Jacob’s Disease: Case Series, Extensive Literature Review and Classification Proposal
Abstract
1. Introduction
2. Review of the Literature
3. Case Presentation
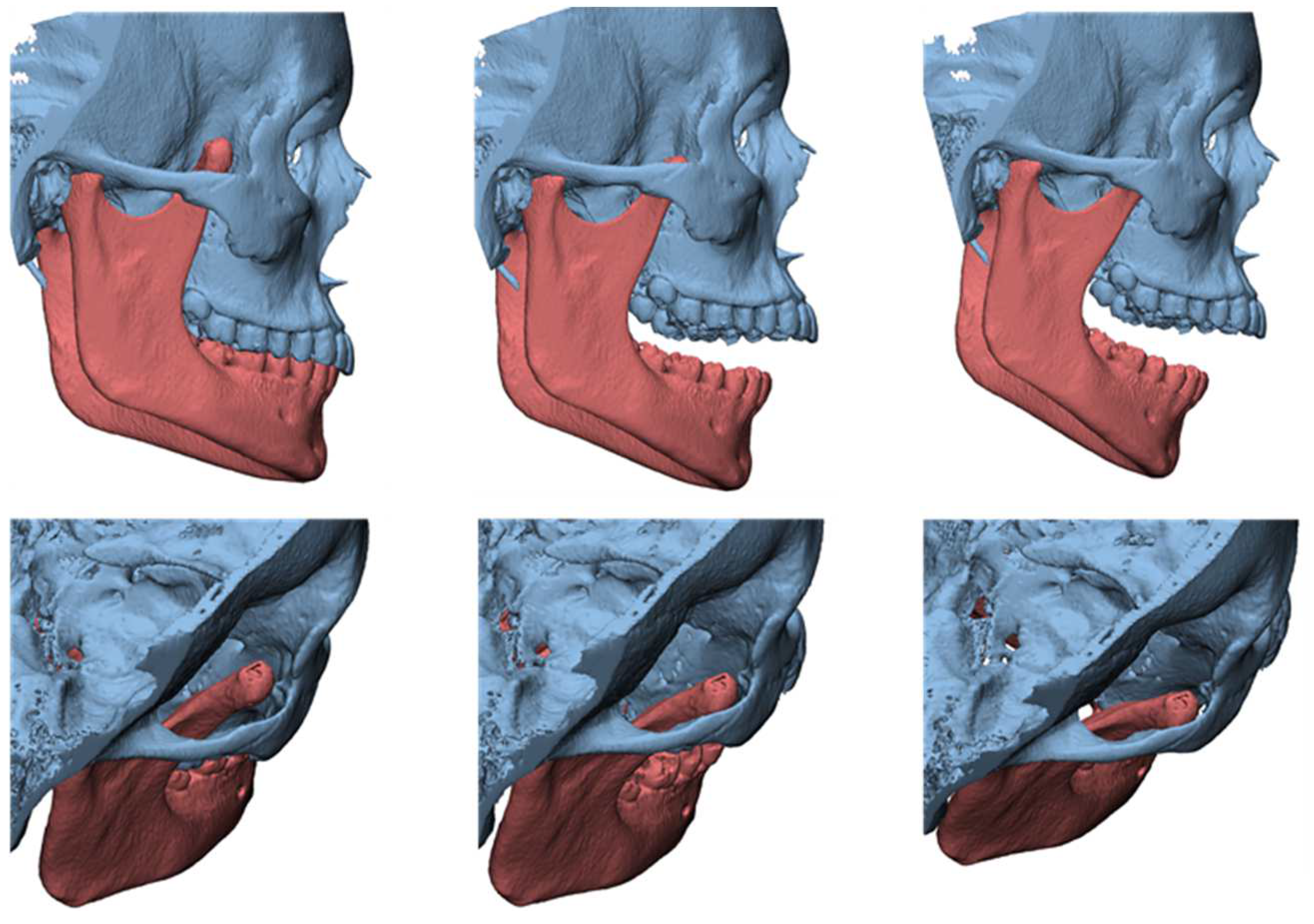
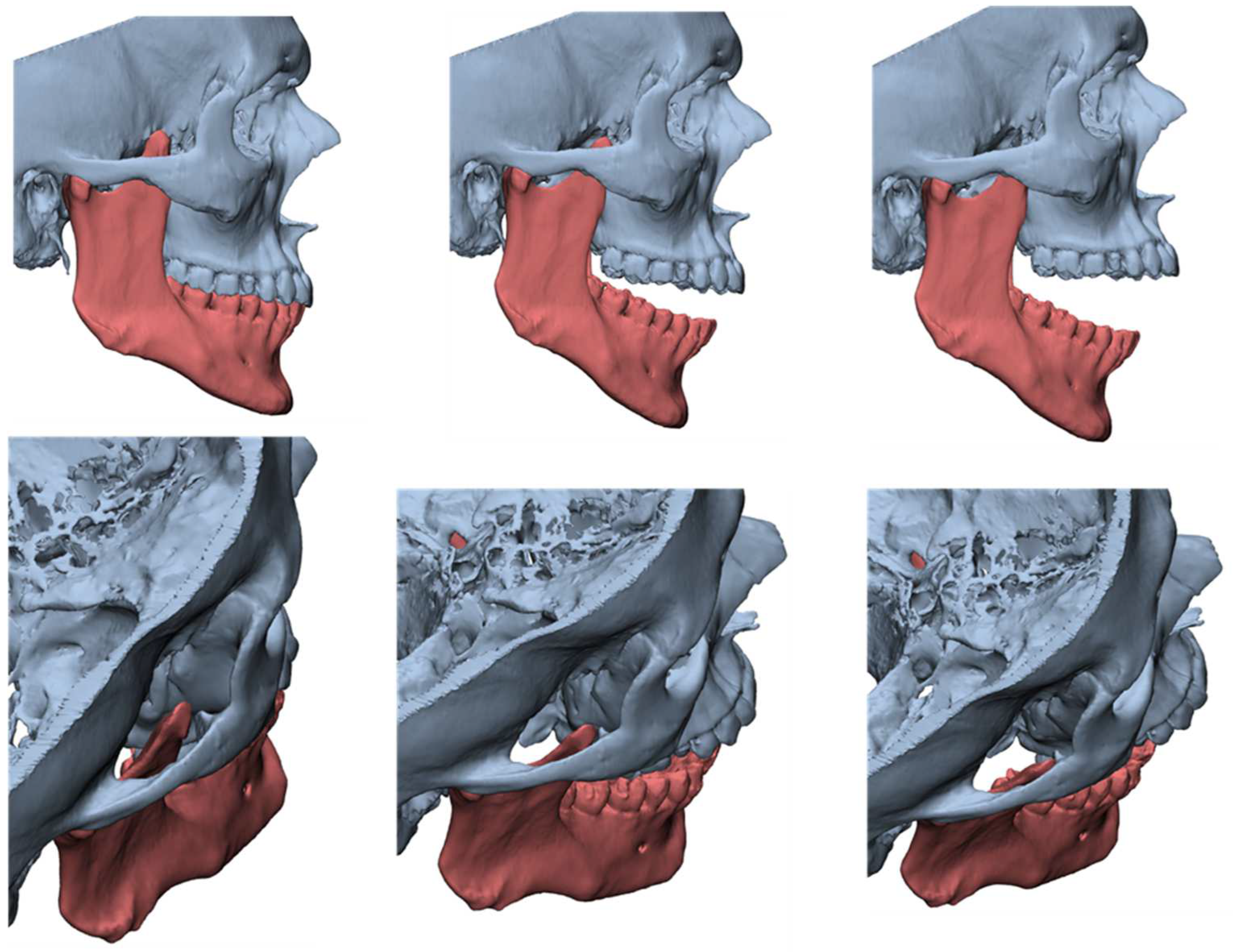
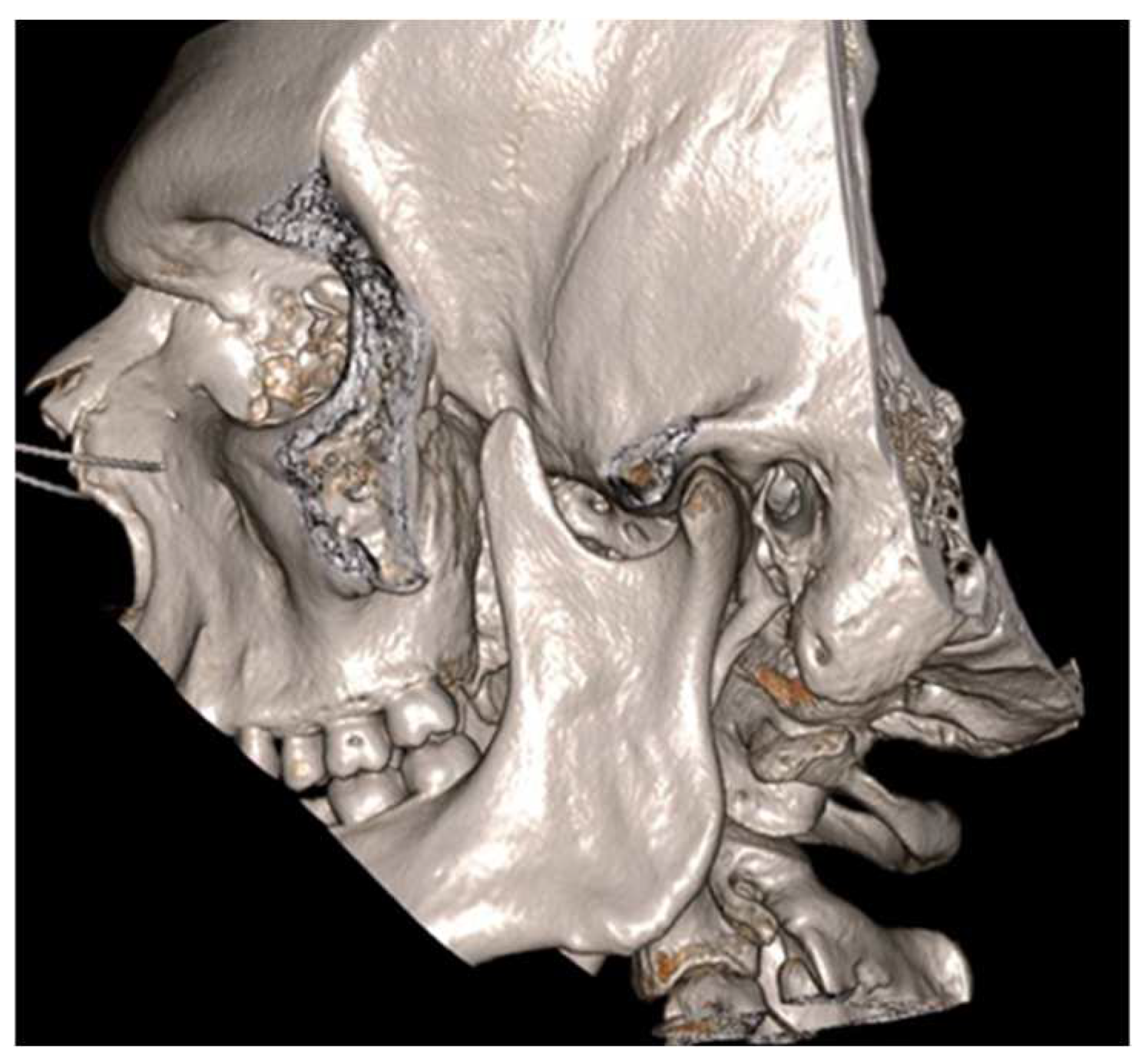
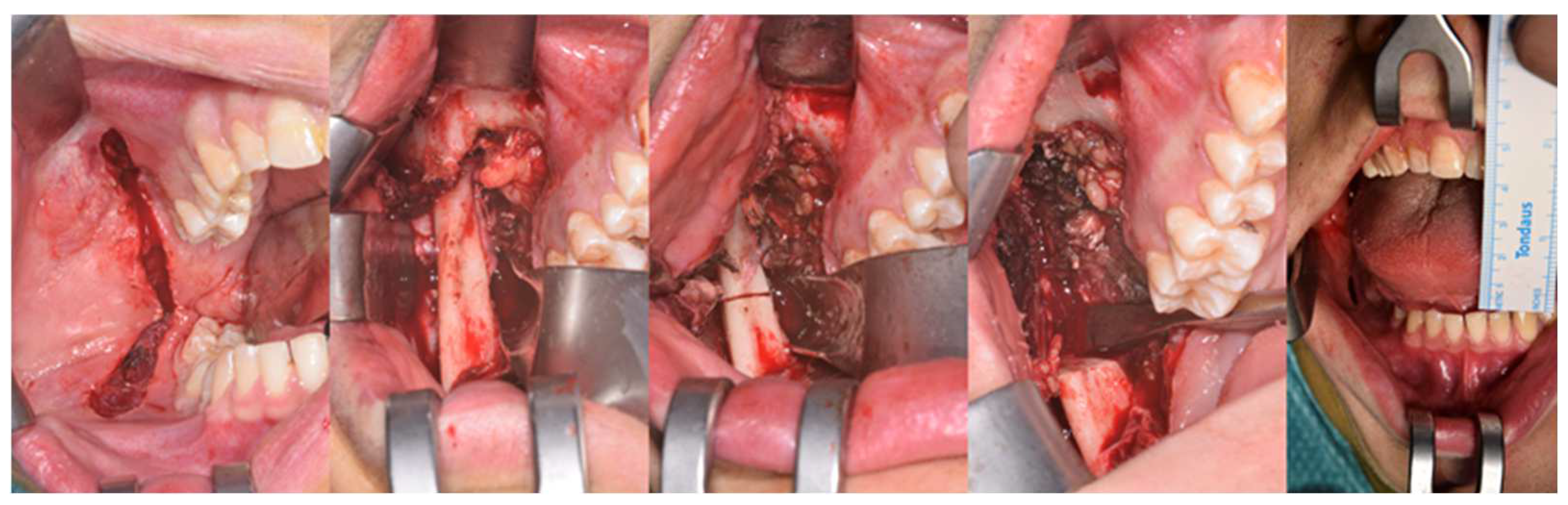
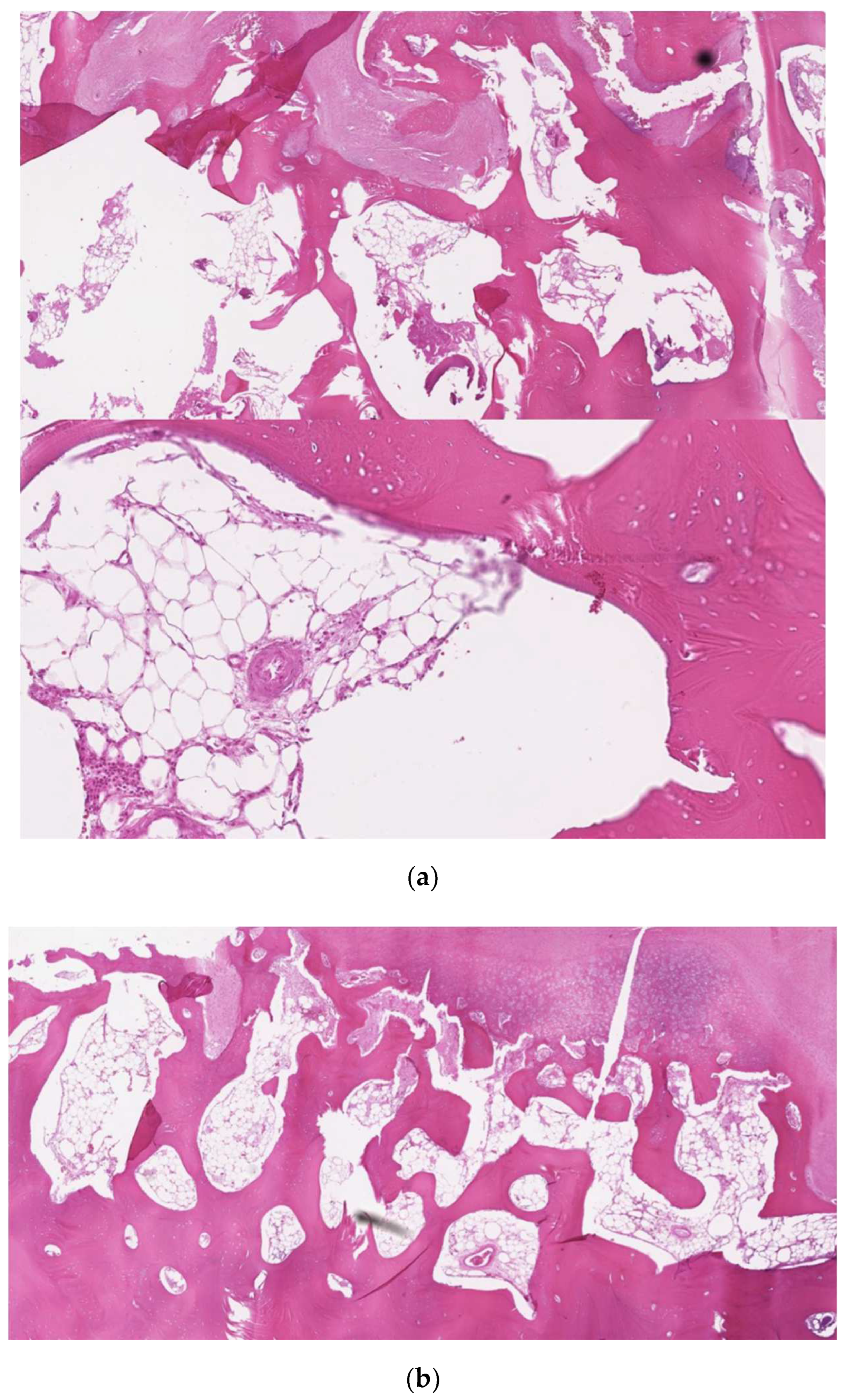
3.1. Case 1
3.2. Case 2
3.3. Case 3
4. Results and Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jacob, O. Une cause rare de constriction permanente des machoires. Bull. Mem. Soc. Anat. Paris 1899, 1, 917. [Google Scholar]
- Langenbeck, B. Angeborene Kleinert der Unterkiefer. Langenbecks Arch. 1861, 1, 451. [Google Scholar]
- McLoughlin, P.; Hopper, C.; Bowley, N. Hyperplasia of the mandibular coronoid process: An analysis of 31 cases and a review of the literature. J. Oral Maxillofac. Surg. 1995, 53, 250–255. [Google Scholar] [CrossRef]
- Emekli, U.; Aslan, A.; Onel, D.; Cizmeci, O.; Demiryont, M. Osteochondroma of the coronoid process (Jacob’s disease). J. Oral Maxillofac. Surg. 2002, 60, 1354–1356. [Google Scholar] [CrossRef]
- Patel, R.; Obeid, G. Osteochondroma of the Zygomatic Arch: A Case Report and Review of the Literature. J. Oral Maxillofac. Surg. 2018, 76, 1912–1916. [Google Scholar] [CrossRef]
- Roychoudhury, A.; Gupta, Y.K.; Parkash, H.; Karak, A.K. Jacob disease: Report of a case and review of the literature. J. Oral Maxillofac. Surg. 2002, 60, 699–703. [Google Scholar] [CrossRef]
- Sreeramaneni, S.K.; Chakravarthi, P.S.; Krishna Prasad, L.; Raja Satish, P.; Beeram, R.K. Jacob’s disease: Report of a rare case and literature review. Int. J. Oral Maxillofac. Surg. 2011, 40, 753–757. [Google Scholar] [CrossRef]
- Hernández-Alfaro, F.; Escuder, O.; Marco, V. Joint formation between an osteochondroma of the coronoid process and the zy-gomatic arch (Jacob disease): Report of case and review of literature. J. Oral Maxillofac. Surg. 2000, 58, 227–232. [Google Scholar] [CrossRef]
- Jha, A.; Gupta, P.; Khalid, M.; Naseem, I.; Gupta, G. Sarcomatous Transformation of Osteochondroma of the Coronoid Process Forming Pseudoarthrosis with Zygomatic Arch Mistaken for Jacob Disease. J. Craniofac. Surg. 2014, 25, e101–e102. [Google Scholar] [CrossRef]
- Peacock, Z.S.; Resnick, C.; Faquin, W.C.; Kaban, L.B. Accessory Mandibular Condyle at the Coronoid Process. J. Craniofac. Surg. 2011, 22, 2168–2171. [Google Scholar] [CrossRef]
- Capote, A.; Rodríguez, F.J.; Blasco, A.; Muñoz, M.F. Jacob’s disease associated with temporomandibular joint dysfunction: A case report. Med. Oral Patol. Oral Cir. Bucal. 2005, 10, 210–214. [Google Scholar]
- Coll Anglada, M.; Acero Sanz, J.; Vila Masana, I.; Navarro Cuéllar, C.; Ochandiano Caycoia, S.; López de Atalaya Gutiérrez, J.; Navarro Vila, C. Jacob’s disease secondary to coronoid process osteochondroma. A case report. Med. Oral Patol. Oral Cir. Bucal 2011, 15, e708Ye710. [Google Scholar]
- D’Ambrosio, N.; Kellman, R.M.; Karimi, S. Osteochondroma of the coronoid process (Jacob’s disease): An unusual cause of re-stricted jaw motion. Am. J. Otolaryngol. 2011, 32, 52Y54. [Google Scholar] [CrossRef]
- Escuderi de la Torre, O.; Vert Klok, E.; Mari i Roig, A.; Mommaerts, M.Y.; Pericot i Ayats, J. Jacob’s disease: Report of two cases and review of the literature. J. Craniomaxillofac. Surg. 2001, 29, 372Y376. [Google Scholar]
- Shackelford, R.T.; Brown, W.H. Osteochondroma of the coronoid process of the mandible. Surg. Gynecol. Obstet. 1943, 77, 51–54. [Google Scholar]
- Brandt, K. Deformation congenitale de l’apophyse coronoid du maxillaire inferieur. Acta Orthop. Scand. 1943, 14, 219–324. [Google Scholar] [CrossRef]
- Hallam, J.W. Exostosis of the coronoid process of the mandible and true joint formation with zygomatic arch; case report. Br. J. Surg. 1947, 34, 432. [Google Scholar] [CrossRef]
- Shackelford, R.T.; Brown, W.H. Restricted jaw motion due to ostcochondroma of the coronoid process. J. Bone Jt. Surg. 1949, 31, 107–114. [Google Scholar] [CrossRef]
- Brailsford, F.J. An Unusual Osteochondroma from the Coronoid Process of the Mandible. Br. J. Radiol. 1952, 25, 555–556. [Google Scholar] [CrossRef]
- Holmes, F.H. Mandibular Block by Osteochondroma of the Coronoid Processes. Radiology 1956, 67, 578–580. [Google Scholar] [CrossRef]
- Ginestet, G.; Dupuis, A.; Merville, L.; Guerin, J.; Dondey, P.L. Constriction des machoires d’origine coronoıdo-malaire. Bulletin officiel de la societe’ de Stomatologie et de Chirurgie Maxillo-Faciale de France. Rev. Stomatol. 1957, 58, 233–237. [Google Scholar]
- Van Zile, W.N.; Johnson, W.B. Bilateral coronoid process exostoses simulating partial ankylosis of the temporoman-dibular joint. J. Oral Surg. 1957, 15, 72–77. [Google Scholar]
- Levine, M.H.; Chessen, J.; McCarty, W.D. Osteochondroma of the coronoid process of the mandible. N. Engl. J. Med. 1957, 257, 374–376. [Google Scholar] [CrossRef]
