The Relationship between Social Support and Anxiety Symptoms in Informal Carers: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
Social Support and Caregiving
2. Materials and Methods
2.1. Design
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Data Extraction and Synthesis
2.5. Quality Assessment
2.6. Analyses
3. Results
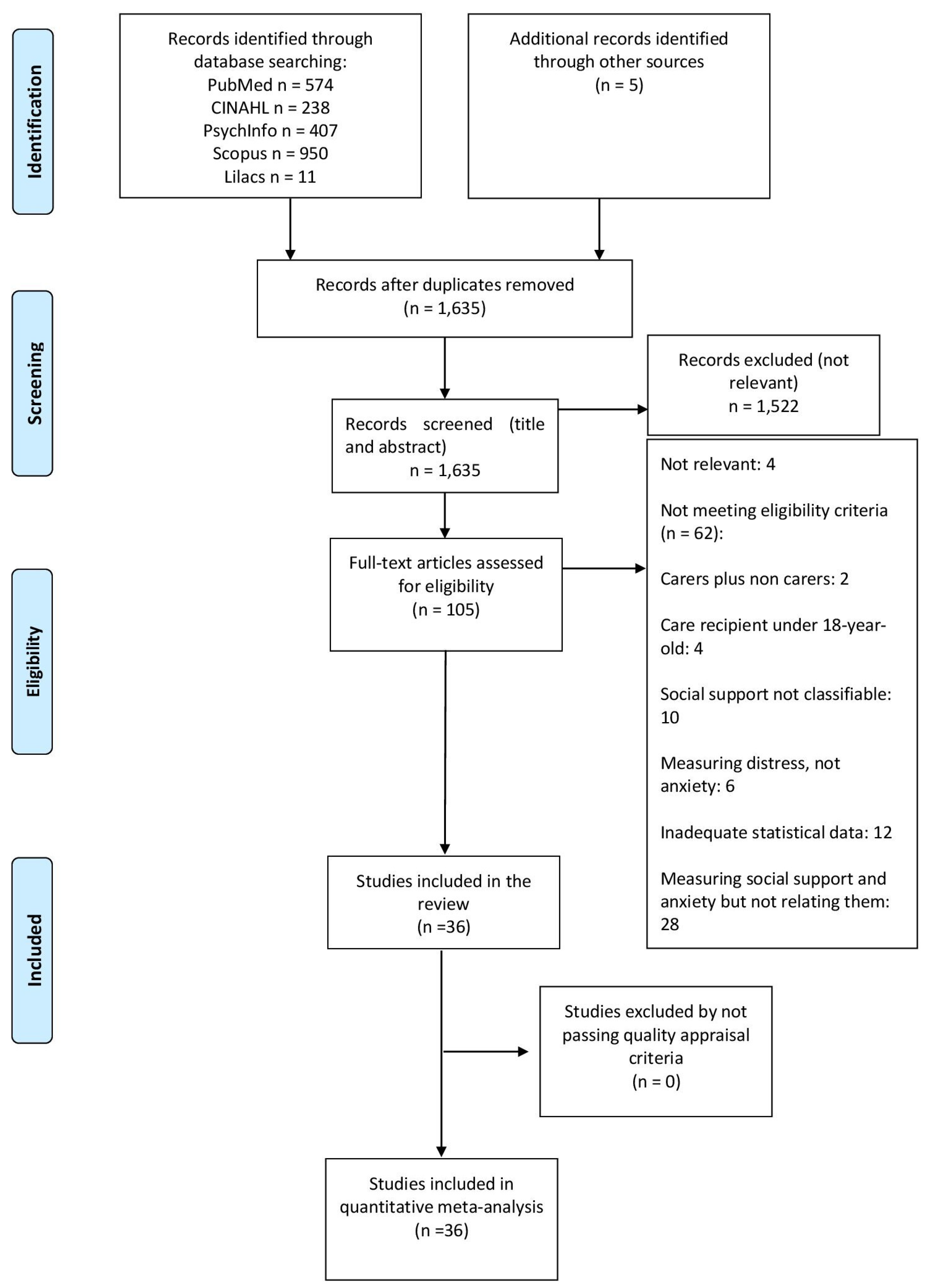
3.1. Search Results
3.2. Description of Included Studies
3.3. Quality Assessment
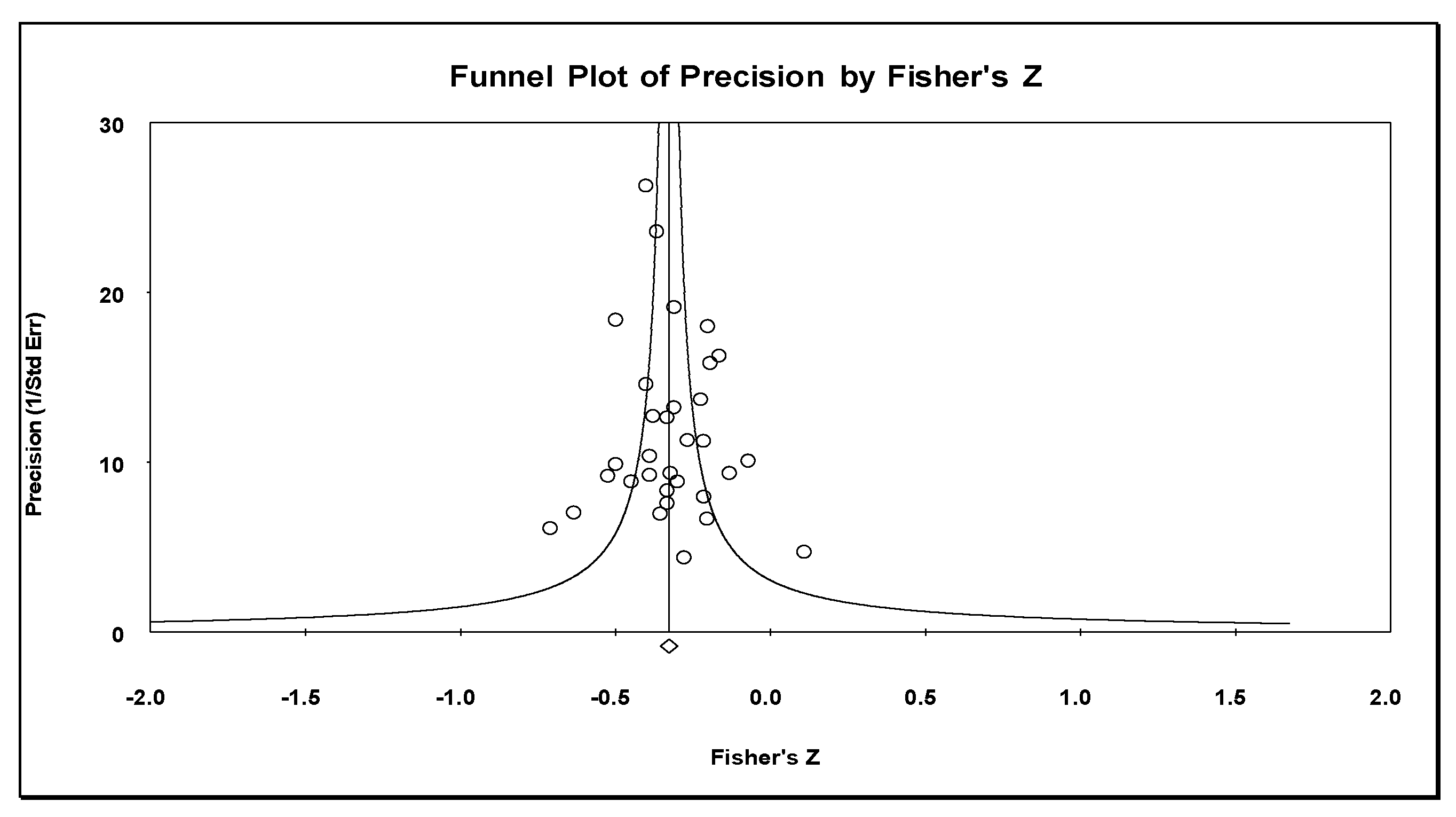
3.4. Results of the Meta-Analysis
3.4.1. Perceived Social Support
3.4.2. Received Social Support
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Social Support | |
| CPASS | Cancer Perceived Agents of Social Support |
| DSSI-Short | Duke Social Support Index (short version) |
| DUKE-UNC | Duke-UNK functional social support questionnaire |
| ESSS | Satisfaction with Social Support Scale |
| ISEL | Interpersonal Support Evaluation List |
| MG-SS | Social support subscale of the McGill Quality of Life Questionnaire |
| MSPSS | Multidimensional Scale of Perceived Social Support |
| MOS-SS | Medical Outcomes Study—Social Support Scale |
| OSS-3 | Oslo Social Support Scale |
| SSL-12-I | Social Support List—Interaction |
| SSSQ | Sarason Social Support Questionnaire |
| SSSS | Satisfaction with Social Support Scale |
| TBI-CareQOL | Social support factor of the Traumatic Brain Injury Caregiver Quality of Life |
| Anxiety | |
| BAI | Beck Anxiety Inventory |
| BSI | Brief Symptom Inventory |
| DASS | Depression Anxiety Stress Scale |
| EADS | Anxiety, Depression and Stress Scale |
| GAD | Generalized Anxiety Disorder Assessment |
| GAS | Goldberg Anxiety Scale |
| HADS | Hospital Anxiety Depression Scale |
| HARS | Hamilton Anxiety Rating Scale |
| IDA | Irritability, Depression, and Anxiety Scale |
| SCID | Structured Clinical Interview for the DSM-IV |
| POMS | Profile of Mood States |
| SAS | Self-Rating Anxiety Scale |
| STAI | State Trait Anxiety Inventory |
| TBI-CareQOL | Anxiety factor of the Traumatic Brain Injury Caregiver Quality of Life |
References
- Organisation for Economic Co-operation and Development. Health at a Glance 2021: OECD Indicators; OECD Publishing: Paris, France, 2021. [Google Scholar]
- Zarit, S.H. Diagnosis and management of caregiver burden in dementia. Handb. Clin. Neurol. 2008, 89, 101–106. [Google Scholar] [PubMed]
- Pearlin, L.I. The Stress Process Revisited: Reflections on Concepts and Their Interrelationships. In Handbook on the Sociology of Mental Health; Aneshensel, C.S., Phelan, J., Eds.; Plenum Press: New York, NY, USA, 1999; pp. 395–415. [Google Scholar]
- Quinn, C.; Toms, G. Influence of Positive Aspects of Dementia Caregiving on Caregivers’ Well-Being: A Systematic Review. Gerontologist 2019, 59, e584–e596. [Google Scholar] [CrossRef] [PubMed]
- Loh, A.Z.; Tan, J.S.; Zhang, M.W.; Ho, R.C. The Global Prevalence of Anxiety and Depressive Symptoms among Caregivers of Stroke Survivors. Journal of the American Medical Directors Association. Oncologist 2017, 18, 111–116. [Google Scholar]
