Comparison of Flexible Ureteroscope Performance between Reusable and Single-Use Models
Abstract
1. Introduction
2. Material and Methods
2.1. Operative Technique
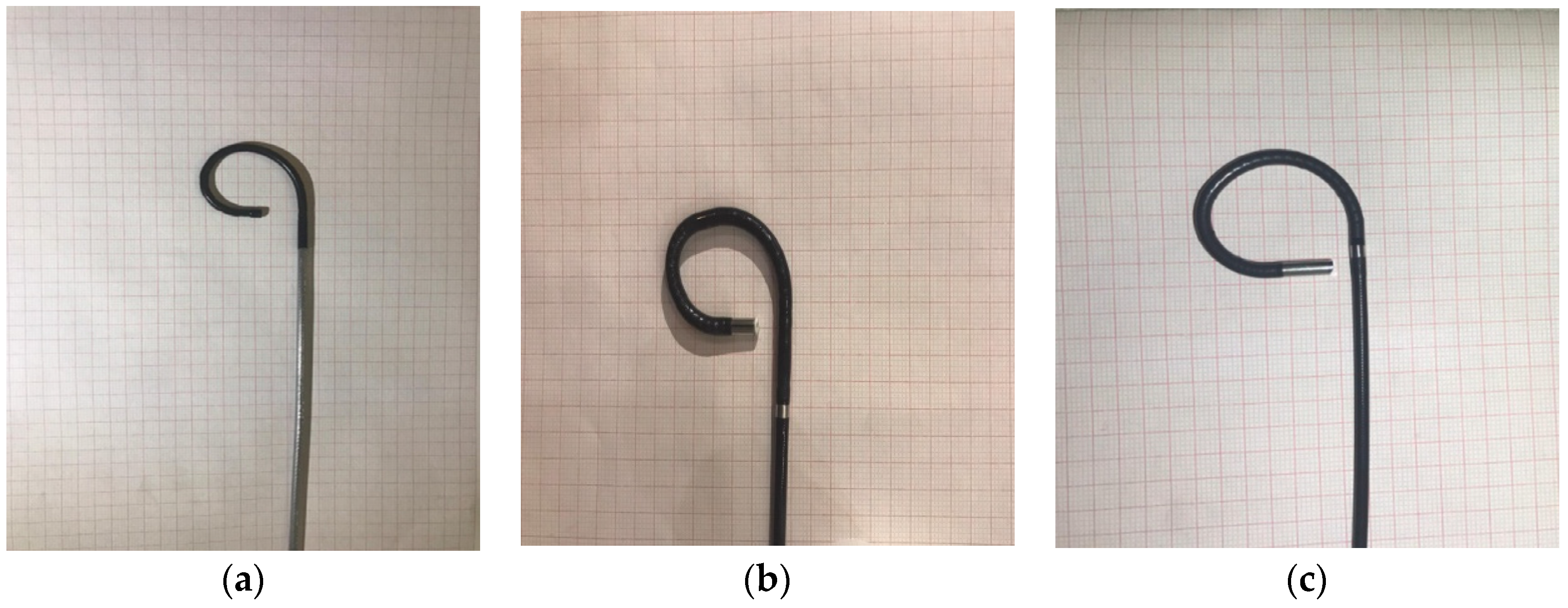
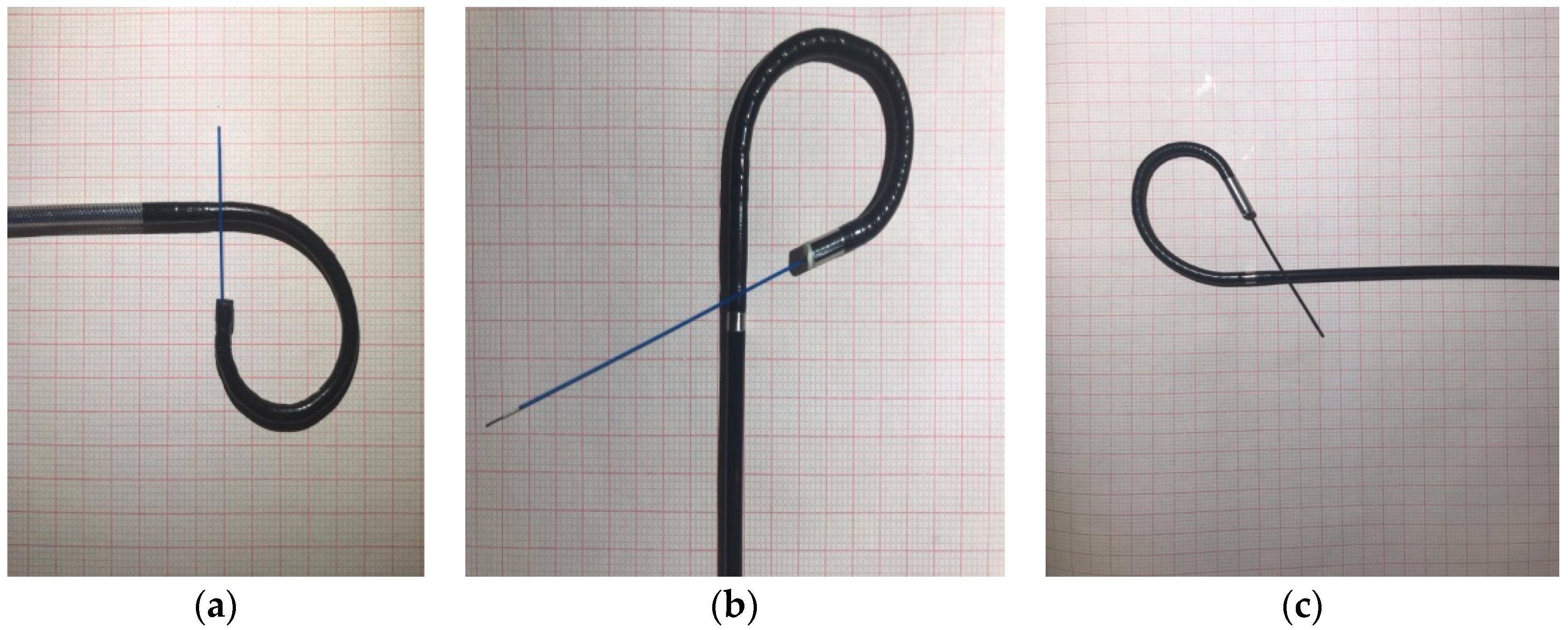
2.2. Description of Physical Characteristics of Flexible Ureteroscopes (UscopeUE3022, URF-V, and URF-V2)
2.3. Ex Vivo Comparison of Flexible Ureteroscopes (Uscope UE3022, URF-V, and URF-V2)
2.4. In Vivo Assessment of Flexible Ureteroscopes (Uscope UE3022, URF-V, and URF-V2)
3. Results
4. Discussion
5. Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nesbit, R.M. Congenital valvular obstruction of the prostatic urethra. J. Urol. 1944, 2, 167–169. [Google Scholar] [CrossRef]
- Marshall, V.F. Fiber Optics in Urology. J. Urol. 1964, 91, 10–14. [Google Scholar] [CrossRef]
- Grosso, A.A.; Sessa, F.; Campi, R.; Viola, L.; Polverino, P.; Crisci, A.; Minervini, A. Intraoperative and postoperative surgical complications after ureteroscopy, retrograde intrarenal surgery, and percutaneous nephrolithotomy: A systematic review. Minerva Urol. Nephrol. 2021, 73, 309–332. [Google Scholar] [CrossRef]
- Bagley, D.H.; Huffman, J.L.; Lyon, E.S. Flexible ureteropyeloscopy: Diagnosis and treatment in the upper urinary tract. J. Urol. 1987, 138, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Gridley, C.M.; Knudsen, B.E. Digital ureteroscopes: Technology update. Res. Rep. Urol. 2017, 9, 9–25. [Google Scholar] [CrossRef]
- Alenezi, H.; Denstedt, J.D. Flexible ureteroscopy: Technological advancements, current indications and outcomes in the treatment of urolithiasis. Asian J. Urol. 2015, 2, 133–141. [Google Scholar] [CrossRef]
- Proietti, S.; Dragos, L.; Molina, W.; Doizi, S.; Giusti, G.; Traxer, O. Comparison of New Single-Use Digital Flexible Ureteroscope Versus Nondisposable Fiber Optic and Digital Ureteroscope in a Cadaveric Model. J. Endourol. 2016, 30, 655–659. [Google Scholar] [CrossRef]
- Taguchi, K.; Usawachintachit, M.; Tzou, D.T.; Sherer, B.A.; Metzler, I.; Isaacson, D.; Chi, T. Micro-Costing Analysis Demonstrates Comparable Costs for LithoVue Compared to Reusable Flexible Fiberoptic Ureteroscopes. J. Endourol. 2018, 32, 267–273. [Google Scholar] [CrossRef]
- Martin, C.J.; McAdams, S.B.; Abdul-Muhsin, H.; Lim, V.M.; Nunez-Nateras, R.; Tyson, M.D.; Humphreys, M.R. The Economic Implications of a Reusable Flexible Digital Ureteroscope: A Cost-Benefit Analysis. J. Urol. 2017, 197 Pt 1, 730–735. [Google Scholar] [CrossRef] [PubMed]