- Dingman, R.O.; Natvig, P. Reduced mandibular motion due to osteochondroma of the coronoid process of the mandible. Am. J. Surg. 1957, 94, 907–910. [Google Scholar] [CrossRef]
- Pap, C.; Friedmann, E. Restricted mandibular movements due to osteochondroma of the coronoid process. Br. J. Plast. Surg. 1958, 11, 169–173. [Google Scholar] [CrossRef]
- Antoni, A.A.; Johnson, J.H. Osteochondroma of the coronoid process of the mandible. J. Oral Surg. 1958, 16, 514–517. [Google Scholar]
- Chemin, J.; Bercher, J.; Ginestet, G. La maladie de O. Jacob. Cah Odonto-Stomatol. 1958, 8, 17–33. [Google Scholar]
- Shira, R.B.; Lister, R.L. Limited mandibular movements due to enlargement of the coronoid processes. J. Oral Surg. 1958, 16, 183–191. [Google Scholar]
- Lebo, C.P. Osteochondroma of the mandibular coronoid process. A report of one case and a review of the literature. Laryngoscope 1961, 71, 814–822. [Google Scholar] [CrossRef]
- Mohnac, A.M. Bilateral coronoid osteochondromas. J. Oral Surg. 1962, 20, 500–506. [Google Scholar]
- Van de Vijver, L.M. Een zeldzame van beperking van de mondopening: De zietke van O. Jacob. Acta Stomatol. Belg. 1962, 59, 187–193. [Google Scholar]
- Dechaume, M.; Grellet, M.; Bonneau, M.; Payen, J.; Cayron, R.; Guilbert, F. Constriction permanente des maˆchoires d’origine extra-articulaire coronoıdo-malaire: Maladie de Jacob. Rev. Stomatol. 1964, 65, 513–518. [Google Scholar]
- Rottke, B.; Dunker, R. Ein Beitragzuden Spatfolgenunbehandelter Frakturen im Jochbogenbereich. Kiefer Gesichtschir 1967, 12, 123–125. [Google Scholar]
- Allan, I.M.D.B.; Reid, W.H. Unilateral exostosis of the coronoid process of the mandible: A report of two cases. Br. J. Oral Surg. 1967, 5, 20–24. [Google Scholar] [CrossRef]
- Meyer, R.A. Osteochondroma of Coronoid Process of the Mandible: Report of a Case. J. Oral Surg. 1972, 30, 297–300. [Google Scholar]
- James, R.B.; Alexander, R.W.; Traver, J.G. Osteochondroma of the mandibular coronoid process: Report of a case. Oral Surg. Oral Med. Oral Pathol. 1974, 37, 189–195. [Google Scholar] [CrossRef]
- Cooper, J.C.; Finch, C.D. Coronoid Osteochondroma Presenting as a Corono-zygomatic Ankylosis. Br. Dent. J. 1974, 137, 99–102. [Google Scholar] [CrossRef]
- Takeda, S.; Osanai, G.; Morita, T.; Kitawada, S.; Takizawa, T.; Hirabayashi, Y.; Kotani, A. Osteochondroma of the left coronoid process followed by extremely restricted mandibular movement: Report of a case. Jpn. J. Oral Maxillofac. Surg. 1975, 21, 580–586. (In Japanese) [Google Scholar] [CrossRef]
- Singer, R.; Schulz, P. Eingeschr~inkte MundiSffnung durch Hyperplasie oder Osteochondrom des Processus coronoideus; Literaturiibersicht. ZWR 1976, 85, 685–690. [Google Scholar]
- Ramon, Y.; Horowitz, I.; Oberman, M.; Freedman, A.; Tadmor, R. Osteochondroma of the coronoid process of the mandible. Oral Surg. Oral Med. Oral Pathol. 1977, 43, 692–697. [Google Scholar] [CrossRef]
- Michel, R.G.; Hudson, W.R.; Drawbaugh, E.J.; Baylin, G.J. Exostosis of the Mandibular Coronoid Process. Ann. Otol. Rhinol. Laryngol. 1977, 86, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Norman, J.E.B.; Painter, D.M. Hyperplasia of the mandibular condyle. A historical review of important early cases with a presentation and analysis of twelve patients. J. Maxillofac. Surg. 1980, 8, 161–175. [Google Scholar] [PubMed]
- Ito, N.; Otsu, T.; Fujioka, Y.; Takeda, Y.; Suzuki, A. Osteochondroma of the coronoid process of the mandible: Report of a case and a review of the literature. Jpn. J. Oral Maxillofac. Surg. 1981, 27, 863–872. (In Japanese) [Google Scholar] [CrossRef]
- Boland, T.; Beirne, O.R. Zygomatic exostosis. Int. J. Oral Surg. 1983, 12, 124–126. [Google Scholar] [CrossRef]
- Ishii, J.; Amagasa, T.; Akashi, K.; Shioda, S.; Yuki, K. Restricted jaw movement due to osteochondroma of the mandibular co-ronoid process: Report of two cases. Jpn. J. Oral Maxillofac. Surg. 1983, 29, 507–513. (In Japanese) [Google Scholar] [CrossRef]
- Revington, P.J. ‘Turret exostosis’ of the coronoid process. Br. J. Oral Maxillofac. Surg. 1984, 22, 37–41. [Google Scholar] [CrossRef]
- Tucker, M.R.; Guilford, W.B.; Howard, C.W. Coronoid process hyperplasia causing restricted opening and facial asymmetry. Oral Surg. 1984, 58, 130–132. [Google Scholar] [CrossRef]
- MacLeod, A.W.G. Limitation of mandibular opening due to enlarged coronoid processes. Aust. Dent. J. 1987, 32, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, H.C. Use of the hemicoronal flap to approach the coronoid process. J. Oral Maxillofac. Surg. 1988, 46, 519. [Google Scholar] [CrossRef]
- Halling, F.; Kuhn, D.; Gaebel, M. Einseitige Hypertrophie des Processus coronoideus mit Gesichtsasymmetrie. Ein Fallbericht Unilateral hypertrophy of the coronoid process associated with facial asymmetry. Case report. Dtsch. Z. Mund. Kiefer. Gesichtschir. 1989, 13, 377–381. [Google Scholar]