- Sallim, A.B.; Sayampanathan, A.A.; Cuttilan, A.; Chun-Man Ho, R. Prevalence of Mental Health Disorders among Caregivers of Patients with Alzheimer Disease. J. Am. Med. Dir. Assoc. 2015, 16, 1034–1041. [Google Scholar] [CrossRef]
- Geng, H.M.; Chuang, D.M.; Yang, F.; Yang, Y.; Liu, W.M.; Liu, L.H.; Tian, H.M. Prevalence and determinants of depression in caregivers of cancer patients: A systematic review and meta-analy. Medicine 2018, 97, e11863. [Google Scholar]
- Cheng, S.T. Dementia Caregiver Burden: A Research Update and Critical Analysis. Curr. Psychiatry Rep. 2017, 19, 64. [Google Scholar] [CrossRef]
- Cooper, C.; Balamurali, T.B.; Livingston, G. A systematic review of the prevalence and covariates of anxiety in caregivers of people with dementia. Int. Psychogeriatr. 2007, 19, 175–195. [Google Scholar] [CrossRef]
- Mahoney, R.; Regan, C.; Katona, C.; Livingston, G. Anxiety and depression in family caregivers of people with Alzheimer disease: The LASER-AD study. Am. J. Geriatr. Psychiatry 2005, 13, 795–801. [Google Scholar] [CrossRef]
- Farina, N.; Page, T.E.; Daley, S.; Brown, A.; Bowling, A.; Basset, T.; Livingston, G.; Knapp, M.; Murray, J.; Banerjee, S. Factors associated with the quality of life of family carers of people with dementia: A systematic review. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2017, 13, 572–581. [Google Scholar] [CrossRef]
- Del-Pino-Casado, R.; Priego-Cubero, E.; Lopez-Martinez, C.; Orgeta, V. Subjective caregiver burden and anxiety in informal caregivers: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0247143. [Google Scholar] [CrossRef]
- Kahn, R.L.; Antonucci, T.C. Convoys over the life course: Attachment, roles, and social support. In Life-Span Development and Behavior; Baltes, P.B., Featherman, D.L., Lerner, R.M., Eds.; Academic Press: New York, NY, USA, 1980; pp. 254–263. [Google Scholar]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Cohen, S.; Wills, T. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [PubMed]
- Kaniasty, K.; Norris, F. Distinctions that Matter: Received Social Support, Perceived Social Support, and Social Embeddedness after Disasters. In Mental Health and Disasters; Neria, Y., Galea, S., Norris, F., Eds.; Cambridge University Press: Cambridge, UK, 2009; pp. 175–200. [Google Scholar] [CrossRef]
- Thompson, E.H., Jr.; Futterman, A.M.; Gallagher-Thompson, D.; Rose, J.M.; Lovett, S.B. Social support and caregiving burden in family caregivers of frail elders. J. Gerontol. 1993, 48, S245–S254. [Google Scholar] [CrossRef] [PubMed]
- del-Pino-Casado, R.; Frias-Osuna, A.; Palomino-Moral, P.A.; Ruzafa-Martinez, M.; Ramos-Morcillo, A.J. Social support and subjective burden in caregivers of adults and older adults: A meta-analysis. PLoS ONE 2018, 13, e0189874. [Google Scholar] [CrossRef]
- Barrera, M. Distinctions between social support concepts, measures, and models. Am. J. Community Psychol. 1986, 14, 413–445. [Google Scholar] [CrossRef]
- Reinhardt, J.; Boerner, K.; Horowitz, A. Good to Have but Not to Use: Differential Impact of Perceived and Received Support on Well-Being. J. Soc. Pers. Relatsh. 2006, 23, 117–129. [Google Scholar] [CrossRef]
