goes well” | - |
| Fears themes | ||
| Failure or prolapse relapse | “fear of relapse”, “afraid that the net does not hold” | “risk of recurrence”, “failure” |
| Perioperative concerns | “fear of anesthesia”, “afraid of not waking up”, “afraid of nausea on waking”, “postoperative problem”, “surgical complications” | “complication during the operation” |
| Urinary disorder | “being incontinent”, “continuing to smell the odor of pee!” | “risk of urinary leakage” |
| Pain | “fear of pain” | “fear of pain” |
| Sexual issues | “decreased sexual desire”, “won’t recover sexual desire” | “pain during sex” |
| Other fear | “that my belly will be even bigger”, “infection”, “health disorder”, “gynecologic problem”, “sequelae” | “infection” |
| Physical impairment | “Fear of not being able to resume my physical activities”, “stay physically diminished” | “duration of convalescence” |
| Mesh-related complications | “mesh exposure”, “fear the implant will be rejected” | “Serious adverse effect due to the mesh” |
| Worsened condition | “have to pay attention to everything”, “being worse after than before”, “fear of not recovering my general fairly satisfactory condition” | “worse than before” |
| Bowel problems | “constipation”, “afraid of more severe constipation” | “Improvement in anorectal disorders“ |
| No fears | “I’m not afraid, he knows what to do”, “I am confident that this operation will make me more comfortable” | - |
| Sample | Women (w)/Surgeons (s) | ||||||
|---|---|---|---|---|---|---|---|
| Hopes | 1st Nw/Ns 261/16 nw/ns | 2nd Nw/Ns 189/16 nw/ns | 3rd Nw/Ns 110/16 nw/ns | 4th Nw/Ns 40/16 nw/ns | 5th Nw/Ns 5/11 nw/ns | Overall * Women Nw = 261 nw (%) | Overall * Surgeons Ns = 16 ns (%) |
| Prolapse repair | 132/11 | 20/1 | 9/1 | 1/. | ./. | 156 (60) | 13 (81) |
| Improved urinary function | 37/. | 58/6 | 21/4 | 6/6 | ./. | 103 (39) | 15 (94) |
| Capacity for physical activities | 21/. | 36/4 | 23/3 | 11/2 | 3/3 | 74 (28) | 11 (69) |
| Improved sexual function | 13/. | 30/1 | 29/4 | 4/2 | 1/2 | 70 (27) | 9 (56) |
| Well-being or comfort | 36/5 | 18/2 | 16/1 | 7/1 | 2/2 | 66 (25) | 10 (62) |
| End of pain or heaviness | 17/. | 19/2 | 7/2 | 7/1 | ./1 | 49 (19) | 5 (31) |
| Improved bowel function | 3/. | 7/. | 4/1 | 3/3 | ./3 | 16 (6) | 7 (44) |
| No more pads or other | 1/. | 1/. | 2/. | ./1 | ./. | 3 (1) | 1 (6) |
| Sample | Women (w)/Surgeons (s) | ||||||
|---|---|---|---|---|---|---|---|
| Fears | 1st Nw/Ns 229/16 nw/ns | 2nd Nw/Ns 115/16 nw/ns | 3rd Nw/Ns 38/16 nw/ns | 4th Nw/Ns 18/15 nw/ns | 5th Nw/Ns 6/11 nw/ns | Summary * Women Nw = 229 nw (%) | Summary * Surgeons Ns = 16 ns (%) |
| Failure or prolapse relapse | 63/8 | 27/2 | 4/1 | ./2 | 2/3 | 87 (38) | 15 (94) |
| Perioperative concerns | 49/5 | 20/5 | 7/4 | 3/. | 1/. | 64 (28) | 14 (87) |
| Urinary disorders | 40/1 | 14/4 | 7/8 | ./2 | ./. | 60 (26) | 14 (87) |
| Pain | 16/1 | 20/3 | 5/2 | 4/4 | ./4 | 44 (19) | 10 (62) |
| Sexual problems | 7/1 | 10/. | 2/. | 2/3 | 1/3 | 22 (10) | 7 (44) |
| Other fear | 2/. | 7/. | 7/1 | 6/1 | 2/2 | 17 (7) | 3 (19) |
| Physical impairment | 2/. | 7/. | 4/. | ./1 | ./1 | 13 (6) | 1 (6) |
| Mesh-related | 5/. | 4/1 | 1/. | 1/1 | ./. | 11 (5) | 2 (12) |
| Worsened condition | 4/. | 2/1 | 1/. | 1/. | ./. | 7 (3) | 2 (12) |
| Bowel problems | 1/. | 3/. | ./. | 1/1 | ./1 | 5 (2) | 1 (6) |
| No fears | 40/. | 1/. | ./. | ./. | ./. | 40 (17) | . |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fritel, X.; Ravit, M.; Pizzoferrato, A.-C.; Campagne-Loiseau, S.; Bader, G.; Capmas, P.; Cosson, M.; Debodinance, P.; Deffieux, X.; Fernandez, H.; et al. Do Surgeons Anticipate Women’s Hopes and Fears Associated with Prolapse Repair? A Qualitative Analysis in the PROSPERE Trial. J. Clin. Med. 2023, 12, 1332. https://doi.org/10.3390/jcm12041332
Fritel X, Ravit M, Pizzoferrato A-C, Campagne-Loiseau S, Bader G, Capmas P, Cosson M, Debodinance P, Deffieux X, Fernandez H, et al. Do Surgeons Anticipate Women’s Hopes and Fears Associated with Prolapse Repair? A Qualitative Analysis in the PROSPERE Trial. Journal of Clinical Medicine. 2023; 12(4):1332. https://doi.org/10.3390/jcm12041332
Chicago/Turabian StyleFritel, Xavier, Marion Ravit, Anne-Cécile Pizzoferrato, Sandrine Campagne-Loiseau, Georges Bader, Perrine Capmas, Michel Cosson, Philippe Debodinance, Xavier Deffieux, Hervé Fernandez, and et al. 2023. "Do Surgeons Anticipate Women’s Hopes and Fears Associated with Prolapse Repair? A Qualitative Analysis in the PROSPERE Trial" Journal of Clinical Medicine 12, no. 4: 1332. https://doi.org/10.3390/jcm12041332
APA StyleFritel, X., Ravit, M., Pizzoferrato, A.-C., Campagne-Loiseau, S., Bader, G., Capmas, P., Cosson, M., Debodinance, P., Deffieux, X., Fernandez, H., Ferry, P., Garbin, O., Jacquetin, B., Legendre, G., Saussine, C., de Tayrac, R., Wagner, L., Lucot, J.-P., Fauconnier, A., & the PROSPERE team. (2023). Do Surgeons Anticipate Women’s Hopes and Fears Associated with Prolapse Repair? A Qualitative Analysis in the PROSPERE Trial. Journal of Clinical Medicine, 12(4), 1332. https://doi.org/10.3390/jcm12041332