- Goudot, P.; Guilbert, F.; Buthiau, D.; Auriol, M. Apport de l’imagerie moderne dans l’exploration des dysmorphoses corono-ïdo-malaires. A propos de deux cas. Value of modern imagery in the study of coronoido-malar malformations. Apropos of 2 cases. Rev. Stomatol. Chir. Maxillofac. 1989, 90, 424–427. [Google Scholar] [PubMed]
- Totsuka, Y.; Fukuda, H.; Iizuka, T.; Shindoh, M.; Amemiya, A. Osteochondroma of the coronoid process of the mandible. Report of a case showing histological evidence of neoplasia. J. Craniomaxillofac. Surg. 1990, 18, 27–32. [Google Scholar] [CrossRef]
- Rames, P.; Urban, F. Hyperplasia of the coronoid processes of the mandible—Case-history. Prakt. Zubn. Lek. 1990, 38, 277–280. [Google Scholar]
- Asanami, S.; Kasazaki, Y.; Uchida, I. Large exostosis of the mandibular coronoid process. Report of a case. Oral Surg. Oral Med. Oral Pathol. 1990, 69, 559–562. [Google Scholar] [CrossRef]
- Hönig, J.F.; Merten, H.A.; Korth, O.E.; Halling, F. Coronoid process enlargement. Dentomaxillofac. Radiol. 1994, 23, 108–110. [Google Scholar] [CrossRef]
- Kerscher, A.; Piette, E.; Tideman, H.; Wu, P. Osteochondroma of the coronoid process of the mandible: Report of a case and review of the literature. Oral Surg. Oral Med. Oral Pathol. 1993, 75, 559–564. [Google Scholar] [CrossRef]
- Smyth, A.; Wake, M. Recurrent bilateral coronoid hyperplasia: An unusual case. Br. J. Oral Maxillofac. Surg. 1994, 32, 100–104. [Google Scholar] [CrossRef]
- Gibbons, A.J. Case report: Computed tomography in the investigation of bilateral mandibular coronoid hyperplasia. Br. J. Radiol. 1995, 68, 531–533. [Google Scholar] [CrossRef]
- Cenetoglu, S.; Yavuzert, R.; Oygiir, T.; Akyol, G.; Baran, N.K. Osteochondroma of the coronoid process of the mandible. Eur. J. Plast. Surg. 1996, 19, 333–334. [Google Scholar] [CrossRef]
- Kermer, C.; Rasse, M.; Undt, G.; Lang, S. Cartilaginous exostoses of the mandible. Int. J. Oral Maxillofac. Surg. 1996, 25, 373–375. [Google Scholar] [CrossRef]
- Mizumoto, T.; Hamakawa, H.; Miyoshi, T.; Takarada, M.; Tanioka, H.; Hatakeyama, T. A case of osteochondroma of the coronoid process in which the zygomatic arch was reconstructed with an outer cortical layer of the frontal bone. Jpn. J. Oral Maxillofac. Surg. 1996, 42, 185–187. [Google Scholar] [CrossRef]
- Constantinides, M.; Lagmay, V.; Miller, P. Coronoid osteochondroma of the mandible: Transzygomatic access and autogenous bony reconstruction. Otolaryngol. Head Neck Surg. 1997, 117, S86–S91. [Google Scholar] [CrossRef]
- Gross, M.; Gavish, A.; Calderon, S.; Gazit, E. The coronoid process as a cause of mandibular hypomobility—Case reports. J. Oral Rehabil. 1997, 24, 776–781. [Google Scholar] [CrossRef]
- Chen, P.K.-T.; Chang, S.C.-N.; Huang, F.; Chen, Y.-R.; Yeow, V.K.; Williams, W.G. Transzygomatic Coronoidectomy through an Extended Coronal Incision for Treatment of Trismus Due to an Osteochondroma of the Coronoid Process of the Mandible. Ann. Plast. Surg. 1998, 41, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Toshihiko, T.; Yoshihiko, F.; Norio, A.; Motohiro, K.; Masaharu, M. A case of osteochondroma of the coronoid process of the mandible. Jpn. J. Oral Maxillofac. Surg. 1998, 44, 762–764. [Google Scholar]
- Manganaro, A.M. Osteochondroma of the coronoid process. Gen. Dent. 1998, 46, 92–94. [Google Scholar] [PubMed]
- Ishii, H.; Shimizu, H.; Kasahara, H.; Sasaki, S.; Goke, H.; Seto, K. Restricted jaw movement due to unilateral hyperplasia of the mandibular coronoid process: Report of a case. Jpn. J. Oral Maxillofac. Surg. 1998, 44, 85–87. [Google Scholar] [CrossRef]
- Chichareon, V.; Arpornmaeklong, P.; Donsakul, N. Osteochondroma of the coronoid process in child. Plast. Reconstr. Surg. 1999, 103, 1238–1243. [Google Scholar] [CrossRef]
- Matsumoto, G.; Suga, M.; Lee, U.; Matsuzawa, S.; Kubota, N.; Kubota, E. Osteochondroma on the Coronoid Process of the Mandible. Asian J. Oral Maxillofac. Surg. 2005, 17, 121–124. [Google Scholar] [CrossRef]
- Akan, H.; Mehreliyeva, N. The value of three-dimensional computed tomography in diagnosis and management of Jacob’s disease. Dentomaxillofac. Radiol. 2006, 35, 55–59. [Google Scholar] [CrossRef]
- Villanueva, J.; Gonzalez, A.; Cornejo, M.; Nunez, C.; Encina, S. Osteochondroma of the coronoid process. Med. Oral Pathol. Oral Cir. Bucal 2006, 11, E289–E291. [Google Scholar]
- DeDe, U.; Tuzuner, A.; Kisnisci, R. Osteochondroma of coronoid process: Jacob’s disease. Int. J. Oral Maxillofac. Surg. 2007, 36, 1101. [Google Scholar] [CrossRef]
- Zhong, S.-C.; Xu, Z.-J.; Zhang, Z.-G.; Zheng, Y.-H.; Li, T.-X.; Su, K. Bilateral coronoid hyperplasia (Jacob disease on right and elongation on left): Report of a case and literature review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2009, 107, e64–e67. [Google Scholar] [CrossRef]
- Thota, G.; Cillo, J.E.; Krajekian, J.; Dattilo, D.J. Bilateral Pseudojoints of the Coronoid Process (Jacob Disease): Report of a Case and Review of the Literature. J. Oral Maxillofac. Surg. 2009, 67, 2521–2524. [Google Scholar] [CrossRef]