- Cohen, S.; Gottlieb, B.; Underwood, L. Social Support Measurement and Intervention: A Guide for Health and Social Scientists; Oxford University Press: Oxford, UK, 2000. [Google Scholar]
- Del-Pino-Casado, R.; López-Martínez, C.; Osuna, A.F.; Orgeta, V. The relationship between perceived social support and psychological distress in carers of older relatives: A longitudinal cross-lagged analysis. J. Affect. Disord. 2022, 297, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Ma, C.; Han, H.; He, R.; Zhou, L.; Liang, R.; Yu, H. Caregiver burden in Alzheimer’s disease: Moderation effects of social support and mediation effects of positive aspects of caregiving. Int. J. Geriatr. Psychiatry 2018, 33, 1198–1206. [Google Scholar] [CrossRef]
- Smerglia, V.L.; Miller, N.B.; Sotnak, D.L.; Geiss, C.A. Social support and adjustment to caring for elder family members: A multi-study analysis. Aging Ment. Health 2007, 11, 205–217. [Google Scholar] [CrossRef]
- Vrabec, N. Literature review of social support and caregiver burden, 1980 to 1995. J. Nurs. Scholarsh. 1997, 29, 383–388. [Google Scholar]
- Costa, S.; Leite, Â.; Pinheiro, M.; Pedras, S.; Pereira, M.G. Burden and quality of life in caregivers of patients with amputated diabetic foot. PsyCh J. 2020, 9, 707–715. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Moher, D.; Booth, A.; Stewart, L. How to reduce unnecessary duplication: Use PROSPERO. Int. J. Obstet. Gynaecol. 2014, 121, 784–786. [Google Scholar]
- Booth, A.; Clarke, M.; Dooley, G.; Ghersi, D.; Moher, D.; Petticrew, M. The nuts and bolts of PROSPERO: An international prospective register of systematic reviews. Syst. Rev. 2012, 1, 2. [Google Scholar]
- Viswanathan, M.; Berkman, N.D.; Dryden, D.M.; Hartling, L. Assessing Risk of Bias and Confounding in Observational Studies of Interventions or Exposures: Further Development of the RTI Item Bank; Agency for Healthcare Rsearch and Quality: Rockville, MD, USA, 2013. [Google Scholar]
- Boyle, M.H. Guidelines for evaluating prevalence studies. Evid. Based Ment. Health 1998, 1, 37–39. [Google Scholar] [CrossRef]
- Watson, B.; Tatangelo, G.; McCabe, M. Depression and Anxiety Among Partner and Offspring Carers of People With Dementia: A Systematic Review. Gerontologist 2019, 59, e597–e610. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M.; Sorensen, S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. J. Gerontol. B Psychol. Sci. Soc. Sci. 2003, 58, P112–P128. [Google Scholar]
- Dekkers, O.M.; Vandenbroucke, J.P.; Cevallos, M.; Renehan, A.G.; Altman, D.G.; Egger, M. COSMOS-E: Guidance on conducting systematic reviews and meta-analyses of observational studies of etiology. PLoS Med. 2019, 16, e1002742. [Google Scholar] [CrossRef]
- Rothman, K.J.; Greenland, S.; Lash, T.L. Modern Epidemiology; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008. [Google Scholar]
- Atkins, D.; Best, D.; Briss, P.A.; Eccles, M.; Falck-Ytter, Y.; Flottorp, S.; Guyatt, G.H.; Harbour, R.T.; Haugh, M.C.; Henry, D.; et al. Grading quality of evidence and strength of recommendations. BMJ 2004, 328, 1490–1494. [Google Scholar] [CrossRef]