- Emiliani, E.; Traxer, O. Single use and disposable flexible ureteroscopes. Curr. Opin. Urol. 2017, 27, 176–181. [Google Scholar] [CrossRef]
- Ziemba, J.B.; Matlaga, B.R. Understanding the costs of flexible ureteroscopy. Minerva Urol. Nefrol. 2016, 68, 586–591. [Google Scholar]
- Borofsky, M.D.C.; York, N.; Hoovler, C.; Lingeman, J. Global costs of modern flexible ureteroscopy at a high volume teaching hospital AUA, San Francisco. J. Urol. 2018, 195, e406. [Google Scholar]
- Ofstead, C.L.; Heymann, O.L.; Quick, M.R.; Johnson, E.A.; Eiland, J.E.; Wetzler, H.P. The effectiveness of sterilization for flexible ureteroscopes: A real-world study. Am. J. Infect. Control. 2017, 45, 888–895. [Google Scholar] [CrossRef] [PubMed]
- Scotland, K.B.; Chan, J.Y.H.; Chew, B.H. Single use flexible ureteroscopes: How do they compare to reusable ureteroscopes? J. Endourol. 2018, 2, 71–78. [Google Scholar] [CrossRef]
- Ventimiglia, E.; Godinez, A.J.; Traxer, O.; Somani, B. Cost comparison of single-use versus reusable flexible ureteroscope: A systematic review. Turk. J. Urol. 2020, 46 (Suppl. 1), S40–S45. [Google Scholar] [CrossRef]
- Kam, J.; Yuminaga, Y.; Beatttie, K.; Ling, K.I.; Arianayagaham, M.; Canagasingham, B.; Ferguson, R.; Varol, C.; Khadra, M.; Winter, M.; et al. Single use versus reusable digital flexible ureteroscopes: A prospective comparative study. Int. J. Urol. 2019, 10, 999–1005. [Google Scholar] [CrossRef]
- Multescu, R.; Geavlete, B.; Georgescu, D.; Geavlete, P. Improved durability of flex-Xc digital flexible ureteroscope: How long can you expect it to last? Urology 2014, 84, 32–35. [Google Scholar] [CrossRef]
- Marchini, G.S.; Batagello, C.A.; Monga, M.; Torricelli, F.C.M.; Vicentini, F.C.; Danilovic, A.; Mazzucchi, E. In Vitro Evaluation of Single-Use Digital Flexible Ureteroscopes: A Practical Comparison for a Patient-Centered Approach. J. Endourol. 2018, 32, 84–191. [Google Scholar] [CrossRef] [PubMed]
- Salvadó, J.A.; Olivares, R.; Cabello, J.M.; Cabello, R.; Moreno, S.; Pfeifer, J.; Velasco, A. Retrograde intrarenal surgery using the single–use flexible ureteroscope Uscope 3022 (Pusen™): Evaluation of clinical results. Cent. Eur. J. Urol. 2018, 71, 02–207. [Google Scholar]
- Johnston, T.J.; Baard, J.; Jean, d.l.R.; Doizi, S.; Giusti, G.; Knoll, T.; Proietti, S.; Brehmer, M.; Emiliani, E.; Pérez-Fentes, D.; et al. A clinical evaluation of the new digital single-use flexible ureteroscope (UscopePU3022): An international prospective multicentered study. Cent. Eur. J. Urol. 2018, 71, 453–461. [Google Scholar]