- Osman, A.; Alper, A.; Ali, Y. Osteochondroma of the mandibular coronoid process: A rare cause of limited mouth opening. Br. J. Oral Maxillofac. Surg. 2009, 47, 409–411. [Google Scholar]
- Yesildag, A.; Yariktas, M.; Doner, F.; Aydin, G.; Munduz, M.; Topal, U. Osteochondroma of the Coronoid Process and Joint Formation with Zygomatic Arch (Jacob Disease): Report of a Case. Eur. J. Dent. 2010, 4, 91–94. [Google Scholar] [CrossRef]
- Hiroyuki, T.; Kazuma, F.; Katu, T.; Masasi, Y.; Yasunori, O.; Kazuhisa, B. A case of oste-ochondroma of the coronoid process. Jpn. J. Oral Maxillofac. Surg. 2011, 57, 25–29. [Google Scholar]
- Ajila, V.; Hegde, S.; Gopakumar, R.; Babu, G.S. Imaging and Histopathological Features of Jacob’s Disease: A Case Study. Head Neck Pathol. 2011, 6, 51–53. [Google Scholar] [CrossRef]
- Acosta-Feria, M.; Villar-Puchades, R.; Haro-Luna, J.J.; Ramos-Medina, B.; García-Solano, E. Limitation of mouth opening caused by osteochondroma of the coronoid process. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2011, 112, e64–e68. [Google Scholar] [CrossRef]
- Aoki, N.; Okamura, K.; Niino, D.; Iwamoto, O.; Kusukawa, J. Osteochondroma of the right coronoid process (Jacob disease): A case report. Cranio 2013, 31, 66–69. [Google Scholar] [CrossRef]
- Ruiz, L.P.; Lara, J.C. Craniomaxillofacial features in hereditary multiple exostosis. J. Craniofac. Surg. 2012, 23, e336–e338. [Google Scholar] [CrossRef]
- Tavassol, F.; Spalthoff, S.; Essig, H.; Bredt, M.; Gellrich, N.C.; Kokemüller, H. Elongated coronoid process: CT-based quantitative analysis of the coronoid process and review of literature. Int. J. Oral Maxillofac. Surg. 2012, 41, 331–338. [Google Scholar] [CrossRef]
- Choi, J.G.; Kim, S.Y.; Perez-Atayde, A.R.; Padwa, B.L. Bilateral coronoid process hyperplasia with pseudocartilaginous joint formation: Jacob disease. J. Oral Maxillofac. Surg. 2013, 71, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Stringer, D.E.; Chatelain, K.B.; Tandon, R. Surgical Treatment of Jacob’s Disease: A Case Report Involving an Osteochondroma of the Coronoid Process. Case Rep. Surg. 2013, 2013, 253740. [Google Scholar] [CrossRef]
- Hosein, M.M. Osteochondromatosis and the coronoid-zygomatic pseudojoint (Jacob’s disease) as an unusual cause of midfacial asymmetry and jaw restriction. Pak. Oral Dent. J. 2013, 33, 232–235. [Google Scholar]
- Losa-Muñoz, P.M.; Burgueño-García, M.; González-Martín-Moro, J.; Sánchez-Burgos, R. Osteochondroma of coronoid process: A rare etiology of jacob disease. Craniomaxillofac. Trauma Reconstr. 2014, 7, 306–309. [Google Scholar] [CrossRef]
- Dandriyal, R.; Giri, K.Y.; Pant, S.; Alam, S.; Joshi, A. Giant osteo-chondroma of the coronoid process. J. Maxillofac. Oral Surg. 2015, 14, S412–S416. [Google Scholar] [CrossRef]
- Zarembinski, C.; Graff-Radford, S. An unusual challenge in performing sphenopalatine ganglion block with enlarged coronoid process: Jacob’s disease. Pain Med. 2014, 15, 329–332. [Google Scholar] [CrossRef]
- Fan, H.; Lv, X.; Shi, J.; Hu, J.; Luo, E. One-stage treatment to osteochondroma of the coronoid process and secondary facial asymmetry with coronoidectomy and reduction malarplasty: A case report and literature review. J. Oral Maxillofac. Surg. 2014, 72, 1870.e1–1870.e13. [Google Scholar] [CrossRef]
- Rahim, I.; Balasundaram, I.; Kanzaria, A.; Kane, S.; Bridle, C. Jacob’s Disease: An Exceedingly Rare Cause of Limited Mouth Opening. Br. J. Oral Maxillofac. Surg. 2014, 52, e113. [Google Scholar] [CrossRef]
- Reddy, N.V.; Rajan, R.; Rachalapally, V.K.; Kallam, S.R. Jacob’s disease: A rare case report. J. NTR Univ. Health Sci. 2014, 3, 202–205. [Google Scholar] [CrossRef]
- Sinha, S.K.; Kumar, S. Osteochondroma of Coronoid Process and Joint Formation with Zygomatic Arch (Jacob Disease): A Rare Case Report. Int. J. Sci. Study 2014, 1, 63–65. [Google Scholar]
- Sawada, K.; Schulze, D.; Matsumoto, K.; Hirai, S.; Hashimoto, K.; Honda, K. Osteochondroma of the coronoid process of the mandible. J. Oral Sci. 2015, 57, 389–392. [Google Scholar] [CrossRef]
- Shin, D.W.; Kim, J.E.; Kim, H.S.; Lee, H. Jacob’s disease: Report of a case. Cranio 2017, 35, 58–63. [Google Scholar] [CrossRef]
- Mohanty, S.; Gupta, H.; Dabas, J.; Kumar, P. Osteochondroma of maxillofacial region: Tumor arising from two different developmental bones. J. Oral Maxillofac. Pathol. 2016, 20, 329. [Google Scholar] [CrossRef]
- Robiony, M.; Casadei, M.; Scott, C.A.; Chiarini, L. Progressive Limitation in Mouth Opening: Jacob Disease. J. Craniofac. Surg. 2016, 27, 821. [Google Scholar] [CrossRef] [PubMed]
- Imen, C.; Zouha, M.; Ahmed, Z.; Dorra, C.; Habib, K.; Touhami, B.A. Clinical and radiological features of Jacob’s disease.A case report involving an osteochondroma of the coronoid process. Méd. Buccale Chir. Buccale 2016, 22, 145–149. [Google Scholar] [CrossRef]