- Cooper, H.; Hedges, L.V.; Valentine, J.C. The Handbook of Research Synthesis and Meta-Analysis; Russell Sage Foundation Publications: New York, NY, USA, 2009. [Google Scholar]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. Br. Med. J. 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and Fill: A Simple Funnel Plot-Based Method of Testing and Adjusting for Publication Bias in Meta-Analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [PubMed]
- Ali, N.; Kausar, R. Social Support and Coping as Predictors of Psychological Distress in Family Caregivers of Stroke Patients. Pak. J. Psychol. Res. 2016, 31, 587–608. [Google Scholar]
- Ar, Y. Predictors of Depression, Anxiety, Grief and Growth among Turkish Offspring as Caregivers of Parents with Alzheimer’S Disease: A Multi-Method Study; Middle East Technical University: Ankara, Turkey, 2017. [Google Scholar]
- Bonsu, K.; Kugbey, N.; Ayanore, M.A.; Atefoe, E.A. Mediation effects of depression and anxiety on social support and quality of life among caregivers of persons with severe burns injury. BMC Res. Notes 2019, 12, 772. [Google Scholar] [CrossRef]
- Cabral, L.; Duarte, J.; Ferreira, M.; dos Santos, C. Anxiety, stress and depression in family caregivers of the mentally ill. Aten. Primaria 2014, 46, 176–179. [Google Scholar] [CrossRef]
- Crespo-López, M.; López-Martínez, J. Estrés y estado emocional en cuidadores de familiares mayores con y sin demencia. Rev. Esp. Geriatr. Gerontol. 2005, 40 (Suppl. S3), 55–61. [Google Scholar] [CrossRef]
- Cumming, T.B.; Cadilhac, D.A.; Rubin, G.; Crafti, N.; Pearce, D.C. Psychological Distress and Social Support in Informal Caregivers of Stroke Survivors. Brain Impair. 2008, 9, 152–160. [Google Scholar]
- Durkin, D.W. Changes in Emotional Well-Being and Self-Perceived Physical Health over Time among African American and White Male Caregivers of Older Adults; The University of Alabama: Tuscaloosa, AL, USA, 2010. [Google Scholar]
- Giovannetti, A.M.; Covelli, V.; Sattin, D.; Leonardi, M. Caregivers of patients with disorder of consciousness: Burden, quality of life and social support. Acta Neurol. Scand. 2015, 132, 259–269. [Google Scholar] [CrossRef]
- Gotze, H.; Brahler, E.; Gansera, L.; Schnabel, A.; Gottschalk-Fleischer, A.; Kohler, N. Anxiety, depression and quality of life in family caregivers of palliative cancer patients during home care and after the patient’s death. Eur. J. Cancer Care 2018, 27, e12606. [Google Scholar] [CrossRef]
- Hasson-Ohayon, I.; Goldzweig, G.; Braun, M.; Galinsky, D. Women with advanced breast cancer and their spouses: Diversity of support and psychological distress. Psycho-Oncol. 2010, 19, 1195–1204. [Google Scholar] [CrossRef]
- Jeong, A.; An, J.Y. The moderating role of social support on depression and anxiety for gastric cancer patients and their family caregivers. PLoS ONE 2017, 12, e0189808. [Google Scholar] [CrossRef]