- Hennesey, D.B.; Fojecki, G.L.; Papa, N.P.; Lawrentschuk, N.; Bolton, D. Single-use disposable digital flexible ureteroscope: An ex vivo assessment and cost analysis. BJU Int. 2018, 121 (Suppl. 3), 55–61. [Google Scholar] [CrossRef]
- Wiseman, O.; Keeley, F.; Traxer, O.; Giusti, G.; Lipkin, M.; Preminger, G. MP51-03 Comparison of a new single-use digital flexible ureteroscope (LithoVue™) to a non-disposable fibre-optic flexible ureteroscope in a live porcine model. J. Urol. 2016, 195, e682. [Google Scholar] [CrossRef]
- Dale, J.; Kaplan, A.G.; Radvak, D.; Shin, R.; Ackerman, A.; Chen, T.; Lipkin, M.E. Evaluation of a novel single-use flexible ureteroscope. J. Endourol. 2017, 6, 903–907. [Google Scholar] [CrossRef] [PubMed]
- Molina, W.; Abrahams, M.; Lipkin, M.; Preminger, G.; Knoll, K. Evaluating the image quality of a novel single-use digital flexible ureteroscope. J. Endourol. 2016, 30, 11. [Google Scholar]
- Wollin, D.; Jiang, R.; Radvak, D.; Scales, C.; Ferrandino, M.; Simmons, W.N.; Lipkin, M. PD35-09 Comparison of a novel single-use flexible ureteroscope to currently existing reusable and single-use flexible ureteroscopes. J. Urol. 2017, 197, e666. [Google Scholar] [CrossRef]
- Schlager, D.; Hein, S.; Obaid, M.A.; Wilhelm, K.; Miernik, A.; Schoenthaler, M. Performance of single-use Flexorvue vs reusable Boavision ureteroscope for visualization of calices and stone extraction in an artificial kidney model. J. Endourol. 2017, 31, 1139–1144. [Google Scholar] [CrossRef]
- Carey, R.I.; Gomez, C.S.; Maurici, G.; Lynne, C.M.; Leveillee, R.J.; Bird, V.G. Frequency of ureteroscope damage seen at a tertiary care center. J. Urol. 2006, 176, 607–610. [Google Scholar] [CrossRef]
- Carey, R.I.; Martin, C.J.; Knego, J.R. Prospective evaluation of refurbished flexible ureteroscope durability seen in a large public tertiary care center with multiple surgeons. Urology 2014, 84, 42–45. [Google Scholar] [CrossRef]
- Baboudjian, M.; Pradere, B.; Martin, N.; Gondran-Tellier, B.; Angerri, O.; Boucheron, T.; Bastide, C.; Emiliani, E.; Misrai, V.; Breda, A.; et al. Life Cycle Assessment of Reusable and Disposable Cystoscopes: A Path to Greener Urological Procedures. Eur. Urol. Focus 2022. epub ahead of print. [Google Scholar] [CrossRef]