- Gangoli, N.; Meara, D.J. Osteochondroma of Coronoid Process in a Pediatric Patient: Treatment and Literature Review of Jacob’s Disease. J. Oral Maxillofac. Surg. 2017, 75, e393–e394. [Google Scholar] [CrossRef]
- Choontharu, M.M.; Buch, S.A.; Babu, G.S.; Castelino, R.L.; Rao, S.; Rao, K. A Rare Clinical Presentation of an Osteochondroma of Coronoid Process of Mandible. J. Dent. 2018, 19, 325–330. [Google Scholar]
- Roscher, D.; Attaguile, A.; Benitez, J.; Giannunzio, G. Jacob’s Disease: A Case Report and Literature Review. Dentistry 2018, 8, 1000485. [Google Scholar] [CrossRef]
- Villegas Cisneros, A.; Miranda Villasana, E.; Varela Ibáñez, E. Bilateral hyperplasia of the coronoid process. Clinical case report with unusual presentation and literary review. J. Oral Res. 2018, 7, 373–377. [Google Scholar] [CrossRef]
- Lan, T.; Liu, X.; Liang, P.S.; Tao, Q. Osteochondroma of the coronoid process: A case report and review of the literature. Oncol. Lett. 2019, 18, 2270–2277. [Google Scholar] [CrossRef] [PubMed]
- Kono, T.; Yamada, K.; Ueno, S.; Matsushima, Y.; Izeki, T.; Morita, A. A case of osteochondroma of the coronoid process with long-term limited mouth opening. Jpn. J. Oral Maxillofac. Surg. 2019, 65, 22–28. [Google Scholar] [CrossRef]
- Samandari, M.H.; Shalamzari, M.E.; Ghazizadeh, M.; Navaei, H. Coronoid Hyperplasia (Jacob’s Disease) as a Rare Cause of Restricted Mouth Opening: A Case Report. Dent. Hypotheses 2020, 11, 62–68. [Google Scholar]
- Gómez, M.; Mejia-Ortega, L.; Hernández-Andara, A.; Ortega-Pertuz, A.I.; Villarroel-Dorrego, M. Chronic mandibular hypomobility related to a unilateral accessory condyle. A case report. Cranio 2022, 40, 502–508. [Google Scholar] [CrossRef]
- Alvarez, J.A.J.; Reyes, J.M.V. Jacob’s Disease, a rare Disease of the Coronoid Process of the Mandible. SVOA Dent. 2020, 1, 22–26. [Google Scholar]
- Avelar, R.L.; Neto, R.S.M.; da Silva Gaspar, B.; de Lima Praxedes Neto, R.A.; Silva, P.P.G.B. Development of temporomandibular ankylosis after diagnosis of Jacob’s disease: Clinical and tomographic assessment. Arch. Health Investig. 2020, 9, 426–428. [Google Scholar] [CrossRef]
- Okazawa, N.; Ueda, J.; Kawakami, T.; Yamamoto, Y.; Matsusue, Y.; Kirita, T. A case of Jacob’s disease and masticatory muscle tendon hyperplasia. J. Jpn. Temporomandibular Jt. Soc. 2020, 32, 77–83. [Google Scholar]
- Khadembaschi, D.; Arvier, J.; Beech, N.; Dolan, D.; McGill, J. Successful management of severe coronoid process hyperplasia in a patient with mucopolysaccharidosis VI: A case report. J. Surg. Case Rep. 2020, 2020, rjz388. [Google Scholar] [CrossRef]
- Alam, M.; Hasan, S.A.; Chandra, K. Zygomatico-Coronoid Pseudoarthrosis Due to Osteochandroma of Coronoid Process: A Rare Entity. Iran. J. Otorhinolaryngol. 2021, 33, 183–186. [Google Scholar]
- Leal, M.O.C.D.; Moreira, L.D.; Passador-Santos, F.; Soares, A.B.; Teixeira, R.G.; Jodas, C.R.P. Doença de Jacob: Relato de caso. RGO—Rev. Gaúcha Odontol. 2021, 69, e20210056. [Google Scholar] [CrossRef]
- Praal, F.R. Limitation of mandibular movement due to bilateral mandibular coronoid process enlargement. J. Oral Maxillofac. Surg. 1984, 42, 534–536. [Google Scholar] [CrossRef] [PubMed]
- Kaban, L.B.; Perrott, D.H.; Fisher, K. A protocol for management of temporomandibular joint ankylosis. J. Oral Maxillofac. Surg. 1990, 48, 1145–1151. [Google Scholar] [CrossRef] [PubMed]
- Sidebottom, A.J. Guidelines for the replacement of temporomandibular joints in the United Kingdom. Br. J. Oral Maxillofac. Surg. 2008, 46, 146–147. [Google Scholar] [CrossRef] [PubMed]
- Robiony, M.; Casadei, M.; Costa, F. Minimally invasive surgery for coronoid hyperplasia: Endoscopically assisted intraoral coronoidectomy. J. Craniofac. Surg. 2012, 23, 1838–1840. [Google Scholar] [CrossRef] [PubMed]







| Case No. | Author | Year | Age | Gender | Side | Type | MMO before Treatment (mm) | MMO after Treatment (mm) | Treatment | Treatment Follow-Up (Months) | Treatment Recurrence |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Jacob [1] | 1899 | 62 | / | / | CCE | / | / | None | Not applicable | Not applicable |
| 2 | Shakleford et al. [15] | 1943 | 15 | M | L | OC | 13 | / | Extraoral coronoidectomy | Not reported | Not reported |
| 3 | Shakleford et al. [15] | 1943 | 19 | M | R | OC | 10 | / | Extraoral coronoidectomy | Not reported | Not reported |
| 4 | Brandt [16] | 1943 | 37 | F | R | CCE | 25 | / | Extraoral coronoidectomy | Not reported | Not reported |
| 5 | Hallam [17] | 1947 | 18 | / | / | CCE | / | / | Extraoral coronoidectomy | Not reported | Not reported |
| 6 | Shakleford et al. [18] | 1949 | 38 | M | R | OC | / | / | Extraoral coronoidectomy | Not reported | Not reported |
| 7 | Brailsford et al. [19] | 1952 | 24 | M | L | OC | 13 | / | Not reported | Not reported | Not reported |
| 8 | Holmes et al. [20] | 1956 | 30 | M | R/L | OC | 7 | / | Intraoral coronoidectomy | Not reported | Not reported |