- Kruithof, W.J.; Post, M.W.; Van Mierlo, M.L.; Van den Bos, G.A.; Man-van Ginkel, J.M.; Visser-Meily, J.M. Caregiver burden and emotional problems in partners of stroke patients at two months and one year post-stroke: Determinants and prediction. Patient Educ. Couns. 2016, 99, 1632–1640. [Google Scholar] [CrossRef] [PubMed]
- Kuscu, M.K.; Dural, U.; Önen, P.; Yaşa, Y.; Yayla, M.; Basaran, G.; Turhal, S.; Bekiroğlu, N. The association between individual attachment patterns, the perceived social support, and the psychological well-being of Turkish informal caregivers. Psycho-Oncol. 2009, 18, 927–935. [Google Scholar]
- Leibach, G. Examining the Relations between the Mental Health and Physical Examining the Relations between the Mental Health and Physical Health of Caregivers of MS in a Mexican Sample; Virginia Commonwealth University: Richmond, VA, USA, 2013. [Google Scholar]
- López Martinez, C. Sentido de Coherencia, Sobrecarga Subjetiva, Ansiedad y Síntomas Depresivos en Personas Cuidadoras de Familiares Mayores Dependientes. Ph.D. Thesis, Universidad de Jaén, Jaén, Spain, 2019. [Google Scholar]
- Manso Martinez, M.; Sánchez López, M.; Cuellar Flores, I. Salud y sobrecarga percibida en personas cuidadoras familiares de una zona rural. Clínica Y Salud 2013, 24, 37–45. [Google Scholar] [CrossRef]
- Moral Serrano, M.S.; Juan Ortega, J.; López Matoses, M.J.; Pellicer Magraner, P. Perfil y riesgo de morbilidad psíquica en cuidadores de pacientes ingresados en su domicilio. Aten Primaria 2003, 32, 77–87. [Google Scholar] [PubMed]
- Pagnini, F.; Rossi, G.; Lunetta, C.; Banfi, P.; Castelnuovo, G.; Corbo, M.; Molinari, E. Burden, depression, and anxiety in caregivers of people with amyotrophic lateral sclerosis. Psychol. Health Med. 2010, 15, 685–693. [Google Scholar] [CrossRef]
- Pearce, M.J.; Singer, J.L.; Prigerson, H.G. Religious coping among caregivers of terminally ill cancer patients: Main effects and psychosocial mediators. J. Health Psychol. 2006, 11, 743–759. [Google Scholar] [CrossRef]
- Raad, J.H.; Tulsky, D.S.; Lange, R.T.; Brickell, T.A.; Sander, A.M.; Hanks, R.A.; French, L.; Miner, J.A.; Kisala, P.A.; Carlozzi, N.E. Establishing the Factor Structure of a Health-Related Quality of Life Measurement System for Caregivers of Persons Living With Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2020, 101, 1220–1232. [Google Scholar] [CrossRef]
- Raveis, V.H.; Karus, D.; Pretter, S. Correlates of anxiety among adult daughter caregivers to a parent with cancer. J. Psychosoc. Oncol. 1999, 17, 1–26. [Google Scholar] [CrossRef]
- Rivera-Navarro, J.; Sepúlveda, R.; Contador, I.; Fernández-Calvo, B.; Ramos, F.; Tola-Arribas, M.; Goñi, M. Detection of maltreatment of people with dementia in Spain: Usefulness of the Caregiver Abuse Screen (CASE). Eur. J. Ageing 2018, 15, 87–99. [Google Scholar] [CrossRef]
- Rodi, N. Understanding Posttraumatic Stress Symptoms in Caregivers and Relatives of Adults. Ph.D. Thesis, Hofstra University, Hempstead, NY, USA, 2015. [Google Scholar]
- Serrano-Ortega, N. Afrontamiento, Sobrecarga Subjetiva y Ansiedad y Síntomas Depresivos en Personas Cuidadoras de Familiares Mayores Dependientes. Ph.D. Thesis, Universidad de Jaén, Jaén, Spain, 2017. [Google Scholar]