- Liao, P.; Wei, W.; Xiaoshuai, G.; Xingpeng, D.; Deyi, L. Fluoroless versus conventional ureteroscopy for urinary stones: A systematic review and meta-analysis. Minerva Urol. Nephrol. 2021, 73, 299–308. [Google Scholar] [CrossRef]
| Model | Diameter (Tip/Tube) | Working Channel | Working Length | Deflection (Up/Down) | Field Of View | Direction of View |
|---|---|---|---|---|---|---|
| Olympus URF-V | 8.5 F/9.9 F | 1 × 3.6 F | 670 mm | 180°/275° | 90° | 0° |
| Olympus URF-V2 | 8.4 F | 1 × 3.6 F | 670 mm | 275°/275° | 80° | 0° |
| Uscope UE3022 | 9.2 F | 1 × 3.6 F | 650 mm | 270°/270° | 120° | 0° |
| Model | Visibility Score | Maneuverability Score |
|---|---|---|
| Olympus URF-V | 4.8 | 3.8 |
| Olympus URF-V2 | 4.7 | 4.2 |
| Uscope UE3022 | 4.8 | 4.2 |
| Type of Accessory Instruments | 150 cm H2O Irrigation (mL/min) | ||
|---|---|---|---|
| URF-V | URF-V2 | Uscope UE3022 | |
| None (empty channel) | 22 | 21 | 35 |
| 0.035 Guidewire | 1 | 1 | 2 |
| Ho:YAG laser fiber | 9 | 10 | 19 |
| ZeroTip basket | 1 | 0 | 2 |
| Type of Accessory Instruments | Maximal Deflection (One Direction/Second Direction) | ||
|---|---|---|---|
| URF-V | URF-V2 | USCOPE UE3022 | |
| Manufacturer data | 270°/180° | 275°/275° | 270°/270° |
| None (empty channel) | 271°/172° | 273°/274° | 275°/269° |
| 0.035 Guidewire | 265°/157° | 244°/240° | 270°/269° |
| Ho:YAG laser fiber | 249°/156° | 238°/238° | 270°/269° |
| ZeroTip basket | 261°/155° | 252°/248° | 272°/260° |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bragaru, M.; Multescu, R.; Geavlete, P.; Popescu, R.; Geavlete, B. Comparison of Flexible Ureteroscope Performance between Reusable and Single-Use Models. J. Clin. Med. 2023, 12, 1093. https://doi.org/10.3390/jcm12031093
Bragaru M, Multescu R, Geavlete P, Popescu R, Geavlete B. Comparison of Flexible Ureteroscope Performance between Reusable and Single-Use Models. Journal of Clinical Medicine. 2023; 12(3):1093. https://doi.org/10.3390/jcm12031093
Chicago/Turabian StyleBragaru, Marius, Razvan Multescu, Petrisor Geavlete, Razvan Popescu, and Bogdan Geavlete. 2023. "Comparison of Flexible Ureteroscope Performance between Reusable and Single-Use Models" Journal of Clinical Medicine 12, no. 3: 1093. https://doi.org/10.3390/jcm12031093
APA StyleBragaru, M., Multescu, R., Geavlete, P., Popescu, R., & Geavlete, B. (2023). Comparison of Flexible Ureteroscope Performance between Reusable and Single-Use Models. Journal of Clinical Medicine, 12(3), 1093. https://doi.org/10.3390/jcm12031093