| 9 | Holmes et al. [21] | 1956 | 36 | M | L | OC | 8 | / | Intraoral coronoidectomy | Not reported | Not reported |
| 10 | Ginestet et al. [22] | 1956 | 19 | / | R/L | / | / | / | Intraoral coronoidectomy | Not reported | Not reported |
| 11 | Van Ziles et al. [22] | 1957 | 30 | M | R/L | CCE | 7 | / | Extraoral coronoidectomy | Not reported | Not reported |
| 12 | Levine et al. [23] | 1957 | 73 | F | L | OC | 6 | / | Not reported | Not reported | Not reported |
| 13 | Dingman et al. [24] | 1957 | 27 | M | R | OC | 8 | / | Extraoral coronoidectomy | Not reported | Not reported |
| 14 | Pap et al. [25] | 1958 | 30 | M | L | OC | 10 | / | Extraoral coronoidectomy | Not reported | Not reported |
| 15 | Antoni et al. [26] | 1958 | 29 | M | L | OC | / | / | Intraoral coronoidectomy | Not reported | Not reported |
| 16 | Chemin et al. [27] | 1958 | 20 | / | / | / | / | / | Intraoral coronoidectomy | Not reported | Not reported |
| 17 | Shira et al. [28] | 1958 | 14 | M | R/L | / | 8 | / | Extraoral coronoidectomy | Not reported | Not reported |
| 18 | Lebo [29] | 1961 | 18 | M | L | OC | 14 | 29 | Extraoral coronoidectomy | Not reported | Not reported |
| 19 | Mohnac [30] | 1962 | 18 | M | R/L | OC | 18 | / | Extraoral coronoidectomy | Not reported | Not reported |
| 20 | Van de Vijver [31] | 1962 | 18 | / | R/L | / | / | / | Intraoral coronoidectomy | Not reported | Not reported |
| 21 | Dechaume et al. [32] | 1964 | 13 | / | / | / | / | / | Intraoral coronoidectomy | Not reported | Not reported |
| 22 | Rottke et al. [33] | 1967 | 29 | / | / | / | / | / | Intraoral coronoidectomy | Not reported | Not reported |
| 23 | Allan et al. [34] | 1967 | 32 | F | R | CCE | 16 | 40 | Intraoral coronoidectomy | Not reported | Not reported |
| 24 | Allan et al. [34] | 1967 | 22 | M | L | CCE | 13 | 40 | Intraoral coronoidectomy | Not reported | Not reported |
| 25 | Meyer [35] | 1972 | 10 | F | R | OC | 20 | / | Intraoral coronoidectomy | Not reported | Not reported |
| 26 | James et al. [36] | 1974 | 52 | F | R | OC | 5 | 40 | Extraoral coronoidectomy | 12 | No |
| 27 | Cooper et al. [37] | 1974 | 43 | F | L | OC | 6 | / | Intraoral coronoidectomy | Not reported | Not reported |
| 28 | Takeda et al. [38] | 1975 | 14 | F | L | OC | 10 | / | Extraoral coronoidectomy | Not reported | Not reported |
| 29 | Singer et al. [39] | 1976 | 64 | M | R | OC | 5 | / | Intra/extraoral coronoidectomy | Not reported | Not reported |
| 30 | Ramon et al. [40] | 1977 | 45 | M | R | OC | / | / | Intra/extraoral coronoidectomy | Not reported | Not reported |
| 31 | Michel et al. [41] | 1977 | 30 | F | R | / | 10 | / | Intraoral coronoidectomy | Not reported | Not reported |
| 32 | Norman et al. [42] | 1980 | 21 | M | L | OC | 3 | / | Intraoral coronoidectomy | Not reported | Not reported |
| 33 | Ito et al. [43] | 1981 | 20 | F | L | OC | 3 | / | Extraoral coronoidectomy | Not reported | Not reported |
| 34 | Boland et al. [44] | 1983 | 25 | / | / | / | / | / | Intraoral coronoidectomy | Not reported | Not reported |
| 35 | Ishii et al. [45] | 1983 | 32 | F | L | OC | 7 | 41 | Intraoral coronoidectomy | Not reported | Not reported |
| 36 | Ishii et al. [45] | 1983 | 53 | M | R | OC | 20 | 37 | Intra/extraoral coronoidectomy | Not reported | Not reported |
| 37 | Revington [46] | 1984 | 24 | M | R | CCE | 9 | / | Extraoral coronoidectomy | 6 | Not reported |
| 38 | Tucker et al. [47] | 1984 | 16 | M | R | CH | 22 | / | Intraoral coronoidectomy | Not reported | Not reported |
| 39 | Macleod [48] | 1987 | 46 | F | / | CCE | 5 | / | Intraoral coronoidectomy | Not reported | Not reported |
| 40 | Schwartz et al. [49] | 1987 | 15 | M | L | OC | 18 | / | Extraoral coronoidectomy | Not reported | Not reported |
| 41 | Halling et al. [50] | 1989 | 22 | M | R | / | 21 | / | Intraoral coronoidectomy | Not reported | Not reported |
| 42 | Goudot et al. [51] | 1989 | 45 | / | L | / | / | / | Intraoral coronoidectomy | Not reported | Not reported |
| 43 | Totsuka et al. [52] | 1990 | 37 | F | L | OC | 2 | 28 | Intraoral coronoidectomy | Not reported | Not reported |
| 44 | Rames et al. [53] | 1990 | 36 | / | R/L | CH | / | / | Intraoral coronoidectomy | Not reported | Not reported |
| 45 | Asanami et al. [54] | 1990 | 17 | M | L | CCE | 8 | 64 | Intra/extraoral coronoidectomy | 36 | Not reported |
| 46 | Honig et al. [55] | 1993 | 22 | M | R | CH | 21 | / | Intraoral coronoidectomy | Not reported | Not reported |
| 47 | Kerscher et al. [56] | 1993 | 45 | M | L | OC | 14 | 32 | Intraoral coronoidectomy | Not reported | Not reported |
| 48 | Smyth et al. [57] | 1994 | 15 | M | R/L | CH | 4 | 40 | Extraoral coronoidectomy | 96 | Yes (96 months) |
| 49 | Gibbons et al. [58] | 1995 | 34 | M | R/L | OC | 19 | 34 | Intraoral coronoidectomy | Not reported | Not reported |
| 50 | Cenetoglu et al. [59] | 1996 | 19 | M | L | OC | 12 | 48 | Intraoral coronoidectomy | 12 | Not reported |
| 51 | Kermer et al. [60] | 1996 | 40 | M | L | OC | / | / | Extraoral coronoidectomy | Not reported | Not reported |