- Shaughnessy, V. The Impact of Mild Cognitive Impairment on Spouses: A Multi-Modal Investigation; York University: Toronto, ON, Canada, 2012. [Google Scholar]
- Shi, J.; Huang, A.; Jia, Y.; Yang, X. Perceived stress and social support influence anxiety symptoms of Chinese family caregivers of community-dwelling older adults: A cross-sectional study. Psychogeriatrics 2020, 20, 377–384. [Google Scholar] [CrossRef]
- Shu, C.C.; Cumming, R.G.; Kendig, H.L.; Blyth, F.M.; Waite, L.M.; Le Couteur, D.G.; Handelsman, D.J.; Naganathan, V. Health status, health behaviours and anxiety symptoms of older male caregivers: Findings from the Concord Health and Ageing in Men Project. Australas. J. Ageing 2017, 36, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Shukri, M.; Mustofai, M.; Md Yasin, M.; Tuan Hadi, T. Burden, quality of life, anxiety, and depressive symptoms among caregivers of hemodialysis patients: The role of social support. Int. J. Psychiatry Med. 2020, 55, 397–407. [Google Scholar] [CrossRef] [PubMed]
- Stevens, L.F.; Perrin, P.B.; Gulin, S.; Rogers, H.L.; Villaseñor Cabrera, T.; Jiménez-Maldonado, M.; Arango-Lasprilla, J.C. Examining the influence of three types of social support on the mental health of mexican caregivers of individuals with traumatic brain injury. Am. J. Phys. Med. Rehabil. 2013, 92, 959–967. [Google Scholar] [CrossRef] [PubMed]
- Tyler, C.M.; Henry, R.S.; Perrin, P.B.; Watson, J.; Villaseñor, T.; Lageman, S.K.; Smith, E.R.; Curiel, G.R.; Avila, J.; Jimenez Maldonado, M.E.; et al. Structural Equation Modeling of Parkinson’s Caregiver Social Support, Resilience, and Mental Health: A Strength-Based Perspective. Neurol. Res. Int. 2020, 2020, 7906547. [Google Scholar] [CrossRef]
- Vázquez Mata, E. Variables Psicológicas y Calidad de Vida Del Paciente con cÁncer de Mama Y Su Cuidador Principal; Universidad Autónoma De Nuevo León: San Nicolás de los Garza, Mexico, 2018. [Google Scholar]
- Vérez Cotelo, N.; Andrés Rodriguez, N.F.; Fornós Perez, J.A.; Andrés Iglesias, J.C.; Rios Lago, M. Burden and associated pathologies in family caregivers of Alzheimer’s disease patients in Spain. Pharm. Pract. 2015, 13, 521. [Google Scholar]
- Wooden, F. Psychological Factors and Heart Rate Variability in Family Caregivers of Alzheimer’S Patients; Unversity San Diego: San Diego, CA, USA, 2012. [Google Scholar]
- Thomas, S.; Kanske, P.; Schafer, J.; Hummel, K.V.; Trautmann, S. Examining bidirectional associations between perceived social support and psychological symptoms in the context of stressful event exposure: A prospective, longitudinal study. BMC Psychiatry 2022, 22, 736. [Google Scholar] [CrossRef]
- Melrose, K.L.; Brown, G.D.A.; Wood, A.M. When is received social support related to perceived support and well-being? When it is needed. Pers. Individ. Dif. 2015, 77, 97–105. [Google Scholar] [CrossRef]


| Studies (Author, Year) Country | n | Measure of Social Support | Measure of Anxiety | Design | Care Recipients |
|---|---|---|---|---|---|
| Ali, 2016 [42] Pakistan | 90 | MSPSS | DASS | Cross-sectional | Stroke |
| Ar, 2017 [43] Turkey | 190 | MSPSS | STAI | Cross-sectional | Dementia |
| Bonsu, 2019 [44] Ghana | 100 | MSPSS | BAI | Cross-sectional | Severe burns injury |
| Cabral, 2014 [45] Portugal | 104 | ESSS | EADS | Cross-sectional | Mental illness |
| Costa, 2020 [26] Portugal | 110 | SSSS | DASS | Cross-sectional | Diabetes |
| Crespo López, 2005 [46] Spain | 66 | SSSQ | HADS | Cross-sectional | Dementia and older people without dementia |
| Cumming, 2008 [47] Australia | 174 | MOS-SS | IDA | Cross-sectional (1) | Stroke |
| Durkin, 2010 [48] U.S.A. | 130 | ISEL-6 | STAI | Repeated measures | Frail older adults |
| Giovannetti, 2015 [49] Italy | 129 | MOS-SS | STAI | Cross-sectional | Disorders of consciousness |
| Götze, 2016 [50] Germany | 72 | OSS-3 | HADS | Repeated measures | Cancer |
| Hasson-Ohayon, 2010 [51] Israel | 150 | CPASS | BSI | Cross-sectional | Cancer |
| Jeong, 2017 [52] South Korea | 52 | DUKE-UNC | HADS | Cross-sectional | Cancer |
| Kruithof, 2016 [53] Netherlands | 183 | SSL-12-I | HADS | Repeated measures | Stroke |
| Kuscu, 2009 [54] Turkey | 51 | MSPSS | STAI | Cross-sectional | Cancer |
| Leibach, 2013 [55] Mexico | 81 | ISEL-12 | STAI | Cross-sectional | Multiple sclerosis |
| López-Martínez, 2019 [56] Spain | 81 | DUKE-UNC | GAS | Repeated measures | Frail older adults |
| Manso Martínez, 2012 [57] Spain | 88 | DUKE-UNC | HADS | Cross-sectional | Frail older adults |
| Moral Serrano, 2003 [58] Spain | 215 | DUKE-UNC | GAS | Cross-sectional | Frail older adults |
| Pagnini, 2010 [59] Italy | 40 | MG-SS | STAI | Cross-sectional | Amyotrophic lateral sclerosis |
| Pearce, 2006 [60] U.S.A. | 162 | ISEL | SCID | Cross-sectional | Cancer |
| Raad, 2020 [61] U.S.A. | 558 | TBI-CareQOL | TBI- CareQOL | Cross-sectional | Traumatic brain injury |
| Raveis, 2000 [62] U.S.A. | 164 | ISEL | STAI | Cross-sectional | Cancer |
| Rivera-Navarro, 2018 [63] Spain | 326 | DUKE-UNC | HADS | Cross-sectional | Dementia |
| Rodi, 2015 [64] U.S.A. | 87 | MOS-SS | BAI | Cross-sectional | Cancer |
| Serrano-Ortega, 2018 [65] Spain | 177 | DUKE-UNC | GAS | Repeated measures | Frail older adults |
| Shaughnessy, 2011 [66] Canada | 60 | MOS-SS | STAI | Cross-sectional | Mild cognitive impairment |
| Shi, 2020 [67] China | 693 | MSPSS | SAS | Cross-sectional | Frail older adults |
| Shu, 2017 [68] Australia | 193 | DSSI-Short | GAS | Cross-sectional | Frail older adults |
| Shukri,2020 [69] Malaysia | 340 | MSPSS | HADS | Cross-sectional | Haemodialysis patients |
| Stevens, 2013 [70] Mexico | 90 | ISEL | STAI | Cross-sectional | Traumatic brain injury |
| Tyler, 2020 [71] Mexico | 253 | ISEL | GAD | Cross-sectional | Parkinson’s disease |
| Vazquez Mata, 2018 [72] Mexico | 47 | DUKE-UNC | HADS | Cross-sectional (1) | Cancer |
| Verez Cotelo, 2015 [73] Spain | 25 | DUKE-UNC | STAI | Cross-sectional | Dementia |
| Wooden, 2012 [74] U.S.A. | 22 | MSPSS | POMS | Cross-sectional | Dementia |