| 52 | Mizumoto et al. [61] | 1996 | 43 | M | L | OC | 11 | 49 | Extraoral coronoidectomy | 12 | Not reported |
| 53 | Constantinides et al. [62] | 1997 | 31 | M | R | OC | 10 | / | Extraoral coronoidectomy | 12 | Not reported |
| 54 | Gross et al. [63] | 1997 | 22 | M | L | OC | 20 | 40 | Intraoral coronoidectomy | Not reported | Not reported |
| 55 | Chen et al. [64] | 1998 | 57 | F | L | OC | 14 | 42 | Extraoral coronoidectomy | 72 | No |
| 56 | Takenobu et al. [65] | 1998 | 56 | F | L | OC | 2 | 30 | Intraoral coronoidectomy | 12 | Not reported |
| 57 | Manganaro [66] | 1998 | 26 | F | L | OC | / | / | Intraoral coronoidectomy | Not reported | Not reported |
| 58 | Ishii et al. [67] | 1998 | 25 | M | R | CH | 22 | 40 | Intraoral coronoidectomy | Not reported | Not reported |
| 59 | Chicareon et al. [68] | 1999 | 5 | M | R | OC | / | / | Not reported | Not reported | Not reported |
| 60 | Hernandez-Alfaro et al. [8] | 2000 | 22 | M | L | OC | 21 | 52 | Extraoral coronoidectomy | 6 | Not reported |
| 61 | Escuder y de la Torre et al. [14] | 2001 | 19 | M | L | / | 7 | / | Intraoral coronoidectomy | Not reported | Not reported |
| 62 | Escuder y de la Torre et al. [14] | 2001 | 16 | / | R/L | OC | 14 | 49 | Intraoral coronoidectomy | 12 | No |
| 63 | Emekli et al. [4] | 2002 | 26 | F | R | OC | 10 | 35 | Intraoral coronoidectomy | 6 | No |
| 64 | Emekli et al. [4] | 2002 | 21 | M | R | OC | 8 | 40 | Intra/extraoral coronoidectomy | Not reported | Not reported |
| 65 | Roychoudhury et al. [6] | 2002 | 32 | M | L | OC | 0 | 39 | Extraoral coronoidectomy | >12 | Not reported |
| 66 | Capote et al. [11] | 2005 | 23 | F | L | CCE | 30 | 40 | Intraoral coronoidectomy | 12 | Not reported |
| 67 | Matsumoto et al. [69] | 2005 | 38 | M | L | OC | 12 | 41 | Intra/extraoral coronoidectomy | 3 | Not reported |
| 68 | Akan et al. [70] | 2006 | 24 | M | R/L | CCE | 15 | 30 | Intraoral coronoidectomy | Not reported | Not reported |
| 69 | Villanueva et al. [71] | 2006 | 44 | F | L | OC | 30 | 43 | Intraoral coronoidectomy | Not reported | Not reported |
| 70 | Dede et al. [72] | 2007 | 20 | M | R/L | OC | 6 | / | Intraoral coronoidectomy | Not reported | Not reported |
| 71 | Zhong et al. [73] | 2009 | 39 | F | R | OC | 8 | 31 | Intraoral coronoidectomy | 9 | Not reported |
| 72 | Thota et al. [74] | 2009 | 15 | M | R/L | CCE | 15 | 44 | Intraoral coronoidectomy | 14 | No |
| 73 | Osman et al. [75] | 2009 | 43 | F | R | OC | 14 | 30 | Intraoral coronoidectomy | 6 | Not reported |
| 74 | D’Ambrosio et al. [13] | 2009 | 39 | M | L | OC | / | / | Intraoral coronoidectomy | Not reported | Not reported |
| 75 | Yesildag et al. [76] | 2010 | 16 | M | R | OC | 12 | 52 | Extraoral coronoidectomy | 14 | Not reported |
| 76 | Takafuji et al. [77] | 2011 | 21 | M | R | OC | 20 | 48 | Intraoral coronoidectomy | Not reported | Not reported |
| 77 | Ajila et al. [78] | 2011 | 28 | M | L | OC | 7 | / | Intraoral coronoidectomy | 12 | No |
| 78 | Coll-Anglada et al. [12] | 2011 | 52 | F | R | OC | 8 | 41 | Intraoral coronoidectomy | 6 | Not reported |
| 79 | Acosta-Feria et al. [79] | 2011 | 55 | F | R | OC | 20 | 40 | Extraoral coronoidectomy | 24 | No |
| 80 | Sreeramaneni et al. [7] | 2011 | 45 | F | L | OC | 5 | 40 | Intra/extraoral coronoidectomy | 3 | Not reported |
| 81 | Aoki et al. [80] | 2012 | 18 | M | R | OC | 51 | 61 | Intraoral coronoidectomy | 15 | No |
| 82 | Pacheco Ruiz et al. [81] | 2012 | 28 | M | R/L | OC | 2 | 40 | Intra/extraoral coronoidectomy | 3 | Not reported |
| 83 | Tavassol et al. [82] | 2012 | 13 | M | R/L | CH | 10 | 48 | Intraoral coronoidectomy | Not reported | Not reported |
| 84 | Choi et al. [83] | 2013 | 13 | M | R/L | CCE | 15 | 40 | Intraoral coronoidectomy | 4 | Not reported |
| 85 | Choi et al. [83] | 2013 | 13 | M | R/L | CCE | 20 | 45 | Intraoral coronoidectomy | Not reported | Yes (36 months) |
| 86 | Stringer et al. [84] | 2013 | 27 | M | L | OC | 10 | 40 | Intraoral coronoidectomy | Not reported | Not reported |
| 87 | Hosein et al. [85] | 2013 | 15 | M | L | OC | 22 | 41 | Intraoral coronoidectomy | 18 | Not reported |
| 88 | Losa-Munoz et al. [86] | 2014 | 42 | M | R | OC | 20 | 41 | Intraoral coronoidectomy | Not reported | Not reported |
| 89 | Dandriyal et al. [87] | 2014 | 20 | F | L | OC | 15 | 40 | Intraoral coronoidectomy | 54 | No |
| 90 | Zarembinski et al. [88] | 2014 | 50 | M | R | / | 35 | / | None | Not reported | Not reported |
| 91 | Fan et al. [89] | 2014 | 20 | M | L | OC | 25 | 45 | Intra/extraoral coronoidectomy | 20 | No |
| 92 | Rahim et al. [90] | 2014 | 19 | M | L | OC | 22 | / | Not reported | Not reported | Not reported |
| 93 | Reddy et al. [91] | 2014 | 21 | F | R | OC | 12 | 42 | Extraoral coronoidectomy | Not reported | Not reported |
| 94 | Sinha et al. [92] | 2014 | 58 | M | L | OC | / | / | Intraoral coronoidectomy | Not reported | Not reported |