| Studies | Probabilistic Sampling | Reliability and Validity of Measures (Mandatory) | Control of Confounders | Absence of Attrition |
|---|---|---|---|---|
| Ali, 2016 [42] | - | + | ? | N/A |
| Ar, 2017 [43] | - | + | ? | N/A |
| Bonsu, 2019 [44] | - | + | ? | N/A |
| Cabral, 2014 [45] | - | + | ? | N/A |
| Costa, 2020 [26] | - | + | ? | N/A |
| Crespo López, 2005 [46] | - | + | ? | N/A |
| Cumming, 2008 [47] | - | + | ? | N/A |
| Durkin, 2010 [48] | - | + | ? | + |
| Giovannetti, 2015 [49] | - | + | ? | N/A |
| Götze, 2016 [50] | - | + | - | N/A |
| Hasson-Ohayon, 2010 [51] | - | + | ? | N/A |
| Jeong, 2017 [52] | - | + | ? | N/A |
| Kruithof, 2016 [53] | - | + | ? | + |
| Kuscu, 2009 [54] | - | + | ? | N/A |
| Leibach, 2013 [55] | - | + | - | N/A |
| López-Martínez, 2019 [56] | + | + | + | + |
| Manso Martínez, 2012 [57] | - | + | + | N/A |
| Moral Serrano, 2003 [58] | - | + | - | N/A |
| Pagnini, 2010 [59] | - | + | + | N/A |
| Pearce, 2006 [60] | - | + | ? | N/A |
| Raad, 2020 [61] | - | + | ? | N/A |
| Raveis, 2000 [62] | - | + | - | N/A |
| Rivera-Navarro, 2018 [63] | - | + | ? | N/A |
| Rodi, 2015 [64] | - | + | ? | N/A |
| Serrano-Ortega, 2018 [65] | + | + | + | + |
| Shaughnessy, 2011 [66] | - | + | ? | N/A |
| Shi, 2020 [67] | - | + | ? | N/A |
| Shu, 2017 [68] | - | + | ? | N/A |
| Shukri,2020 [69] | - | + | ? | N/A |
| Stevens, 2013 [70] | - | + | + | N/A |
| Tyler, 2020 [71] | - | + | ? | N/A |
| Vazquez Mata, 2018 [72] | - | + | ? | N/A |
| Verez Cotelo, 2015 [73] | - | + | ? | N/A |
| Wooden, 2012 [74] | - | + | ? | N/A |
| Studies | Samples | n | Mean per Sample | r | 95% CI | I2 | Publication Bias | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | Funnel Plot | Egger’s Test p-Value | Trim and Fill | ||||||||
| Estimate | Variation | |||||||||||
| Perceived social support | 32 | 32 | 4970 | 155.3 | −0.31 | −0.35 | −0.27 | 6.5% | Asymmetric | 0.65 | −0.31 | 0.0 |
| Received social support | 3 | 3 | 526 | 397.4 | −0.15 | −0.22 | −0.08 | 0% | Asymmetric | 0.4 | −0.15 | 0.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Priego-Cubero, E.; Orgeta, V.; López-Martínez, C.; del-Pino-Casado, R. The Relationship between Social Support and Anxiety Symptoms in Informal Carers: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 1244. https://doi.org/10.3390/jcm12031244
Priego-Cubero E, Orgeta V, López-Martínez C, del-Pino-Casado R. The Relationship between Social Support and Anxiety Symptoms in Informal Carers: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(3):1244. https://doi.org/10.3390/jcm12031244
Chicago/Turabian StylePriego-Cubero, Emilia, Vasiliki Orgeta, Catalina López-Martínez, and Rafael del-Pino-Casado. 2023. "The Relationship between Social Support and Anxiety Symptoms in Informal Carers: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 3: 1244. https://doi.org/10.3390/jcm12031244
APA StylePriego-Cubero, E., Orgeta, V., López-Martínez, C., & del-Pino-Casado, R. (2023). The Relationship between Social Support and Anxiety Symptoms in Informal Carers: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(3), 1244. https://doi.org/10.3390/jcm12031244