| 95 | Sawada et al. [93] | 2015 | 14 | M | L | OC | 10 | 20 | Intraoral coronoidectomy | Not reported | No |
| 96 | Shin et al. [94] | 2016 | 39 | F | L | / | 21 | 41 | Intra/extraoral coronoidectomy | 36 | No |
| 97 | Mohanty et al. [95] | 2016 | 18 | M | R | OC | 11 | 40 | Extraoral coronoidectomy | 36 | No |
| 98 | Robiony et al. [96] | 2016 | 59 | F | R | OC | 9 | 49 | Extraoral coronoidectomy | 6 | Not reported |
| 99 | Imen et al. [97] | 2016 | 29 | M | L | OC | 5 | 55 | Extraoral coronoidectomy | Not reported | Not reported |
| 100 | Gangoli et al. [98] | 2017 | 15 | F | L | OC | 9 | 34 | Intraoral coronoidectomy | Not reported | Not reported |
| 101 | Choontharu et al. [99] | 2018 | 16 | F | L | OC | 43 | / | Intraoral coronoidectomy | 6 | No |
| 102 | Roscher et al. [100] | 2018 | 18 | F | L | OC | 20 | 41 | Intraoral coronoidectomy | 12 | Not reported |
| 103 | Villegas Cisneros et al. [101] | 2018 | 10 | M | R/L | CH | 19 | 35 | Intra/extraoral coronoidectomy | Not reported | Not reported |
| 104 | Lan et al. [102] | 2019 | 34 | F | R | OC | 5 | 36 | Intraoral coronoidectomy | 21 | No |
| 105 | Kono et al. [103] | 2019 | 51 | M | L | OC | 20 | 42 | Intraoral coronoidectomy | 30 | No |
| 106 | Samandari et al. [104] | 2019 | 28 | M | L | CH | 25 | / | Intraoral coronoidectomy | Not reported | Not reported |
| 107 | Gomez et al. [105] | 2020 | 54 | F | L | OC | 12 | 22 | Intraoral coronoidectomy | 12 | Not reported |
| 108 | Jimenez Alvarez et al. [106] | 2020 | 15 | M | R | OC | 10 | 40 | Intraoral coronoidectomy | 72 | Not reported |
| 109 | Avelar et al. [107] | 2020 | 6 | M | R/L | CH | 10 | 28 | Extraoral coronoidectomy | Not reported | No |
| 110 | Okazawa et al. [108] | 2020 | 27 | M | L | OC | 4 | 60 | Intra/extraoral coronoidectomy | 12 | No |
| 111 | Khadembaschi et al. [109] | 2020 | 14 | M | R/L | CCE | 8 | 45 | Extraoral coronoidectomy | 18 | Not reported |
| 112 | Alam et al. [110] | 2021 | 32 | M | R | OC | 8 | 38 | Extraoral coronoidectomy | Not reported | Not reported |
| 113 | Leal et al. [111] | 2021 | 11 | F | L | CCE | 20 | 25 | Intraoral coronoidectomy | Not reported | Not reported |
| 114 | Raccampo et al. | 2022 | 19 | F | R | CCE | 25 | 40 | Intraoral coronoidectomy | 12 | No |
| 115 | Raccampo et al. | 2022 | 18 | M | R | OC | 20 | 44 | Intraoral coronoidectomy | 12 | No |
| 116 | Raccampo et al. | 2022 | 23 | M | R/L | CH | 20 | 37 | Intraoral coronoidectomy | 14 | No |
| Classification Proposal | ||
|---|---|---|
| Grade 1 | Grade 1 A | An ipsilateral formation of a pseudojoint between an abnormal CPM and the inner aspect of the zygomatic bone determining an extra-articular ankylosis with a MMO ≥ 20 mm. |
| Grade 1 B | A bilateral formation of a pseudojoint between an abnormal CPM and the inner aspect of the zygomatic bone determining an extra-articular ankylosis with a MMO ≥ 20 mm. | |
| Grade 2 | Grade 2 A | An ipsilateral formation of a pseudojoint between an abnormal CPM and the inner aspect of the zygomatic bone determining an extra-articular ankylosis with a 20 ≤ MMO ≥ 10 mm. |
| Grade 2 B | A bilateral formation of a pseudojoint between an abnormal CPM and the inner aspect of the zygomatic bone determining an extra-articular ankylosis with a 20 ≤ MMO ≥ 10 mm. | |
| Grade 3 | Grade 3 A | An ipsilateral formation of a pseudojoint between an abnormal CPM and the inner aspect of the zygomatic bone determining an extra-articular ankylosis with a MMO ≤ 10 mm. |
| Grade 3 B | A bilateral formation of a pseudojoint between an abnormal CPM and the inner aspect of the zygomatic bone determining an extra-articular ankylosis with a MMO ≤ 10 mm. | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raccampo, L.; Panozzo, G.; Tel, A.; Di Cosola, M.; Colapinto, G.; Trevisiol, L.; D’agostino, A.; Sembronio, S.; Robiony, M. Jacob’s Disease: Case Series, Extensive Literature Review and Classification Proposal. J. Clin. Med. 2023, 12, 938. https://doi.org/10.3390/jcm12030938
Raccampo L, Panozzo G, Tel A, Di Cosola M, Colapinto G, Trevisiol L, D’agostino A, Sembronio S, Robiony M. Jacob’s Disease: Case Series, Extensive Literature Review and Classification Proposal. Journal of Clinical Medicine. 2023; 12(3):938. https://doi.org/10.3390/jcm12030938
Chicago/Turabian StyleRaccampo, Luca, Giorgio Panozzo, Alessandro Tel, Michele Di Cosola, Gianluca Colapinto, Lorenzo Trevisiol, Antonio D’agostino, Salvatore Sembronio, and Massimo Robiony. 2023. "Jacob’s Disease: Case Series, Extensive Literature Review and Classification Proposal" Journal of Clinical Medicine 12, no. 3: 938. https://doi.org/10.3390/jcm12030938
APA StyleRaccampo, L., Panozzo, G., Tel, A., Di Cosola, M., Colapinto, G., Trevisiol, L., D’agostino, A., Sembronio, S., & Robiony, M. (2023). Jacob’s Disease: Case Series, Extensive Literature Review and Classification Proposal. Journal of Clinical Medicine, 12(3), 938. https://doi.org/10.3390/jcm12030938







